Search
- Page Path
- HOME > Search
Original Articles
- Biomechanical finite element analysis of a femoral neck system fixation construct for femur neck fractures and clinical implications
- Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):133-142. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00108
-
 Abstract
Abstract
 PDF
PDF - Background
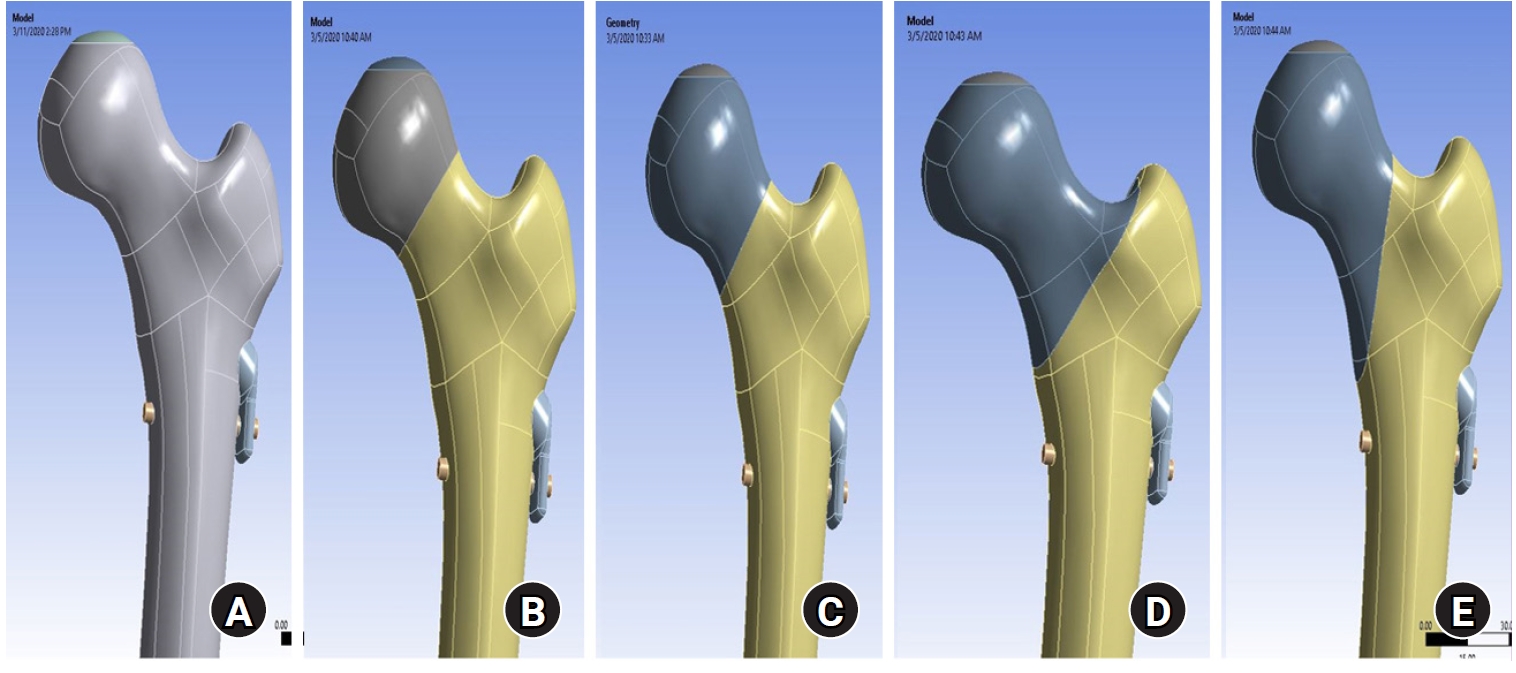
This study assessed the structural/mechanical stability of fixation constructs with a femoral neck system (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications.
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital, 68.56 MPa for a transcervical, 344.54 MPa for a basicervical, and 130.59 MPa for a vertical model. The maximum VMS of FNS was 840.34 MPa for a subcapital, 637.37 MPa for a transcervical, 464.07 MPa for a basicervical, and 421.01 MPa for a vertical model. The stress distribution of basicervical and vertical fractures differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
FNS fixation should be performed with consideration the osseous anchorage in the femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution. Level of evidence: IV.
- 1,614 View
- 74 Download

- Intra-Articular Alterations after Suprapatellar Nailing in Tibial Shaft Fractures: An Arthroscopic Evaluation
- GwangChul Lee, Sung Hun Yang, Sung Min Jo, Jeong Min Kook
- J Korean Fract Soc 2022;35(4):129-134. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.129
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study attempted to study the intra-articular changes due to intramedullary nailing through the suprapatellar approach by evaluating the joint cartilage damage and presence of foreign bodies through a comparison of the pre- and post-operative status evaluated by knee arthroscopy.
Materials and Methods
This retrospective study analyzed fifteen patients who underwent intramedullary nailing through the suprapatellar approach for proximal tibial shaft fracture from January 2017 to March 2020. The condition of the joint cartilage and the presence of foreign substances in the patellofemoral joint were evaluated. The cartilage status of the patellofemoral joint was evaluated using the International Cartilage Repair Society (ICRS) grading system. Data from the ICRS grading and the visual analogue scale (VAS) scores of the femoral and patellar cartilage were compared to each independent variable surveyed.
Results
All the intra-articular structures before nailing were normal. In all cases after nailing, articular cartilage damage of the patellofemoral joint and intra-articular debris were observed. The average VAS score was 0.6 (0-1) before surgery and 2.27 (0-4) after surgery. There were no statistically significant differences except for the correlation in the diameter of the tibia nail and femoral ICRS grade (p=0.001) and the damage to the cartilage was greater in the femoral cartilage than that to the patella (p=0.001).
Conclusion
Intra-articular damage appears to be unavoidable in suprapatellar nailing. Further research is needed on the long-term effects of intra-articular damage and on methods to reduce this damage.
- 402 View
- 6 Download

Case Report
- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture
- Soon Ho Huh, Hong-Man Cho, Ji-Yeon Park
- J Korean Fract Soc 2021;34(3):112-116. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.112
-
 Abstract
Abstract
 PDF
PDF - A helical blade type of hip screw is used widely for the operative management of femoral trochanteric fractures. A 73-year-old female patient was admitted for femoral trochanteric fracture AO/OTA type 31A2.2. A helical blade locking sleeve dissembled 18 weeks after surgery did not achieve accurate reduction. The patient underwent bipolar hip hemiarthroplasty because the fracture reduction was lost, and it was impossible to remove the remaining helical blade without bone loss. The authors report this case of a rare complication of helical blade.
- 458 View
- 3 Download

Review Article
- Pediatric around Elbow Fracture
- Taehun Kim, Jaeho Cho, Seungmin Chung
- J Korean Fract Soc 2021;34(1):44-49. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.44
-
 Abstract
Abstract
 PDF
PDF - This study assessed the current concepts of pediatric elbow fractures. PubMed and Embase databases were searched for publications in English on elbow fractures. Papers believed to yield significant findings to this area were included in this review. The supracondyle of humerus, lateral condyle of the humerus, proximal radius, and proximal ulna fractures were included. Sixteen papers and textbooks were selected. Pediatric elbow fractures should be evaluated for combined injuries. Treatment should be done accurately for each fracture for the further growth of children.
- 400 View
- 9 Download

Original Articles
- Comparison of the Clinical and Radiographic Results between 125° and 130° Caput-Collum-Diaphyseal Angle Proximal Femoral Nail Anti-Rotation II in Patients with Intertrochanteric Fracture
- Soo Jae Yim, Yong Bok Park, Hyun Kwon Kim, Sin Hyung Park
- J Korean Fract Soc 2020;33(4):210-216. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.210
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the clinical and radiographic results of two proximal femoral nail antirotation II (PFNA-II) angled by 125° and 130° in patients with intertrochanteric fractures.
Materials and Methods
From March in 2015 to September in 2016, 65 patients who underwent a closed reduction and internal fixation with PFNA-II for a femoral intertrochanteric fracture were evaluated retrospectively. The minimum follow-up period was two years. Of those, 30 and 35 patients underwent 125° angled PFNA-II and 130° angled PFNA-II, respectively. The clinical performance was evaluated using the Harris hip score, WOMAC (Western Ontario and McMaster Universities Osteoarthrtis Index), and UCLA (University of California Los Angeles) score. Radiographic analyses were performed using standardized anteroposterior and lateral radiographs to assess the implant position and quality of reduction. The blade length, distance between the blade tip and the tip of the greater trochanter, and distance between the blade tip and the most lateral protrusion point of the greater trochanter in the two groups were measured and compared.
Results
The clinical results, including the Harris hip score, WOMAC, and UCLA, were similar in the two groups at the last follow-up postoperatively. In the radiography evaluation, the implant position, quality of reduction, and the blade length were similar in the two groups. The distances between the blade tip and the tip of the greater trochanter were 52.60±3.53 mm and 58.07±5.54 mm in the 125° angled PFNA-II and 130° angled PFNA-II groups, respectively. The distance between the blade tip and the most lateral protrusion point of greater trochanter were 16.48±2.54 mm and 21.19±4.43 mm in the 125° angled PFNA-II and 130° angled PFNA-II groups, respectively. The differences were significant (p=0.031, p=0.012).
Conclusion
The operation with the 125° angled PFNA-II showed a more superior and lateral position of the blade than that with the 130° angled PFNA-II. Nevertheless, lateral thigh pain can occur when the blade is positioned superolaterally.
- 474 View
- 2 Download

- Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
- Se Jin Kim, Hong Man Cho, Jiyeon Park, Ki Yong An, Young Woo Chung, Woojin Shin
- J Korean Fract Soc 2020;33(4):179-188. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.179
-
 Abstract
Abstract
 PDF
PDF - Purpose
Intertrochanteric fractures can be treated using proximal femoral nail antirotation (PFNA). This study examined the clinical and radiological results of the intraoperative fracture compression.
Materials and Methods
Ninety-four patients underwent intraoperative compression (Group I), and 88 patients underwent natural sliding only (Group II). The patients were followed-up for more than two years. All patients met the following seven conditions: (1) AO/OTA 31-A1, A2 type intertrochanter fracture, (2) availability of compression of more than one cortical bone in the anterior or medial region of the fracture site under the preoperative imaging test, (3) Singh index grade ≥3, (4) blade position: center-center, center-inferior, (5) tip-apex distance <25 mm, (6) reduction status of good or very good, and (7) positive or neutral medial cortical support position with slightly valgus reduction.
Results
A slight tendency toward significant differences in acute phase pain between the two groups was observed at six weeks postoperatively (p=0.073). Twenty-four months after surgery, lateral extension of the PFNA helical blade between the two groups showed significant differences (p=0.017). Fracture gaps measured immediately after surgery showed significant differences (p=0.001), and a clear tendency for a significant difference in the average fracture union time was found (p=0.065).
Conclusion
Intraoperative fracture compression, intraoperative fracture compression appears beneficial to achieve a successful union of trochanteric fractures provided that all conditions are met to apply the method safely. -
Citations
Citations to this article as recorded by- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
Journal of the Korean Fracture Society.2022; 35(4): 151. CrossRef
- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- 616 View
- 3 Download
- 1 Crossref

Case Report
- Treatment of Neglected Proximal Interphalangeal Fracture Dislocation Using a Traction Device: A Case Report
- Yongun Cho, Jai Hyung Park, Se Jin Park, Ingyu Lee, Eugene Kim
- J Korean Fract Soc 2019;32(4):222-226. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.222
-
 Abstract
Abstract
 PDF
PDF - This paper reports the use of a traction device for the treatment of neglected proximal interphalangeal fracture dislocations. A 44-year-old man with a fracture dislocation of a right ring finger proximal interphalangeal joint was admitted 17 days after the injury. Closed reduction and external fixation were performed using a dynamic traction device and C-arm under a brachial plexus block. Passive range of motion exercise was started after two weeks postoperatively and active range of motion exercise was started after three weeks. The traction device was removed after five weeks. No infection occurred during the traction period. No subluxation or displacement was observed on the X-ray taken two months postoperatively. The active range of motion of the proximal interphalangeal joint was 90°. The patient was satisfied with the functional result of the treatment with the traction device. The dynamic traction device is an effective treatment for neglected fracture dislocations of the proximal interphalangeal joint of a finger.
- 1,198 View
- 2 Download

Original Articles
- Use of a Distraction Dynamic External Fixator in the Treatment of Comminuted Middle Phalanx Base Fractures
- Sang Woo Kim, Chae Chil Lee, Sang Hun Ko, Il Yeong Hwang, Min Seok Kim, Woo Young Jin
- J Korean Fract Soc 2019;32(1):1-5. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This paper suggests the use of distraction dynamic external fixators (DDEF) for the treatment of proximal middle phalanx fractures.
MATERIALS AND METHODS
Seven patients, who were diagnosed with comminuted intra-articular fractures at the base of the middle phalanx from February 2014 to November 2016, were enrolled in this study (volar aspect 6 cases, dorsal aspect 1 case). They underwent a closed reduction under a C-arm image intensifier, and DDEF was applied with general anesthesia. Range of motion (ROM) exercise was encouraged after 3 to 5 days postoperatively, and DDEF was removed after 5 weeks. Subluxation, angulation and displacement were evaluated 6 weeks postoperatively.
RESULTS
The patients who were treated with DDEF showed a normal proximal interphalangeal joint ROM (100°), and there was no subluxation or displacement on the X-ray film 6 weeks postoperatively. In addition, there were no signs of infection, such as local heat, redness, and pus-like discharge.
CONCLUSION
DDEF helps maintain the reduction and reducing forces through the ligamentotaxis. The joint stiffness is reduced, which it makes early return to daily life easier. -
Citations
Citations to this article as recorded by- Treatment of Neglected Proximal Interphalangeal Fracture Dislocation Using a Traction Device: A Case Report
Yongun Cho, Jai Hyung Park, Se-Jin Park, Ingyu Lee, Eugene Kim
Journal of the Korean Fracture Society.2019; 32(4): 222. CrossRef
- Treatment of Neglected Proximal Interphalangeal Fracture Dislocation Using a Traction Device: A Case Report
- 815 View
- 0 Download
- 1 Crossref

- Computational Simulation of Multiple Cannulated Screw Fixation for Femoral Neck Fractures and the Anatomic Features for Clinical Applications
- Jin Hoon Jeong, Gu Hee Jung
- J Korean Fract Soc 2018;31(2):37-44. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.37
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To identify the anatomic features for clinical applications through a computational simulation of the fixation of three cannulated screws for a femoral neck fracture.
MATERIALS AND METHODS
Thirty cadaveric femurs underwent computed tomography and the images were transferred to the Mimics® program, resulting in three-dimensional proximal femur models. A three-dimensional scan of the 7.0 mm cannulated screw was performed to enable computerized virtual fixation of multiple cannulated screws for femoral neck fractures. After positioning the screws definitively for cortical support, the intraosseous position of the cannulated screws was evaluated in the anteroposterior image and axial image direction.
RESULTS
Three cannulated screws located at the each ideal site showed an array of tilted triangles with anterior screw attachment and the shortest spacing between posterior and central screws. The central screw located at the lower side was placed in the mid-height of the lesser trochanter and slightly posterior, and directed toward the junction of femoral head and neck to achieve medial cortical support. All the posterior screws were limited in height by the trochanteric fossa and were located below the vastus ridge, but the anterior screws were located higher than the vastus ridge in 10 cases. To obtain the maximum spacing of the anterior and posterior screws on the axial plane, they should be positioned parallel to the cervical region nearest the cortical bone at a height not exceeding the vastus ridge.
CONCLUSION
The position of cannulated screws for cortical support were irregular triangular arrangements with the anterosuperior apex. The position of the ideal central screw in the anteroposterior view was at the mid-height of the lesser trochanter toward the junction of the femoral head and neck, and the anterior and posterior screws were parallel to the neck with a maximal spread just inferior to the vastus ridge. -
Citations
Citations to this article as recorded by- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
Ju-Yeong Kim
Journal of the Korean Fracture Society.2023; 36(1): 1. CrossRef
- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
- 561 View
- 0 Download
- 1 Crossref

Review Article
- Conservative Treatment of Proximal Humeral Fracture
- Hwansub Hyun, Jonghyun Ahn, Sang Jin Shin
- J Korean Fract Soc 2018;31(1):29-35. Published online January 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.1.29
-
 Abstract
Abstract
 PDF
PDF - A proximal humeral fracture is an osteoporotic fracture that often occurs in elderly women. Approximately 80% of all proximal humeral fractures are non-displaced fractures, which can be treated with conservative treatment to achieve stable union. The treatment plan for fractures involving displaced and comminuted fractures is controversial. Malunion, avascular necrosis of the humeral head, and shoulder stiffness due to conservative treatment can occur but the functional deterioration is low and the patient satisfaction is high. The indications for the conservative management of proximal humeral fractures include a non-displaced fracture and a 2-part fracture, low-functional demanded 3-part fracture, and operative-limited 4-part fracture. Recently, the surgical indications have expanded as technological advances in surgical fixation methods and functional needs of elderly patients are increasing. Current treatment policy decisions tend to be determined by the personal preference and expert opinion rather than by evidence-based decision-making.
-
Citations
Citations to this article as recorded by- The Effect of Postoperative Korean Traditional Medicine for the of Proximal Humeral Fracture: A Case Report
Hyun Il Go, Hangyul Choi, Jieun Hong, Nam geun Cho
Journal of Acupuncture Research.2019; 36(1): 50. CrossRef
- The Effect of Postoperative Korean Traditional Medicine for the of Proximal Humeral Fracture: A Case Report
- 446 View
- 8 Download
- 1 Crossref

Original Article
- The Determination of Optimal Entry Point for Proximal Femoral Nail Antirotation-II by Fluoroscopic Simulation: A Cadaveric Study
- Jin Hoon Jeong, Gu Hee Jung
- J Korean Fract Soc 2017;30(4):173-179. Published online October 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.4.173
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study seeks to determine the anatomically optimal entry point of proximal femoral nail antirotation-II (PFNA-II®) according to geographic features of Korean cadaveric femoral trochanters for successful reduction of osteoporotic proximal femoral fractures.
MATERIALS AND METHODS
Forty-three adult cadaveric femurs without previous fractures or surgeries were included. Anteroposterior (AP) and lateral images of all femurs and PFNA-II® were taken with an image intensifier. Using the image synthesis process via the image editing program (Adobe Photoshop CS6), the optimal entry point was verified and compared with the tip of the greater trochanter (GT) and the cervicotro-chanteric junction on AP images, as well as the width of the trochanter and the neck on lateral images.
RESULTS
The optimal entry point of PFNA-II® was an average distance of 9.1 mm (range, 7–15 mm) medially from the tip of GT on AP images. The center of the nail was located at an average of 30% (range, 21%–44%) area from the posterior margin of the middle neck, which is an average area of 38% (range, 26%–48%) from the posterior cortex of the trochanter on lateral images. Furthermore, the ideal entry point was at the extended line of the cervico-trochanteric junction.
CONCLUSION
The optimal entry point, which was found to be medial to the tip of the GT and posterior to the center of the middle femoral neck and the trochanter, was at on the extended line of the cervicotrochanteric junction. -
Citations
Citations to this article as recorded by- Clinical Research through Computational Anatomy and Virtual Fixation
Ju Yeong Kim, Dong-Geun Kang, Gu-Hee Jung
Journal of the Korean Orthopaedic Association.2023; 58(4): 299. CrossRef - Does the Entry Point of Proximal Femoral Nail Antirotation Affect the Malalignment of Intertrochanteric Fracture? A Cadaveric Study
Chittawee Jiamton, Nonpawit Nimmankiatkul, Pongsakorn Rungchamrassopa, Wichan Kanchanatawan, Pariyut Chiarapatanakom, Wirat Kongcharoensombat
Journal of Southeast Asian Orthopaedics.2022;[Epub] CrossRef
- Clinical Research through Computational Anatomy and Virtual Fixation
- 1,424 View
- 35 Download
- 2 Crossref

Case Reports
- Medial Plating of Distal Femoral Fracture with Locking Compression Plate-Proximal Lateral Tibia: Cases' Report
- Se Ang Jang, Young Soo Byun, In Ho Han, Dongju Shin
- J Korean Fract Soc 2016;29(3):206-212. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.206
-
 Abstract
Abstract
 PDF
PDF - Generally, lateral plating is used for a comminuted fracture of the distal femur. However, in some cases, it has been shown that using a medial plate is necessary to achieve better outcome. Nevertheless, there are no available anatomical plates that fit either the distal medial femoral condyle or fracture fixation, except for the relatively short plate developed for distal femoral osteotomy. We found that locking compression plate-proximal lateral tibia (LCP-PLT) fits anatomically well for the contour of the ipsilateral medial femoral condyle. Moreover, LCP-PLT has less risk of breaking the thread holes since it rarely needs to be bent. We report a plastic bone model study and two cases of distal femoral fractures fixed with medial plating using LCP-PLT.
-
Citations
Citations to this article as recorded by- A novel anatomical locked medial femoral condyle plate: a biomechanical study
M. A. Ozer, S. Keser, D. Barıs, O. Yazoglu
European Journal of Orthopaedic Surgery & Traumatology.2024; 34(5): 2767. CrossRef - Medial plating of distal femur: which pre-contoured angular stable plate fits best?
Shaam Achudan, Rex Premchand Antony Xavier, Sze Ern Tan
European Journal of Orthopaedic Surgery & Traumatology.2024; 34(6): 3297. CrossRef - Medial augmentation of distal femur fractures using the contralateral distal femur locking plate: A technical note
Jaime Andrés Leal
OTA International.2024;[Epub] CrossRef - The missing piece of the trauma armoury-medial femoral condyle plate
Piyush Upadhyay, Farhan Syed, Darryl N Ramoutar, Jayne Ward
Injury.2022; 53(3): 1237. CrossRef - Surgical Tips and Tricks for Distal Femur Plating
Christopher Lee, Dane Brodke, Ajay Gurbani
Journal of the American Academy of Orthopaedic Surgeons.2021; 29(18): 770. CrossRef - Medial minimally invasive helical plate osteosynthesis of the distal femur – a new technique
G.M. Hohenberger, A.M. Schwarz, P. Grechenig, B. Clement, Mario Staresinic, Bore Bakota
Injury.2021; 52: S27. CrossRef - Feature-Based Design of Personalized Anatomical Plates for the Treatment of Femoral Fractures
Xiaozhong Chen, Zhijian Mao, Xi Jiang
IEEE Access.2021; 9: 43824. CrossRef
- A novel anatomical locked medial femoral condyle plate: a biomechanical study
- 1,183 View
- 59 Download
- 7 Crossref

- Medial and Lateral Dual Plate Fixation for Osteoporotic Proximal Humerus Comminuted Fracture: 2 Case Reports
- Sam Guk Park
- J Korean Fract Soc 2016;29(1):61-67. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.61
-
 Abstract
Abstract
 PDF
PDF - Some proximal humeral fractures in elderly patients are accompanied by medial metaphyseal comminution and quality of the bone is so poor that head preserving osteosynthesis seems to be amenable. In cases of medial metaphyseal comminution, lateral locking compression plate (LCP) fixation also has a tendency to become a matter of screw cut out or loss of fixation. The author reports on successful treatment of two osteoporotic proximal humeral fractures combined with medial meta-physeal comminution, with application of additional direct medial supporting plate fixation. Medial plate fixations were added when the fractures were still unstable after the conventional lateral LCP fixation and anterior circumflex humeral arteries had been ruptured before. The fixations were stable enough to start exercise immediately after surgery. The inclinations of the humeral neck were not changed until the last follow-up and clinical results were satisfactory without humeral head osteonecrosis which was a concern.
-
Citations
Citations to this article as recorded by- Dual-Plate Fixation for Proximal Humerus Fractures With Unstable Medial Column in Patients With Osteoporosis
Hyun-Gyu Seok, Sam-Guk Park
Journal of Orthopaedic Trauma.2023; 37(10): e387. CrossRef - The plate fixation strategy of complex proximal humeral fractures
Qi Sun, Xiaoming Wu, Lei Wang, Ming Cai
International Orthopaedics.2020; 44(9): 1785. CrossRef - Biomechanical evaluation of a novel dualplate fixation method for proximal humeral fractures without medial support
Yu He, Yaoshen Zhang, Yan Wang, Dongsheng Zhou, Fu Wang
Journal of Orthopaedic Surgery and Research.2017;[Epub] CrossRef
- Dual-Plate Fixation for Proximal Humerus Fractures With Unstable Medial Column in Patients With Osteoporosis
- 573 View
- 6 Download
- 3 Crossref

- Breakage of Cephalomedullary Nail Used in the Treatment of Proximal Femur Fractures: Case Report
- Seok Hyun Kweon, Chang Hyun Shin, Jin Sung Park, Byoung San Choi
- J Korean Fract Soc 2016;29(1):42-49. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.42
-
 Abstract
Abstract
 PDF
PDF - Internal fixation using a cephalomedullary nail as treatment for proximal femur fracture has recently been popular for early ambulation and rehabilitation. However metal breakage at the lag screw insertion site was reported due to non-union, delayed-union, and early weight bearing. In our orthopedic department, we experienced 2 cases of nail breakage at the lag screw insertion site, therefore we report on evaluation of the cause of metal failure and prevention of complications with literature review.
-
Citations
Citations to this article as recorded by- Breakage of the Tail Portion of the Lag Screw during Removal of Proximal Femoral Zimmer Natural Nail: Report of Two Cases with Technical Notes
Asep Santoso, Ik-Sun Choi, Kyung-Soon Park, Taek-Rim Yoon
Hip & Pelvis.2017; 29(3): 199. CrossRef
- Breakage of the Tail Portion of the Lag Screw during Removal of Proximal Femoral Zimmer Natural Nail: Report of Two Cases with Technical Notes
- 578 View
- 2 Download
- 1 Crossref

- Irreducible Open Dorsal Dislocation of the Proximal Interphalangeal Joint: A Case Report
- Youn Tae Roh, Il Jung Park, Hyoung Min Kim, Jae Young Lee, Sung Lim You, Youn Soo Kim
- J Korean Fract Soc 2015;28(1):65-70. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.65
-
 Abstract
Abstract
 PDF
PDF - Dorsal dislocation of the proximal interphalangeal joint is a common injury in the orthopedic department. In most cases, the joint is reduced simply by closed manipulation. However, in rare cases, the joint is not reducible by closed manipulation, therefore, surgery is required. We report on a case of irreducible open dorsal dislocation of the proximal interphalangeal joint which was surgically treated. Because the flexor tendon interposed between the head of the proximal phalanx and the base of the middle phalanx, we could reduce the joint only after repositioning of the flexor tendon.
- 370 View
- 2 Download

- Rupture of the Extensor Pollicis Longus Tendon at the Proximal Screw of Volar Plate Fixation for Distal Radius Fracture: A Case Report
- Dong Ju Shin, Seung Oh Nam, Hun Sik Cho
- J Korean Fract Soc 2013;26(4):338-342. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.338
-
 Abstract
Abstract
 PDF
PDF - As volar plate fixation of distal radius fracture becomes more common, reports of ruptured extensor pollicis longus tendon by a protruding distal screw tip are also increasing steadily. Authors have experienced a rare case of ruptured extensor pollicis longus tendon at the prominent proximal screw of fixed volar plate for distal radius fracture, and we report it herein with a review of the literature.
- 439 View
- 1 Download

Original Articles
- Comparative Study of Proximal Femoral Nail Antirotation and Zimmer Natural Nail for the Treatment of Stable Intertrochanteric Fractures
- Jee Hoon Kim, Oog Jin Shon
- J Korean Fract Soc 2013;26(4):305-313. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.305
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the results between Proximal femoral nail antirotation II (PFNA II) and Zimmer natural nail Asia type (ZNN) for the treatment of stable intertrochanteric fractures.
MATERIALS AND METHODS
Between September 2011 and September 2012, 40 consecutive patients with stable intertrochanteric femoral fractures were treated with PFNA II or ZNN. We reviewed 20 cases of PFNA II and 20 cases of ZNN prospectively. We evaluated the operation time, amount of bleeding, mean hospital day, and capability of mobility and function using 'mobility score of Parker and Palmer' and 'social score of Jensen'. We also evaluated the reduction state by the Fogagnolo, Cleveland index, change of tip and apex distance (TAD), sliding distance of cervical screw, change of neck shaft angle and bone union time.
RESULTS
There were no significant differences between the groups treated with PFNA and ZNN. Both groups showed good clinical results. PFNA showed less TAD change and ZNN showed a shorter sliding distance of cervical screw, but they were not statistically different. The bone union time was approximately 13 weeks in both groups.
CONCLUSION
PFNA and ZNN produced good clinical and radiologic results in the treatment of stable intertrochanteric fractures. There were no significant differences between the groups. Both implants provide good stability and union, so we can conclude that they are both suitable for the treatment of stable intertrochanteric fractures. -
Citations
Citations to this article as recorded by- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef - Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef - Comparison of osteoporotic intertrochanteric fracture fixation using a proximal femoral nail with a helical blade and lag screw type proximal femoral nail
Woong Chae Na, Chae Won Lim, Sang Hong Lee
Medical Biological Science and Engineering.2018; 1(2): 45. CrossRef - BONE HEALING PATTERNS OF INTERLOCKED INTRAMEDULLARY NAIL-FIXATED FEMORAL SHAFT FRACTURES: AGE-MATCHED RADIOGRAPHIC PRESENTATION OF UNION PATTERN
Myung-Sang Moon, Dong-Hyeon Kim, Bong-Keun Park, Min-Geun Yoon
Journal of Musculoskeletal Research.2017; 20(02): 1750010. CrossRef - The Curative Effect Comparison Between Prolonged Third Generation of Gamma Nail and Prolonged Dynamic Hip Screw Internal Fixation in Treating Femoral Intertrochanteric Fracture and the Effect on Infection
Wenye He, Wei Zhang
Cell Biochemistry and Biophysics.2015; 71(2): 695. CrossRef
- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- 1,900 View
- 1 Download
- 5 Crossref

- The Result of Conservative Treatment of Proximal Humerus Fracture in Elderly Patients
- Seung Gil Baek, Chang Wug Oh, Young Soo Byun, Jong Keon Oh, Joon Woo Kim, Jong Pil Yoon, Hyun Joo Lee, Hyung Sub Kim
- J Korean Fract Soc 2013;26(4):292-298. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.292
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
With the increase in the old age population, proximal humerus fractures have been increasing recently. However, complications after operative treatment, such as fixation failure, are common because of osteoporosis. We treated proximal humerus fractures in patients with osteoporosis conservatively, and evaluated the radiographic and functional results by analyzing the factors affecting the results.
MATERIALS AND METHODS
Nineteen out of 30 cases for whom the clinical follow-up was over 1 year were included in this retrospective study. There were 17 females and 2 males, and the mean age was 73.2 years. The causes were slip from a short height (18 cases) and a minor car accident (1 case). We evaluated the union period, nonunion, malunion and the Constant score and analyzed several factors affecting the functional result, such as age, fracture pattern, and malunion.
RESULTS
Seventeen cases (89.5%) obtained union within 12.8 weeks on average. Neck-shaft angle was 125.3degrees on average, with seven cases of malunion. The Constant score was 84.1 on average, and there were excellent scores in 11 cases, good scores in 4 cases, and fair scores in 2 cases. Fracture pattern, neck-shaft angle, or malunion did not affect the functional outcome, and elderly patients showed poorer shoulder function.
CONCLUSION
Proximal humeral fractures with osteoporosis may achieve a high rate of bony union when treated with conservative methods. Despite the common occurrence of malunion, a satisfactory functional outcome may be expected.
- 614 View
- 6 Download

- The Treatment of Subtrochanteric Fractures with Proximal Femoral Nail Antirotation
- Chi Hyoung Pak, Sang Hong Lee, Sang Ho Ha, Gwang Chul Lee, Kyoung Chul Song
- J Korean Fract Soc 2013;26(4):284-291. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.284
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to analyze the results of treating subtrochanteric femoral fractures with proximal femoral nail antirotation (PFNA).
MATERIALS AND METHODS
Twenty five consecutive patients diagnosed with subtrochanteric femoral fractures underwent intramedullary fixation using PFNA and followed-up for over 12 months. According to the Seinsheimer's classification, there were 2 type IIA, 9 type IIB, 2 type IIIA, 3 type IV and 9 type V. According to the AO classification, there were 10 type A, 9 type B and 6 type C. There were 16 cases of closed reduction group and 9 cases of limited open reduction group. Retrospectively, radiological outcomes were assessed at the union period, change of neck shaft angle, tip-apex distance, Cleveland index, sliding of lag screw and complication.
RESULTS
Union was achieved in 23 of 25 cases, over an average of 17 weeks. Limb length shortening below 2 cm occurred in 7 patients. The Cleveland index was shown in 80% of 5, 6, 8 and 9 zone; the tip apex distance was 19.6 mm; the mean sliding distance was 4.4 mm; and the mean change of femur neck and shaft angle was varus 3 degree at the final follow-up. Complications included 3 cases of delayed union and 2 cases of nonunion.
CONCLUSION
With its early bony union, ambulation, rehabilitation and low complication, PFNA is a useful and reliable choice for the treatment of subtrochanteric fractures of the femur. Limited open reduction and additional fixation such as cable grip are recommended if it is difficult to obtain anatomical reduction by closed reduction. -
Citations
Citations to this article as recorded by- Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
Gyu Min Kong
Journal of the Korean Fracture Society.2019; 32(2): 107. CrossRef
- Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
- 927 View
- 6 Download
- 1 Crossref

Case Reports
- Insufficiency Fracture of Proximal Femur Shaft without Bisphosphonate Therapy: Report of Three Cases
- Suk Kyu Choo, Dae Yeon Jo, Hyoung Keun Oh
- J Korean Fract Soc 2013;26(3):217-220. Published online July 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.3.217
-
 Abstract
Abstract
 PDF
PDF - There is a growing interest in the factors related to insufficiency fractures. We are going to report three insufficiency fracture cases which are considered to be caused by osteoporosis, rheumatoid arthritis, steroid use and femoral shaft bowing among the patients not taking bisphosphonate. All cases are caused by low energy trauma and among these cases, one patient is being presented with a prodromal symptom and another patient complains of both prodromal symptoms and bilateral lesions.
- 290 View
- 0 Download

- Excessive Sliding of the Helical Blade and the Femoral Neck Fracture after Insertion of Proximal Femoral Nail Anti-Rotation for Type A2 Intertrochanteric Fractures - A Case Report -
- Bong Ju Park, Hong Man Cho, Ju Han Kim, Woo Jin Sin
- J Korean Fract Soc 2013;26(2):151-155. Published online April 30, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.2.151
-
 Abstract
Abstract
 PDF
PDF - Proximal femoral nail anti-rotation (PFNA) with a lag screw that is shaped like a spiral blade shape is an orthopedic implant to fix trochanteric fractures of the proximal femur. In addition the reason of the biomechanical advantages, PFNA widely been used recently. We report an 83-year-old man with excessive sliding of the helical blade and a femoral neck fracture after AO/OTA type A2 intertrochanteric fracture, which was fixed with a PFNA.
-
Citations
Citations to this article as recorded by- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture - A Case Report -
Soon Ho Huh, Hong-Man Cho, Ji-Yeon Park
Journal of the Korean Fracture Society.2021; 34(3): 112. CrossRef - Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
Se Jin Kim, Hong Man Cho, Jiyeon Park, Ki Yong An, Young Woo Chung, Woojin Shin
Journal of the Korean Fracture Society.2020; 33(4): 179. CrossRef - Failure of a Rotation Control Gamma 3 Lag Screw Used to Treat a Trochanteric Fracture
Kyungho Choi, Yongtae Kim, Shicheng Zhou, Jihyo Hwang
Hip & Pelvis.2018; 30(2): 129. CrossRef - Femoral neck fractures after internal fixation of trochanteric fractures with implants in situ in adults: A systematic review
Antonio Barquet, Peter V. Giannoudis, Andrés Gelink
Injury.2018; 49(12): 2121. CrossRef
- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture - A Case Report -
- 639 View
- 5 Download
- 4 Crossref

Original Articles
- Comparative Study of Intertrochanteric Fracture Treated with the Proximal Femoral Nail Anti-Rotation and the Third Generation of Gamma Nail
- Jae Cheon Sim, Tae Ho Kim, Ki Do Hong, Sung Sik Ha, Jong Seong Lee
- J Korean Fract Soc 2013;26(1):37-43. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.37
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the result between the third generation gamma nail (gamma 3 nail) and proximal femoral nail anti-rotation (PFNA) in the treatment of unstable intertrochanteric fractures.
MATERIALS AND METHODS
Between March 2009 and June 2011, 47 consecutive patients with unstable intertrochanteric femoral fractures were treated with gamma 3 nail or PFNA. We reviewed 24 cases of gamma 3 nail and 23 cases of PFNA. Retrospectively, we evaluated the mean operation time, amount of bleeding, average union period, reduction status, change of neck shaft angle, Tip-apex distance, Cleveland index, sliding of lag screw and complication on set of telephone interview and outpatient. We also evaluated the postoperative capability of function and mobility, using 'Modified Koval index'.
RESULTS
There were no significant differences between the groups, which were treated with gamma 3 nail and PFNA. In addition, they did not show statistical difference. We experienced 2 cases of complication (gamma 3 nail 1 case, PFNA 1 case), which were cut-out of the femoral head.
CONCLUSION
The gamma 3 nail and PFNA were seen with good results in the treatment of unstable intertrochanteric fracture. -
Citations
Citations to this article as recorded by- Comparative analysis of operation time and intraoperative fluoroscopy time in intramedullary and extramedullary fixation of trochanteric fractures
Milan Mitkovic, Sasa Milenkovic, Ivan Micic, Predrag Stojiljkovic, Igor Kostic, Milorad Mitkovic
Vojnosanitetski pregled.2022; 79(2): 177. CrossRef - Does the Helical Blade Lead to Higher Rates of Fixation Failure as Compared to Lag Screw in the Cephalomedullary Nailing Treatment of Hip Fractures? A Systematic Review and Meta-Analysis
Chul-Ho Kim, Han Soul Kim, Yong-Chan Kim, Dou Hyun Moon
Journal of Orthopaedic Trauma.2021; 35(8): 401. CrossRef - The Curative Effect Comparison Between Prolonged Third Generation of Gamma Nail and Prolonged Dynamic Hip Screw Internal Fixation in Treating Femoral Intertrochanteric Fracture and the Effect on Infection
Wenye He, Wei Zhang
Cell Biochemistry and Biophysics.2015; 71(2): 695. CrossRef - Accuracy of the Lesser Trochanter for Guiding Lag Screw Insertion in Hip Fracture Management
Jianlin Xiao, Zhongli Gao, Yanguo Qin, Xuezhou Li, Ao Wang, Lanyu Zhu, Jincheng Wang
Orthopedics.2014;[Epub] CrossRef
- Comparative analysis of operation time and intraoperative fluoroscopy time in intramedullary and extramedullary fixation of trochanteric fractures
- 1,292 View
- 5 Download
- 4 Crossref

- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
- Youn Soo Hwang, Kwang Yeol Kim, Hyung Chun Kim, Su Han Ahn, Dong Eun Lee
- J Korean Fract Soc 2013;26(1):14-20. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.14
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the effectiveness of optimal treatment of proximal humeral fractures and humeral shaft fractures in elderly patients with osteoporosis using the Polarus nail.
MATERIALS AND METHODS
Twenty-three patients with proximal humeral and humeral shaft fractures in elderly osteoporosis patients were treated using the Polarus intramedullary nail. Nine patients had proximal humeral fracture, 10 had humeral shaft fracture and 4 had the proximal humeral frac-ture extended diaphyseally. Radiological outcomes included the bone-union and the degree of re-sidual deformity. The residual deformities of the proximal humerus were assessed by the neck-shaft angle and the shaft angulation. Clinical outcome was assessed with the American Shoulder and Elbow Surgeons (ASES) score.
RESULTS
All cases had bony union and the mean union period was 16.5 weeks. The average neck/shaft alignment at the time of bone union was 135degrees and varus deformities of neck-shaft angle was not seen in all patients. Varus shaft angulation was seen in 5 patients. The mean ASES score after surgery was 86.7 points.
CONCLUSION
The Polarus intramedullary nail is effective for the treatment of proximal humeral and humeral shaft fractures in elderly patients with osteoporosis because it not only enables early postoperative mobilization, but also obtains bone-union without avascular necrosis and nonunion. -
Citations
Citations to this article as recorded by- Surgical Management of Osteoporotic Fractures: Humerus Shaft Fractures
Shankar Ramaprasad Kurpad
Indian Journal of Orthopaedics.2025; 59(8): 1053. CrossRef
- Surgical Management of Osteoporotic Fractures: Humerus Shaft Fractures
- 570 View
- 0 Download
- 1 Crossref

- Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
- Hyoung Keun Oh, Suk Kyu Choo, Jung Il Lee, Dong Hyun Seo
- J Korean Fract Soc 2012;25(4):305-309. Published online October 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.4.305
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Our study aimed to investigate the clinical and radiological results of humerus proximal or distal shaft fractures treated with minimally invasive plate osteosynthesis (MIPO) using a 3.5/5.0 metaphyseal locking plate.
MATERIALS AND METHODS
We reviewed the clinical and radiographic records of 17 patients with humeral proximal or distal shaft fractures who had undergone 3.5/5.0 metaphyseal locking plate osteosynthesis with a minimally invasive technique. We evaluated the results with respect to the anatomical reduction and union of the humerus shaft fracture through radiologic studies. We also evaluated the clinical results using the motion of shoulder and elbow functional outcome, American Shoulder and Elbow Surgeons (ASES) score, Mayo elbow performance score (MEPS), and postoperative complications.
RESULTS
Complete union was achieved in all cases. The mean union time was 14.2 weeks. According to the functional outcome rated by the ASES score and MEPS, 15 cases were considered excellent and 2 cases were good. There were no cases of surgically-related complications like metal failure, loss of anatomical reduction, or postoperative nerve injuries.
CONCLUSION
Using a 5.0 metaphyseal locking plate for humerus shaft fracture has the limitation that difficulties can arise in achieving sufficient screw fixation for small bony fragments. The 3.5/5.0 metaphyseal locking plate used in MIPO for humerus 1/3 proximal or distal shaft fractures was concluded to give good clinical and radiologic results. -
Citations
Citations to this article as recorded by- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
Youn-Soo Hwang, Kwang-Yeol Kim, Hyung-Chun Kim, Su-Han Ahn, Dong-Eun Lee
Journal of the Korean Fracture Society.2013; 26(1): 14. CrossRef
- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
- 625 View
- 1 Download
- 1 Crossref

- Clinical Outcome of Surgical Treatment for Fracture of the Femoral Shaft with Ipsilateral Fracture of the Proximal Femur
- Hee Gon Park, Jae Sung Yoo
- J Korean Fract Soc 2011;24(4):307-312. Published online October 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.4.307
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze diagnostic process and clinical data in cases of fracture of the femoral shaft with fracture of the proximal femur.
MATERIALS AND METHODS
We reviewed 24 cases of patient who undergone surgery for fracture of the femoral shaft with ipsilateral fracture of the proximal femur and more than 1 year of examination of follow up was available. Age, sex.location and classification of the fracture, the time of diagnosis and operation, the method of operation, the associated injuries, the time of bony union and complication were investigated, postoperative function was evaluated on Friedman and Wyman criteria.
RESULTS
Bony union showed significant difference in the displacement and comminution of fracture, postoperative function revealed significant difference according to the associated injuries. The 6 cases (25%) out of 24 cases are failed early diagnosis, 4 cases out of 6 cases was detected during operation and 2cases was found after surgery. 21 cases out of 24 cases of femoral shaft fractures showed union, 23 cases out of 24 cases of femoral neck fractures showed union. There were eleven good, eleven fair, and two poor functional result according to Friedman and Wyman criteria.
CONCLUSION
Precious clinical and radiologic examination is needed not to miss the diagnosis of proximal femur fractures in ipsilateral femoral shaft fractures with proximal femur fractures. Anatomical reduction and rigid fixation of proximal femur are important to reduce avascular necrosis of femoral head and nonunion of proximal femoral fractures.
- 313 View
- 2 Download

- Intramedullary Nailing for Complex Fractures of the Proximal and Midshaft of the Humerus
- Chul Hyun Cho, Gu Hee Jung, Kyo Wook Kim
- J Korean Fract Soc 2011;24(3):237-242. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.237
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the results of antegrade interlocking intramedullary nailing for complex fractures of the proximal and midshaft of the humerus.
MATERIALS AND METHODS
We retrospectively analyzed the clinical and radiologic results in 11 cases, which were treated by antegrade interlocking intramedullary nail. We assessed clinical outcomes according to ASES scoring system and radiological result.
RESULTS
All cases had bony union and the mean union period was 14.7 weeks. Postoperative complications were 1 loss of fixation, 2 proximal protrusion of nail and 2 temporary shoulder pain. A case with loss of fixation was treated open reduction and refixation and had union at 14 weeks postoperatively. The mean ASES score was 85.9 and the clinical outcomes were 4 excellent, 5 good, 1 fair and 1 poor.
CONCLUSION
Intramedullary nailing for complex fractures of the proximal and midshaft of the humerus can offer a reliable treatment option.
- 299 View
- 0 Download

- Treatment of the Intertrochanteric Femoral Fracture with Proximal Femoral Nail: Nailing Using the Provisional K-wire Fixation
- Gu Hee Jung
- J Korean Fract Soc 2011;24(3):223-229. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.223
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the efficiency of provisional K-wire fixation in intertrochanteric fractures treated with proximal femoral nail (PFN).
MATERIALS AND METHODS
Twenty seven patients (by AO/OTA classification, A1 8 cases, A2 19 cases) were treated with PFN with percutaneous reduction and provisional K-wire fixation, and followed a mean 24.5 months. The adequacy of fracture reduction was assessed by Fogagnolo's classification and reestablishment of bone-to-bone contact with the medial anatomy. Functional results were evaluated by postoperative complications, Jensen's method and Harris hip score (HHS).
RESULTS
In all cases, the bone-to-bone contact with the medial anatomy was reestablished by percutaneous reduction and examination of Fogagnolo's classification showed a good reduction. The technical complications and error of starting point were not occurred. The mean HHS was 76.5 and means Jensen's grade was 2.1 grades. Complications included excessive sliding in 1 case and early cutting-out of screw in 1 case.
CONCLUSION
The provisional K-wire fixation in trochanteric fracture treated with PFN had an advantage in preventing technical complications because it facilitates a nail insertion in ideal position. -
Citations
Citations to this article as recorded by- Analysis of Low-Energy Trochanter Fracture Using the Multiplanar Computed Tomography Image: Application for Intramedullary Nail Fixation
Gu-Hee Jung, Sung-Keun Heo, Hyun-Je Seo
Journal of the Korean Fracture Society.2015; 28(3): 155. CrossRef - Morbidity and Mortality of the Elderly after Early Operation for Trochanteric Fractures
Se-Ang Jang, Young-Ho Cho, Young-Soo Byun, Ki-Hong Park, Hyun-Seong Yoo, Chul Jung
Journal of the Korean Fracture Society.2013; 26(3): 199. CrossRef
- Analysis of Low-Energy Trochanter Fracture Using the Multiplanar Computed Tomography Image: Application for Intramedullary Nail Fixation
- 676 View
- 1 Download
- 2 Crossref

- The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
- Jeoung Ho Kim, Sang Hong Lee, Kwang Chul Lee, Sung Won Cho
- J Korean Fract Soc 2011;24(3):217-222. Published online July 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.3.217
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to analyze the results of intertrochanteric fractures treatment with proximal femoral nail antirotation (PFNA) without using fracture tables and thereby prevent complications.
MATERIALS AND METHODS
Forty cases of intertrochanteric fracture of 39 patients that were treated with PFNA without using fracture tables between January 2008 to December 2009 were analyzed. There were 13 males and 27 females. The mean age was 76 years old. Using AO classification, 6 cases were A1, 25 cases were A2 and 9 cases were A3. The operation was done without using fracture tables at supine position. Operation time, intraoperative bleeding were checked. For the result, Cleveland index, tip apex distance, fracture site sliding rate, change of femur neck and shaft angle were evaluated. Bone union time and complications were also estimated from the follow up radiograph. Statistics were analyzed using Independent T-test.
RESULTS
The mean operation time was 40 minutes (25 to 70 minutes) and mean intraoperative bleeding was 113 cc (40 to 250 cc). The Cleveland index was shown 94% of 5, 6, 8 and 9 zone, the tip apex distance was 12.96 mm (6 to 22 mm), the fracture sliding distance was 1.9 mm (0 to 6 mm), the change of femur neck and shaft angle was 2.5 degree (0~10 degree) and the average bone union time was 15 weeks (8 to 24 weeks). The complication include 2 cases of delayed union and 2 cases of varus deformities.
CONCLUSION
We have shortened the operation time by closed reduction methods without using the fracture tables, and the complication were minimized with using simple tools like a reduction forcep or bone hook at PFNA blade insertion. -
Citations
Citations to this article as recorded by- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef - The Treatment of Subtrochanteric Fractures with Proximal Femoral Nail Antirotation
Chi Hyoung Pak, Sang Hong Lee, Sang Ho Ha, Gwang Chul Lee, Kyoung Chul Song
Journal of the Korean Fracture Society.2013; 26(4): 284. CrossRef
- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- 652 View
- 1 Download
- 2 Crossref

Case Report
- Periprosthetic Fracture after Proximal Humeral Intramedullary Nail, Treated by Functional Bracing: A Case Report
- Jae Hyuk Shin, Ho Guen Chang, Young Woo Kim, Nam Kyou Rhee, Yong Bok Park, Yong Kuk Kim
- J Korean Fract Soc 2011;24(2):185-190. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.185
-
 Abstract
Abstract
 PDF
PDF - Periprosthetic fracture following a proximal humeral intramedullary (IM) nailing is rarely reported neither for its occurrence nor for its treatment. Proximal humeral IM nail (Acumed, LLC, Hillsboro, OR, USA) has been increasingly reported of its successful treatment outcomes, yet there is paucity of data describing its complications. Here we report a 26 year-old female patient, who sustained a proximal humerus fracture which was initially successfully treated by proximal humeral IM nail, and was complicated by a periprosthetic fracture distal to the nail tip at postoperative 4 months. Serial application of U-shaped coaptation splint, hanging cast, and functional bracing resulted in satisfactory clinical outcome. Periprosthetic fracture after proximal humerus IM nail can occur by a low energy injury, which need to reminded in treating young and sports-active patients.
-
Citations
Citations to this article as recorded by- Locking compression plate fixation of periprosthetic distant humeral fracture after intramedullary nail for humeral shaft fracture: A case report
Mei-Ren Zhang, Kui Zhao, Jiang-Long Guo, Hai-Yun Chen
Trauma Case Reports.2022; 37: 100565. CrossRef - Distal Humeral Fixation of an Intramedullary Nail Periprosthetic Fracture
Hiren M. Divecha, Hans A. J. Marynissen, K. Erler, D. A. Fisher, J. Mayr, A. Sakamoto
Case Reports in Orthopedics.2013;[Epub] CrossRef
- Locking compression plate fixation of periprosthetic distant humeral fracture after intramedullary nail for humeral shaft fracture: A case report
- 635 View
- 3 Download
- 2 Crossref

Original Article
- Comparison of Results between Internal Plate Fixation and Hemiarthroplasty in Comminuted Proximal Humerus Fracture
- Doo Sup Kim, Dong Kyu Lee, Chang Ho Yi, Jang Hee Park, Jung Ho Rah
- J Korean Fract Soc 2011;24(2):144-150. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.144
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Authors compare clinical and radiological results of internal fixation group and hemiarthroplasty group for comminuted proximal humerus fracture to find out which the treatment method have to be chose for comminuted proximal humerus fractures.
MATERIALS AND METHODS
Patients who were treated from March 2005 to March 2007 and available for 2 years follow-up were targets of this study. The internal fixation group had 38 cases, and hemiarthroplasty group included 26 cases. The results were analyzed both clinically and radiologically.
RESULTS
On average, Bone union took 15.6 weeks in the internal fixation group. Constant score between the internal fixation and hemiarthroplasty groups were on average 75+/-6.5 points and 70+/-7.4 points (p=0.034). In 3-part fracture, Constant score between both groups were 78+/-5.4 points from the former and 71+/-2 points, respectively (p=0.028). In 4-part fracture group, Constant score were 72+/-8 points for the internal fixation group and 69+/-9.2 points for the hemiarthroplasty group (p=0.041).
CONCLUSION
Internal plate fixation can gain better outcome than hemiarthroplasty in 4-part fracture as well as 3-part fracture of proximal humerus by careful dissection for preservation of blood supply for humeral head and optimal reduction. -
Citations
Citations to this article as recorded by- Surgical treatment of proximal humerus fractures: a systematic review and meta-analysis
Erik Hohmann, Natalie Keough, Vaida Glatt, Kevin Tetsworth
European Journal of Orthopaedic Surgery & Traumatology.2022; 33(6): 2215. CrossRef - Effectiveness and Safety of Interventions for Treating Adults with Displaced Proximal Humeral Fracture: A Network Meta-Analysis and Systematic Review
Long Chen, Fei Xing, Zhou Xiang, Ara Nazarian
PLOS ONE.2016; 11(11): e0166801. CrossRef - Meta-analysis comparing locking plate fixation with hemiarthroplasty for complex proximal humeral fractures
Jiezhi Dai, Yimin Chai, Chunyang Wang, Gen Wen
European Journal of Orthopaedic Surgery & Traumatology.2014; 24(3): 305. CrossRef
- Surgical treatment of proximal humerus fractures: a systematic review and meta-analysis
- 833 View
- 2 Download
- 3 Crossref

Case Reports
- Conservative Treatment of Valgus Impacted Four-Part Fracture of the Proximal Humerus: A Case Report
- Moon Chan Kim, Jae Lim Cho, Hung Tae Chung, Dong Jun Kim, In Bo Kim
- J Korean Fract Soc 2011;24(1):96-99. Published online January 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.1.96
-
 Abstract
Abstract
 PDF
PDF - For valgus impacted four part fracture of the proximal humerus, surgical stabilization and early mobilization of the joint can produce the best clinical outcomes. But, we have experienced a case of conservative treatment and gained good clinical results. We have reported this case and included a review of the relevant literatures.
- 561 View
- 5 Download

- Simultaneous Fractures of the Ipsilateral Distal and Proximal Clavicle: Double Clavicle Fracture: A Case Report
- Kyoung Jun Park, Hoon Sang Sohn, Kyoung Young Baek
- J Korean Fract Soc 2011;24(1):92-95. Published online January 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.1.92
-
 Abstract
Abstract
 PDF
PDF - Clavicular fracture is common injury in the upper extremity, but ipsilateral proximal, distal or middle-third clavicular fractures which occur simultaneously are an extremely rare. Seven cases have been reported in the English and Japanese literatures, but it has never been reported in Korea. We report a case of ipsilateral proximal and distal clavicular fracture caused by fall from height and describe its presumed mechanism, diagnosis, treatment with a review of literatures.
- 530 View
- 2 Download

Original Articles
- Minimally Invasive Plate Osteosynthesis for Proximal Tibial Shaft Fracture
- Young Soo Byun, Ki Chul Park, Hyun Jong Bong, Chang Hoon Lee
- J Korean Fract Soc 2011;24(1):23-27. Published online January 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.1.23
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To report the results of patients treated by minimally invasive plate osteosynthesis (MIPO) for proximal tibial shaft fractures.
MATERIALS AND METHODS
From September 2003 to June 2008, thirty-two patients with proximal tibial shaft fractures weretreated by MIPO. There were 22 men and 10 women and mean age was 43.8 years (range; 21~72 years). Follow-up was available for all patients and the mean follow-up period was 19.5 months (range; 12~40 months). Duration of union, range of knee motion and postoperative complications were evaluated.
RESULTS
Twenty-nine patients (90.6%) healed after the MIPO technique. The mean duration of radiographic union was 18.3 weeks (range; 10~28 weeks). The mean range of knee motion was 134 degrees at the last follow-up. There were 1 non-union, 2 delayed unions, 1 superficial infection, 1 deep infection, 2 malunions with more than 5 degrees of malalignment and 14 cases of skin irritation by plate.
CONCLUSION
MIPO is an effective treatment for closed, proximal tibialshaft fractures. More aggressive treatment such as dual plating should be considered in fractures with severe comminution or bone loss. -
Citations
Citations to this article as recorded by- Medial Minimally Invasive Percutaneous Plate Osteosynthesis in Proximal Tibial Comminuted Fractures
Jae-Ang Sim, Kwang-Hui Kim, Yong-Seuk Lee, Sang-Jin Lee, Beom-Koo Lee
Journal of the Korean Orthopaedic Association.2014; 49(4): 278. CrossRef - Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures - Technical Note -
Jae Ang Sim, Beom Koo Lee, Kwang Hui Kim, Yong Seuk Lee
Journal of the Korean Fracture Society.2013; 26(4): 327. CrossRef
- Medial Minimally Invasive Percutaneous Plate Osteosynthesis in Proximal Tibial Comminuted Fractures
- 692 View
- 10 Download
- 2 Crossref

- Comparison of the Compression Hip Screw (CHS) and the Proximal Femoral Nail Antirotation (PFNA) for Intertrochanteric Femoral Fracture
- Jong Min Lim, Jeung Il Kim, Jong Seok Oh, Kuen Tak Suh, Jae Min Ahn, Dong Joon Kang
- J Korean Fract Soc 2010;23(4):360-366. Published online October 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.4.360
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the radiologic, clinical results between who had intertrochanteric fracture, treated with Compression Hip Screw (CHS) and Proximal Femoral Nail Antirotation (PFNA).
MATERIALS AND METHODS
We retrospectively reviewed each 36 and 48 patients of intertrochanteric fracture which were treated with CHS or PFNA by one surgeon from January 2005 to June 2009. We evaluated mean operation time, amount of bleeding, radiologic results, and the clinical outcomes with the mobility score of Parker and Palmer, social function scoring system.
RESULTS
The mean operation time, amount of bleeding were less in the PFNA group, there were 116.7 min, 486.1 ml for the CHS group versus 87.7 min, 289.6 ml for the PFNA group. The radiologic results were not significantly different. Decrease of mobility score of Parker and Palmer, social function score were similar. Proximal migration of leg screw and perforation of femoral head was 2 case and deep infection was 1 cases in CHS group.
CONCLUSION
There were no significant differences that are clinical and radiological results in treatment of intertrochanteric fracture using the CHS and PFNA. But PFNA is less invasive device than CHS, therefore it may be useful device in elderly patients. -
Citations
Citations to this article as recorded by- Chronic kidney disease patients with intertrochanteric fracture have a high mortality rate
Tae Woo Kim, Sang-Min Lee, Nam Hoon Moon, Won Chul Shin
Injury.2021; 52(8): 2350. CrossRef - Comparison between the Results of Internal Fixation Using Proximal Femur Nail Anti-rotation and Bipolar Hemiarthroplasty in Treatment of Unstable Intertrochanteric Fractures of Elderly Patients
Sung-Hwan Kim, Soo-Won Lee, Gyu-Min Kong, Mid-Um JeaGal
Hip & Pelvis.2012; 24(1): 45. CrossRef - Treatment of Intertrochanteric Fractures Using Targon Proximal Femoral Nails
Il Ho Park, Jong Kyoung Won, Kye Young Han
Hip & Pelvis.2012; 24(2): 117. CrossRef - A Comparison of Intramedullary and Extramedullary Fixations for the Treatment of Reverse Oblique or Transverse Intertrochanteric Femoral Fractures
Yerl-Bo Sung, Jung-Yun Choi, Eui-Yub Jung
Hip & Pelvis.2012; 24(2): 109. CrossRef
- Chronic kidney disease patients with intertrochanteric fracture have a high mortality rate
- 1,898 View
- 4 Download
- 4 Crossref

- Treatment of the Unstable Intertrochanteric Fracture with Proximal Femoral Nail Antirotation: Comparison with Compression Hip Screw with Trochanteric Stabilizing Plate
- Tae Ho Kim, Jong Oh Kim, Seung Yup Lee, Geon Ung Yun
- J Korean Fract Soc 2010;23(4):353-359. Published online October 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.4.353
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the effectiveness of Proximal Femoral Nail Anti-rotation (PFNA) for the treatment of unstable intertrochanteric fracture comparing with Compression Hip Screw (CHS) with Trochanteric Stabilizing Plate (TSP).
MATERIALS AND METHODS
With clinical study, 43 patients who were treated surgically for unstable intertrochanteric fractures were retrospectively evaluated. One group was treated with CHS and TSP (Group 1, 22 cases) and the other was treated with PFNA (Group 2, 21 cases). By postoperative radiograph and last follow up radiograph we measured Tip-apex distance, Cleveland index, Lag screw slippage, Neck-shaft angle change and Union time. And By retrospective medical record review, the clinical results were evaluated with the operation time, intraoperative estimated blood loss, amount of drainage, amount of transfusion, walking ability change and complication.
RESULTS
There was a lower operation time, intraoperative estimated blood loss, amount of drainage, amount of transfusion, lag screw slippage and neck shaft angle change in the Group 2 than in the Group 1 (p<0.05).
CONCLUSION
PFNA showed better results than CHS with TSP in operation time, estimated blood loss, amount of drainage and transfusion, lag screw slippage and neck-shaft angle change. -
Citations
Citations to this article as recorded by- Results of Asian Type Gamma 3 Nail in Treatment of Trochanteric Fractures
Bing Zhe Huang, Yong Wook Park, Jin Su Park, Kyu Cheol Noh, Soung Yon Kim, Kook Jin Chung, Hong Kyun Kim, Hyong Nyun Kim, Yong Hyun Yoon, Ji Hyo Hwang
Journal of the Korean Fracture Society.2014; 27(3): 213. CrossRef - Comparative Study of Intertrochanteric Fracture Treated with the Proximal Femoral Nail Anti-Rotation and the Third Generation of Gamma Nail
Jae-Cheon Sim, Tae-Ho Kim, Ki-Do Hong, Sung-Sik Ha, Jong-Seong Lee
Journal of the Korean Fracture Society.2013; 26(1): 37. CrossRef - Comparative Study of Proximal Femoral Nail Antirotation and Zimmer Natural Nail for the Treatment of Stable Intertrochanteric Fractures
Jee-Hoon Kim, Oog-Jin Shon
Journal of the Korean Fracture Society.2013; 26(4): 305. CrossRef - A Comparison between Compression Hip Screw and Intramedullary Nail for the Treatment of AO/OTA A2.2 Intertrochanteric Femoral Fracture
Phil Hyun Chung, Suk Kang, Jong Pil Kim, Young Sung Kim, Ho Min Lee, Jong Hyun Kim
Journal of the Korean Fracture Society.2013; 26(1): 44. CrossRef - The Treatment of Intertrochanteric Femoral Fracture with Proximal Femoral Nail Antirotation
Jong Won Kim, Hyun Soo Park, Young Soo Jang, Jae Hyuk Choi, Sung Ju Bae, Chan Il Bae
Journal of the Korean Fracture Society.2012; 25(4): 257. CrossRef - Operative Treatment with Gamma 3 Nail in Femur Intertrochanteric Fracture
Ki-Do Hong, Jae-Chun Sim, Sung-Sik Ha, Tae-Ho Kim, Yoon-Ho Choi, Jong-Hyun Kim
Journal of the Korean Fracture Society.2011; 24(1): 7. CrossRef
- Results of Asian Type Gamma 3 Nail in Treatment of Trochanteric Fractures
- 795 View
- 2 Download
- 6 Crossref

Case Report
- Osteochondral Autograft Using Head of Proximal Phalanx of Toe for Partial Osteochondral Defect of Proximal Interphalangeal Joint: A Case Report
- Tong Joo Lee, Kyung Ho Moon, Yoon Sang Jeon, Do Seung Kwon
- J Korean Fract Soc 2010;23(3):321-325. Published online July 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.3.321
-
 Abstract
Abstract
 PDF
PDF - Osteochondral injury due to the trauma of the hand is relatively common. If the size of the osteochondral fracture fragment is large, open reduction and internal fixation are often feasible in treating these problems. However, arthroplasty using osteochondral graft is more preferred when the particle is small and articular surface is comminuted or fully defected. There are many reports of osteochondral graft using the costal osteochondral graft but the osteochondral graft using the interphalangeal joint of the toe is rarely reported. Thoroughly reviewed with relevant articles, this report presents a case of a 33 year old male who was successfully treated with osteochondral autograft using the proximal interphalangeal joint of the toe due to the traumatic osteochondral defect in the head of the second proximal phalanx.
- 310 View
- 3 Download

Original Articles
- Comparison of Bone Mineral Density in Elderly Patients over 65 Years according to Presence and Types of Hip Fracture
- Myung Ho Kim, Moon Jib Yoo, Joong Bae Seo, Hyun Yul Yoo, Sang Young Moon
- J Korean Fract Soc 2010;23(3):263-269. Published online July 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.3.263
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We measured the BMD of elderly patients with osteoporotic hip fracture in order to understand the relationship between BMD of each sites and hip fracture occurrence or the types, and also to suggest a reference point for starting an osteoporosis treatment program.
MATERIALS AND METHODS
From July 2007 to February 2010, we investigated total 147 elderly osteoporotic hip fracture patients over 65 years. For control group, 80 patients who were over 65-year-old and did not have any fracture were selected. BMD was compared at each site between each groups statistically.
RESULTS
In the comparison of femur intertrochanter and neck fracture groups, BMD of femur neck and trochanter areas and L2, L3 areas were significantly less in intertrochanteric fracture group. In the analysis according to the classification of intertrochanteric fracture, BMD of intertrochanter and Ward's triangle area were significantly less in unstable fracture group than stable one. Each of the fracture threshold of intertrochanteric and neck fracture group was -1.10 and -1.36 of the T-score in proximal femur, and -1.40 and -1.40 of the T-score in lumbar vertebrae.
CONCLUSION
To examine the BMD of both proximal femur and lumbar vertebrae areas is helpful to predict the hip fracture occurrence and the type of hip fracture. And for the prevention of hip fracture in elderly patients over 65 years, we propose that the aggressive treatment of osteoporosis should be started to prevent fracture for patients with a T-score less than -1.40. -
Citations
Citations to this article as recorded by- Risk factors affecting hip fracture patterns in an elderly Korean patient population
Sug Hun Che, Myung-Rae Cho, Patrick Michael Quinn, Suk-Kyoon Song
Medicine.2023; 102(33): e34573. CrossRef - Does Fracture Severity of Intertrochanteric Fracture in Elderly Caused by Low-Energy Trauma Affected by Gluteus Muscle Volume?
Byung-Kook Kim, Suk Han Jung, Donghun Han
Hip & Pelvis.2022; 34(1): 18. CrossRef
- Risk factors affecting hip fracture patterns in an elderly Korean patient population
- 540 View
- 0 Download
- 2 Crossref

- Proximal Femoral Nail Antirotation versus Compression Hip Screw with Trochanter Stabilizing Plate for Unstable Intertrochanteric Hip Fractures
- Jae Young Rho, Sang Bum Kim, Youn Moo Heo, Seong Jin Cho, Dong Sik Chae, Woo Suk Lee
- J Korean Fract Soc 2010;23(2):161-166. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.161
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze and compare the clinical and radiologic results of treatments in unstable intertrochanteric fractures of the femur with proximal femoral nail antirotation (PFNA) and compression hip screw with trochanter stabilizing plate (CHS with TSP).
MATERIALS AND METHODS
We retrospectively reviewed the results of 66 cases of unstable intertrochanteric fractures of the femur treated with PFNA (Group I) and CHS with TSP (Group II) which could be followed up for minimum a year. We evaluated several comparative factors such as operation time, blood loss, time to bone union, changes in neck-shaft angle, sliding of screw (or blade), complications, postoperative pain, social-function score of Jensen, and mobility score of Parker and Palmer.
RESULTS
Group I showed shorter operation time and less blood loss with significance than group II (p<0.05), but there were no differences between the groups in the mean time to bone union, changes in neck-shaft angle, sliding of screw (or blade), complications, postoperative pain, and social-function score of Jensen (p>0.05). Two cases of cutting out of the blade through the femoral head were found in group I. One case of cutting out of the screw, one case of the breakage of the plate, and loosening of the plate were found in group II as complications.
CONCLUSION
We think that there were no significant differences between PFNA and CHS with TSP in view point of radiologic and clinical outcomes in unstable intertrochanteric fractures of the femur, but PFNA is less invasive device than CHS with TSP, therefore it may be useful device in elderly patients. -
Citations
Citations to this article as recorded by- Results of Use of Compression Hip Screw with Trochanter Stabilizing Plate for Reverse Oblique Intertrochanteric Fracture
Byung-Woo Min, Kyung-Jae Lee, Gyo-Wook Kim, Ki-Cheor Bae, Si-Wook Lee, Du-Han Kim
Journal of the Korean Fracture Society.2014; 27(2): 120. CrossRef - Effectiveness of the Valgus Reduction Technique in Treatment of Intertrochanteric Fractures Using Proximal Femoral Nail Antirotation
Ji-Kang Park, Hyun-Chul Shon, Yong-Min Kim, Eui-Sung Choi, Dong-Soo Kim, Kyoung-Jin Park, Byung-Ki Cho, Jung-Kwon Cha, Sang-Woo Kang
Journal of the Korean Orthopaedic Association.2013; 48(6): 441. CrossRef - A Comparison of Intramedullary and Extramedullary Fixations for the Treatment of Reverse Oblique or Transverse Intertrochanteric Femoral Fractures
Yerl-Bo Sung, Jung-Yun Choi, Eui-Yub Jung
Hip & Pelvis.2012; 24(2): 109. CrossRef
- Results of Use of Compression Hip Screw with Trochanter Stabilizing Plate for Reverse Oblique Intertrochanteric Fracture
- 757 View
- 1 Download
- 3 Crossref

- Helical Blade versus Lag Screw for Treatment of Intertrochanteric Fracture
- Kwang Jun Oh, Sung Tae Lee, Suk Ha Lee, Jin Ho Hwang, Min Suk Kang
- J Korean Fract Soc 2010;23(1):6-12. Published online January 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.1.6
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the radiographic and functional outcomes between who had unstable intertrochanteric fracture, treated with the ITST (lag screw design) and the PFNA (helical blade design).
MATERIALS AND METHODS
We selected each 17 and 13 patients of unstable intertrochanteric fracture which were treated with ITST or PFNA from April 2005 to December 2008. We evaluated the radiographic results by follow-up radiography and the clinical outcomes with the mobility score of Parker and Palmer, Social function scoring system.
RESULTS
The mean sliding distance of cervical screw with ITST nails was not shown significant differences than with using PFNA nails. The other factors were not statistically different. Decrease of mobility score of Parker and Palmer, Social function score were similar. 2 cases of cutting out was noted with ITST nails and 1 case of cutting out was noted with PFNA nails.
CONCLUSION
Unlike the existed biomechanical reposts, there are no differences that are clinical and radiological results in treatment of unstable intertrochanteric fracture using the ITST nails and PFNA nails. -
Citations
Citations to this article as recorded by- Does the Helical Blade Lead to Higher Rates of Fixation Failure as Compared to Lag Screw in the Cephalomedullary Nailing Treatment of Hip Fractures? A Systematic Review and Meta-Analysis
Chul-Ho Kim, Han Soul Kim, Yong-Chan Kim, Dou Hyun Moon
Journal of Orthopaedic Trauma.2021; 35(8): 401. CrossRef - Comparative Study of Intertrochanteric Fracture Treated with the Proximal Femoral Nail Anti-Rotation and the Third Generation of Gamma Nail
Jae-Cheon Sim, Tae-Ho Kim, Ki-Do Hong, Sung-Sik Ha, Jong-Seong Lee
Journal of the Korean Fracture Society.2013; 26(1): 37. CrossRef - Treatment of Intertrochanteric Fractures Using Targon Proximal Femoral Nails
Il Ho Park, Jong Kyoung Won, Kye Young Han
Hip & Pelvis.2012; 24(2): 117. CrossRef
- Does the Helical Blade Lead to Higher Rates of Fixation Failure as Compared to Lag Screw in the Cephalomedullary Nailing Treatment of Hip Fractures? A Systematic Review and Meta-Analysis
- 1,046 View
- 9 Download
- 3 Crossref

- Treatment of Proximal Tibia Fractures Using LCP by MIPO Technique
- Sang Ho Ha, Dong Hui Kim, Jun Young Lee
- J Korean Fract Soc 2010;23(1):34-41. Published online January 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.1.34
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We wanted to evaluate the efficacy of MIPO (minimal invasive plate osteosynthesis) technique by LCP (locking compression plate) for treating proximal tibia fractures.
MATERIALS AND METHODS
Twenty-three patients, who had operation due to proximal tibia fracture and available for follow up for more than 1 year were included in this study. Cause of injury and accompanied injuries were checked. Operation time, period to bone union, range of joint motion and alignment were evaluated with complications.
RESULTS
Mean bone union time was 13.7 weeks (10~20). Twenty-one cases of the patients showed angulation of less than 5 degrees and 17 cases had normal range of motion. Five cases showed skin irritation by the plate and 2 cases had superficial infection.
CONCLUSION
LCP by MIPO technique for treating proximal tibia fracture showed excellent results. Delicate technique is required for the proper adjustment of LCP and the alignment of the lower leg. -
Citations
Citations to this article as recorded by- EVALUATION OF FUNCTIONAL OUTCOME OF SURGICAL TREATMENT FOR FRACTURE AROUND KNEE WITH LOCKING PLATE
VIKAS KUNTWAD, AMOL WAGH, SATYAJEET A HORE
Asian Journal of Pharmaceutical and Clinical Research.2023; : 213. CrossRef - Medial Minimally Invasive Percutaneous Plate Osteosynthesis in Proximal Tibial Comminuted Fractures
Jae-Ang Sim, Kwang-Hui Kim, Yong-Seuk Lee, Sang-Jin Lee, Beom-Koo Lee
Journal of the Korean Orthopaedic Association.2014; 49(4): 278. CrossRef - Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures - Technical Note -
Jae Ang Sim, Beom Koo Lee, Kwang Hui Kim, Yong Seuk Lee
Journal of the Korean Fracture Society.2013; 26(4): 327. CrossRef
- EVALUATION OF FUNCTIONAL OUTCOME OF SURGICAL TREATMENT FOR FRACTURE AROUND KNEE WITH LOCKING PLATE
- 774 View
- 9 Download
- 3 Crossref

- Limited Open Reduction and Intramedullary Nailing of Proximal Femoral Shaft Fracture
- Sang Ho Ha, Jun Young Lee, Sang Hong Lee, Sung Hwan Jo, Jae Cheul Yu
- J Korean Fract Soc 2009;22(4):225-231. Published online October 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.4.225
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the result of treatment of proximal femoral shaft fracture with limited open reduction and intramedullary nailing. MATERIALS AND METHODS: Fifteen patients who had limited open reduction and intramedullary nailing due to proximal femoral shaft fracture for follow-up for more than 12 months were selected between March 2001 and December 2005. The clinical and radiologic results were analyzed. Winquist-Hansen classification and OTA/AO classification were used. RESULTS: Thirteen cases achieved bone union and 2 cases showed delayed union. The mean bone union period was 21.3 weeks (14~32). There was no postoperative infection. Nonunion was observed in 2 cases of which bone union was acquired with the exchange of intramedullary nail and bone graft in one case and with the additional plate fixation and bone graft in the other case. CONCLUSION: Treating proximal femoral shaft fracture with limited open reduction and intramedullary nailing seems to be a technique to manage proximal femoral shaft fracture that has combined fracture or ipsilateral femoral fracture or is unable to acquire acceptable reduction with closed reduction.
- 617 View
- 2 Download

- Staged Management of High Energy Proximal Tibia Fractures with Severe Soft Tissue Damage
- Seung Ryul Lee, Jae Hoon Yang, June Kyu Lee, Hyun Dae Shin, Kyung Cheon Kim, Kyu Woong Yeon, Young Mo Kim
- J Korean Fract Soc 2009;22(3):152-158. Published online July 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.3.152
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To find out the efficiency of two staged operation of patients with high energy proximal tibia fracture with severe soft tissue damage, the first step being external fixation, and the second, internal fixation with plates.
MATERIALS AND METHODS
The study group was the 42 patients who had followed for one year out of a group of 56, performed the first step external fixation and the second step internal fixation with plates retrospectively, from March 2003 to March 2007. The average age of the study group was 51.4, 26 men, and 16 women participating in this study. The average time of follow up was 32 months. In the final follow up, investigations of the radiological assessments and functional abilities of the bony fusion were carried out along with the complications of the soft tissue.
RESULTS
The duration after the first step external fixation until second step internal fixation to be performed was 14.9 (6~40) days in average. The final bone fusion took about 15 weeks, and according to the final follow up, the range of motion of the knee was around 110.8 degrees (6.2~117 degrees). In 31 cases, only the internal fixation was performed, while in 11 cases, soft tissue reconstruction was carried out with the internal fixations. As for the complications there were 2 cases of deep soft tissue infection, 2 cases of nonunion, 1 case of malunion and 1 case of knee joint stiffness.
CONCLUSION
In cases of proximal tibia fracture with severe soft tissue damage, external fixation was important to secure the safety of the fracture, carry forward the anatomical alignment, plan the soft tissue safety and manage the wound to decrease the number of microbial in the next operation, which is the internal fixation with plates.
- 485 View
- 3 Download

- Treatment of the Proximal Femoral Fractures with Proximal Femoral Nail Antirotation (PFNA)
- Myung Sik Park, Young Jin Lim, Young Sin Kim, Kyu Hyung Kim, Hong Man Cho
- J Korean Fract Soc 2009;22(2):91-97. Published online April 30, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.2.91
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the clinical and radiologic results of treatments in proximal femoral fracture with Proximal Femoral Nail-Antirotation (PFNA).
MATERIALS AND METHODS
We retrospectively reviewed the results of 21 cases of proximal femoral fracture treated with PFNA from September 2006 to October 2007 which could be followed up for minimum of more than a year. The mean age was 61.5 (20~88) years old. Male were involved in 12 cases, female in 9 cases. The mean follow up was 14.3 (12~18) months. The Garden alignment index, Cleveland index, tip apex distance were evaluated by post-operative radiologic evaluation and complications of bone union, failure of internal fixation and deformity were evaluated by follow up radiologic findings. Clinical results were assessed by social function score of Jensen and mobility score of Parker and Palmer at last follow up.
RESULTS
All fractures were united and the mean time to bone union was 15.7 (13~18) weeks. Garden alignment index showed good results of above 'good' in 15 cases (71.4%), Cleveland index showed 14 cases (66.4%) positioning in zone 5 and tip apex distance showed 17.81 (+/-5.65~27.52) mm in radiologic findings. The mean sliding of blade was 1.32 (0.34~2.94) mm in follow up radiologic findings and fracture of distal locking screw area was found in 1 case as a complication. Among 21 cases, the function before injury was completely recovered in 15 cases (71.4%) which were assessed by social function score of Jensen and 13 cases (61.9%) by mobility score of Parker and Palmer.
CONCLUSION
We think that PFNA is effective osteosynthetic device for proximal femur fracture with satisfactory radiologic and clinical outcomes. -
Citations
Citations to this article as recorded by- Clinical and radiological outcome of the Chimaera short nailing system in inter- and subtrochanteric fractures
Aurélien Traverso, Trieu-Hoai-Nam Ngo, Guillem Fernandez Gil, Xavier Lannes, Sylvain Steinmetz, Kevin Moerenhout
Injury.2023; 54(3): 970. CrossRef - Comparative Study of Intertrochanteric Fracture Treated with the Proximal Femoral Nail Anti-Rotation and the Third Generation of Gamma Nail
Jae-Cheon Sim, Tae-Ho Kim, Ki-Do Hong, Sung-Sik Ha, Jong-Seong Lee
Journal of the Korean Fracture Society.2013; 26(1): 37. CrossRef - The Treatment of Intertrochanteric Femoral Fracture with Proximal Femoral Nail Antirotation
Jong Won Kim, Hyun Soo Park, Young Soo Jang, Jae Hyuk Choi, Sung Ju Bae, Chan Il Bae
Journal of the Korean Fracture Society.2012; 25(4): 257. CrossRef - Cementless Bipolar Hemiarthroplasty Using a Rectangular Cross-section Stem for Type A2 or above Intertrochanteric Fractures
Bong-Ju Park, Hong-Man Cho, Cheol Park, Hwang-Se Bong
Hip & Pelvis.2012; 24(3): 222. CrossRef - Hip Arthroplasty for Failed Internal Fixation of Intertrochanteric Fractures
Ju-Oh Kim, Hong-Man Cho, Cheol Park, Ju-Hyun Sim
Hip & Pelvis.2012; 24(2): 94. CrossRef - Anatomical Measurement of Normal Korean Proximal Femur Using Plain Radiography: A Problem when using Proximal Femoral Nail Anti-rotation
Jong-Seok Park, Woo-Jong Kim, Jae-Wan Soh, Byung-Woong Jang, Tae-Heon Kim, You-Sung Suh
Hip & Pelvis.2011; 23(4): 303. CrossRef - The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
Jeoung Ho Kim, Sang Hong Lee, Kwang Chul Lee, Sung Won Cho
Journal of the Korean Fracture Society.2011; 24(3): 217. CrossRef - PFNA and PFN in Intertrochanteric Fractures - Comparison Study of Sliding -
Suk Kyu Choo, Hyoung Keun Oh, Jun Young Choi
Hip & Pelvis.2010; 22(1): 79. CrossRef - Proximal Femoral Nail Antirotation versus Compression Hip Screw with Trochanter Stabilizing Plate for Unstable Intertrochanteric Hip Fractures
Jae-Young Rho, Sang-Bum Kim, Youn-Moo Heo, Seong-Jin Cho, Dong-Sik Chae, Woo-Suk Lee
Journal of the Korean Fracture Society.2010; 23(2): 161. CrossRef - Treatment of the Unstable Intertrochanteric Fracture with Proximal Femoral Nail Antirotation: Comparison with Compression Hip Screw with Trochanteric Stabilizing Plate
Tae-Ho Kim, Jong-Oh Kim, Seung-Yup Lee, Geon-Ung Yun
Journal of the Korean Fracture Society.2010; 23(4): 353. CrossRef
- Clinical and radiological outcome of the Chimaera short nailing system in inter- and subtrochanteric fractures
- 826 View
- 2 Download
- 10 Crossref

- Staged Minimally Invasive Plate Osteosynthesis of Proximal Tibial Fracture
- Joon Woo Kim, Chang Wug Oh, Jong Keon Oh, Hee Soo Kyung, Woo Kie Min, Byung Chul Park, Kyung Hoon Kim, Hee Joon Kim
- J Korean Fract Soc 2009;22(1):6-12. Published online January 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.1.6
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the results of staged MIPO (Minimally Invasive Plate Osteosynthesis) for proximal tibial fractures with compromised soft tissue.
MATERIALS AND METHODS
Eighteen proximal tibial fractures (AO 41:9 cases, AO 42:9 cases) included this study. Ten were open fractures. After temporary external fixation until soft tissue healed (mean 27.3 days), MIPO was performed secondarily without bone graft. We assessed the bony union and knee function, and affecting factors of the results were investigated.
RESULTS
All fractures united at 20 weeks (range, 11~32) except 1 case. Mean range of knee flexion was 134.4degrees and mean IOWA knee score was 89.1. There were 2 superficial and 2 delayed deep infections from open fractures (grade II:1 case, grade III:3 cases), although they healed after implant removal. Open fractures seem to influence the infection rate. Otherwise, there was no related factor affecting the results.
CONCLUSION
MIPO after temporary external fixation can provide favorable results in proximal tibial fractures with soft tissue injuries, but attention of delayed infection should be paid in open fractures. -
Citations
Citations to this article as recorded by- MINIMALLY INVASIVE OSTEOSYNTHESIS WITH PLATE OR NAIL FOR META-DIAPHYSEAL TIBIAL FRACTURES - WHAT IS BETTER?
B. Makelov
Trakia Journal of Sciences.2023; 21(4): 357. CrossRef - Effect of Korean Medicine Treatments in Patients with Proximal Tibia Fracture: A Retrospective Observational Study
Jung Min Lee, Eun-Jung Lee
Journal of Korean Medicine Rehabilitation.2020; 30(3): 141. CrossRef - Comparison of Time to Operation and Efficacies of Ultrasound-Guided Nerve Block and General Anesthesia in Emergency External Fixation of Lower Leg Fractures (AO 42, 43, 44)
Chan Kang, Sang-Bum Kim, Youn-Moo Heo, You-Gun Won, Byung-Hak Oh, June-Bum Jun, Gi-Soo Lee
The Journal of Foot and Ankle Surgery.2017; 56(5): 1019. CrossRef - Minimally Invasive Plate Osteosynthesis for Proximal Tibial Shaft Fracture
Young-Soo Byun, Ki-Chul Park, Hyun-Jong Bong, Chang-Hoon Lee
Journal of the Korean Fracture Society.2011; 24(1): 23. CrossRef - The Use of Fresh Frozen Allogenic Bone Graft in the Impacted Tibial Plateau Fractures
Yeung Jin Kim, Soo Uk Chae, Jung Hwan Yang, Ji Wan Lee, Dae Han Wi, Duk Hwa Choi
Journal of the Korean Fracture Society.2010; 23(1): 26. CrossRef - Management of Open Fracture
Gu-Hee Jung
Journal of the Korean Fracture Society.2010; 23(2): 236. CrossRef - Staged Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures
Sung-Ki Park, Chang-Wug Oh, Jong-Keon Oh, Kyung-Hoon Kim, Woo-Kie Min, Byung-Chul Park, Won-Ju Jeong, Joo-Chul Ihn
Journal of the Korean Fracture Society.2010; 23(3): 289. CrossRef - Intramedullary Nailing of Proximal Tibial Fractures
Young-Soo Byun, Dong-Ju Shin
Journal of the Korean Fracture Society.2009; 22(3): 197. CrossRef - Proximal Tibia Fracture: Plating
Ki-Chul Park
Journal of the Korean Fracture Society.2009; 22(3): 206. CrossRef
- MINIMALLY INVASIVE OSTEOSYNTHESIS WITH PLATE OR NAIL FOR META-DIAPHYSEAL TIBIAL FRACTURES - WHAT IS BETTER?
- 566 View
- 0 Download
- 9 Crossref

- Cause and Treatment of Extraarticular Proximal Tibial Nonunion
- Sung Soo Kim, Sung Keun Shon, Kyu Yeol Lee, Chul Hong Kim, Myung Jin Lee, Min Soo Kang, Lih Wang, Im Sic Ha
- J Korean Fract Soc 2008;21(4):279-285. Published online October 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.4.279
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the factors affecting the nonunion of extraarticular proximal tibial fracture and the outcome of nonunion treatment.
MATERIALS AND METHODS
We investigated 51 cases of extraarticular proximal tibial fractures from June 2002 to May 2006. The nonunion rate was assessed in relation to several risk factors and the treatment outcome of nonunion using plate fixation with bone graft was assessed by Klemm and BOrner functional rating system.
RESULTS
6 cases of nonunion (11.8%) was noted among 51 cases, and the risk factors examined, OTA A3 comminuted fracture was associated with a high nonunion rate with statistical significance and initial bone graft had a significant effect in bone healing. Excellent and good results were obtained in 5 cases (83.3%) and bone union was achieved in all nonunion cases.
CONCLUSION
Comminution was found to be an important factor affecting the nonunion in extraarticular proximal tibial fracture, and bone graft in primary operation could reduce the chance of nonunion. Accurate plate fixation with bone graft is a reliable option in nonunion treatment.
- 397 View
- 1 Download

- Hemiarthoplasty with Bone Block Graft and Low Profile Prosthesis for the Comminuted Proximal Humerus Fractures
- Chung Hee Oh, Joo Han Oh, Sae Hoon Kim, Ki Hyun Jo, Sung Woo Bin, Hyun Sik Gong
- J Korean Fract Soc 2008;21(3):213-219. Published online July 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.3.213
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the outcome of hemiarthroplasty with bone block graft and low profile prosthesis (Aequalis(R) fracture prosthesis) for the comminuted proximal humerus fractures.
MATERIALS AND METHODS
Sixteen low profile prostheses were used since July 2004, and 11 patients were followed-up for average 19.9 (12~30) months. Their mean age was 67.3 (52~78) years. Pain and satisfaction visual analog scale (VAS), range of motion, and modified UCLA score for hemiarthroplasty were evaluated at every visit. Radiography was also checked for stem position, loosening, and tuberosity union.
RESULTS
Mean pain VAS was 2.7 (0~5), and mean satisfaction VAS was 8.4 (5~10). Mean active forward flexion was 137 degrees (90~170), external rotation at side was 45.5 degrees (25~70), and internal rotation at back was T10 (T7~L1). Modified UCLA score was 19 (12~30) at final visit. All stems were stable, and there were no loosening at the final follow-up. All tuberosities were united except two tuberosity absorptions.
CONCLUSION
The outcome of hemiarthroplasty with bone block graft and low profile prosthesis was comparable to other implants for comminuted proximal humerus fractures. This system had unique advantages for tuberosity union. Further study with more patients and longer follow-up are necessary to clarify the effectiveness of this prosthesis. -
Citations
Citations to this article as recorded by- A Separate Approach and Cephalo-Diaphyseal Plate Fixation for the Comminuted Metadiaphyseal Fractures of the Proximal Humerus
Sung-Weon Jung
Journal of the Korean Fracture Society.2013; 26(1): 8. CrossRef - Comparison of Results between Internal Plate Fixation and Hemiarthroplasty in Comminuted Proximal Humerus Fracture
Doo-Sup Kim, Dong-Kyu Lee, Chang-Ho Yi, Jang-Hee Park, Jung-Ho Rah
Journal of the Korean Fracture Society.2011; 24(2): 144. CrossRef
- A Separate Approach and Cephalo-Diaphyseal Plate Fixation for the Comminuted Metadiaphyseal Fractures of the Proximal Humerus
- 504 View
- 0 Download
- 2 Crossref

- Double Tension Band Wiring for Olecranon Fractures
- Suk Kang, Chung Soo Hwang, Phil Hyun Chung, Young Sung Kim, Jin Wook Chung, Jong Pil Kim
- J Korean Fract Soc 2008;21(2):130-134. Published online April 30, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.2.130
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the clinical results of double tension band wiring for communited olecranon fractures involving proximal 1/3.
MATERIALS AND METHODS
We reviewed 9 cases of communited olecranon fractures involving proximal 1/3 treated with double tension band wiring followed for minimum 10 months. There were 2 cases of olecranon fractures involving only proximal 1/3, 6 cases of olecranon fractures involving from proximal 1/3 to middle 1/3 and 1 case of olecranon fractures involving from proximal 1/3 to distal 1/3. We analyzed the bone union time, radiologic results for gap, reduction loss, pin migration, pain, range of motion, complications and functional outcomes at last follow up.
RESULTS
All patients had solid bone union without additional surgery and average union time was 10.3 weeks. Anatomical reduction could be obtained in 8 of 9 cases but there was 1 mm step off in one case. 36 pins were used to fix the fractures, 1 pin of 18 distal pins and 2 pins of 18 proximal pins were migrated to backward but there was no reduction loss. Only 1 distal pin needed early removal due to skin irritation. Average range of motion ranged from flexion contracture 3.3 degrees to further flexion 137.8 degrees. On functional analysis, we got 8 cases of good result, 1 case of fair result and there was no poor result.
CONCLUSION
Double tension band wiring for comminuted olecranon fracture involving proximal 1/3 was concluded to give a firm fixation of the fracture site as bone union could be acquired without serious pin problems. -
Citations
Citations to this article as recorded by- Treatment of Olecranon Fractures with Proximal Ulna Comminution Using Locking Compression Plates
Ki-Do Hong, Tae-Ho Kim, Jae-Cheon Sim, Sung-Sik Ha, Min-Chul Sung, Jong-Hyun Jeon
Journal of the Korean Fracture Society.2015; 28(1): 59. CrossRef - Olecranon Nonunion after Operative Treatment of Fracture
Ho-Jung Kang, Ji-Sup Kim, Myung-Ho Shin, Il-Hyun Koh, Yun-Rak Choi
Journal of the Korean Fracture Society.2015; 28(1): 30. CrossRef
- Treatment of Olecranon Fractures with Proximal Ulna Comminution Using Locking Compression Plates
- 573 View
- 0 Download
- 2 Crossref

- Classification and Treatment of Unstable Intertrochanteric Fracture according to the Existence of Posterior Fragment : Preliminary Report
- Lih Wang, Sung Keun Shon, Kyu Yeol Lee, Chul Hong Kim, Myung Jin Lee, Chul Won Lee, Sung Soo Kim
- J Korean Fract Soc 2008;21(2):110-116. Published online April 30, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.2.110
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To predict the feature and stability of intertrochanteric fractures with posterior fragment using preoperative 3D computed tomography and to investigate the importance of the posterior fragment in treatment of unstable intertrochanteric fracture.
MATERIALS AND METHODS
15 cases of unstable fractures with posterior fragment which were treated with nail only between October 2006 to August 2007 were classified into 2 groups: study group (5 cases with cannulated screw fixation of posterior fragment) and control group (10 cases without cannulated screw fixation). The average difference of neck-shaft angle, neck screw sliding distance and the complications in the two groups were compared retrospectively after a follow up of at least 3 months.
RESULTS
The average difference of neck-shaft angle in study and control group was 3.8 and 7.5 degree (p>0.05), respectively. The average difference of neck screw sliding distance was 1.6 and 6.6 mm (p<0.05), respectively. Complication which required reoperation was not noted in study group and complications of 3 cases about neck screw lateral protrusion, proximal migration and Z-effect phenomenon were noted in control group.
CONCLUSION
The recognition and fixation of the posterior wall was found to be an important predictive factor in unstable intertrochanteric fracture treatment. -
Citations
Citations to this article as recorded by- Outcomes of dynamic hip screw augmented with trochanteric wiring for treatment of unstable type A2 intertrochanteric femur fractures
Chetan Puram, Chetan Pradhan, Atul Patil, Vivek Sodhai, Parag Sancheti, Ashok Shyam
Injury.2017; 48: S72. CrossRef - Additional Fixations for Sliding Hip Screws in Treating Unstable Pertrochanteric Femoral Fractures (AO Type 31-A2): Short-Term Clinical Results
Su Hyun Cho, Soo Ho Lee, Hyung Lae Cho, Jung Hoei Ku, Jae Hyuk Choi, Alex J Lee
Clinics in Orthopedic Surgery.2011; 3(2): 107. CrossRef
- Outcomes of dynamic hip screw augmented with trochanteric wiring for treatment of unstable type A2 intertrochanteric femur fractures
- 1,420 View
- 4 Download
- 2 Crossref

- Treatment with Modified Steinmann Pins and Tension Band Wiring Technique in Proximal Humeral Comminuted Fractures with Osteoporosis
- Soo Tai Chung, Joo Hak Kim, Hyung Soo Kim, Sang Joon Park
- J Korean Fract Soc 2007;20(2):184-189. Published online April 30, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.2.184
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the usefulness of internal fixation with modified Steinmann pins and tension band wiring technique in comminuted proximal humeral fracture with osteoporosis and the correlations among bone mineral density, age, Neer's score and period of union.
MATERIALS AND METHODS
Twelve cases of comminuted proximal humeral fracture with osteoporosis were surgically treated with modified Steinmann pins and tension band technique, and followed up for an average 20.8 months (range, 6~39 months). Average age was 73.6 years old (range, 59~85 years old). Results were assessed using Neer's evaluation criteria.
RESULTS
Excellent results were noted in eight cases and satisfactory results in four cases. Radiological union was obtained in all cases. Two cases showed impingement syndrome of the proximal portions of Steinmann pins, which were managed by early removal of the metal. One case developed operative wound infection, which were managed by antibiotics therapy, irrigation and secondary closure.
CONCLUSION
Internal fixation using modified Steinmann pins and tension band wiring technique for proximal humeral fracture, with osteoporosis, makes complete union of fracture, minimizes risk of complications, and enables early rehabilitation by rendering relatively rigid fixation.
- 363 View
- 1 Download

- Open Intramedullary Nail with Tension Band Sutures & Lock Sutures on Proximal Humeral Three-part Fracture
- Jin Oh Park, Jin Young Park, Sung Tae Lee, Hong Keun Park
- J Korean Fract Soc 2007;20(1):45-52. Published online January 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.1.45
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the results according to the difference of age and bone mineral density (BMD) of the surgical treatments using open intramedullary nail with tension sutures and lock suture on proximal humeral three part fracture.
MATERIALS AND METHODS
30 patients treated by open intramedullary nail with tension band and lock suture technique on proximal humeral fractures were reviewed. After treatment, average follow up periods was 50 months (range; 17~143 month). Postoperative clinical outcome was evaluated using ASES functional score, Neer score and constant score.
RESULTS
Bony union were obtained all except one case. Range of motion, mean forward elevation was 142°, mean external rotation was 56°, mean external rotation at 90° abduction was 68°. Average pain score of visual analog scale was 1.5. Average functional score of American Shoulder and Elbow Society was 86. Average Neer score was 89. Constant score was 85. Pain and functional score of group I were better than those of group, however, there was no statistically significant difference (p>0.05). In the comparison between group III and group IV, the results were same (p>0.05).
CONCLUSION
The patients treated using open intramedullary nailing, tension band and lock suture could enable early ROM exercise and show good clinical results. This treatment method will be useful in old age osteoprorotic patients. -
Citations
Citations to this article as recorded by- Hemiarthoplasty with Bone Block Graft and Low Profile Prosthesis for the Comminuted Proximal Humerus Fractures
Chung Hee Oh, Joo Han Oh, Sae Hoon Kim, Ki Hyun Jo, Sung Woo Bin, Hyun Sik Gong
Journal of the Korean Fracture Society.2008; 21(3): 213. CrossRef
- Hemiarthoplasty with Bone Block Graft and Low Profile Prosthesis for the Comminuted Proximal Humerus Fractures
- 538 View
- 0 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


