Funded articles
- Page Path
- HOME > Browse articles > Funded articles
Original Articles
- Correlation of bone mineral density with ankle fractures in older adults in Korea: a retrospective cohort study
- Seung Hyun Lee, Chae Hun Lee, Seo Jin Park, Jun Young Lee
- J Musculoskelet Trauma 2025;38(4):186-192. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00150
- Funded: Chosun University
-
 Abstract
Abstract
 PDF
PDF - Background
Bone mineral density (BMD) is well-documented in relation to fractures of the spine, hip, distal radius, and proximal humerus; however, its correlations with other fracture types are less established. This study aimed to analyze BMD and associated risk factors in older adults (≥65 years of age) with osteoporotic ankle fractures. These fractures involve low-energy trauma, resulting from falls from a standing height or lower, and occur from impacts which typically do not cause fractures in individuals with normal bone.
Methods
This retrospective study analyzed data from 1,411 patients diagnosed with ankle fractures admitted to Chosun University Hospital between February 2012 and April 2023. After applying inclusion criteria (age ≥65 years; low energy ankle fracture) and exclusion criteria (high energy trauma, open/multiple fractures, missing dual X-ray absorptiometry [DXA]), 73 of 1,411 patients were analyzed. Lumbar spine, femoral neck, and total hip T scores were obtained with a Horizon Wi DXA scanner, and associations with age, sex, mechanism of injury, comorbidities, smoking status, alcohol consumption, body mass index (BMI), and history of fractures were tested by ANOVA with Scheffe post hoc and Fisher exact tests.
Results
Lower BMD correlated significantly with older age, female sex, and lower BMI (P<0.05) in older adults with ankle fractures. No significant associations were observed for comorbidities (diabetes, hypertension, dementia), smoking, alcohol consumption, injury mechanism, or prior fractures.
Conclusion
These results indicate that older age, female, and lower BMI are linked to reduced BMD in ankle fracture patients over 65 years of age. Focused osteoporosis screening and management may therefore be most beneficial for older, low BMI women presenting with ankle fractures. Level of evidence: IV.
- 831 View
- 2,147,483,670 Download

- Risk factors for ankle fractures in older adults based on clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities in Korea: a retrospective case-control study
- Myeong Jun Song, Se Woong Jang, Jun Young Lee, Seojin Park
- J Musculoskelet Trauma 2025;38(4):193-202. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00143
- Funded: Chosun University Hospital
-
 Abstract
Abstract
 PDF
PDF - Background
Ankle fractures are common in older adults; however, their relationship with osteoporotic fractures remains unclear. This study aimed to evaluate potential risk factors for ankle fractures in older adults by analyzing individual clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities.
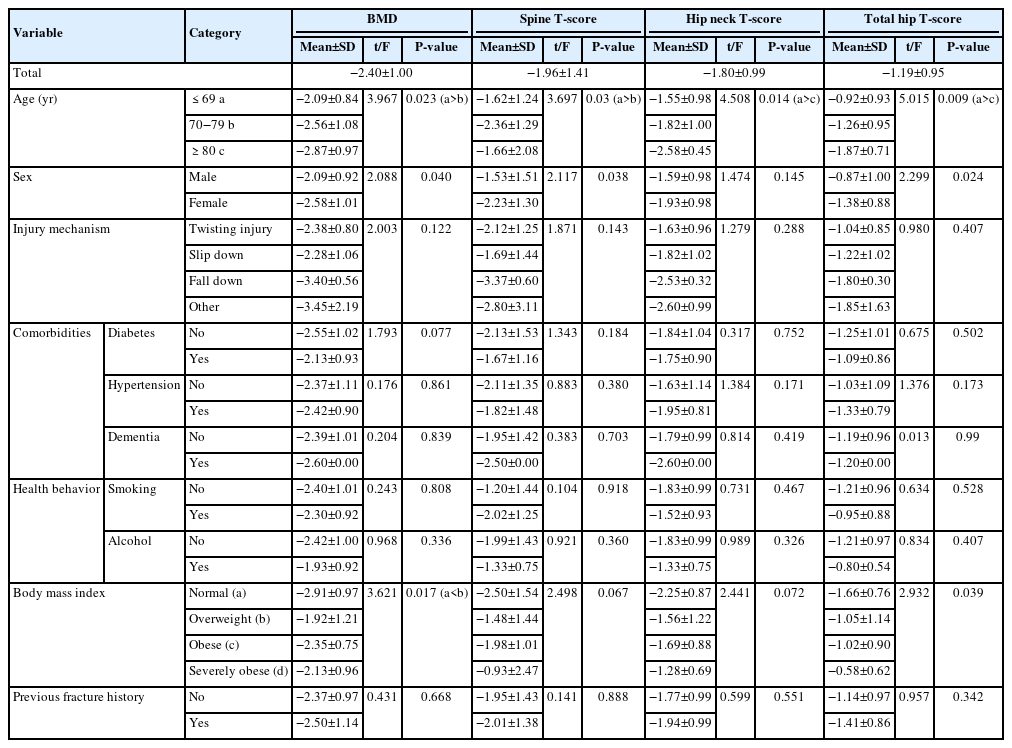
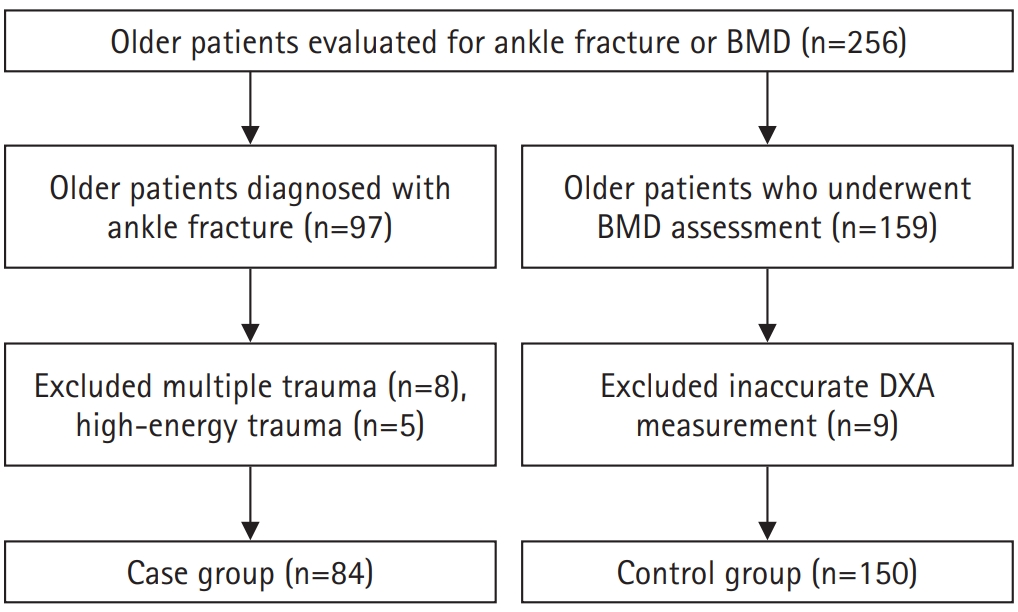
Methods
We conducted a retrospective case-control study including 84 patients aged ≥65 years with ankle fractures and 150 controls who underwent bone mineral density (BMD) testing without prior ankle fractures. The variables analyzed included age, sex, body mass index, smoking, alcohol consumption, prior fracture history, and comorbidities such as hypertension, diabetes mellitus, and dementia. BMD was measured at the spine, total hip, and femoral neck.
Results
Univariate analysis showed that alcohol consumption, diabetes mellitus, and total hip T-score categories were significantly associated with ankle fractures. In binary logistic regression, alcohol consumption remained significantly associated with higher ankle fracture risk (odds ratio [OR], 5.302; 95% confidence interval [CI], 1.778–15.811; P=0.003), and both osteopenia and osteoporosis at the total hip were also associated with increased risk (OR, 3.260, P=0.049; OR, 3.561, P=0.031, respectively). Diabetes mellitus did not reach statistical significance in the adjusted model (P=0.074). Model fit was adequate (Hosmer-Lemeshow P=0.377), and post hoc power analysis confirmed sufficient sample size.
Conclusions
These findings suggest that lower total hip BMD and alcohol-related factors may be associated with ankle fracture risk in older adults. The FRAX score itself was not calculated; instead, this study focused on analyzing selected clinical components. Limitations include the retrospective design, lack of fall and medication data, and cross-sectional BMD assessment. Level of evidence: III.
- 1,044 View
- 21 Download

- Computational simulation of coracoclavicular screw insertion through the superior distal clavicular plate for clinical applications in Korean cadavers
- Hyung-Lae Cho, Ji Han Choi, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):143-151. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00122
- Funded: Gyeongsang National University
-
 Abstract
Abstract
 PDF
PDF - Background
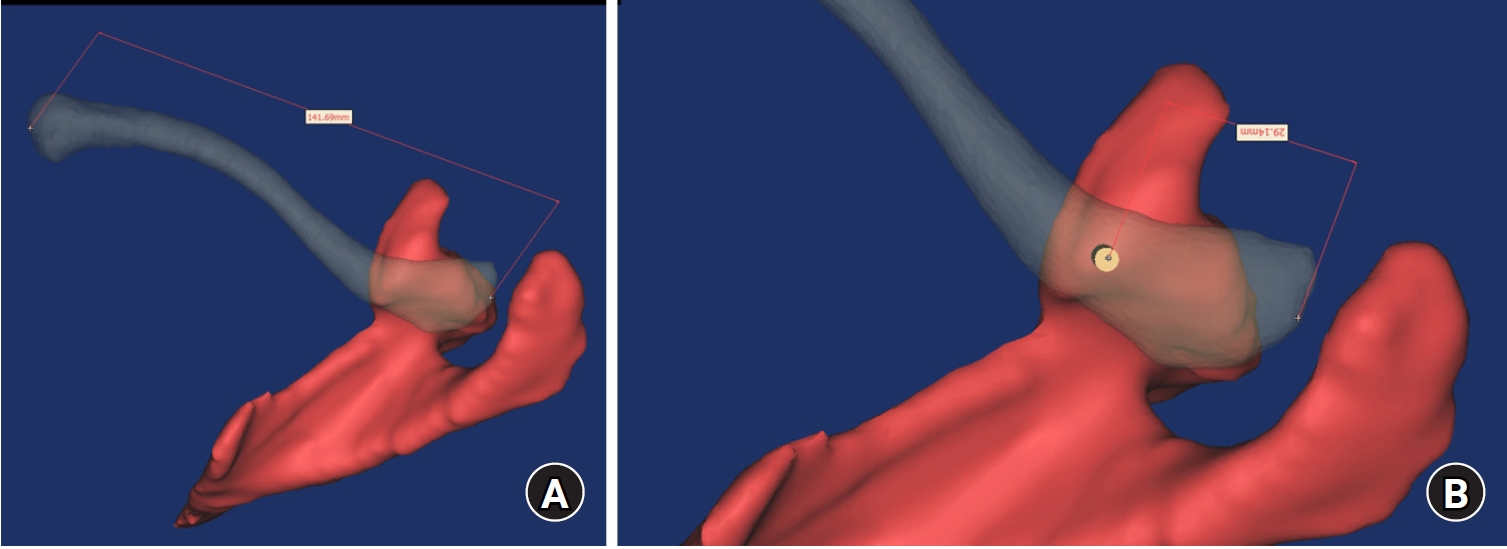
The study was conducted to determine the practical area for inserting the coracoclavicular (CC) screw through the plate by analyzing three-dimensional (3D) shoulder models featuring virtually implanted, actual-size plates and screws.
Methods
Ninety cadaveric shoulders (41 males and 49 females) underwent continuous 1.0-mm slice computed tomography scans. The data were imported into image-processing software to generate a 3D shoulder model, including the scapula and clavicle. The overlapping area between the clavicle and the horizontal portion of the coracoid process (horizontal portion_CP) was analyzed in the cranial view. A curved pelvic recon plate was virtually placed on the upper surface of the distal clavicle, and an actual-size (3.5 mm) CC screw was inserted through the plate.
Results
The distal clavicle directly overlapped with the horizontal portion_CP in the vertical direction. The overlapping area was sufficient to place the 3.5 mm and 4.5 mm-sized screws. In all shoulder models, the CC screw could be inserted through the plate into the vertical direction, with an average length of 35.5 mm (range, 26.2–62.5 mm; standard deviation, 1.2 mm). In 87 models, the CC screw was inserted through the third hole from the lateral end of the plate. Two models were inserted through the second hole, and one model through the fourth hole.
Conclusions
The upper surface of the clavicle has sufficient overlapping area to place CC screws through the plate in the vertical direction in the corresponding hole. Supplemental CC screw fixation through the plate can be performed without additional or special equipment. Level of evidence: IV
- 615 View
- 21 Download

- Biomechanical finite element analysis of a femoral neck system fixation construct for femur neck fractures and clinical implications
- Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):133-142. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00108
- Funded: Gyeongsang National University
-
 Abstract
Abstract
 PDF
PDF - Background
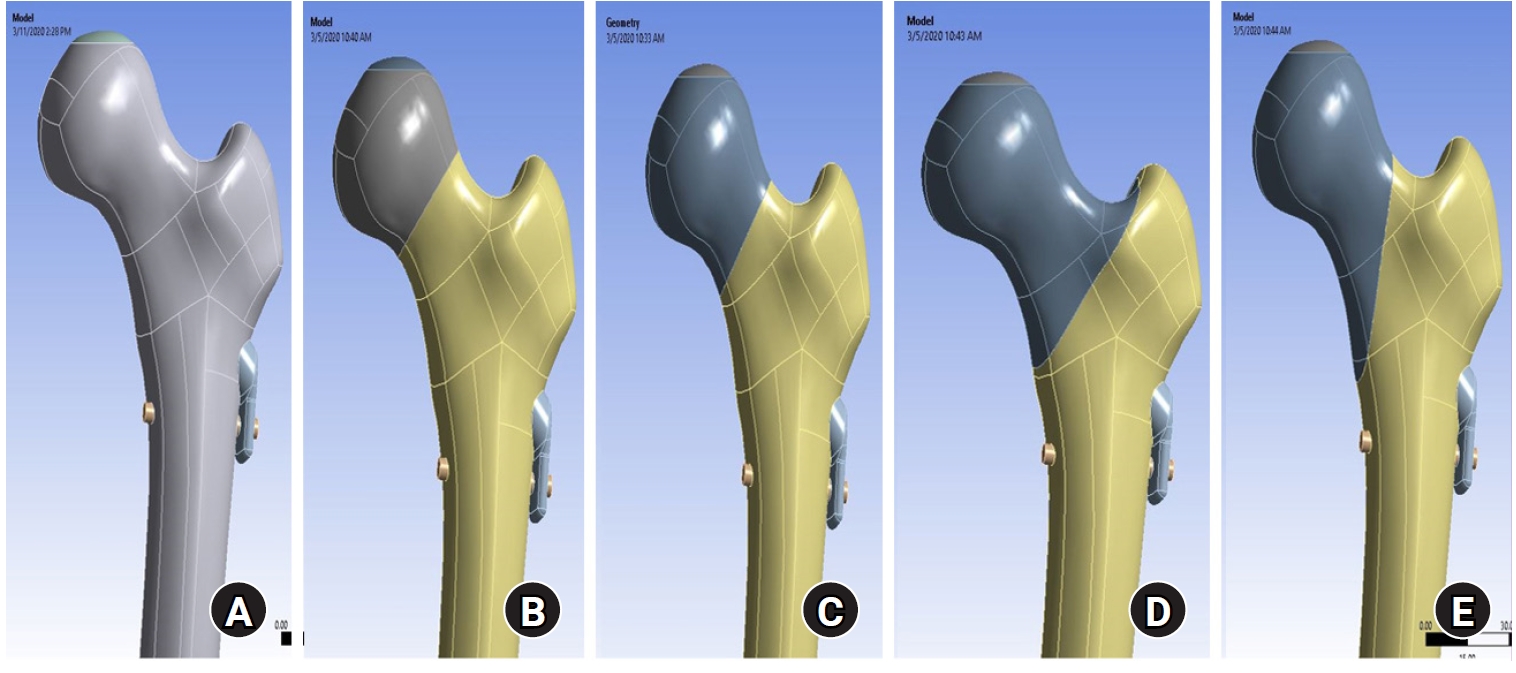
This study assessed the structural/mechanical stability of fixation constructs with a femoral neck system (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications.
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital, 68.56 MPa for a transcervical, 344.54 MPa for a basicervical, and 130.59 MPa for a vertical model. The maximum VMS of FNS was 840.34 MPa for a subcapital, 637.37 MPa for a transcervical, 464.07 MPa for a basicervical, and 421.01 MPa for a vertical model. The stress distribution of basicervical and vertical fractures differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
FNS fixation should be performed with consideration the osseous anchorage in the femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution. Level of evidence: IV.
- 1,814 View
- 82 Download

Review Article
- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
- Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(2):74-85. Published online March 31, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00024
- Funded: Ministry of Science and ICT, Ministry of Trade, Industry and Energy, Ministry of Health and Welfare, Ministry of Food and Drug Safety

-
 Abstract
Abstract
 PDF
PDF - Distal tibial metaphyseal fractures are commonly caused by high-energy injuries in young men and osteoporosis in older women. These fractures should be clearly distinguished from high-energy pilon fractures. Although the optimal surgical intervention methods for distal tibial metaphyseal fractures remain uncertain and challenging, surgical treatments for nonarticular distal tibia fractures can be broadly divided into two types: plate fixation and intramedullary nail (IMN) fixation. Once functional reduction is achieved using an appropriate technique, distal tibial nailing might be slightly superior to plate fixation in reducing postoperative complications. Thus, the surgical strategy should focus on functional realignment and proceed in the following sequence: (1) restoring the original tibial length, regardless of whether fibular fixation is to be done; (2) making the optimal entry point through an anteroposterior (AP) projection based on the overlapping point between the fibular tip and lateral plateau margin; (3) placing Kirschner wires (Ø2.4 mm) as blocking pins (in the AP orientation for coronal control and in the mediolateral [ML] orientation for sagittal control) as close to the upper locking hole as possible without causing further comminution on the concave aspect of the short fragment; and (4) making the the distal fixation construct with at least two ML and one AP interlocking screw or two ML interlocking screws and blocking screws. After the IMN is adequately locked, blocking pins (Ø2.4 mm) need to be replaced by a 3.5 mm screw.
-
Citations
Citations to this article as recorded by- Impact of Foot Width on Patient-Reported Outcomes Assessed by 3-Dimensional Foot Morphometry in Hallux Valgus
Jungtae Ahn, Dae-Cheol Nam, Gu-Hee Jung
Clinics in Orthopedic Surgery.2025; 17(6): 1062. CrossRef
- Impact of Foot Width on Patient-Reported Outcomes Assessed by 3-Dimensional Foot Morphometry in Hallux Valgus
- 2,709 View
- 52 Download
- 1 Crossref

Original Article
- The clinical outcome of treating elderly distal radius fractures by long volar locking plate with the elimination of irreducible metaphyseal comminuted volar cortical fragments: a retrospective case series
- Soo Min Cha
- J Musculoskelet Trauma 2025;38(1):13-22. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00003
- Funded: Chungnam National University

-
 Abstract
Abstract
 PDF
PDF - Background
In severe comminuted metaphyseal distal radius fracture (DRF) of elderly patients, after maintaining only radiological parameters of the radius using long volar locking plates (VLPs), we inevitably eliminated a few volar cortical fragments of metaphysis. Here, we report the final radiological and clinical outcomes of our method. Methods: For the patients who were treated between 2014 and 2018, the demographic factors, the preoperative radiologic factors, area of the eliminated volar cortical fragment, and final radiologic parameter, were evaluated. Clinical outcomes and ranges of active motion were evaluated. Results: In total, 31 patients were included. The mean patient age was 77.3 years and the mean eliminated cortical area was 3.30 cm2. At the final follow-up, the mean volar tilt, radial inclination, articular step-off, and ulnar variance were 10.35°, 20.00°, 0.58 mm, and 0.71 mm, respectively. There were no definitive correlations between bone mineral density, fragment area, the largest cortical fragment diameter ratio and differences in final and immediate postoperative measurements of these radiological parameters, respectively. Visual analog scale and disabilities of the arm, shoulder, and hand (DASH) scores were satisfactory, and the mean arcs of flexion-extension and pronation-supination were 124.35° and 133.23°. Clinical outcomes were not significantly different according to the AO system category. Conclusions: For maintenance of radiological parameters of the radius, long VLPs are useful in older patients with DRFs who exhibit volar metaphyseal comminution, despite concurrent ulnar fractures. Inevitable elimination of irreducible free comminuted cortical fragments when filling the defect does not affect final radiological and clinical outcomes. Level of evidence: Level IV, case series.
- 1,194 View
- 44 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


