Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(4); 2020 > Article
- Original Article Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
- Se Jin Kim, Hong Man Cho, Jiyeon Park, Ki Yong An, Young Woo Chung, Woojin Shin
-
Journal of Musculoskeletal Trauma 2020;33(4):179-188.
DOI: https://doi.org/10.12671/jkfs.2020.33.4.179
Published online: October 31, 2020
2Department of Orthopedic Surgery, Gwangju Veterans Hospital, Gwangju, Korea
- 790 Views
- 3 Download
- 1 Crossref
- 0 Scopus
Abstract
Purpose
Intertrochanteric fractures can be treated using proximal femoral nail antirotation (PFNA). This study examined the clinical and radiological results of the intraoperative fracture compression.
Materials and Methods
Ninety-four patients underwent intraoperative compression (Group I), and 88 patients underwent natural sliding only (Group II). The patients were followed-up for more than two years. All patients met the following seven conditions: (1) AO/OTA 31-A1, A2 type intertrochanter fracture, (2) availability of compression of more than one cortical bone in the anterior or medial region of the fracture site under the preoperative imaging test, (3) Singh index grade ≥3, (4) blade position: center-center, center-inferior, (5) tip-apex distance <25 mm, (6) reduction status of good or very good, and (7) positive or neutral medial cortical support position with slightly valgus reduction.
Results
A slight tendency toward significant differences in acute phase pain between the two groups was observed at six weeks postoperatively (p=0.073). Twenty-four months after surgery, lateral extension of the PFNA helical blade between the two groups showed significant differences (p=0.017). Fracture gaps measured immediately after surgery showed significant differences (p=0.001), and a clear tendency for a significant difference in the average fracture union time was found (p=0.065).
Conclusion
Intraoperative fracture compression, intraoperative fracture compression appears beneficial to achieve a successful union of trochanteric fractures provided that all conditions are met to apply the method safely.
Published online Oct 22, 2020.
https://doi.org/10.12671/jkfs.2020.33.4.179
Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
 , M.D.,
Hong Man Cho
, M.D.,
Hong Man Cho , M.D.,*
Jiyeon Park
, M.D.,*
Jiyeon Park , M.D.,*
Ki Yong An
, M.D.,*
Ki Yong An , M.D.,*
Young Woo Chung
, M.D.,*
Young Woo Chung , M.D.,*
and Woojin Shin
, M.D.,*
and Woojin Shin , M.D.*
, M.D.*
Abstract
Purpose
Intertrochanteric fractures can be treated using proximal femoral nail antirotation (PFNA). This study examined the clinical and radiological results of the intraoperative fracture compression.
Materials and Methods
Ninety-four patients underwent intraoperative compression (Group I), and 88 patients underwent natural sliding only (Group II). The patients were followed-up for more than two years. All patients met the following seven conditions: (1) AO/OTA 31-A1, A2 type intertrochanter fracture, (2) availability of compression of more than one cortical bone in the anterior or medial region of the fracture site under the preoperative imaging test, (3) Singh index grade ≥3, (4) blade position: center-center, center-inferior, (5) tip-apex distance <25 mm, (6) reduction status of good or very good, and (7) positive or neutral medial cortical support position with slightly valgus reduction.
Results
A slight tendency toward significant differences in acute phase pain between the two groups was observed at six weeks postoperatively (p=0.073). Twenty-four months after surgery, lateral extension of the PFNA helical blade between the two groups showed significant differences (p=0.017). Fracture gaps measured immediately after surgery showed significant differences (p=0.001), and a clear tendency for a significant difference in the average fracture union time was found (p=0.065).
Conclusion
Intraoperative fracture compression, intraoperative fracture compression appears beneficial to achieve a successful union of trochanteric fractures provided that all conditions are met to apply the method safely.
Fig. 1
(A, B) True reamer head and blade diameter was measured in two ways using a ruler and calipers. The tip apex distance (TAD) was calculated using the intraoperative image intensifier films. The measured anteroposterior (AP) and lateral radiograph distances were combined to calculate the measured TAD. (C) Intraoperative image intensifier shows AP and lateral radiograph after reaming. To calculate the TAD, XAP is the distance from the tip of the reamer to the apex of the femoral head in the AP image, and XLAT is the distance in the translateral image. (D) Intraoperative image intensifier shows AP and lateral radiographs of the inserted blade before locking. The TAD was calculated using the same method. (E) Radiographs show the AP and lateral images of the inserted blade after locking. The TAD was calculated using the same method. (F) Radiograph shows an AP image after locking the blade and removing the impactor. The image shows that the lateral extension of the blade is small.
Fig. 2
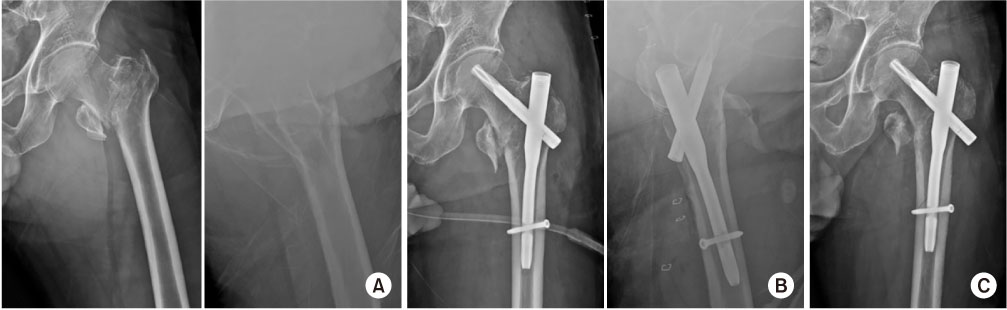
Radiographs of a 73-year-old female patient with AO/OTA 31-A2 trochanteric fracture treated with proximal femoral nail antirotation. (A) Preoperative hip anteroposterior and translateral radiographs suggesting a right trochanteric femoral fracture AO/OTA 31-A2. (B) Intraoperative radiograph under fluoroscopy before intraoperative fracture compression. (C) After intraoperative fracture compression, intraoperative radiograph under fluoroscopy, showing a reduction of the fracture gap.
Fig. 3
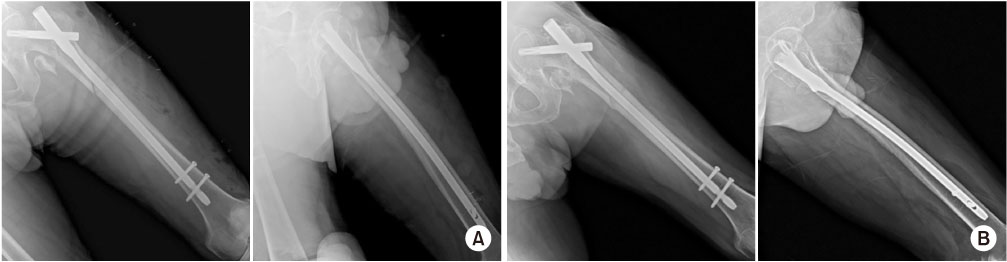
(A) Immediate postoperative hip anteroposterior (AP) and translateral (Lat) radiographs showing a good reduction state. The blade position was within the center-inferior tip apex distance of 25 mm. (B) Complete union was achieved in the follow-up hip AP and Lat radiographs four months after the operation.
Fig. 4
Radiograph of a 70-year-old male patient with AO/OTA 31-A2 trochanteric fracture treated with proximal femoral nail antirotation. (A) Preoperative hip anteroposterior (AP) and translateral (Lat) radiographs, suggesting a left trochanteric femoral fracture AO/OTA 31-A2. (B) Immediate postoperative hip AP and Lat radiographs showing a good reduction state. (C) Non-displaced fracture was found around the distal screw at five months after the operation due to falling from a ladder.
Fig. 5
(A) Immediate postoperative hip anteroposterior and lateral radiographs after revision with a longer nail showing a good reduction state. (B) Complete union was achieved in the follow-up radiograph at four months after revision surgery.
Table 1
Demographic Data of Group I and Group II
Table 2
Perioperative Results and Complications in Group I and Group II
Table 3
Clinical Results in Group I and Group II
Table 4
Radiological Results and Complications in Group I and Group II
Financial support:None.
Conflict of interests:None.
References
-
Wild M, Jungbluth P, Thelen S, et al. The dynamics of proximal femoral nails: a clinical comparison between PFNA and Targon PF. Orthopedics 33;2010 [doi: 10.3928/01477447-2010062504]
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS








 Cite
Cite

