Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 24(1); 2011 > Article
-
Original Article
- Minimally Invasive Plate Osteosynthesis for Proximal Tibial Shaft Fracture
- Young-Soo Byun, M.D., Ki-Chul Park, M.D., Hyun-Jong Bong, M.D., Chang-Hoon Lee, M.D.
-
Journal of the Korean Fracture Society 2011;24(1):23-27.
DOI: https://doi.org/10.12671/jkfs.2011.24.1.23
Published online: January 19, 2011
Department of Orthopaedic Surgery, Guri Hospital, Hanyang University College of Medicine, Guri, Korea.
*Department of Orthopaedic Surgery, Daegu Fatima Hospital, Daegu, Korea.
- Address reprint requests to: Ki-Chul Park, M.D. Department of Orthopaedic Surgery, Guri Hospital, Hanyang University College of Medicine, 249-1, Gyomun-dong, Guri 471-701, Korea. Tel: 82-31-560-2316·Fax: 82-31-557-8781, kcpark@hanyang.ac.kr
• Received: October 7, 2010 • Revised: October 25, 2010 • Accepted: October 26, 2010
Copyright © 2011 The Korean Fracture Society
- 669 Views
- 9 Download
- 2 Crossref
Abstract
-
Purpose
- To report the results of patients treated by minimally invasive plate osteosynthesis (MIPO) for proximal tibial shaft fractures.
-
Materials and Methods
- From September 2003 to June 2008, thirty-two patients with proximal tibial shaft fractures weretreated by MIPO. There were 22 men and 10 women and mean age was 43.8 years (range; 21~72 years). Follow-up was available for all patients and the mean follow-up period was 19.5 months (range; 12~40 months). Duration of union, range of knee motion and postoperative complications were evaluated.
-
Results
- Twenty-nine patients (90.6%) healed after the MIPO technique. The mean duration of radiographic union was 18.3 weeks (range; 10~28 weeks). The mean range of knee motion was 134 degrees at the last follow-up. There were 1 non-union, 2 delayed unions, 1 superficial infection, 1 deep infection, 2 malunions with more than 5 degrees of malalignment and 14 cases of skin irritation by plate.
-
Conclusion
- MIPO is an effective treatment for closed, proximal tibialshaft fractures. More aggressive treatment such as dual plating should be considered in fractures with severe comminution or bone loss.
- 1. Boldin C, Fankhauser F, Hofer HP, Szyszkowitz R. Three-year results of proximal tibia fractures treated with the LISS. Clin Orthop Relat Res, 2006;445:222-229.Article
- 2. Böstman O, Hänninen A. The fibular reciprocal fracture in tibial shaft fractures caused by indirect violence. Arch Orthop Trauma Surg, 1982;100:115-121.ArticlePDF
- 3. Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma, 2004;18:528-535.
- 4. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res, 2000;375:69-77.Article
- 5. D'Aubigne RM, Maurer P, Zucman J, Masse Y. Blind intramedullary nailing for tibial fractures. Clin Orthop Relat Res, 1974;105:267-275.
- 6. Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ. Staged management of high-energy proximal tibia fractures (OTA types 41): the results of a prospective, standardized protocol. J Orthop Trauma, 2005;19:448-455.
- 7. Gerber A, Ganz R. Combined internal and external osteosynthesis a biological approach to the treatment of complex fractures of the proximal tibia. Injury, 1998;29:Suppl 3. C22-C28.Article
- 8. Helfet DL, Suk M. Minimally invasive percutaneous plate osteosynthesis of fractures of the distal tibia. Instr Course Lect, 2004;53:471-475.
- 9. Kim JW, Oh CW, Oh JK, et al. Staged minimally invasive plate osteosynthesis of proximal tibial fracture. J Korean Fract Soc, 2009;22:6-12.Article
- 10. Lachiewicz PF, Funcik T. Factors influencing the results of open reduction and internal fixation of tibial plateau fractures. Clin Orthop Relat Res, 1990;259:210-215.Article
- 11. Laflamme GY, Heimlich D, Stephen D, Kreder HJ, Whyne CM. Proximal tibial fracture stability with intramedullary nail fixation using oblique interlocking screws. J Orthop Trauma, 2003;17:496-502.Article
- 12. Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop Relat Res, 1995;315:64-74.
- 13. Littenberg B, Weinstein LP, McCarren M, et al. Closed fractures of the tibial shaft. A meta-analysis of three methods of treatment. J Bone Joint Surg Am, 1998;80:174-183.
- 14. Oh CW, Oh JK, Jeon IH, et al. Double plating of proximal tibial fractures using minimally invasive percutaneous osteosynthesis technique. J Korean Fract Soc, 2005;18:250-255.Article
- 15. Oh CW, Oh JK, Jeon IH, et al. Minimally invasive percutaneous plate stabilization of proximal tibial fractures. J Korean Fract Soc, 2004;17:224-229.
- 16. Peindl RD, Zura RD, Vincent A, Coley ER, Bosse MJ, Sims SH. Unstable proximal extraarticular tibia fractures: a biomechanical evaluation of four methods of fixation. J Orthop Trauma, 2004;18:540-545.
- 17. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br, 2002;84:1093-1110.
- 18. Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma, 2007;21:83-91.Article
- 19. Sarmiento A, Gersten LM, Sobol PA, Shankwiler JA, Vangsness CT. Tibial shaft fractures treated with functional braces. Experience with 780 fractures. J Bone Joint Surg Br, 1989;71:602-609.ArticlePDF
- 20. Schatzker J, Lambert DC. Supracondylar fractures of the femur. Clin Orthop Relat Res, 1979;138:77-83.Article
- 21. Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res, 1979;138:94-104.
- 22. Tejwani NC, Achan P. Staged management of high-energy proximal tibia fractures. Bull Hosp Jt Dis, 2004;62:62-66.
- 23. Whiteside LA, Lesker PA. The effects of extraperiosteal and subperiosteal dissection. II. On fracture healing. J Bone Joint Surg Am, 1978;60:26-30.Article
REFERENCES
Fig. 1
(A, B) A 68-year old man with severe communited proximal tibial fracture.
(C, D) The fracture was healed 20 weeks after surgery.
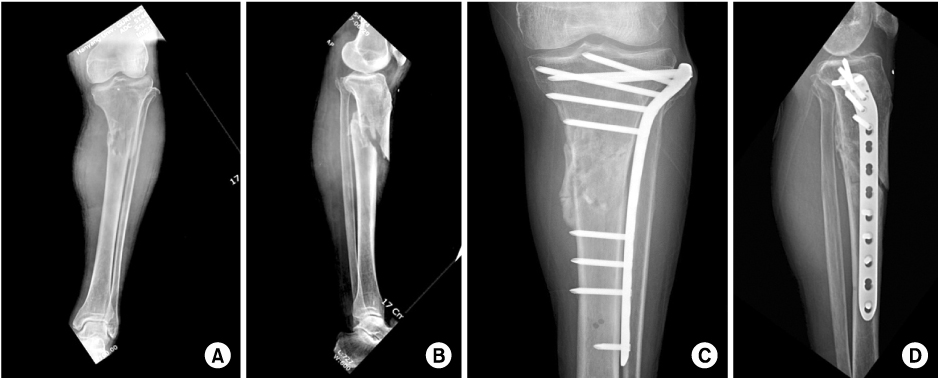
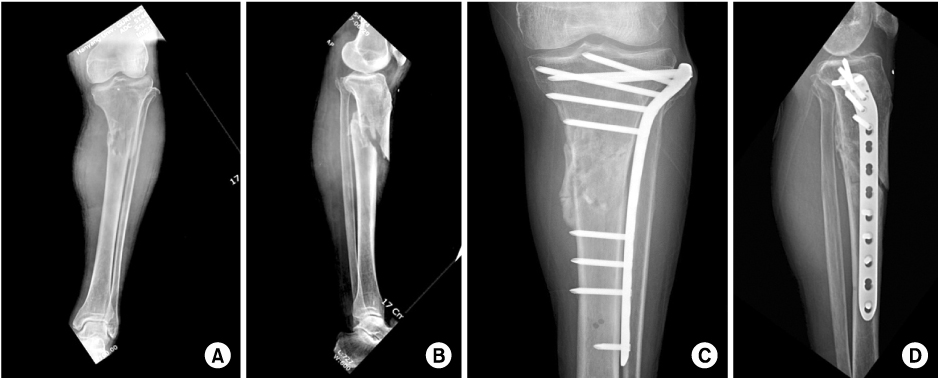
Fig. 2
(A, B, C) A 69-year-old man with severe communited, open proximal tibial fracture by traffic acident.
(D) Clinical photograph after application of external fixator.
(E) Follow-up radiograph after 16 weeks shows metal failure.
(F, G) The dual plating was performed after removal of internal devices.
(H, I) Bone union with satisfactory functional results was achieved at 6 months after second operation.
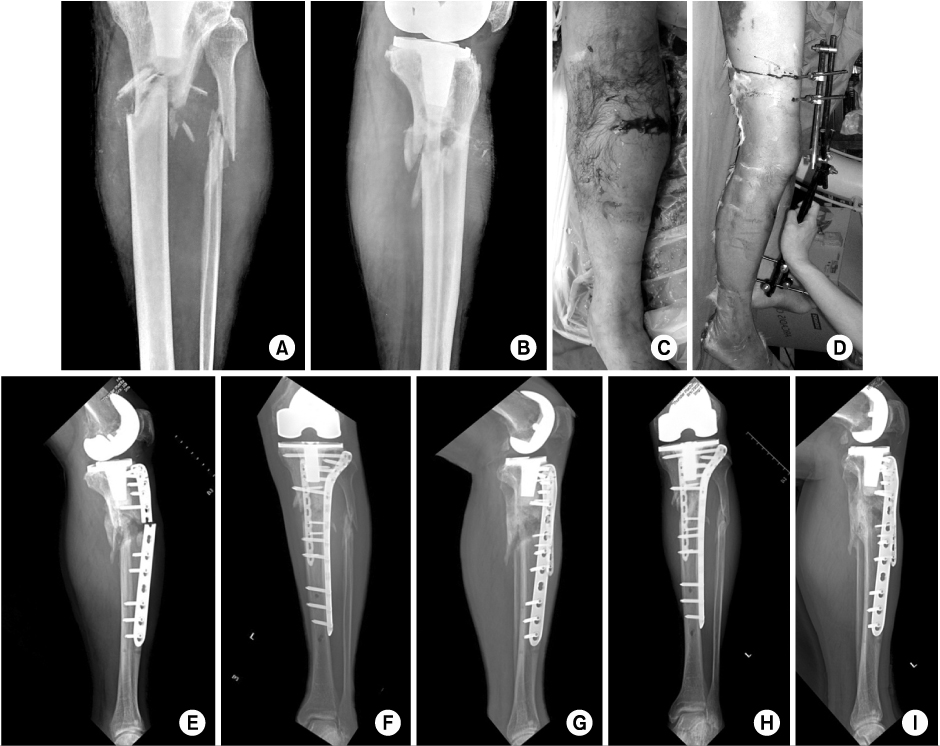
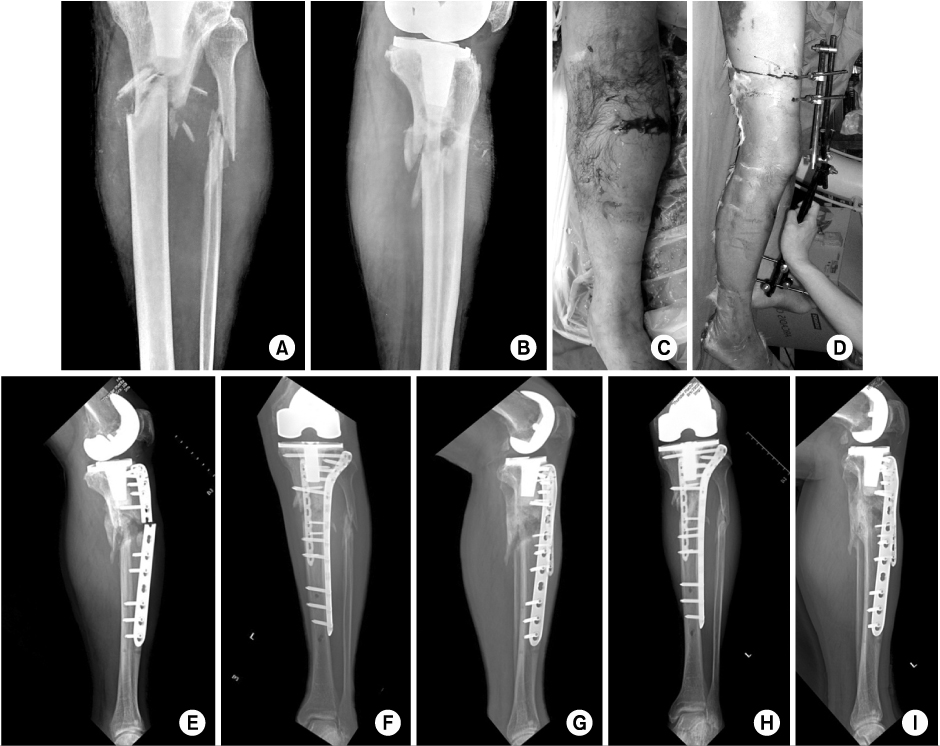
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Medial Minimally Invasive Percutaneous Plate Osteosynthesis in Proximal Tibial Comminuted Fractures
Jae-Ang Sim, Kwang-Hui Kim, Yong-Seuk Lee, Sang-Jin Lee, Beom-Koo Lee
Journal of the Korean Orthopaedic Association.2014; 49(4): 278. CrossRef - Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures - Technical Note -
Jae Ang Sim, Beom Koo Lee, Kwang Hui Kim, Yong Seuk Lee
Journal of the Korean Fracture Society.2013; 26(4): 327. CrossRef
Minimally Invasive Plate Osteosynthesis for Proximal Tibial Shaft Fracture
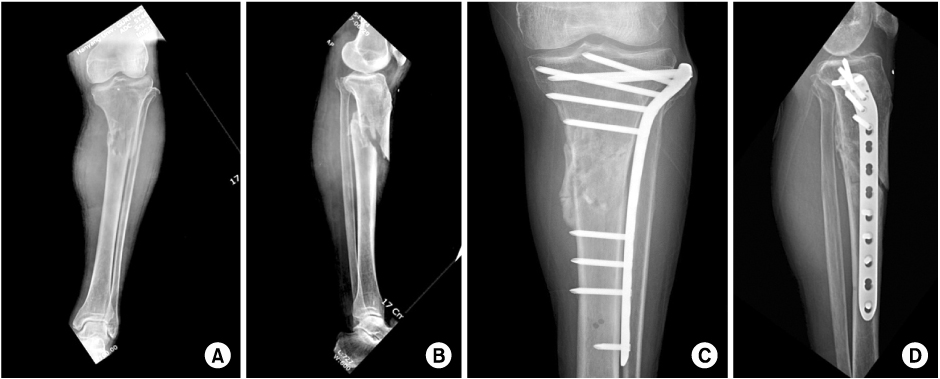
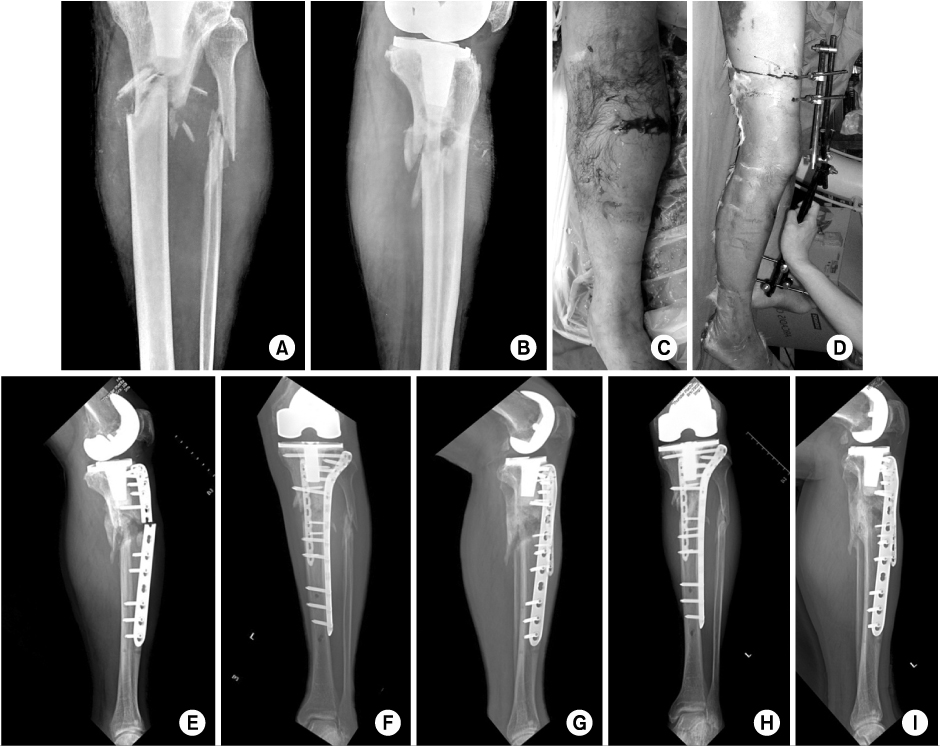
Fig. 1
(A, B) A 68-year old man with severe communited proximal tibial fracture.
(C, D) The fracture was healed 20 weeks after surgery.
Fig. 2
(A, B, C) A 69-year-old man with severe communited, open proximal tibial fracture by traffic acident.
(D) Clinical photograph after application of external fixator.
(E) Follow-up radiograph after 16 weeks shows metal failure.
(F, G) The dual plating was performed after removal of internal devices.
(H, I) Bone union with satisfactory functional results was achieved at 6 months after second operation.
Fig. 1
Fig. 2
Minimally Invasive Plate Osteosynthesis for Proximal Tibial Shaft Fracture

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

