Most cited articles
- Page Path
- HOME > Browse articles > Most cited articles
Most-cited are based on citations from 2024 ~ 2026.
Review Article
- Fracture-related infections: a comprehensive review of diagnosis and prevention
- HoeJeong Chung, Hoon-Sang Sohn
- J Musculoskelet Trauma 2025;38(2):86-95. Published online April 25, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00164
-
 Abstract
Abstract
 PDF
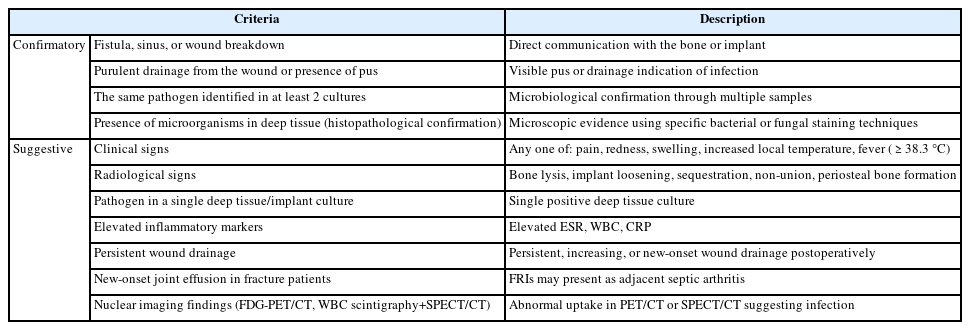
PDF - Fracture-related infections are challenging complications in orthopedic trauma that often require prolonged treatment and impose a significant healthcare burden. Accurate diagnosis and effective prevention strategies are essential for minimizing their occurrence. A recent international consensus has established standardized diagnostic criteria based on clinical, microbiological, radiological, and histopathological findings. Prevention is the top priority and involves a thorough preoperative risk assessment, along with glycemic control, nutritional optimization, and management of comorbidities, as well as intraoperative and postoperative measures such as appropriate antibiotic prophylaxis, surgical site antisepsis, and meticulous wound care. A multidisciplinary approach involving orthopedic surgeons, infectious disease specialists, and microbiologists is crucial for successfully reducing the burden of fracture-related infections.
-
Citations
Citations to this article as recorded by- Personalized Approaches to Diagnostic and Therapeutic Strategies in Periprosthetic Fracture-Related Infections (PFRIs): Case Series and Literature Review
Marianna Faggiani, Marco Zugnoni, Matteo Olivero, Salvatore Risitano, Giuseppe Malizia, Silvia Scabini, Marcello Capella, Stefano Artiaco, Simone Sanfilippo, Alessandro Massè
Journal of Personalized Medicine.2025; 15(12): 576. CrossRef - Pathogen-Specific Risk for Iterative Surgical Debridement in Orthopedic Infections: A Prospective Multicohort Analysis
Flamur Zendeli, Anna Jędrusik, Raymond O. Schaefer, David Albrecht, Michael Betz, Felix W. A. Waibel, Tanja Gröber, Nathalie Kühne, Sören Könneker, İlker Uçkay
Journal of Clinical Medicine.2025; 14(24): 8750. CrossRef
- Personalized Approaches to Diagnostic and Therapeutic Strategies in Periprosthetic Fracture-Related Infections (PFRIs): Case Series and Literature Review
- 6,195 View
- 234 Download
- 2 Crossref

Original Article
- Does the Operator’s Experience Affect the Occurrence of Complications after Distal Radius Fracture Volar Locking Plate Fixation? A Comparative Study of the First Four Years and Thereafter
- Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
- J Musculoskelet Trauma 2024;37(4):175-183. Published online October 25, 2024
- DOI: https://doi.org/10.12671/jmt.2024.37.4.175
- Correction in: J Musculoskelet Trauma 2025;38(1):40
-
 Abstract
Abstract
 PDF
PDF - Purpose
The management of distal radius fractures (DRFs) has evolved with the introduction of volar locking plate (VLP) fixation, offering stable fixation and better outcomes. Nevertheless, the impact of the surgeon’s experience on the complication rates in VLP fixation remains to be determined, particularly for less-experienced surgeons. This study compared the complication rates during the initial four years and subsequent two years of a hand surgeon’s practice of VLP fixation for DRFs.
Materials and Methods
The data between March 2016 and December 2022 were analyzed retrospectively under the Institutional Review Board approval. A single surgeon performed all VLP fixation surgeries after finishing regular hand surgery training, with the first four years representing the less experienced phase (Group 1) and the following two years indicating the experienced phase (Group 2). The patients’ characteristics, operation-related factors, and postoperative complications, including tendon injuries, nerve-related complications, fixation and instrument-related issues, osteosynthesis-related problems, and infections, were compared. In addition, the authors compared the data with a large multicenter study conducted by experienced hand surgeons.
Results
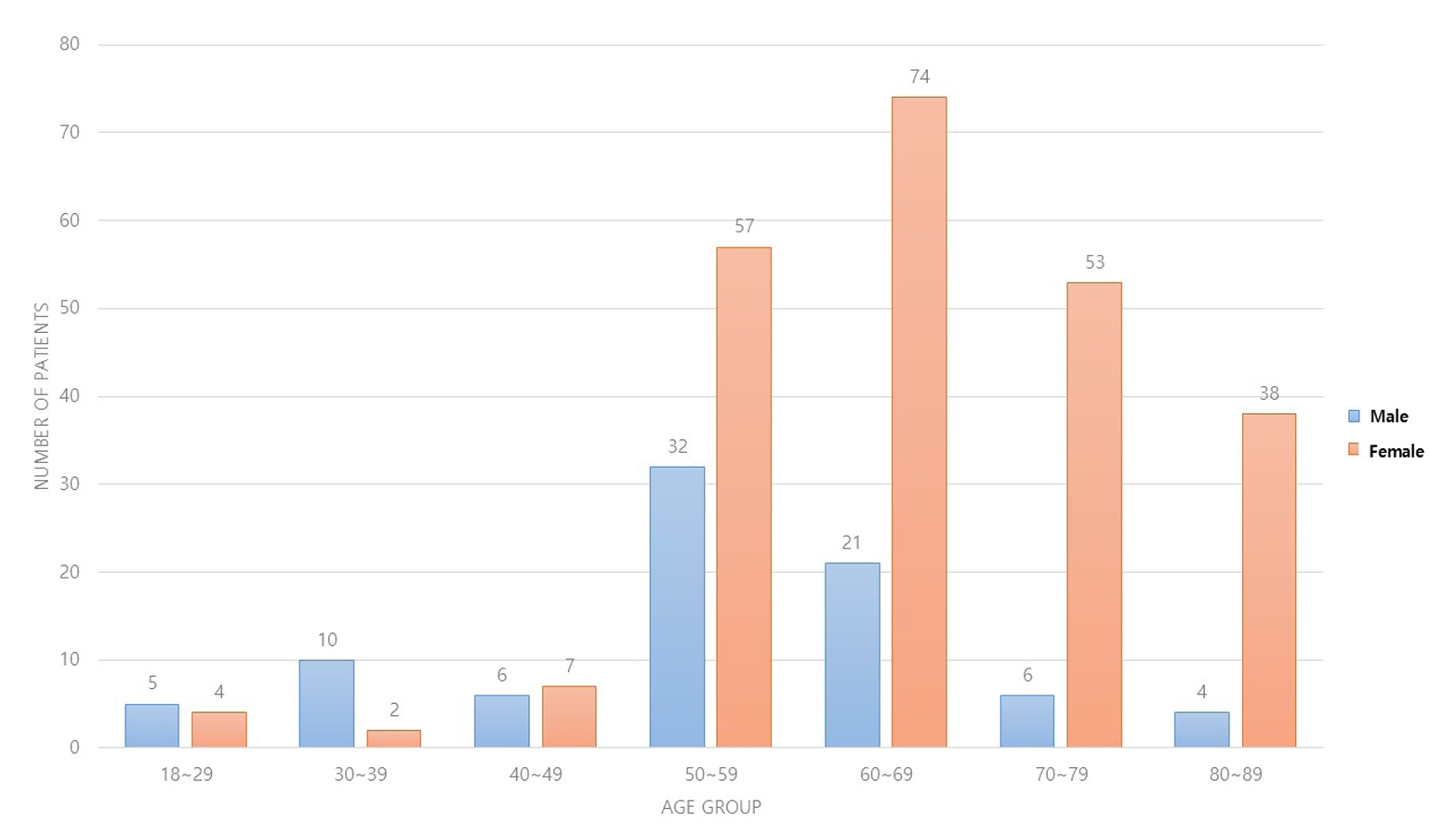
Three hundred and nineteen patients (321 wrists) were included. The mean age was 63.3 years, and 26.3% were male and 73.7% were female. The operation time was 53.7±14.5 minutes and 74.4±26.5 minutes in groups 1 and 2, respectively, which was statistically significantly shorter (p<0.001). The complication rates between the two groups were similar, except for the higher implant removal rates in Group 1. A comparison with a previous multicenter study revealed higher reduction losses and carpal tunnel syndrome in this study, but the overall complication rate was low.
Conclusion
In DRF management, when the operating surgeon has completed an accredited training course, VLP fixation is a good treatment method that can be performed effectively even by less experienced surgeons with low complication rates. -
Citations
Citations to this article as recorded by- Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2025; 38(1): 40. CrossRef - Characteristics of patients with distal radius fracture requiring arthroscopic foveal repair after bone union
Min Jung Park, Cheungsoo Ha, Hyun Tak Kang, Yong Hyun Yoon, Jun-Ku Lee, Soo-Hong Han
Arthroscopy and Orthopedic Sports Medicine.2025; 12(2): 70. CrossRef
- Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
- 2,559 View
- 53 Download
- 2 Crossref

Review Articles
- Treatment of avulsion fractures around the knee
- Jeong-Hyun Koh, Hyung Keun Song, Won-Tae Cho, Seungyeob Sakong, Sumin Lim
- J Musculoskelet Trauma 2025;38(2):63-73. Published online March 31, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00073

-
 Abstract
Abstract
 PDF
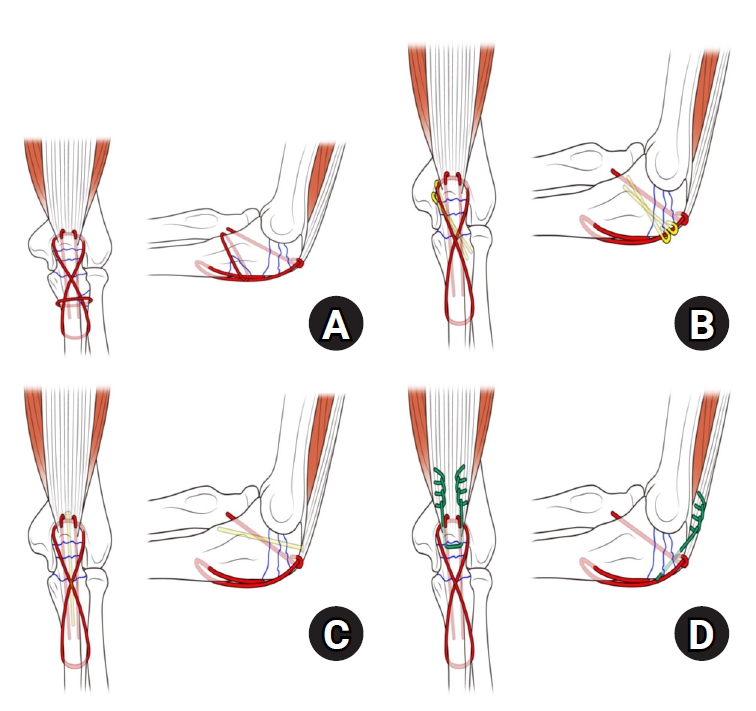
PDF - Avulsion fractures of the knee occur when tensile forces cause a bone fragment to separate at the site of soft tissue attachment. These injuries, which frequently affect adolescent athletes, can involve the cruciate and collateral ligaments, arcuate complex, iliotibial band, and patellar and quadriceps tendons. Radiographs aid in the initial diagnosis, while computed tomography and magnetic resonance imaging facilitate a comprehensive evaluation of injury severity and concomitant damage. Specific avulsion fracture types include: anterior cruciate ligament avulsions (tibial site, Meyers and McKeever classification), posterior cruciate ligament avulsions (tibial attachment, Griffith's classification), Segond fractures (anterolateral complex injury), iliotibial band avulsions, medial collateral ligament avulsions (reverse Segond, Stieda fractures), arcuate complex avulsions ("arcuate sign"), medial patellofemoral avulsions (patellar dislocations), and patellar/quadriceps tendon avulsions. The treatment depends on the fracture location, displacement, and associated injuries. Non-displaced fractures can be managed conservatively, while displaced fractures or those with instability require surgical reduction and fixation. Prompt recognition and appropriate intervention prevent complications such as deformity, nonunion, malunion, and residual instability. This review provides an overview of the pathogenesis, diagnosis, and management of knee avulsion fractures to guide clinical decision-making.
-
Citations
Citations to this article as recorded by- Lateral marginal fractures of the patella and patellofemoral pain
Jae-Ang Sim, Chul-Ho Kim, Ji Wan Kim
Journal of Musculoskeletal Trauma.2025; 38(3): 152. CrossRef
- Lateral marginal fractures of the patella and patellofemoral pain
- 16,407 View
- 180 Download
- 1 Crossref

- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
- Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(2):74-85. Published online March 31, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00024

-
 Abstract
Abstract
 PDF
PDF - Distal tibial metaphyseal fractures are commonly caused by high-energy injuries in young men and osteoporosis in older women. These fractures should be clearly distinguished from high-energy pilon fractures. Although the optimal surgical intervention methods for distal tibial metaphyseal fractures remain uncertain and challenging, surgical treatments for nonarticular distal tibia fractures can be broadly divided into two types: plate fixation and intramedullary nail (IMN) fixation. Once functional reduction is achieved using an appropriate technique, distal tibial nailing might be slightly superior to plate fixation in reducing postoperative complications. Thus, the surgical strategy should focus on functional realignment and proceed in the following sequence: (1) restoring the original tibial length, regardless of whether fibular fixation is to be done; (2) making the optimal entry point through an anteroposterior (AP) projection based on the overlapping point between the fibular tip and lateral plateau margin; (3) placing Kirschner wires (Ø2.4 mm) as blocking pins (in the AP orientation for coronal control and in the mediolateral [ML] orientation for sagittal control) as close to the upper locking hole as possible without causing further comminution on the concave aspect of the short fragment; and (4) making the the distal fixation construct with at least two ML and one AP interlocking screw or two ML interlocking screws and blocking screws. After the IMN is adequately locked, blocking pins (Ø2.4 mm) need to be replaced by a 3.5 mm screw.
-
Citations
Citations to this article as recorded by- Impact of Foot Width on Patient-Reported Outcomes Assessed by 3-Dimensional Foot Morphometry in Hallux Valgus
Jungtae Ahn, Dae-Cheol Nam, Gu-Hee Jung
Clinics in Orthopedic Surgery.2025; 17(6): 1062. CrossRef
- Impact of Foot Width on Patient-Reported Outcomes Assessed by 3-Dimensional Foot Morphometry in Hallux Valgus
- 2,649 View
- 50 Download
- 1 Crossref

- Atypical femoral fractures: an update
- Won-Tae Cho, Jeong-Hyun Koh, Seungyeob Sakong, Jung-Taek Kim
- J Musculoskelet Trauma 2025;38(2):41-52. Published online March 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00031
-
 Abstract
Abstract
 PDF
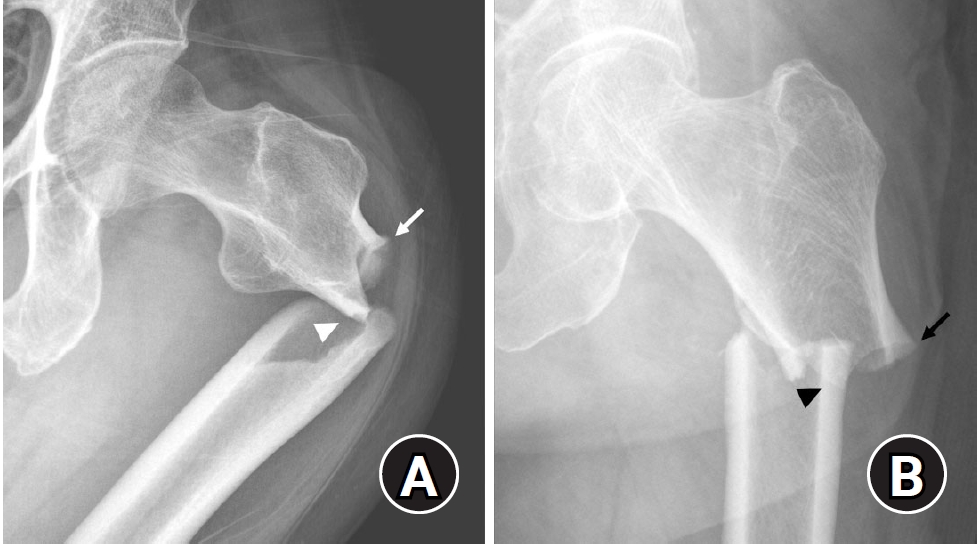
PDF - This narrative review provides an up-to-date overview of atypical femoral fractures (AFFs), emphasizing diagnostic criteria, epidemiology, pathophysiology, risk factors, and evaluation with screening strategies. AFFs are rare but significant complications associated with prolonged bisphosphonate (BP) therapy for osteoporosis. Although the pathogenesis of AFFs has not been fully elucidated, its primary mechanism is thought to involve impaired bone remodeling, leading to unhealed microfractures that progress to stress fractures under repetitive loading. AFFs can occur in various regions of the femur, influenced by femoral geometry and the lower limb axis. Other risk factors include prolonged steroid use, arthroplasty, genetic predispositions, and metabolic bone disorders. The diagnosis of AFFs is based on criteria established by the American Society for Bone and Mineral Research. Key radiographic features include lateral cortical transverse fracture lines and localized cortical thickening, typically with minimal or no comminution on the medial cortex. Dual-energy X-ray absorptiometry for screening tests and magnetic resonance imaging as an advanced imaging modality enable the early detection of incomplete fractures. This multi-modal approach facilitates the prompt identification of prodromal cortical changes, reducing the risk of complete fractures in high-risk populations, particularly patients undergoing prolonged BP therapy. Level of Evidence: V
-
Citations
Citations to this article as recorded by- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
Lorenzo Lucchetta, Carmelinda Ruggiero, Samuele Berardi, Alice Franceschi, Michele Bisaccia, Giuseppe Rinonapoli
Journal of Clinical Medicine.2025; 15(1): 25. CrossRef
- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
- 13,151 View
- 376 Download
- 1 Crossref

Original Articles
- Comparison of outcomes of reinforced tension band wiring and precontoured plate and screw fixation in the management of Mayo type IIIB olecranon fractures
- Hyun Goo Kang, Tong Joo Lee, Samuel Jaeyoon Won
- J Musculoskelet Trauma 2025;38(2):96-101. Published online February 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00059
- Correction in: J Musculoskelet Trauma 2025;38(3):168
-
 Abstract
Abstract
 PDF
PDF - Background
Mayo type IIIB olecranon fractures are characterized by significant displacement and comminution, presenting a challenge in selecting the appropriate fixation technique. This study compared the clinical and radiographic outcomes, complications, and reoperation rates of reinforced tension band wiring (TBW) and precontoured plate and screw fixation (PF) in the surgical treatment of Mayo type IIIB olecranon fractures.
Methods
This retrospective review analyzed 24 patients diagnosed with Mayo type IIIB olecranon fractures, who were treated between 2005 and 2023. Of these, 11 patients underwent reinforced TBW, and 13 received precontoured PF. Clinical outcomes were assessed using Disabilities of the Arm, Shoulder, and Hand (DASH) scores and the Mayo Elbow Performance Score (MEPS). Radiographic outcomes focused on fracture union. Operative times, complication rates, and reoperation rates were compared between the groups.
Results
Both the reinforced TBW and PF groups achieved satisfactory clinical outcomes, with no significant between-group differences in DASH and MEPS scores (P>0.05). Radiographic union was achieved in all patients. The reinforced TBW group demonstrated a significantly shorter operative time than the PF group (93.6±7.4 min vs. 132.3±13.7 min; P<0.001). Complication rates were similar between the two groups (reinforced TBW, 38.4%; PF, 36.3%), but hardware-related irritation occurred more frequently in the reinforced TBW group. Reoperations were required in 15.8% of the reinforced TBW group due to hardware irritation, whereas no reoperations were necessary in the PF group.
Conclusions
Reinforced TBW and PF are both effective surgical options for managing Mayo type IIIB olecranon fractures, yielding comparable clinical and radiographic outcomes. While reinforced TBW offers shorter operative times and lower costs, PF is associated with fewer hardware-related complications. Further prospective studies are needed to optimize treatment strategies for these complex fractures. Level of Evidence: Level III. -
Citations
Citations to this article as recorded by- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
Reva Qiu, Mallika Makkar, Richard Buckley
Injury.2025; 56(11): 112769. CrossRef
- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
- 2,127 View
- 49 Download
- 1 Crossref

- Clinical Outcomes of Triple Tension Band Wirings in Comminuted Patellar Fracture: A Comparison with Conventional Tension Band Wiring
- Hyun-Cheol Oh, Han-Kook Yoon, Joong-Won Ha, Sang Hoon Park, Sungwoo Lee
- J Korean Fract Soc 2024;37(2):82-86. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.82
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study devised triple tension band wirings (TTBW) fixation in patients with comminuted patella fractures to compare the clinical result of TTBW with that of tension band wiring (TBW).
Materials and Methods
This study was conducted on 91 patients who had undergone surgery diagnosed with acute patella fracture from January 2011 to December 2016. The study included 51 double TBW patients (Group 1) and 40 patients with TTBW (Group 2).
Results
Five out of 51 cases had a loss of reduction and fixation failure in Group 1, and no failure of fracture formation healing occurred in Group 2. Nonunion was noted in one case in Group 1 and no case in Group 2. Eight K-wire migration cases were observed in Group 1, which was not observed in Group 2. Six patients in Group 1 underwent revisional surgery. No patients in Group 2 had a reoperation. As a result of a one-year follow-up after the operation, the mean range of motion of the knee joint in groups 1 and 2 was 128.3°±11.3° and 127.9°±10.8°, respectively. The Lysholm’s scores for groups 1 and 2 were 90.8±4.2 and 90.3±3.8 points, respectively, which was not statistically significant.
Conclusion
TTBW is a helpful technique for the surgical treatment of comminuted patella fractures. The TTBW method has less reoperation due to nonunion and fixation failure. After a one-year followup, the clinical results were similar to the conventional TBW method. -
Citations
Citations to this article as recorded by- Lateral marginal fractures of the patella and patellofemoral pain
Jae-Ang Sim, Chul-Ho Kim, Ji Wan Kim
Journal of Musculoskeletal Trauma.2025; 38(3): 152. CrossRef
- Lateral marginal fractures of the patella and patellofemoral pain
- 762 View
- 6 Download
- 1 Crossref

- Biomechanical Investigation to Establish Stable Fixation Strategies for Distal Tibial Fractures in Various Situations: Finite Element Analysis Studies
- Sung Hun Yang, Jun Young Lee, Gu-Hee Jung, Hyoung Tae Kim, Ba Woo Ko
- J Korean Fract Soc 2024;37(2):71-81. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.71
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the structural and mechanical stability as well as the clinical significance of various fixation constructs for distal tibial fractures using finite element analysis.
Materials and Methods
Fracture models with 20 mm and 120 mm defects were produced, and implants of an intramedullary nail and anatomical plate model were applied. An axial load of 800 N with 60% distribution in the medial compartment and 40% in the lateral compartment was applied and analyzed using Ansys ® software.
Results
In the intramedullary nail model, the maximum von Mises stress occurred at the primary lag screw hole and adjacent medial cortex, while in the plate model, it occurred at the locking holes around the fracture. The maximum shear stress on the bone and metal implant in the fracture model with a 20 mm defect was highest in the plate assembly model, and in the fracture model with a 120 mm defect, it was highest in the two-lag screw assembly model.
Conclusion
Based on an analysis of the maximum shear stress distribution, securing the fixation strength of the primary lag screw hole is crucial, and the assembly model of the intramedullary nail with two lag screws and a blocking screw applied was the model that best withstood the optimal load. Securing the locking hole directly above the fracture is believed to provide the maximum fixation strength because the maximum pressure in the plate model is concentrated in the proximal locking hole and the surrounding cortex. -
Citations
Citations to this article as recorded by- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
Journal of Musculoskeletal Trauma.2025; 38(2): 74. CrossRef
- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
- 893 View
- 19 Download
- 1 Crossref

- Prediction of Syndesmotic Instability according to the Lateral Malleolus Fracture Pattern in Supination-External Rotation Type Ankle Fractures: Short Oblique versus Long Oblique Fracture
- Chan-Jin Park, Min-Su Lee, Keun-Bae Lee
- J Korean Fract Soc 2024;37(1):39-45. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.39
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined whether preoperative radiological evaluations can predict syndesmotic instability according to the lateral malleolus fracture pattern in supination-external rotation-type ankle fractures.
Materials and Methods
This study enrolled 132 patients (132 ankles) with supination-external rotation stage 3 and 4 ankle fractures. Three-dimensional computed tomography was used for the morphological classification of the lateral malleolus fractures. A long oblique fracture was defined when the posterior cortical bone height of the fracture was 4.5 cm or more from the plafond of the distal tibial articular surface. A short oblique fracture was defined when the height was less than 4.5 cm. The demographic characteristics and syndesmotic instability of the two groups were evaluated.
Results
Short oblique fractures were confirmed in 102 cases, and long oblique fractures were confirmed in 30 cases. Long oblique fractures occurred at a statistically significantly higher incidence in younger ages and among males compared to short oblique fractures. Syndesmotic instability was more common in long oblique fractures.
Conclusion
In supination-external rotation-type ankle fractures, syndesmotic instability was observed in approximately 13%. Specifically, when the fracture pattern of the lateral malleolus is long oblique, the incidence of syndesmotic instability is approximately three times higher than in short oblique fractures. Therefore, meticulous evaluations of the lateral malleolus fracture pattern and establishing an appropriate treatment plan before surgery are crucial. -
Citations
Citations to this article as recorded by- Relationship of lateral malleolar fracture patterns to posterior malleolar fracture morphology in supination-external rotation ankle fractures in Korea: a retrospective cohort stduy
Jong-Eun Kim, Chan-Jin Park, Jun-Young Lee, Keun-Bae Lee, Gun-Woo Lee
Journal of Musculoskeletal Trauma.2025; 38(4): 212. CrossRef
- Relationship of lateral malleolar fracture patterns to posterior malleolar fracture morphology in supination-external rotation ankle fractures in Korea: a retrospective cohort stduy
- 580 View
- 10 Download
- 1 Crossref

- Triplane Fracture Management: Prediction of Periosteal Entrapment and the Need for Open Reduction by Measurements of the Physeal Fracture Gap in Preoperative Computed Tomography Scans
- Dae Hee Lee, Joo Han Kwon, Jae Uk Jung
- J Korean Fract Soc 2024;37(1):1-7. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study measured the physeal fracture gap on preoperative ankle computed tomography (CT) to predict the periosteal entrapment that requires an open reduction in distal tibia triplane fractures.
Materials and Methods
This study retrospectively reviewed patients who had undergone internal fixation for a triplane fracture from April 2004 to September 2022. The demographic data, including age,body mass index, and past medical history, were analyzed. In the radiographic evaluations, ankle CT and ankle simple radiographs, including anteroposterior (AP), lateral, and mortise views, were taken preoperatively. Postoperatively, simple ankle radiographs were obtained periodically, including AP, mortise, and lateral views. The physeal fracture gap was measured on ankle CT, and the larger gap between the coronal and sagittal view of CT was selected. The residual physeal gap <2 mm was considered an adequate reduction.
Results
Of 17 cases, three demonstrated successful reduction using closed reduction techniques. Periosteal entrapment was observed in 14 cases open reduction cases. In all three closed reduction cases, the physeal gap estimated on preoperative ankle CT was under 3 mm with a mean gap of 2.4±0.2 mm (range, 2.1-2.5 mm). In the remaining 14 open reduction cases, the measured physeal gap was over 3 mm, averaging 5.0±2.7 mm (range, 3.1-12.2 mm). There was a significant difference in the preoperative physeal gap between the two groups (p<0.01). Overall, good reduction was achieved in all 17 cases; the postoperative physeal gap was under 2 mm with a mean of 1.0±0.5 mm (closed reduction group, 0.5±0.2 mm; open reduction group, 1.1±0.5 mm).
Conclusion
Open reduction is strongly recommended for triplane fractures with a physeal fracture gap of 3 mm or more in preoperative ankle CT, suggesting the possibility of an entrapped periosteum in the fracture gap. -
Citations
Citations to this article as recorded by- Diagnostic values of radiographic indices for predicting periosteal entrapment in pediatric proximal phalangeal base physeal fractures of toes
Ho Young Park, Jeong-Seok Moon, Kiwook Kim
Skeletal Radiology.2026; 55(1): 97. CrossRef
- Diagnostic values of radiographic indices for predicting periosteal entrapment in pediatric proximal phalangeal base physeal fractures of toes
- 1,294 View
- 20 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


