Search
- Page Path
- HOME > Search
Original Article
- Three-dimensional computed tomography-based differentiation of engaged versus displaced intertrochanteric fractures using the anterior fracture line: a cross-sectional study from Korea
- Jae-Suk Chang, Jin Yeob Park, Sang-Ok Chun, Chul-Ho Kim
- J Musculoskelet Trauma 2026;39(1):30-37. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00318
-
 Abstract
Abstract
 PDF
PDF - Background
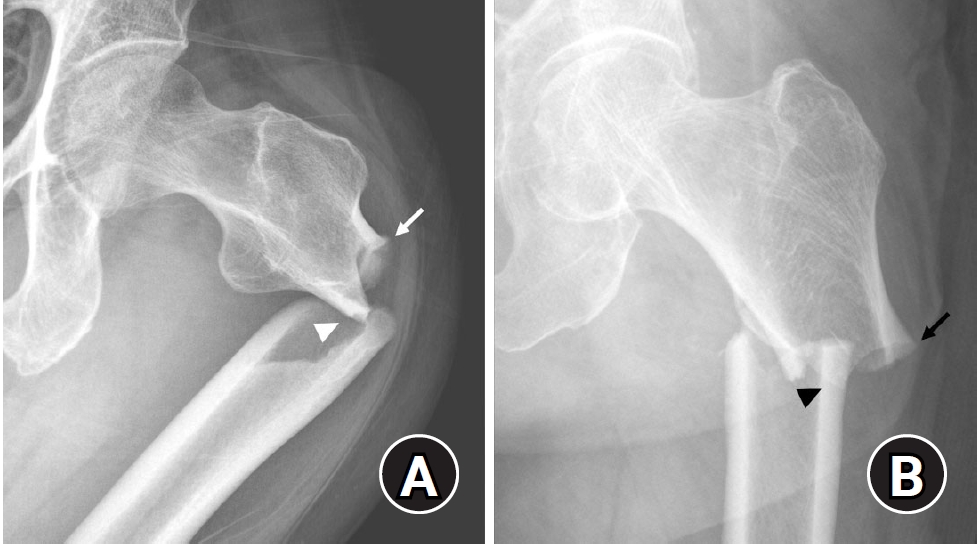
With the advent of an aging society, osteoporotic fractures—particularly hip fractures—are increasing, with a 1-year mortality rate of 17%. Achieving stable fixation that enables early ambulation is essential but remains challenging because complex intertrochanteric (IT) fracture patterns are often underestimated on plain radiographs. Using three-dimensional computed tomography (3D-CT), this study analyzed whether the anterior fracture line lies medial or lateral to the IT line and examined its relationship with displacement or distal medullary canal engagement, highlighting the potential influence of the joint capsule and capsular ligaments on fracture morphology and fixation stability.
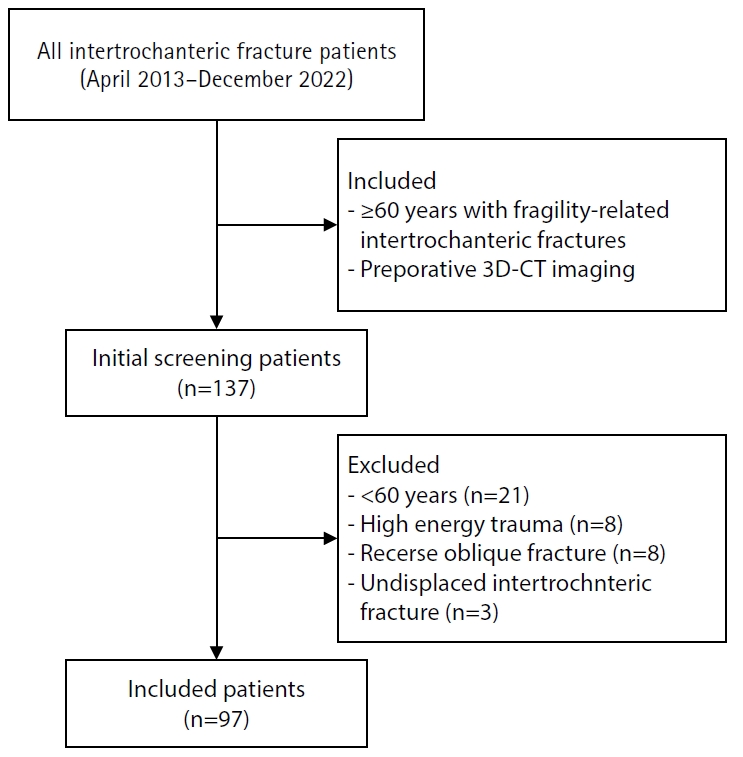
Methods
A retrospective review was conducted on 96 osteoporotic IT fractures in patients aged ≥60 years treated between April 2013 and December 2022 at National Police Hospital and Asan Medical Center, Seoul, Korea. Fractures were classified as engaged, completely displaced, and partially displaced based on 3D-CT findings. The anterior fracture-line position (medial or lateral to the IT line) and the status of the lesser trochanter (LT) were evaluated. The chi-square or Fisher exact test was used for statistical comparisons.
Results
In total, 96 patients were analyzed. Of these, 49 cases (51.0%) were classified as engaged type, 27 cases (28.1%) as completely displaced type, and 20 cases (20.8%) as partially displaced type. When comparing fracture pattern with anterior fracture-line position, the completely displaced type showed a significantly higher proportion of lateral anterior fracture lines than the other two types (P<0.001). However, no significant association was identified between fracture pattern and LT displacement. When the anterior fracture-line position and LT displacement were evaluated together, only the engaged type demonstrated a possible association between a lateral anterior fracture line and LT displacement, though the statistical significance was weak (P=0.047).
Conclusions
Fracture lines lateral to the IT line were strongly associated with displacement in IT fractures; however, their relationship with LT involvement, reflecting iliopsoas tendon traction, was not clearly demonstrated. Although the factors contributing to the engaged-type fracture remain uncertain, the statistical association between fracture pattern and anterior fracture-line position suggests that capsular structures may play a stabilizing role in select fracture configurations. Further studies are needed to clarify these anatomical interactions. Level of evidence:
- 113 View
- 4 Download

Review Article
- Complications of hand fractures: strategies for prevention and management
- Jong Woo Kang
- J Musculoskelet Trauma 2026;39(1):1-11. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00304
-
 Abstract
Abstract
 PDF
PDF - Various complications can occur after hand fractures. Among them, joint stiffness and malunion are the most common and significant complications, which are often accompanied by tendon adhesions and joint contracture. Careful evaluations of injury characteristics, such as fracture patterns, alignment, and soft tissue injury, are the first step to select appropriate management strategies and prevent complications of hand fractures. Close observation of its clinical prognosis is also essential for early detection and preemptive management of complications. Management of complications includes immobilization, rehabilitation, and various surgical techniques such as tenolysis or capsular release for joint stiffness, corrective osteotomy for malunion, and revisional fixation with bone graft for nonunion. The authors discuss prevention, early recognition, and management strategies for complications of hand fractures in this review.
- 206 View
- 9 Download

Original Articles
- Epidemiological changes and surgical trends of distal radius fractures in adults over 50 years during the COVID-19 pandemic in Korea: a nationwide repeated cross-sectional study
- Han-Kook Yoon, So Ra Yoon, Kee-Bum Hong, Youngsu Jung, SeongJu Choi, Jun-Ku Lee
- J Musculoskelet Trauma 2026;39(1):12-19. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00297
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The COVID-19 pandemic is likely to have affected bone health in older adults in Korea. This study aimed to analyze changes in the epidemiology and management of distal radius fractures (DRFs) in older adults before and during the COVID-19 pandemic.
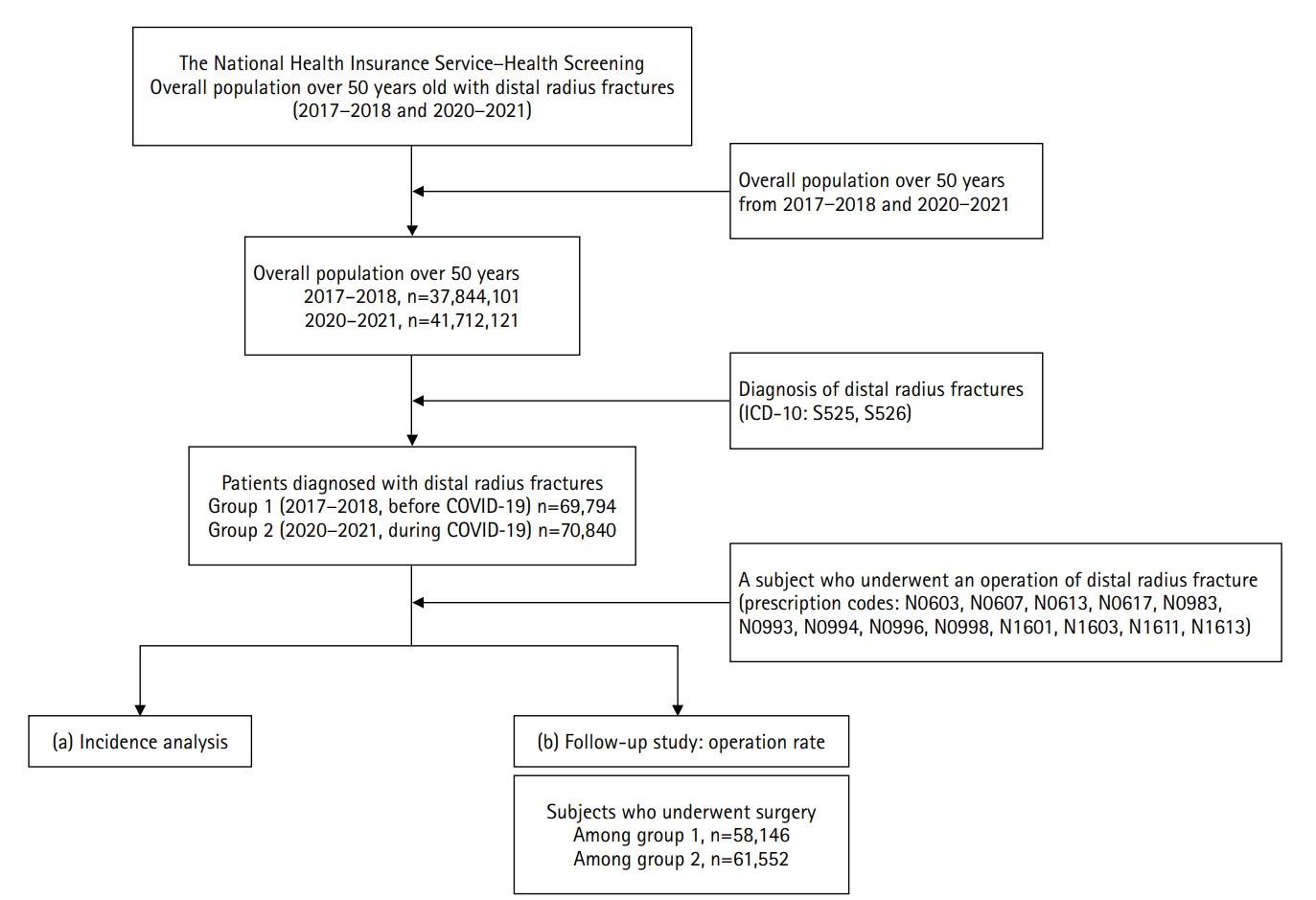
Methods
Patients with DRF aged over 50 years in 2017, 2018, 2020, and 2021 were included in this study. Patients were classified into a group with DRF occurring between 2017 and 2018 (before COVID-19) and a group with DRF occurring between 2020 and 2021 (during COVID-19). We calculated the incidence rates of DRF and compared them between the two groups. We also analyzed and compared demographic data (age, sex, income, residence) and the operation rate for DRF between the two groups. Patient selection and treatment were based on International Classification of Diseases, 10th revision codes.
Results
A total of 140,634 patients with DRF (before COVID-19, 69,794; during COVID-19, 70,840) were included. The incidence of DRF before COVID-19 (184.4/100,000 person-years) was higher than during COVID-19 (169.8/100,000 person-years). The operation rate was higher during COVID-19 (86.9%) than before COVID-19 (83.3%).
Conclusion
During the COVID-19 pandemic, the incidence of DRF decreased in South Korea. However, the rate of surgical treatment increased and exceeded the global surgical rate. Level of evidence: III.
- 168 View
- 4 Download

- Computed tomography plane reformatting to reduce projection error in measuring Pauwels angle of femoral neck fractures: a cross-sectional study
- Gyu Min Kong, Jae-Young Lim, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2026;39(1):38-47. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00038
-
 Abstract
Abstract
 PDF
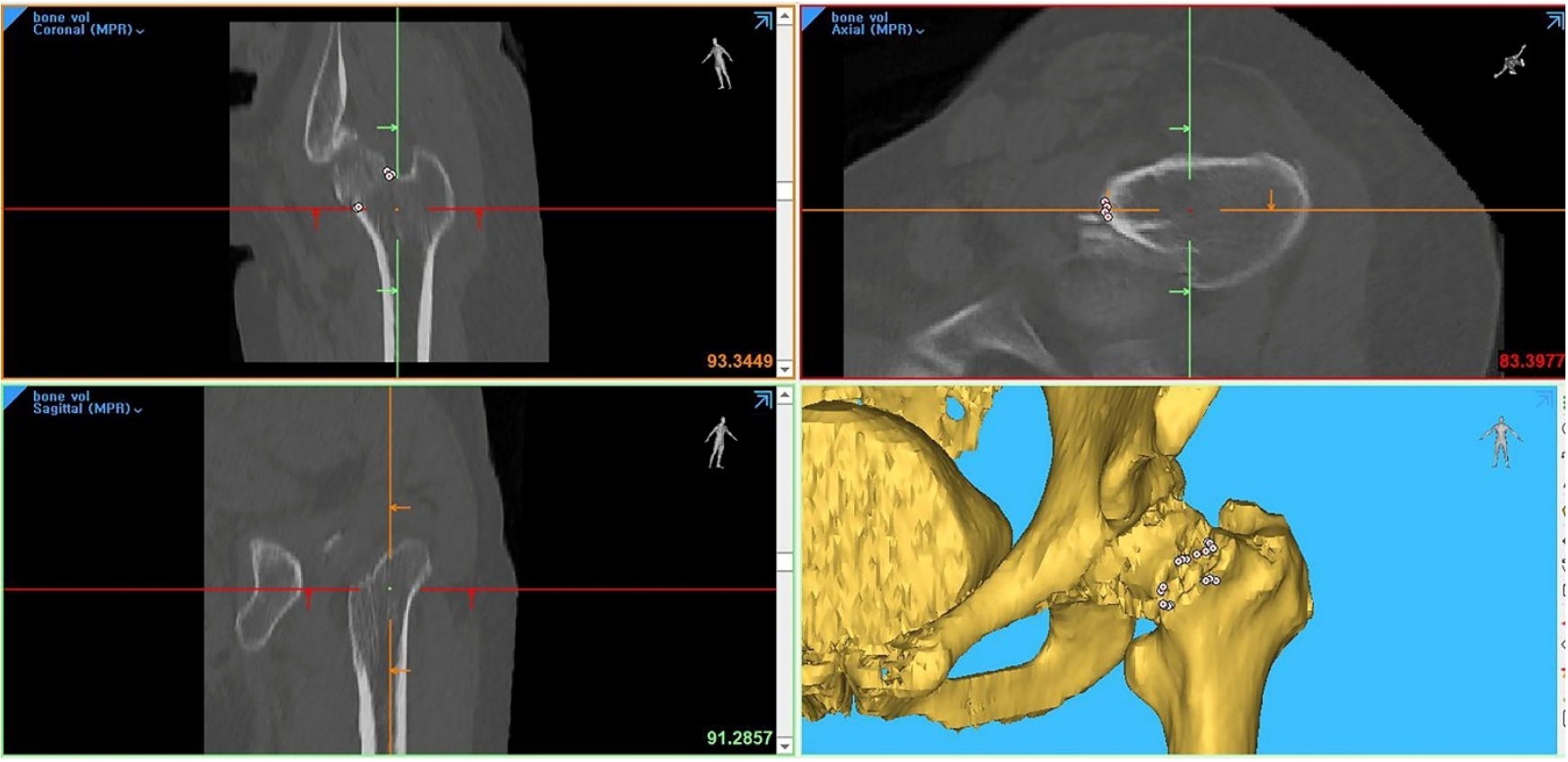
PDF - Objectives
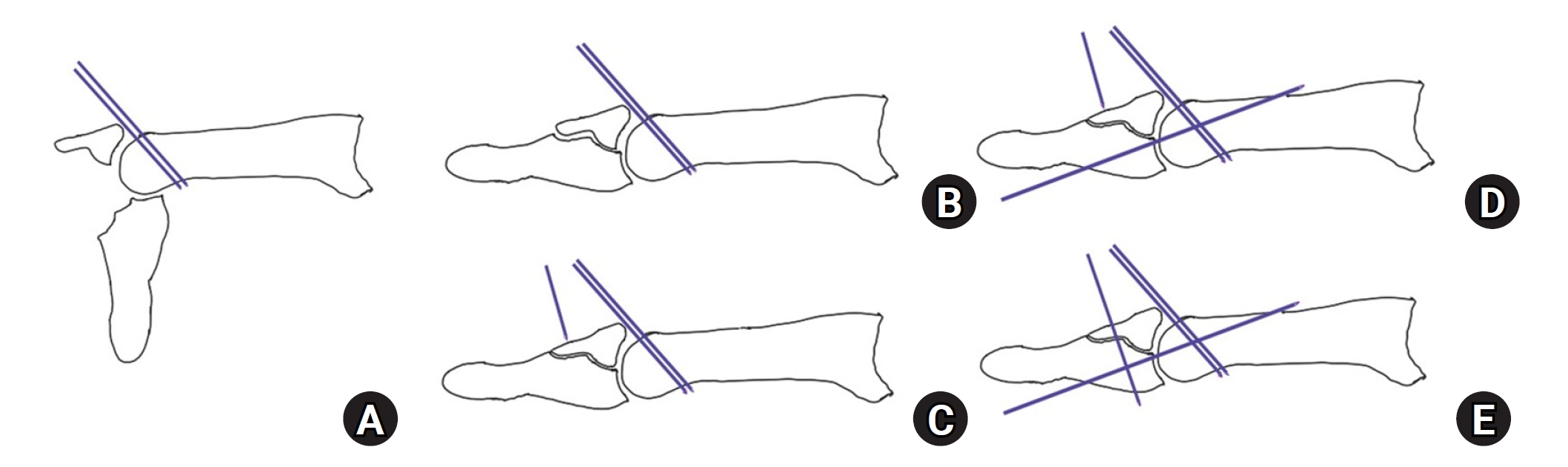
This study aimed to assess fracture verticality in both coronal and axial planes after eliminating projection error in femoral neck fractures among non-older adults, and to demonstrate its clinical utility using computed tomography (CT)-based modeling at actual size.
Methods
This retrospective observational study enrolled 57 patients (30 males and 27 females), aged 20–65 years, with displaced femoral neck fractures. Based on CT images, an actual-size fracture model was constructed. The CT scanning plane was reformatted with the neck-shaft fragment realigned vertically to the ground and parallel to the femoral neck axis. Three consecutive images were used to generate coronal reformats at the centerline and posterior border to measure central and posterior coronal plane verticality as Pauwels’ angle (PA). The central image of the reformatted axial plane was used to assess axial plane verticality. Differences in verticality were analyzed using analysis of variance.
Results
Three coronal morphology types were identified: linear (n=30), concave (n=25), and convex (n=2). Two axial morphology types were observed: cephalad (n=35) and trochanteric (n=22). The mean central PA, posterior PA, and axial verticality were 55.43°±13.79°, 51.44°±11.13°, and 85.74°±18.41°, respectively. Only the central PA showed a significant difference (P<0.001). The PA was significantly higher in the linear coronal type between images (P<0.05) and in the trochanteric axial type (P<0.05).
Conclusions
After reformatting the scanning plane, the central PA showed significant variation between images. Femoral neck fractures of the linear type in the coronal plane and the trochanteric type in the axial plane demonstrated greater verticality than other morphological types. Level of evidence:
- 115 View
- 4 Download

- Surgical outcomes of the coracoid process fracture associated with the acromioclavicular joint injury in Korea: a case series
- Dongju Shin, Sung Choi, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2026;39(1):54-61. Published online January 14, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00346

-
 Abstract
Abstract
 PDF
PDF - Background
Excluding technical reports and isolated case reports, there are no published studies evaluating coracoid process fixation with or without an acromioclavicular joint (ACJ) stabilization procedure for coracoid process fractures associated with ACJ injury. The purpose of this study was to assess the surgical outcomes of coracoid process fractures associated with ACJ injuries and to determine the usefulness of coracoid process fixation with or without an ACJ stabilization procedure.
Methods
From February 2006 to December 2015, patients with coracoid process fractures associated with ACJ injuries were enrolled. Radiological and clinical outcomes were analyzed in 12 patients who underwent coracoid process fixation with or without an ACJ stabilization procedure. A 3.5-mm cannulated screw with a washer or a 3.0-mm headless compression screw was used for coracoid process fixation, and either a clavicle hook plate or Kirschner (K)-wires were used for ACJ injuries when additional fixation was necessary.
Results
Bone union was achieved in 11 patients (91.7%), while one case was determined to be a nonunion at 6 months. Radiological union occurred at an average of 3 months (range, 1.5–4 months) in all patients except the nonunion case. At the final follow-up, the average clinical scores were a visual analogue scale (VAS) pain score of 1.5 (range, 0–4) and a UCLA score of 30.9 (range, 28–35). Clinical outcomes were satisfactory in all patients, including the patient with nonunion.
Conclusion
The clinical and radiological outcomes of treating coracoid process fractures associated with ACJ injuries using coracoid process fixation with or without ACJ stabilization were favorable. A cannulated screw with a washer and clavicle hook plate fixation may provide sufficient stability for both the coracoid process fracture and the ACJ injury when feasible. Level of evidence: IV.
- 158 View
- 5 Download

Technical Note
- Rim plate-assisted intramedullary nail and plate combination technique for complex tibial plateau-to-diaphysis fractures: a technical note and case series
- Whee Sung Son
- J Musculoskelet Trauma 2026;39(1):62-71. Published online December 4, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00290

-
 Abstract
Abstract
 PDF
PDF - Complex tibial plateau-to-diaphysis fractures present a significant surgical challenge due to their intricate fracture patterns and frequent association with severe soft tissue damage and concomitant injuries. This technical note introduces a novel fixation strategy: the rim plate-assisted intramedullary nail-plate combination (NPC) technique. In this approach, a rim plate simplifies the conventional NPC procedure by unifying the tibial plateau fracture into a single structural segment. This modification eliminates the need to address the articular and diaphyseal components simultaneously while enhancing articular stability. Furthermore, the technique preserves soft tissue integrity and promotes early rehabilitation. Clinical case examples demonstrate its successful application in managing complex tibial plateau-to-diaphysis injuries. Level of evidence: V.
- 483 View
- 21 Download

Original Articles
- Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
- Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
- J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00276
-
 Abstract
Abstract
 PDF
PDF - Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
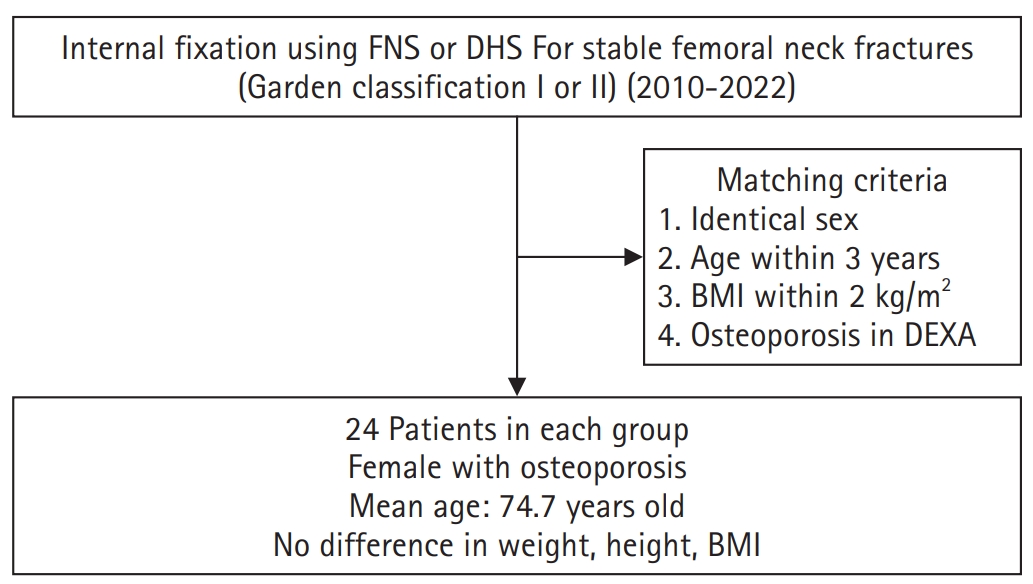
Methods
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results. Level of evidence: IV.
- 1,622 View
- 20 Download

- Relationship of lateral malleolar fracture patterns to posterior malleolar fracture morphology in supination-external rotation ankle fractures in Korea: a retrospective cohort stduy
- Jong-Eun Kim, Chan-Jin Park, Jun-Young Lee, Keun-Bae Lee, Gun-Woo Lee
- J Musculoskelet Trauma 2025;38(4):212-220. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00234
-
 Abstract
Abstract
 PDF
PDF - Background
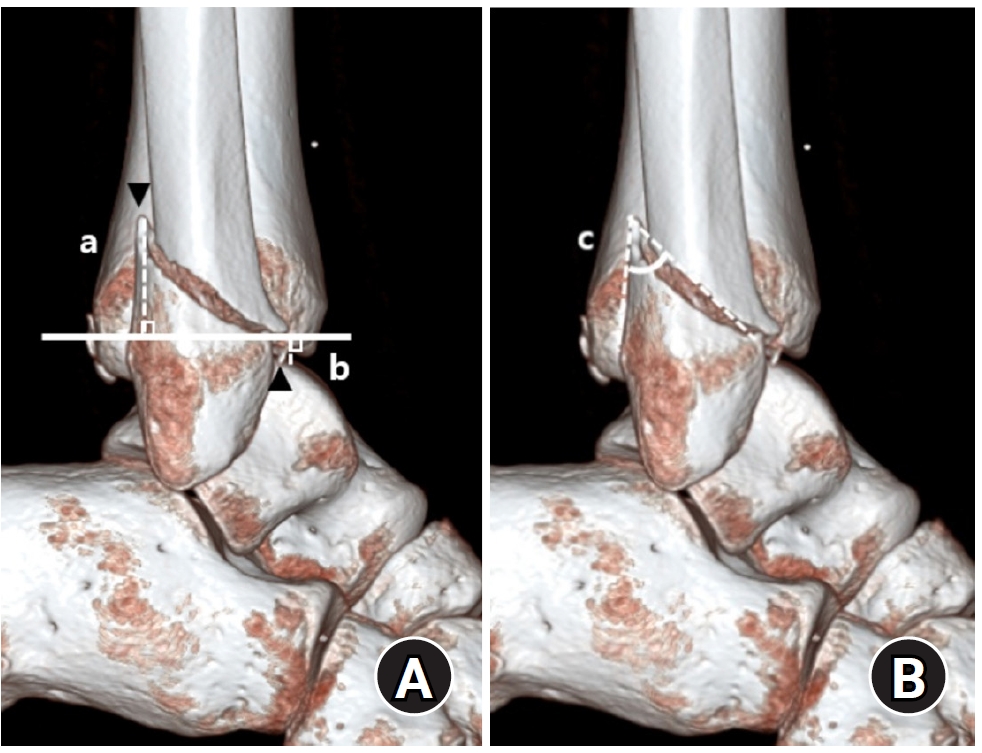
Posterior malleolar fractures frequently accompany rotational ankle fractures. However, the morphological relationship between lateral and posterior malleolar fractures in supination-external rotation (SER) ankle fractures remains unclear. This study aimed to classify lateral malleolar fracture patterns in SER type 3 and 4 ankle fractures and investigated their associations with posterior malleolar fracture morphology.
Methods
We retrospectively reviewed 132 patients with SER type 3 or 4 ankle fractures and concurrent posterior malleolar fractures between January 2016 and December 2021. Lateral malleolar fractures were categorized as fibular fractures extending <4.5 cm proximal to the ankle joint (102 ankles) or fibular fractures extending ≥4.5 cm proximal to the ankle joint (30 ankles) based on posterior cortex height measured using three-dimensional computed tomography (3D-CT). Posterior malleolar fracture morphology was assessed using the Haraguchi and Bartonicek classifications. Quantitative parameters—including fracture height, angle, and articular involvement—were analyzed using 3D-CT imaging.
Results
Fibular fractures extending ≥4.5 cm proximal to the ankle joint were associated with a significantly higher frequency of Haraguchi type II and Bartonicek types 3 and 4 posterior malleolar fractures. This group also exhibited greater articular involvement (19.2% vs. 12.0%) and posterior cortical height (55.4 mm vs. 24.8 mm) compared to the <4.5 cm group (all P<0.001).
Conclusions
In SER type 3 and 4 ankle fractures, a fibular fracture extending ≥4.5 cm proximal to the ankle joint may be associated with posterior malleolar fractures exhibiting greater articular involvement and medial extension. Preoperative evaluation of the lateral malleolar fracture pattern may provide useful insights into posterior malleolar morphology and assist in surgical planning. However, these findings should be interpreted with caution due to inherent study limitations. Level of evidence: IV
- 945 View
- 19 Download

- Correlation of bone mineral density with ankle fractures in older adults in Korea: a retrospective cohort study
- Seung Hyun Lee, Chae Hun Lee, Seo Jin Park, Jun Young Lee
- J Musculoskelet Trauma 2025;38(4):186-192. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00150
-
 Abstract
Abstract
 PDF
PDF - Background
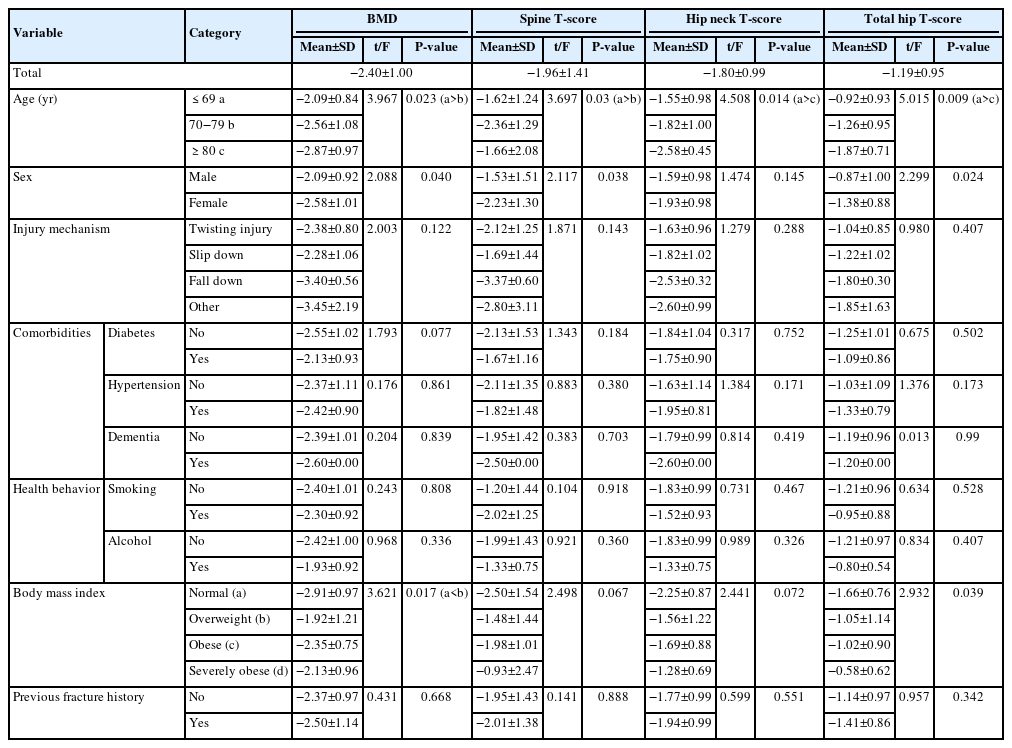
Bone mineral density (BMD) is well-documented in relation to fractures of the spine, hip, distal radius, and proximal humerus; however, its correlations with other fracture types are less established. This study aimed to analyze BMD and associated risk factors in older adults (≥65 years of age) with osteoporotic ankle fractures. These fractures involve low-energy trauma, resulting from falls from a standing height or lower, and occur from impacts which typically do not cause fractures in individuals with normal bone.
Methods
This retrospective study analyzed data from 1,411 patients diagnosed with ankle fractures admitted to Chosun University Hospital between February 2012 and April 2023. After applying inclusion criteria (age ≥65 years; low energy ankle fracture) and exclusion criteria (high energy trauma, open/multiple fractures, missing dual X-ray absorptiometry [DXA]), 73 of 1,411 patients were analyzed. Lumbar spine, femoral neck, and total hip T scores were obtained with a Horizon Wi DXA scanner, and associations with age, sex, mechanism of injury, comorbidities, smoking status, alcohol consumption, body mass index (BMI), and history of fractures were tested by ANOVA with Scheffe post hoc and Fisher exact tests.
Results
Lower BMD correlated significantly with older age, female sex, and lower BMI (P<0.05) in older adults with ankle fractures. No significant associations were observed for comorbidities (diabetes, hypertension, dementia), smoking, alcohol consumption, injury mechanism, or prior fractures.
Conclusion
These results indicate that older age, female, and lower BMI are linked to reduced BMD in ankle fracture patients over 65 years of age. Focused osteoporosis screening and management may therefore be most beneficial for older, low BMI women presenting with ankle fractures. Level of evidence: IV.
- 873 View
- 2,147,483,670 Download

- Risk factors for ankle fractures in older adults based on clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities in Korea: a retrospective case-control study
- Myeong Jun Song, Se Woong Jang, Jun Young Lee, Seojin Park
- J Musculoskelet Trauma 2025;38(4):193-202. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00143
-
 Abstract
Abstract
 PDF
PDF - Background
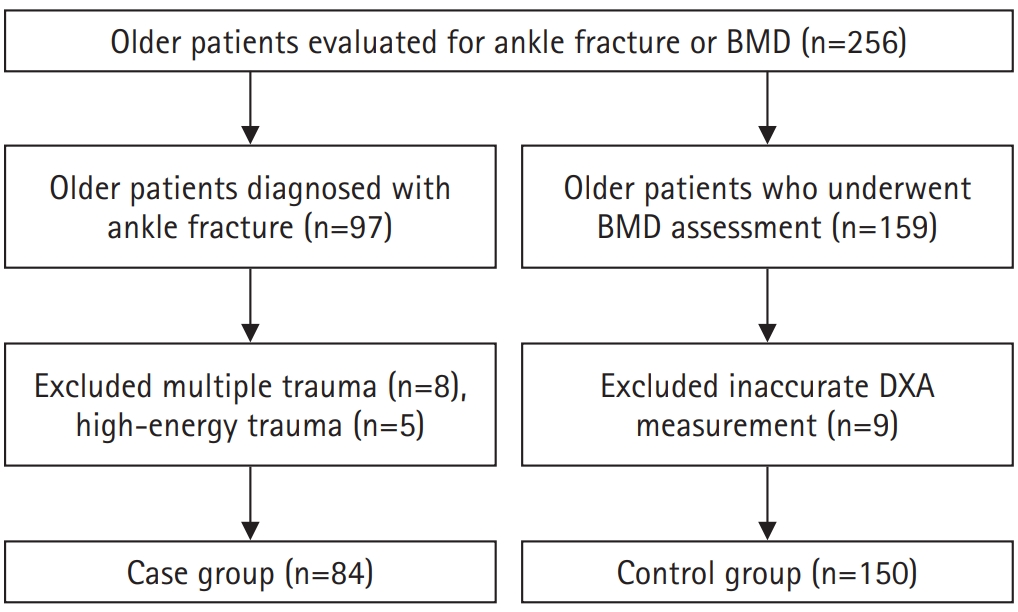
Ankle fractures are common in older adults; however, their relationship with osteoporotic fractures remains unclear. This study aimed to evaluate potential risk factors for ankle fractures in older adults by analyzing individual clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities.
Methods
We conducted a retrospective case-control study including 84 patients aged ≥65 years with ankle fractures and 150 controls who underwent bone mineral density (BMD) testing without prior ankle fractures. The variables analyzed included age, sex, body mass index, smoking, alcohol consumption, prior fracture history, and comorbidities such as hypertension, diabetes mellitus, and dementia. BMD was measured at the spine, total hip, and femoral neck.
Results
Univariate analysis showed that alcohol consumption, diabetes mellitus, and total hip T-score categories were significantly associated with ankle fractures. In binary logistic regression, alcohol consumption remained significantly associated with higher ankle fracture risk (odds ratio [OR], 5.302; 95% confidence interval [CI], 1.778–15.811; P=0.003), and both osteopenia and osteoporosis at the total hip were also associated with increased risk (OR, 3.260, P=0.049; OR, 3.561, P=0.031, respectively). Diabetes mellitus did not reach statistical significance in the adjusted model (P=0.074). Model fit was adequate (Hosmer-Lemeshow P=0.377), and post hoc power analysis confirmed sufficient sample size.
Conclusions
These findings suggest that lower total hip BMD and alcohol-related factors may be associated with ankle fracture risk in older adults. The FRAX score itself was not calculated; instead, this study focused on analyzing selected clinical components. Limitations include the retrospective design, lack of fall and medication data, and cross-sectional BMD assessment. Level of evidence: III.
- 1,121 View
- 21 Download

- Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
- Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
- J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00157
-
 Abstract
Abstract
 PDF
PDF - Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
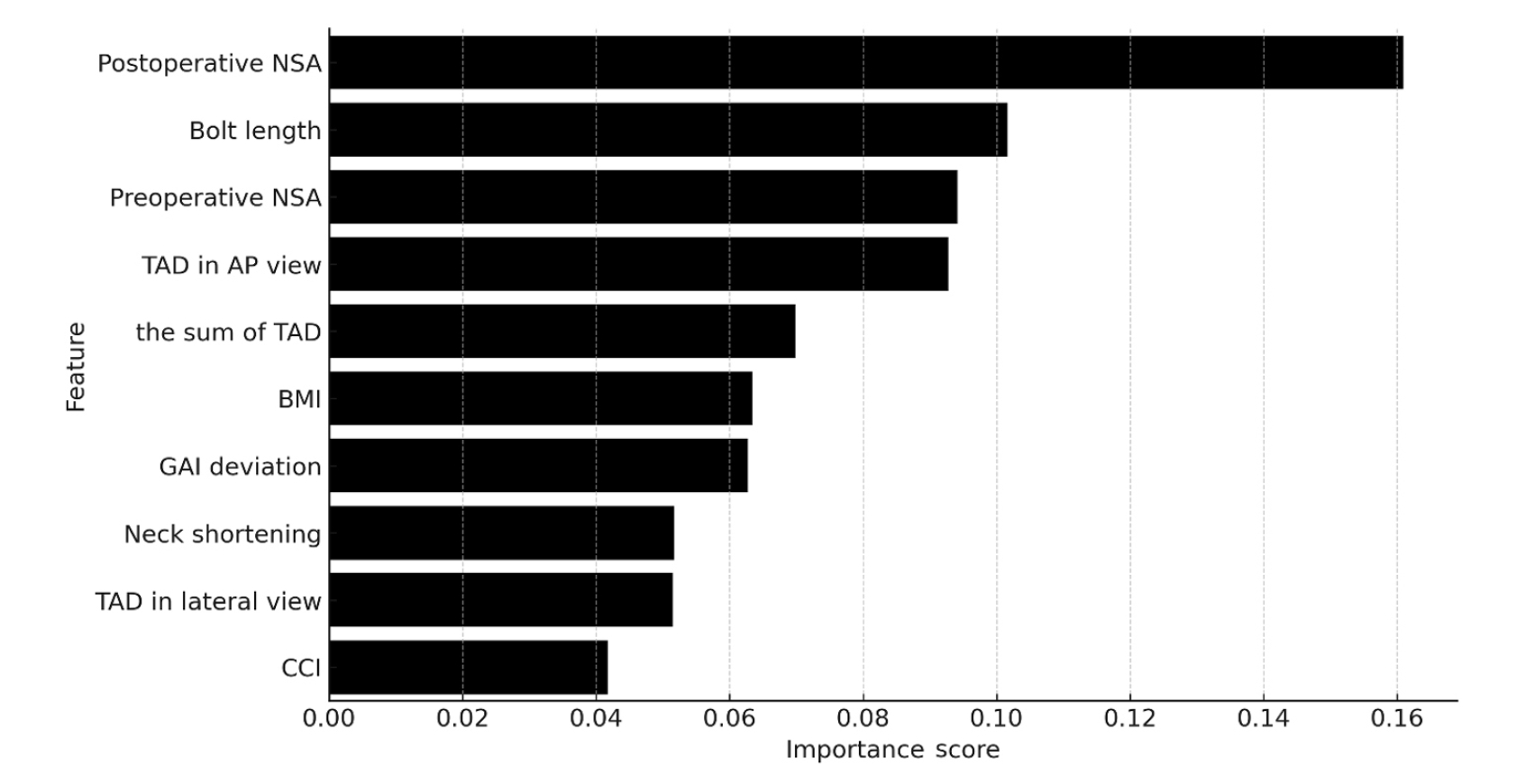
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery. Level of Evidence: III. -
Citations
Citations to this article as recorded by- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
Seonghyun Kang, Wonseok Choi, Jeong Seok Choi, Eic Ju Lim, SungJin Ahn, Jong-Keon Oh, William T. Kent, Whee Sung Son, Jae-Woo Cho
Journal of Orthopaedic Surgery.2026;[Epub] CrossRef
- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
- 1,191 View
- 43 Download
- 1 Crossref

Review Article
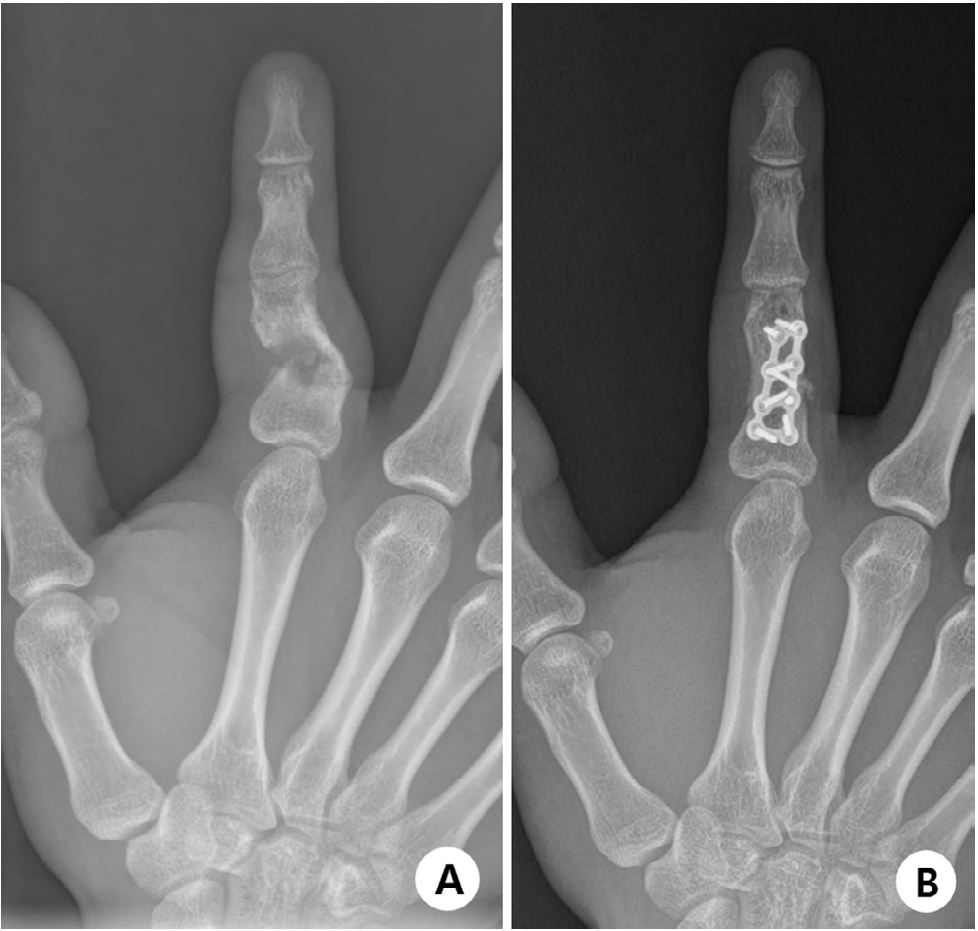
- Current concepts in the management of phalangeal fractures in the hand
- Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):109-123. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00136
-
 Abstract
Abstract
 PDF
PDF - This review focuses on the treatment of hand fractures based on the anatomical location of the fractured phalanx, excluding the thumb, and examines recent studies on the topic. The main points are as follows: in most cases of hand fractures, conservative treatment should be prioritized over surgical intervention. The three key factors in determining whether surgical treatment is necessary are (1) whether the fracture is intraarticular, (2) the stability of the fracture itself, and (3) the extent of damage to surrounding soft tissues. The primary surgical treatment is closed reduction and Kirschner-wire fixation. The risk of rotational deformity increases with fractures closer to the proximal region. Intra- articular fractures may lead to subsequent stiffness and arthritis; thus, computed tomography is recommended to assess the fracture pattern. Anatomic reduction of intraarticular fragments is required, along with correction of the inherent joint instability. No surgical method has proven to be superior; it is advantageous for the surgeon to choose a surgical approach they are familiar with and confident in, based on the specific fracture and patient factors. Complications in hand fractures are various; the most frequent is stiffness, and nonunion is uncommon. Early joint motion is crucial in minimizing the risk of stiffness.
- 16,487 View
- 352 Download

Original Articles
- Computational simulation of coracoclavicular screw insertion through the superior distal clavicular plate for clinical applications in Korean cadavers
- Hyung-Lae Cho, Ji Han Choi, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):143-151. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00122
-
 Abstract
Abstract
 PDF
PDF - Background
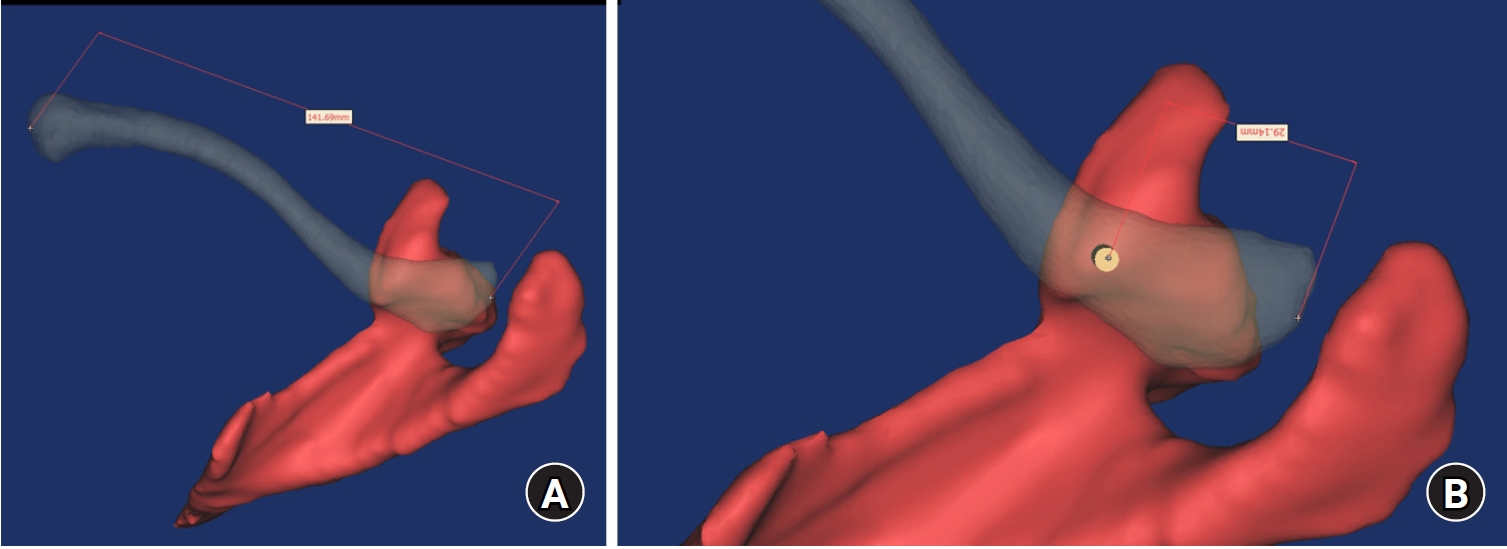
The study was conducted to determine the practical area for inserting the coracoclavicular (CC) screw through the plate by analyzing three-dimensional (3D) shoulder models featuring virtually implanted, actual-size plates and screws.
Methods
Ninety cadaveric shoulders (41 males and 49 females) underwent continuous 1.0-mm slice computed tomography scans. The data were imported into image-processing software to generate a 3D shoulder model, including the scapula and clavicle. The overlapping area between the clavicle and the horizontal portion of the coracoid process (horizontal portion_CP) was analyzed in the cranial view. A curved pelvic recon plate was virtually placed on the upper surface of the distal clavicle, and an actual-size (3.5 mm) CC screw was inserted through the plate.
Results
The distal clavicle directly overlapped with the horizontal portion_CP in the vertical direction. The overlapping area was sufficient to place the 3.5 mm and 4.5 mm-sized screws. In all shoulder models, the CC screw could be inserted through the plate into the vertical direction, with an average length of 35.5 mm (range, 26.2–62.5 mm; standard deviation, 1.2 mm). In 87 models, the CC screw was inserted through the third hole from the lateral end of the plate. Two models were inserted through the second hole, and one model through the fourth hole.
Conclusions
The upper surface of the clavicle has sufficient overlapping area to place CC screws through the plate in the vertical direction in the corresponding hole. Supplemental CC screw fixation through the plate can be performed without additional or special equipment. Level of evidence: IV
- 646 View
- 21 Download

- Biomechanical finite element analysis of a femoral neck system fixation construct for femur neck fractures and clinical implications
- Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):133-142. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00108
-
 Abstract
Abstract
 PDF
PDF - Background
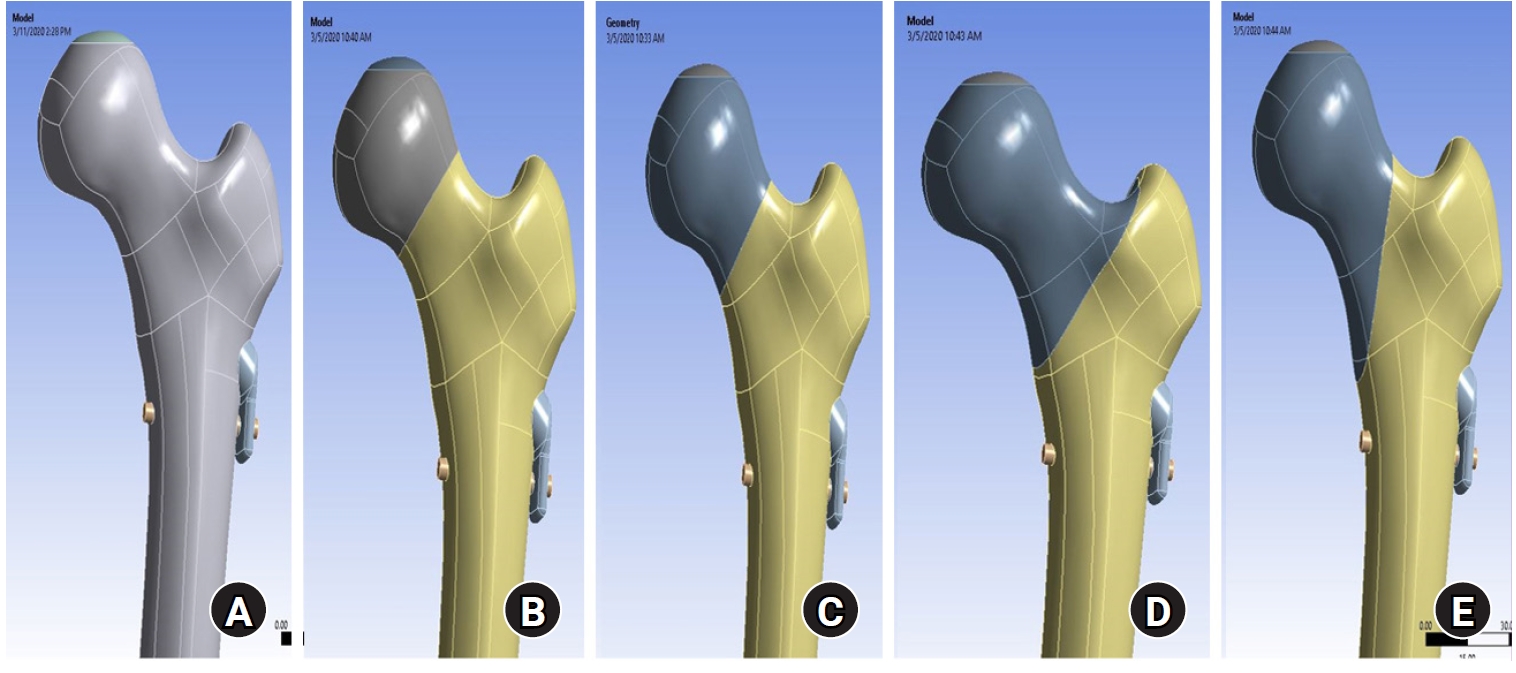
This study assessed the structural/mechanical stability of fixation constructs with a femoral neck system (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications.
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital, 68.56 MPa for a transcervical, 344.54 MPa for a basicervical, and 130.59 MPa for a vertical model. The maximum VMS of FNS was 840.34 MPa for a subcapital, 637.37 MPa for a transcervical, 464.07 MPa for a basicervical, and 421.01 MPa for a vertical model. The stress distribution of basicervical and vertical fractures differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
FNS fixation should be performed with consideration the osseous anchorage in the femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution. Level of evidence: IV. -
Citations
Citations to this article as recorded by- Finite element analysis of screw thread geometry and titanium plate materials in internal fixation of the human femur
Abdessamed Bachiri, Mustapha Amine Arab, Nadia Kadouri
Computer Methods in Biomechanics and Biomedical Engineering.2026; : 1. CrossRef
- Finite element analysis of screw thread geometry and titanium plate materials in internal fixation of the human femur
- 1,876 View
- 82 Download
- 1 Crossref

Review Articles
- Atypical femoral fractures: an update
- Won-Tae Cho, Jeong-Hyun Koh, Seungyeob Sakong, Jung-Taek Kim
- J Musculoskelet Trauma 2025;38(2):41-52. Published online March 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00031
-
 Abstract
Abstract
 PDF
PDF - This narrative review provides an up-to-date overview of atypical femoral fractures (AFFs), emphasizing diagnostic criteria, epidemiology, pathophysiology, risk factors, and evaluation with screening strategies. AFFs are rare but significant complications associated with prolonged bisphosphonate (BP) therapy for osteoporosis. Although the pathogenesis of AFFs has not been fully elucidated, its primary mechanism is thought to involve impaired bone remodeling, leading to unhealed microfractures that progress to stress fractures under repetitive loading. AFFs can occur in various regions of the femur, influenced by femoral geometry and the lower limb axis. Other risk factors include prolonged steroid use, arthroplasty, genetic predispositions, and metabolic bone disorders. The diagnosis of AFFs is based on criteria established by the American Society for Bone and Mineral Research. Key radiographic features include lateral cortical transverse fracture lines and localized cortical thickening, typically with minimal or no comminution on the medial cortex. Dual-energy X-ray absorptiometry for screening tests and magnetic resonance imaging as an advanced imaging modality enable the early detection of incomplete fractures. This multi-modal approach facilitates the prompt identification of prodromal cortical changes, reducing the risk of complete fractures in high-risk populations, particularly patients undergoing prolonged BP therapy. Level of Evidence: V
-
Citations
Citations to this article as recorded by- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
Lorenzo Lucchetta, Carmelinda Ruggiero, Samuele Berardi, Alice Franceschi, Michele Bisaccia, Giuseppe Rinonapoli
Journal of Clinical Medicine.2025; 15(1): 25. CrossRef
- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
- 14,580 View
- 398 Download
- 1 Crossref

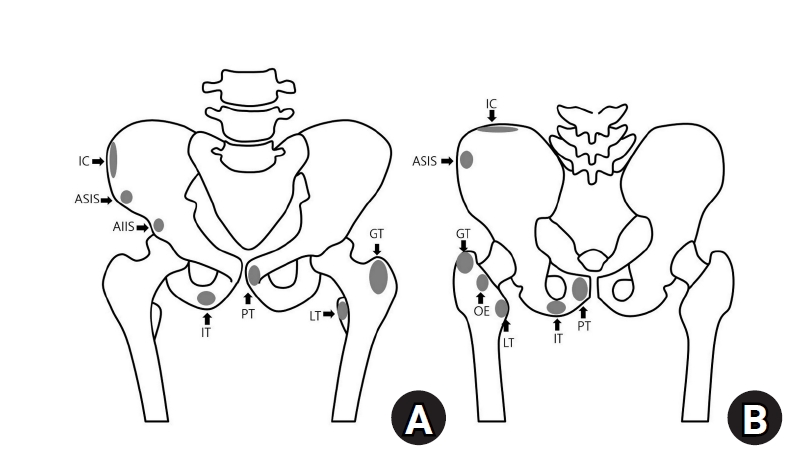
- Avulsion fractures around the hip joint and pelvis
- Won-Sik Choy, Yonghan Cha, Jung-Taek Kim, Jun-Il Yoo, Jin-Woo Kim
- J Musculoskelet Trauma 2025;38(2):53-62. Published online March 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00010
-
 Abstract
Abstract
 PDF
PDF - Avulsion fractures occur when tendons or ligaments are subjected to forces greater than they can withstand at the apophysis or enthesis, regardless of fusion status. The pelvis and hip joint are vulnerable to these injuries due to the diverse muscular structures in these structures, which serve as origins for multiple muscles leading to the lower extremities. Pelvic avulsion fractures commonly affect young athletes, but can also occur in adults. The diagnosis typically involves assessing trauma history, a clinical examination, and radiographic imaging. If the diagnosis is unclear, additional tests such as computed tomography and magnetic resonance imaging may assist in the diagnosis and provide useful information for treatment decisions. While most avulsion fractures respond well to conservative treatment, surgical intervention may be preferred in severe displacements, cases of significant retraction in active athletes, or when a faster recovery is necessary. Chronic or neglected injuries may lead to excessive osseous formation around the pelvis, causing impingement syndromes. Recognizing characteristic radiological findings based on pelvic anatomy helps to make an accurate diagnosis, as chronic injuries can mimic tumors or infectious conditions, necessitating a careful differential diagnosis.
-
Citations
Citations to this article as recorded by- Avulsion Fracture of the Lesser Trochanter and the Use of Conservative Treatment
Dawid Bartosik, Bartlomiej Cwikla, Anna Kowalczyk, Michalina Loson-Kawalec, Anna Palka-Szymaniec, Bartosz Starzynski, Alina Keska, Jakub Szkuta, Klaudia Wojcik
Cureus.2026;[Epub] CrossRef
- Avulsion Fracture of the Lesser Trochanter and the Use of Conservative Treatment
- 8,825 View
- 133 Download
- 1 Crossref

- Easily missed nondisplaced fractures accompanying complete fractures in the lower extremity and pelvis: a narrative review
- Young-Chang Park
- J Musculoskelet Trauma 2025;38(1):5-12. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00017

-
 Abstract
Abstract
 PDF
PDF - Nondisplaced fractures accompanying complete fractures are often difficult to detect on plain radiographs or computed tomography scans, posing a diagnostic challenge. The diagnosis of these frequently overlooked injuries can be delayed, potentially leading to suboptimal patient outcomes. This review discusses four commonly missed fracture patterns in the lower extremity and pelvis, including posterior involvement in fragility fractures of the pelvis, intertrochanteric extensions in isolated greater trochanter fractures, ipsilateral femoral neck fractures in high energy femoral shaft fractures, and posterior malleolar fractures in distal spiral tibial shaft fractures. An accurate diagnosis of these accompanying nondisplaced fractures is critical for optimizing surgical outcomes. Surgeons should incorporate thorough preoperative evaluations into their clinical practice to facilitate early detection and appropriate treatment strategies. Prompt identification and comprehensive management remain essential for improving patient outcomes.
- 1,298 View
- 47 Download

Original Articles
- Outcomes of open reduction and internal fixation using 2.0/2.4 mm locking compression plate in isolated greater tuberosity fractures of humerus
- Sung Choi, Dongju Shin, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2025;38(1):32-39. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00005

-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to retrospectively evaluate the radiographic and clinical results of a small single or double low-profile plate fixation of 2.0/2.4 mm locking compression plate (LCP) in treating isolated greater tuberosity (GT) fractures of the humerus. Methods: From June 2015 to October 2022, patients who underwent LCP in treating isolated GT fractures of the humerus were included in this study. The radiological and clinical results were analyzed in 15 patients who underwent open reduction and internal fixation used 2.0/2.4 mm LCP. Results: Bone union was achieved in 14 patients (93.3%) and one failed case was treated with a 2.4 mm single LCP fixation. Radiological union was achieved within 10–20 weeks. Complications occurred in two patients (13.3%), including the reduction failure and shoulder stiffness. At the final follow-up, the average clinical scores were as follows: a visual analog scale for pain of 2.1 (range, 0–5) and a University of California, Los Angeles score of 27.2 (range, 18–31). Regarding range of motion (ROM), the average active ROMs were 142° for forward flexion (range, 120°–150°), 147.1° for abduction (range, 120°– 180°), and 59.3° for external rotation (range, 45°–80°). For internal rotation, the average was observed to reach the 10th thoracic vertebra (range, 1st lumbar vertebra–7th thoracic vertebra). Conclusions: The clinical and radiologic outcomes of treating isolated GT fracture using 2.0/2.4 mm LCP were favorable, and double low-profile plate fixation may be beneficial for sufficient fracture stability if possible. Level of evidence: Level IV, case series.
- 1,988 View
- 57 Download

- Interpositional tricortical iliac bone graft in nonunion of midshaft clavicular fractures
- Eun-Seok Son, Bum-Soon Park, Chang-Jin Yon, Chul-Hyun Cho
- J Musculoskelet Trauma 2025;38(1):23-31. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00004

-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to investigate the radiological and clinical outcomes after interpositional tricortical iliac bone graft with plate fixation for the nonunion of clavicle midshaft fractures. Methods: Between 2007 and 2020, 17 cases who were treated by interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion combined with bone defect were investigated. The mean age was 53 years (range, 22–70 years). The mean follow-up period was 102.2 months (range, 18–193 months). Serial plain radiographs were used to evaluate radiological outcomes. The University of California, Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, and Quick-disabilities of the arm, shoulder, and hand (DASH) score were used to evaluate clinical outcomes. Complications were also evaluated. Results: All cases achieved complete bony union with mean healing time of 17.6 weeks (range, 14–22 weeks). The mean clavicle length difference was significantly decreased from 9.1 mm preoperatively to 2.6 mm postoperatively (P<0.001). The mean UCLA and ASES scores were significantly improved from 18.1 and 52.2 before surgery to 30.6 and 88.6 after surgery (both P<0.001), respectively. The mean final Quick-DASH score was 18.0. Three cases (17.6%) developed postoperative complications including two cases of shoulder stiffness and one case of screw irritation. Conclusions: Interpositional tricortical iliac bone graft with plate fixation for the clavicle midshaft nonunion demonstrated excellent radiological and clinical outcomes. In cases of atrophic nonunion combined with bone defect, this technique is an effective option that can provide structural support and restore clavicle length. Level of evidence: Level IV, case series.
- 1,954 View
- 42 Download

- Analysis of Missed Fractures by Bone Scan in Elderly Hip Fracture Patients with Osteoporosis
- Tae Hun Lee, Yeong Hyun Lee, Seo Won Kang
- J Korean Fract Soc 2024;37(3):144-149. Published online July 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.3.144
-
 Abstract
Abstract
 PDF
PDF - Purpose
The incidence of hip fractures is increasing due to an increase in elderly populations because elderly patients often have accompanying diseases, such as cognitive impairment or dementia, which may lead to missed fractures. Therefore, this study assessed the utility of bone scans in detecting missed fractures in elderly patients.
Materials and Methods
This study analyzed the data from 178 patients treated from January 2014 to March 2023. The inclusion criteria were patients who had hip fractures with osteoporosis over 70 years old. Bone scans were performed on average 10 days after injury. The rate and trend of missed fractures not detected in the initial diagnosis were determined based on sex, age, dementia status, and the presence of osteoporosis.
Results
Among the 178 hip fracture patients over 70 years old, 37 patients had a history of being diagnosed with dementia, and 141 patients had never been diagnosed. Missed fractures were confirmed in 49 cases (42 patients) (23.6%). The dementia group had 13 missed fractures, and the non-dementia group had 36 missed fractures, but there was no significant difference. Rib fractures were most common, followed by vertebral fractures.
Conclusion
Missed diagnoses of fractures were common among elderly hip fracture patients. A whole body bone scan appeared to be effective in detecting missed fractures. Therefore, identifying accompanying fractures through bone scans and delivering appropriate treatment can play an important role in postoperative rehabilitation.
- 661 View
- 9 Download

- Effect of Coincident Hip Fracture on Distal Radius Fracture in Patients Treated with a Volar Locking Plate: A Matched-Pair Analysis of Elderly Patients
- Hyoung-Seok Jung, Min-Su Chu, Jae-Sung Lee
- J Korean Fract Soc 2024;37(3):137-143. Published online July 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.3.137
-
 Abstract
Abstract
 PDF
PDF - Purpose
Although the incidence of simultaneous distal radius and hip fractures in older patients is minimal, patients with these coincident types of fractures exhibit unique features. This study analyzed the outcomes associated with operative treatment involving volar-locking plates in patients who sustained distal radius fractures and hip fractures and compared them with those in matched control patients who had undergone treatment for isolated distal radius fractures.
Materials and Methods
Between 2010 and 2015, 34 patients, who met the criteria for hip and distal radius fractures, were retrospectively reviewed. Thirty-four matched patients who underwent volarlocking plate fixation for isolated distal radius fractures during the same period were also reviewed. The clinical outcomes between the groups were compared using postoperative radiological parameters.
Results
The radiological assessment revealed a better radial length and inclination in the control group than in the study group at the final follow-up. In other words, patients with coincident hip fractures showed a higher tendency for loss of reduction. Despite the differences in radiological parameters, no significant differences in clinical outcomes were observed, except for grip strength.
Conclusion
Although volar-locking plating provides greater stabilization, a loss of reduction occurred in patients with coincident hip fractures.
- 873 View
- 9 Download

- Comparison of the Radiological Outcomes of an Anatomical Quadrilateral Surface Plate with a Pelvic Reconstruction Plate in Acetabulum Fractures
- Sung Hyun Yoon, Hee Gon Park, Dong Uk Lee
- J Korean Fract Soc 2024;37(2):95-101. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.95
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the radiological outcomes of fixation using an anatomical quadrilateral surface plate with those using a traditional pelvic reconstruction plate for fractures involving the quadrilateral surface or superomedial wall of the acetabulum.
Materials and Methods
From 2015 to 2022, 47 patients who met the inclusion and exclusion criteria were analyzed retrospectively. Internal fixation of an acetabular fracture was achieved with a pelvic reconstruction plate (n=28) or an anatomical quadrilateral surface plate (n=19). The ability to achieve immediate postoperative anatomical reduction and the long-term outcomes were assessed by confirming the arthritic changes. Immediate postoperative reduction quality and long-term radiological outcomes for post-traumatic arthritis were assessed using the Matta scoring system on standard radiographs.
Results
The assessment of immediate postoperative reduction in the pelvic reconstruction plate group was satisfactory in 16 patients (57.1%) and unsatisfactory in 12 patients (42.9%). In the anatomical quadrilateral surface plate group, the results were satisfactory in 16 patients (84.2%) and unsatisfactory in 3 patients (15.8%). When evaluating over an extended follow-up period in the pelvic reconstruction plate group, 19 patients (67.9%) demonstrated satisfactory, while 9 patients (32.1%) had unsatisfactory outcomes. In the anatomical quadrilateral surface plate group, 12 patients (63.2%) achieved satisfactory, and 7 patients (36.8%) had unsatisfactory outcomes. The immediate postoperative reduction quality was superior in the anatomical quadrilateral surface plate group (p=0.03). Comparing longterm results, the anatomical quadrilateral surface plate group did not have statistically more favorable outcomes (p=0.49).
Conclusion
In this study, the anatomical quadrilateral surface plate achieved sufficiently good radiological results without significant difference from the existing pelvic reconstruction plate. It was concluded that it is a useful option that can replace the existing metal plate in the selection of surgery for acetabular fractures.
- 899 View
- 10 Download

Review Articles
- Treatment of Avulsion Fractures around the Knee
- Sumin Lim
- J Korean Fract Soc 2024;37(2):117-124. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.117
-
 Abstract
Abstract
 PDF
PDF - Avulsion fractures are common in athletes and result from high-impact or sudden, forceful movements involving the separation of a bone fragment at the ligament or tendon attachment site. The key focus areas include the anterior and posterior cruciate ligaments, medial collateral ligament, anterolateral complex, arcuate complex, medial patellofemoral ligament, patellar tendon, and quadriceps tendon. Diagnostic approaches combine radiography with advanced imaging techniques, such as computed tomography and magnetic resonance imaging, to elucidate the extent of injury and guide treatment decisions. Treatment ranges from conservative management for non-displaced fractures to surgical intervention for displaced fractures, with strategies customized based on the specific ligament involved and the nature of the fracture.
- 1,257 View
- 10 Download

- Osteoporotic Hip Fracture: How We Make Better Results?
- Byung-Chan Choi, Kyung-Jae Lee
- J Korean Fract Soc 2024;37(1):52-59. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.52
-
 Abstract
Abstract
 PDF
PDF - The prevalence of osteoporosis and incidence of osteoporotic fractures is increasing gradually as life expectancy is prolonged and the aged population increases. Osteoporotic hip fractures (femoral neck fractures and femoral intertrochanteric fractures) have high mortality because the patients with these fractures are elderly and have several comorbidities. Thorough preparation and a multidisciplinary approach in the preoperative period are critical, and early surgery is recommended. There are also several principles to treat osteoporotic hip fractures and prevent fixation failures. Many studies have suggested various treatment methods for femoral neck fractures and femoral intertrochanteric fractures. Functional recovery treatment is essential based on the patient’s health and activity levels. Finally, aggressive management of osteoporosis and the prevention of falling is needed to treat osteoporotic hip fractures successfully.
- 630 View
- 24 Download

- Fracture-Related Complication: Fat Embolism Syndrome
- Beom-Soo Kim
- J Korean Fract Soc 2023;36(3):95-102. Published online July 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.3.95
-
 Abstract
Abstract
 PDF
PDF - Fat embolization is a common occurrence after trauma or during orthopedic procedures involving intramedullary manipulation. Although uncommon, fat embolism syndrome (FES) with respiratory failure, neurologic dysfunction, and petechial rash can be fatal to patients. Two theories are proposed for the manifestation of FES: in the mechanical theory, FES occurs when fat tissue in the bone marrow enters the bloodstream and mechanically blocks it; the biochemical theory proposes that FES occurs due to an inflammatory reaction caused by free fatty acids. There are currently no clear diagnostic criteria for FES, and symptoms and signs are typically nonspecific. For the treatment of FES, conservative and supportive management is performed for the specific symptoms, and close monitoring of the respiratory and neurologic systems is required in high-risk groups. Early fracture fixation of long bones helps prevent and reduce the severity of fat embolism.
- 924 View
- 11 Download

Original Article
- Outcomes of Minimally Invasive Surgery in Intra-Articular Calcaneal Fractures: Sanders Type III, Joint Depressive Type Calcaneal Fracture
- Je Hong Ryu, Jun Young Lee, Kang Yeol Ko, Sung Min Jo, Hyoung Tae Kim
- J Korean Fract Soc 2023;36(3):85-94. Published online July 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.3.85
-
 Abstract
Abstract
 PDF
PDF - Purpose
To evaluate the radiologic and clinical outcomes of a minimally invasive technique using the tarsal sinus approach in the management of Sanders type III, joint depressive type calcaneal fractures.
Materials and Methods
Between July 2011 and September 2019, data of 29 patients who underwent a minimally invasive procedure with the sinus tarsi approach for Sanders type III joint depressive intra-articular calcaneal fractures, and were followed up for more than 1 year were analyzed. We evaluated the radiologic outcomes by assessing the radiologic parameters (Böhler angle, Gissane angle, calca-neal length, calcaneal height, calcaneal width). We also evaluated the clinical outcomes based on the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score and the complications associated with the technique.
Results
The radiological results showed an improvement in the Böhler angle from 2.5° to 18.6° and the Gissane angle from 132.4° to 119.1° after the operation. The mean AOFAS score during the clini-cal evaluation was 79.5. We observed 13 cases of posttraumatic arthritis, 1 case of subtalar arthrodesis, and no case of wound complication.
Conclusion
Minimally invasive technique for Sanders type III joint depressive calcaneal fractures resulted in relatively satisfactory radiologic and clinical outcomes. Open reduction and internal fixation through the sinus tarsi approach reduce complications including wound problems. This approach offers satisfactory results without long-term complications.
- 544 View
- 2 Download

Review Articles
- Hip Fractures in the Elderly: Perioperative Management and Prevention of Medical Complications
- Keong-Hwan Kim
- J Korean Fract Soc 2023;36(1):39-44. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.39
-
 Abstract
Abstract
 PDF
PDF - Elderly patients with hip fractures are at an increased risk of developing medical complications with higher mortality rates. Most patients require surgical treatment, and an early surgical intervention can reduce complications and lower mortality risk. A restrictive red blood cell transfusion strategy is usually applied, and the amount of transfusion can be reduced through medications such as tranexamic acid. Delirium can be prevented using non-pharmacological methods. In addition, it is necessary to prevent venous thromboembolism through mechanical or chemical prophylaxis. A multidisciplinary approach using the ERAS (Enhanced Recovery After Surgery) protocol and orthogeriatric care can help to reduce medical complications and mortality.
-
Citations
Citations to this article as recorded by- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
Jee Young Lee, Gyu Min Kong
Journal of Orthopaedic Trauma.2025; 39(7): 352. CrossRef - Comparison of Operation Time, Vital Signs, Bleeding Tendency, and Recovery Time Based on Anesthesia Methods in Patients Undergoing Hip Fracture Surgery
Je Bog Yoo, Woo Young In, Chang Ok Pyo, Jeung Hee Kwon, Min Ji Lee, Kwang Hee Kim, Kyoung Ok Kim, Mi Yu
Journal of PeriAnesthesia Nursing.2025;[Epub] CrossRef
- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
- 1,390 View
- 40 Download
- 2 Crossref

- Fragility Fractures of the Pelvis and Sacrum
- Se-Won Lee, Ju-Yeong Kim
- J Korean Fract Soc 2023;36(1):29-38. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.29
-
 Abstract
Abstract
 PDF
PDF - The incidence of fragility fractures of the pelvis (FFP) has increased significantly due to the aging popu-lation and improved diagnostic modalities. The evaluation and treatment of these patients differ from that of high-energy pelvic ring injuries typically seen in younger patients. Therefore, it is important to classify the FFP by patterns of the classification system to standardize optimal treatment criteria and appropriate treatment strategy. However, some cases are not classifiable according to the FFP classifi-cation. A newly proposed classification that can be verified by comparing existing FFP classifications is needed to overcome the weak points. Non-operative treatment is usually considered first and should focus on early mobilization. Operative fixation should focus on stabilizing the minimally invasive pelvic ring than the reduction of fractures to facilitate early mobilization and avoid complications that can arise from comorbidities associated with immobility.
- 1,850 View
- 33 Download

Original Article
- Distal Femur Fractures Treated with Distal Femoral Locking Plate Fixation: A Retrospective Study of One Year Mortality and Risk Factors
- Kwang-Hwan Jung, Yoon-Seok Youm, Seung-Hyun Jung, Jae-Min Oh, Ki Bong Park
- J Korean Fract Soc 2023;36(1):10-16. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.10
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the one-year mortality after locking plate fixation for distal femur fractures and the risk factors related to death.
Materials and Methods
From July 2011 to June 2020, 128 patients who underwent locking plate fixation for distal femur fractures were analyzed retrospectively. Epidemiologic information of the patients, characteristics related to fracture and surgery, and death were investigated. The risk factors related to death were investigated using Cox analysis, and a subgroup analysis was also performed based on the age of 65 years.
Results
The one-year mortality rate after locking plate fixation for distal femur fractures was 3.9%, and the mortality rates in patients younger than 65 years and older than 65 years were 0% and 6.7%, respectively. There were no significant risk factors related to death in the total population. On the other hand, in patients aged 65 years or older, however, high-energy fracture and high comorbidity index increased the risk of death after surgery by 6.9-fold and 1.9-fold, respectively.
Conclusion
The one-year mortality rate for the total patients was 3.9%, but the mortality rate for patients over 65 years of age increased to 6.7%. High-energy fractures and high comorbidity index were risk factors related to death after surgery for distal femur fractures in patients aged 65 years or older.
- 507 View
- 3 Download

Review Article
- Treatment of Scaphoid Fractures and Nonunions
- Wan-Sun Choi
- J Korean Fract Soc 2022;35(4):182-189. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.182
-
 Abstract
Abstract
 PDF
PDF - A scaphoid fracture is one of the most common types of wrist fractures, and if treatment is delayed, there is a high possibility of nonunion due to anatomical factors such as limited blood supply to the injured bone. Therefore, it is important to suspect a scaphoid fracture based on the mechanism of wrist injury and physical examination of the patient. A computed tomography scan or magnetic resonance imaging can also aid early diagnosis of the fracture. Stable acute fractures can be treated conservatively, but unstable fractures require surgical treatment, and percutaneous screw fixation is usually performed. Nonunions require bone grafts and are treated with non-vascularized bone grafts and screw fixation. However, if the nonunion is located at the proximal pole, a vascularized bone graft may be considered because there is a possibility of avascular necrosis. Pedicled vascularized and free vascularized medial femoral condyle bone grafts are mainly used in such cases. The treatment of a proximal pole nonunion with impaired blood flow remains controversial. There are conflicting opinions on whether a nonvascularized bone graft is sufficient or whether a vascularized bone graft is necessary.
- 666 View
- 6 Download

Original Articles
- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- Min Sung Kwon, Young Bok Kim, Gyu Min Kong
- J Korean Fract Soc 2022;35(4):162-168. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.162
-
 Abstract
Abstract
 PDF
PDF - Purpose
Trochanteric fixation nail advanced (TFNA) was modified to compensate for the shortcomings of proximal femoral nail antirotation-II (PFNA-II). The clinical and radiological outcomes of surgeries us-ing the PFNA-II and TFNA for femoral intertrochanteric fractures were compared.
Materials and Methods
Eighty-two patients who underwent surgeries using PFNA-II or TFNA were analyzed. Only those who were followed up for more than a year were enrolled. Bone union, shortening of the femoral neck, and the tip–apex distance of the intramedullary nail were compared in the radiological findings. Clinical outcomes, including the frequency of complications and gait ability (Koval score), were also assessed.
Results
The mean follow-up periods were 22 and 19 months for the PFNA-II and TFNA groups, re-spectively. In the PFNA-II group, two cases of femoral head cut-out and one case of varus collapse were observed. In the TFNA group, only one case of femoral head cut-out was observed; however, there was no significant difference in the frequency of complications between the two groups (p=0.37). Ad-ditionally, both the shortening of the femoral neck and the decrease in gait ability after surgery showed relative improvement in the TFNA group compared to the PFNA-II group; however, there was no sig-nificant difference between the two groups.
Conclusion
The use of both TFNA and PFNA-II was associated with satisfactory outcomes. In patients who underwent surgeries using TFNA, the recovery of gait ability, frequency of complications, and short-ening of the femoral neck were not significantly different from PFNA-II, suggesting that both are suitable instrument choices for intertrochanteric fracture treatment. However, the clinical significance must be further assessed using a larger group of patients over a longer follow-up period in future studies. -
Citations
Citations to this article as recorded by- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
Jee Young Lee, Gyu Min Kong
Journal of Orthopaedic Trauma.2025; 39(7): 352. CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef
- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
- 3,553 View
- 53 Download
- 2 Crossref

- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
- J Korean Fract Soc 2022;35(4):151-161. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.151
-
 Abstract
Abstract
 PDF
PDF - Purpose
Osteoporosis causes various fixation failures in patients with intertrochanteric fractures. This study aimed to investigate the effect of a demineralized bone matrix (DBM) for cancellous or cortical bone defects on internal fixation in older osteoporotic patients with intertrochanteric fractures.
Materials and Methods
Among patients with intertrochanteric fractures who underwent surgical treatment from January 2016 to December 2021 at a facility, 171 patients were AO/OTA type 31-A1 and type 2 fractures which are considered relatively stable. The patients were grouped based on DBM use (Group A: DBM use, Group B: DBM non-use), and their clinical and radiology results were analyzed retrospectively. The patients were then subdivided into Group A-a and -b after removing factors that could cause treatment failures, such as the reduction status and location of the helical blade, and then further subdivided (Group A-a-1/2/3/4 and Group B-b-1/2/3/4) according to cancellous or cortical bone defects that could accompany intertrochanteric fractures. The time to full weight-bearing (FWB) and Harris hip score (HSS) 3 months after surgery in these subgroups were investigated.
Results
There was no significant difference in the clinical radiology results and complications between Group A and Group B. However, the time to FWB (p<0.001) and HSS (p=0.029) were significantly superior in Group A. In Group A-a with DBM use, after removing the risk factors for intertrochanteric fracture failure, the time to FWB (p=0.055) was close to the significance level, and HSS (p=0.036) was significantly superior. In Group A-a-1 (cancellous defect only) and Group A-a-3 (cancellous and cortical defect), the time to FWB (p=0.088, 0.052) was close to the significance level, and the HSS (p=0.039, 0.018) was significantly superior when DBM was used.
Conclusion
In patients with intertrochanteric fractures of AO/OTA type 31-A2.3 or less, if stable reduction and firm fixation are achieved, selective DBM use may help early recovery after surgery.
- 453 View
- 2 Download

Review Articles
- Surgical Treatment of Distal Radius Fractures and Treatment of Common Accompanying Lesions
- Joo-Hak Kim
- J Korean Fract Soc 2022;35(3):120-127. Published online July 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.3.120
-
 Abstract
Abstract
 PDF
PDF - There have been major advances in the treatment of distal radius fractures over the past 20 years. Specifically, the development of the volar locking plate in 2001 and the subsequent improvements in its design and performance have enabled the treatment of distal radius fractures that were previously considered difficult to treat. The volar plate is used for fractures and shows good results with anatomical reduction and firm fixation. However, when trying to apply it to more complex fractures, there are still difficulties related to the unique anatomical structure of the distal radius, and there are also several factors that can impair joint function and cause pain after surgery. In this review, the factors to be considered to ensure better outcomes during ORIF (open reduction and internal fixation), and external fixation in the treatment of distal radial fractures are described. The review also details the common accompanying injuries and management methods.
- 735 View
- 18 Download

- Current Treatment of Calcaneal Fractures and Dislocation
- Dae Jin Nam, Sung Hyun Lee
- J Korean Fract Soc 2022;35(2):74-82. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.74
-
 Abstract
Abstract
 PDF
PDF - Calcaneal fractures are the most common fractures occurring in the tarsal bone. In the past, surgical treatments were not preferred because they were accompanied by severe comminution and soft tissue complications. In recent years, there have been great advancements in the treatment of calcaneal fractures owing to the development of new surgical techniques and instruments. However, a standard treatment method has not yet been established. In this review article, we summarize the latest information on the indications and treatment methods of calcaneal fractures.
- 523 View
- 15 Download

Original Articles
- Posterior Anti-Glide Plating for Supination External Rotation Type Lateral Malleolar Fractures: Clinical Comparison of Locking versus Non-Locking One-Third Semi-Tubular Plate Fixation
- Jun Young Lee, Yong Jin Cho, Dong Hyuk Cha, Hyun Bai Choi, Jung Ho Lee
- J Korean Fract Soc 2022;35(2):57-62. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose
The purpose of this study was to evaluate and compare the clinical and radiological outcomes between locking plates and non-locking plates using posterior anti-glide plating for supination external rotation type lateral malleolar fractures.
Materials and Methods
A total of 50 patients who underwent internal fixation of posterior anti-glide plating due to lateral malleolar fractures, classified as supination-external rotation (SER) as per the Lauge-Hansen classification system, at our hospital from January 2017 to November 2018 were retro-spectively evaluated. Patients were divided into two groups: 1/3 semi-tubular locking plate (24 patients) and 1/3 semi-tubular non-locking plate (26 patients). A radiographic assessment was performed after surgery to evaluate the time of bone union. The American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot functional score was measured after the surgery to evaluate the clinical outcomes.
Results
The two groups showed similar distributions in sex, age, height, body mass index, fracture pattern, and mean follow-up period. Complete bone union was obtained in all cases and the mean bone union time was 13.00±3.38 weeks in Group 1 and 12.92±3.26 weeks in Group 2 (p=0.87). The mean AOFAS score at 24 weeks was 95.66±2.86 in Group 1 and 95.84±2.79 in Group 2 (p=0.82). The mean AOFAS score at 48 weeks was 97.25±3.54 in Group 1 and 96.57±3.07 in Group 2 (p=0.47). Two cases of complications were observed in the non-locking plate group.
Conclusion
For the treatment of Lauge-Hansen SER type lateral malleolar fracture, internal fixation us-ing locking 1/3 semi-tubular plate and non-locking 1/3 semi-tubular plate are both favorable fixation methods.
- 347 View
- 2 Download

- Mortality-Related Risk Factors in Total Hip Arthroplasty for Femoral Neck Fractures in Elderly Patients
- Jae Sung Suh, Hyung Gon Ryu, Young Ju Roh, Dae Won Shin
- J Korean Fract Soc 2022;35(2):51-56. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.51
-
 Abstract
Abstract
 PDF
PDF - Purpose
Total hip arthroplasty (THA) using dual mobility components (DMC) is a reasonable surgical option for displaced femoral neck fractures in elderly patients, resulting in lower dislocation rates and improved stability. The purpose of this study was to investigate the clinical outcomes and risk factors responsible for mortality in elderly patients who were diagnosed with a displaced femoral neck fracture and had undergone DMC-THA.
Materials and Methods
Out of 147 cases of THA from December 2018 to June 2020, a total of 79 cases were enrolled in this study, with the following characteristics: (1) Garden stage III or IV, (2) over 75 years of age, and (3) over 1 year of follow-up. All the patients received DMC-THA surgery using the anterolateral approach.
Results
The mean follow-up period was 15.0±8.43 months and a total of one dislocation case was observed. The mortality rate was 17.7% (14/79), and it was especially higher in patients with a past medical history of malignancy (odds ratio [OR]=7.18, p=0.03) or a cognitive disorder such as dementia (OR=5.48, p=0.03). Preoperative low initial hemoglobin levels (OR=0.65, p=0.04) and low UCLA (Uni-versity of California at Los Angeles) score (OR=0.47, p=0.02) were also associated with mortality.
Conclusion
When considering THA as a treatment approach in elderly patients with a displaced femoral neck fracture, a high mortality rate is expected in patients with low preoperative hemoglobin levels or a history of malignancy or cognitive disorders. Hence, thorough monitoring and management should be undertaken before and after surgery. -
Citations
Citations to this article as recorded by- Comparison of Operation Time, Vital Signs, Bleeding Tendency, and Recovery Time Based on Anesthesia Methods in Patients Undergoing Hip Fracture Surgery
Je Bog Yoo, Woo Young In, Chang Ok Pyo, Jeung Hee Kwon, Min Ji Lee, Kwang Hee Kim, Kyoung Ok Kim, Mi Yu
Journal of PeriAnesthesia Nursing.2025;[Epub] CrossRef
- Comparison of Operation Time, Vital Signs, Bleeding Tendency, and Recovery Time Based on Anesthesia Methods in Patients Undergoing Hip Fracture Surgery
- 427 View
- 26 Download
- 1 Crossref

Case Report
- Recurrent Treatment Failure in Vancouver Classification Type C Periprosthetic Fractures around a Well Fixed Short Femoral Stem
- Byeong Yeol Choi, Hong-Man Cho, Jiyeon Park
- J Korean Fract Soc 2022;35(1):16-20. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.16
-
 Abstract
Abstract
 PDF
PDF - A short femoral stem (type 1 cementless stem) is being increasingly used to perform total hip arthroplasty; however, various types of intra- or postoperative periprosthetic fractures have been reported in recent times. A 66-year-old woman with a history of bilateral total hip arthroplasties using a type 1B femoral stem was admitted 2 months post-operation for a Vancouver type C periprosthetic fracture. She underwent open reduction and internal fixation; however, we observed recurrent non-union and plate breakage at the same site. In this case report, we discuss the factors associated with treatment failure in patients with a Vancouver type C periprosthetic fracture following type 1 femoral stem im-plantation.
- 361 View
- 0 Download

Original Article
- Comparing Outcomes of Retrograde Intramedullary Nail and Locking Plate Fixation in Distal Femoral Fractures
- Byung-Ho Yoon, Bo Kwon Hwang, Hyoung-Keun Oh, Suk Kyu Choo, Jong Min Sohn, Yerl-Bo Sung
- J Korean Fract Soc 2021;34(4):131-136. Published online October 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.4.131
-
 Abstract
Abstract
 PDF
PDF - Purpose
We compared the radiological and clinical results of fixation for distal femoral fracture (DFF) using a locking compression plate (LCP) or a retrograde intramedullary nail (RIN).
Materials and Methods
From October 2003 to February 2020, 52 cases of DFF with a minimum 1-year follow-up (with a mean follow-up of 19.1 months) were included: 31 were treated with LCP and 21 with RIN. The operation time, blood loss, and hospitalization period were compared, and the incidence of postoperative nonunion, malunion, delayed union and metal failure and other post-operative complications were evaluated and compared.
Results
There was no significant difference in the operating time between the two groups, but the mean blood loss was significantly higher in the LCP group (LCP 683.5 ml vs RIN; 134.9 ml; p=0.015). In 49 out of 52 cases, bone union was achieved without additional surgery in an average of 6.8 months, and a complete union was achieved after additional surgery in three cases of nonunion (LCP 2 cases vs RIN 1 case; p=0.065). One case of malunion and superficial infection was confirmed in each group.
Conclusion
Internal fixation using LCP and RIN give good outcomes with a low complication rate and can therefore be considered useful surgical treatments for DFF.
- 467 View
- 6 Download

Case Report
- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture
- Soon Ho Huh, Hong-Man Cho, Ji-Yeon Park
- J Korean Fract Soc 2021;34(3):112-116. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.112
-
 Abstract
Abstract
 PDF
PDF - A helical blade type of hip screw is used widely for the operative management of femoral trochanteric fractures. A 73-year-old female patient was admitted for femoral trochanteric fracture AO/OTA type 31A2.2. A helical blade locking sleeve dissembled 18 weeks after surgery did not achieve accurate reduction. The patient underwent bipolar hip hemiarthroplasty because the fracture reduction was lost, and it was impossible to remove the remaining helical blade without bone loss. The authors report this case of a rare complication of helical blade.
- 548 View
- 3 Download

Original Article
- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
- J Korean Fract Soc 2021;34(3):105-111. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.105
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the clinical and radiological outcomes of TFNA (Trochanteric Fixation NailAdvanced; Depuy Synthes) for the treatment of proximal femur fractures.
Materials and Methods
This was a retrospective study of 64 patients diagnosed with a proximal femur fracture from January 2019 to November 2019. The patient’s demographic data, preoperatively and postoperatively Koval grade, modified Harris hip score, EQ-5D (Euro-Qol-5 Dimension), sliding and advancement of the blade, radiologic outcome, and complications were investigated.
Results
Fifty patients were available for evaluation at one year postoperatively. The patients reported the following: the Koval grade decreased after surgery; the modified Harris hip score decreased from 78.56±8.88 to 72.74±6.59 (p=0.149); the mean EQ-5D decreased from 0.75±0.09 to 0.72±0.06 (p=0.000). Satisfactory reduction was achieved on a postoperative radiographic examination in 47 patients in six months. Complications occurred in seven cases.
Conclusion
TFNA is considered an appropriate implant for treating intertrochanteric fractures of the femur with a minimum follow-up of one year. -
Citations
Citations to this article as recorded by- Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
Ramprasad Jasti, Prithvi Mohandas, Mahesh K Ragavan, Sunil D Magadam, Umesh Kannadasan
Cureus.2025;[Epub] CrossRef - GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
Seungcheol Kwon, Minjae Lee, Heeyeon Lee, Jihyo Hwang
Journal of Clinical Medicine.2023; 12(21): 6720. CrossRef - Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef
- Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
- 1,076 View
- 19 Download
- 3 Crossref

Case Report
- Injury of the Ascending Branch of the Lateral Femoral Circumflex Artery Caused by a Spike of the Displaced Lesser Trochanter in an Intertrochanteric Femoral Fracture - A Case Report -
- Soon Ho Huh, Hong-Man Cho, Jiyeon Park
- J Korean Fract Soc 2021;34(2):71-75. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.71
-
 Abstract
Abstract
 PDF
PDF - Although vascular injuries associated with femoral intertrochanteric fractures have been reported infrequently, bleeding due to vascular injury can lead to severe complications that can be potentially life and limb-threatening. The authors report a case of an injury of the ascending branch of the lateral femoral convolutional artery in a patient who underwent surgical treatment for a femoral intertrochanteric fracture. Vascular injury occurred due to the sharp margin of displaced lesser trochanter five weeks after surgery. Percutaneous transcatheter embolization was done and improved without additional complications. Therefore, the surgeons need to be aware of possible associated vascular injuries caused by displaced lesser trochanter fragments in femoral intertrochanteric fractures.
-
Citations
Citations to this article as recorded by- Delayed Deep Femoral Artery Injury Secondary to Migrated Lesser Trochanter Fragment After Intertrochanteric Fracture Fixation: A Case Report and Updated Literature Review
Slavko Čičak, Josip Kocur, Vedran Farkaš, Petra Čičak, Stjepan Ištvanić, Marko Lovrić, Marko Perić, Nenad Koruga, Tomislav Ištvanić
Geriatric Orthopaedic Surgery & Rehabilitation.2025;[Epub] CrossRef - Vascular Complications Following Trans-Trochanteric Fracture: Case Report and Literature Review
Robert Bot, Adrian Tirla, Simona Daniela Cavalu
Reports.2025; 8(4): 191. CrossRef
- Delayed Deep Femoral Artery Injury Secondary to Migrated Lesser Trochanter Fragment After Intertrochanteric Fracture Fixation: A Case Report and Updated Literature Review
- 595 View
- 4 Download
- 2 Crossref

Original Articles
- Comparison of Reductions of Left and Right Proximal Portions of Intertrochanteric Fractures Treated by Intramedullary Nailing
- Hyun Cheol Oh, Joong Won Ha, Yung Park, Sang Hoon Park, Han Kook Yoon
- J Korean Fract Soc 2021;34(2):64-70. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.64
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the effect of lag screw insertion on proximal fragments by separating the right and left sides of intertrochanteric fractures in elderly patients that underwent intramedullary nailing.
Materials and Methods
Patients aged ≥65 years that underwent intramedullary nailing after a diag-nosis of intertrochanteric fractures during the period February 2012 to May 2016 were included in the study. The subjects were divided into right and left side groups. The effect of the clockwise rotational force generated when a lag screw was inserted on the proximal fragment was evaluated in both groups.
Results
In the right and left groups, most proximal fragments were located in the intramedullary canal after surgery (45 cases [75.0%] and 67 cases [73.6%], respectively). Clockwise rotation due to lag screw placement in the right group occurred in two cases (3.3%), which both showed internal rotation, and in four cases (4.4%) in the left group, all of which showed external rotation.
Conclusion
After intramedullary nailing of intertrochanteric fractures in elderly patients, proximal fragments were mostly located in the intramedullary cavity. The results obtained confirmed that the clockwise rotational force generated by lag screw insertion did not affect left or right sides. -
Citations
Citations to this article as recorded by- Which side should be taken care of when positioning a lag screw in intertrochanteric femoral fracture: right or left?
Min Uk Do, Kyeong Baek Kim, Sang-Min Lee, Hyun Tae Koo, Won Chul Shin
European Journal of Trauma and Emergency Surgery.2025;[Epub] CrossRef - Midterm Outcomes of Intramedullary Fixation of Intertrochanteric Femoral Fractures Using Compression Hip Nails: Radiologic and Clinical Results
You-Sung Suh, Jae-Hwi Nho, Min Gon Song, Dong Woo Lee, Byung-Woong Jang
Clinics in Orthopedic Surgery.2023; 15(3): 373. CrossRef
- Which side should be taken care of when positioning a lag screw in intertrochanteric femoral fracture: right or left?
- 666 View
- 3 Download
- 2 Crossref

- Comparison of the U-Blade Gamma3 Nail and the Zimmer Natural Nail for the Treatment of Intertrochanteric Fracture
- Jae Sung Suh, Hyung-Gon Ryu, Young Ju Roh, Dae Won Shin, Sang-Min Kim
- J Korean Fract Soc 2021;34(2):57-63. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study was performed to compare the clinical results and radiological follow-up differences between intertrochanteric fractures treated with the U-blade Gamma3 nail or the Zimmer natural nail (ZNN).
Materials and Methods
The medical records of 129 cases diagnosed with an intertrochanteric frac-ture (90 cases of U-blade Gamma3 nail, 39 cases of ZNN) from July 2015 to December 2018 were reviewed. Patients were assigned to a U-blade Gamma3 nail (n=39) or a ZNN (n=39) group. To reduce selective bias, groups were subjected to Propensity score matching by age, body mass index, bone mineral density, and fracture type. Patients that met the following criteria were excluded; age <65 years, non-ambulatory, high energy or pathologic fracture, and a follow-up of <6 months. Operation times, estimated blood losses, preoperative and postoperative Koval grades, Harris hip score and radiological lag screw positions in the femoral head, reduction quality, cut-out, tip-apex distance (TAD), lag screw sliding distances, and times to union were compared.
Results
Clinical results were similar in the two groups, but lag screw TAD was significantly greater in Ublade Gamma3 nail group (23.4 mm vs. 21.0 mm) (p=0.042). One case of cut-out occurred in the Ublade Gamma3 nail group, but no other nail-related postoperative complication was noted.
Conclusion
No significant difference was observed between the outcomes of U-blade Gamma3 nail or ZNN treatments of intertrochanteric fractures. We conclude that the U-blade confers no specific advan-tage.
- 1,421 View
- 8 Download

Review Article
- Pediatric Femoral Neck Fracture
- Joo Hyung Han, Hoon Park
- J Korean Fract Soc 2021;34(1):34-43. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.34
-
 Abstract
Abstract
 PDF
PDF - Pediatric femoral neck fracture is an uncommon injury with a high complication rate, regardless of the appropriate diagnosis and management. The bony anatomy and blood supply of the proximal femur in a skeletally immature patient differ from those in adult patients. Generally, these fractures result from high-energy trauma, but pathologic hip fractures also occur, usually from low-energy trauma. Pediatric femoral neck fractures are categorized using the Delbet classification system. This classification guides management and aids clinicians in determining the risk of avascular osteonecrosis. The ideal surgical treatment is determined by the fracture type and the age of the patient. Reduction, which is achieved using a closed or open procedure, combined with stable fixation and/or cast immobilization, is recommended for most of these fractures. Anatomical reduction within 24 hours from the injury may result in a good surgical outcome. Although the effects of capsular decompression after reduction and fixation have not been established, decompression is easy to perform and may reduce the risk of avascular necrosis. Despite appropriate management, osteonecrosis can occur after all types of pediatric femur neck fractures. Other complications include coxa vara, nonunion, and premature physeal arrest.
- 1,369 View
- 29 Download

Original Article
- Treatment of Proximal Femur Fracture with a Newly Designed Nail: Trochanteric Fixation Nail-Advanced (TFNA)
- Jae Youn Yoon, Ji Wan Kim
- J Korean Fract Soc 2020;33(4):189-195. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.189
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the clinical results and implant safety of a newly developed implant, Trochanteric Fixation Nail-Advanced (TFNA; DePuy Synthes), in the treatment of proximal femur fractures.
Materials and Methods
This was a retrospective cohort study of 26 patients diagnosed with proximal femur fracture and treated surgically with TFNA. The patients’ demographic data, surgical data, radiologic findings, and functional outcomes, including complications, were evaluated.
Results
The mean age of the patients was 71.2 years (95% confidence interval [CI], 68.2-74.2); 65.4% were female. The mean Carlson comorbidity index score was 5.4, and the mean Koval grade before fracture was 2.1. Fracture classification included four cases of AO/OTA 31.A1, nine cases of A2, six cases of A3, and seven cases of 32A including six cases of atypical femoral fractures. The mean operating time was 53.3 minutes (95% CI, 43.6-63.1). There were no early postoperative complications, such as postoperative infection, deep vein thrombosis, pulmonary embolism, or in-hospital death, except one case of pneumonia. The mean Koval score at the postoperative six-month follow-up was 2.9. EuroQol-5 Dimension (EQ-5D) increased from 0.05 to 0.54 after three months and 0.72 at six months postoperatively. Bone union was observed in all cases with a mean union time of 12.9 weeks. No implant failure occurred, and no cases required secondary revision surgery.
Conclusion
A new intramedullary nail system, TFNA, showed excellent outcomes and safety in the surgical treatment of proximal femur fractures. -
Citations
Citations to this article as recorded by- Intermediate Length Cephalomedullary Nails in Proximal Femoral Fractures: Review of Indications and Outcomes
Daniel Scott Horwitz, Ahmed Nageeb Mahmoud, Michael Suk
Journal of the American Academy of Orthopaedic Surgeons.2025; 33(19): 1071. CrossRef - Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
Ramprasad Jasti, Prithvi Mohandas, Mahesh K Ragavan, Sunil D Magadam, Umesh Kannadasan
Cureus.2025;[Epub] CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef - Prospective randomized multicenter noninferiority clinical trial evaluating the use of TFN-advancedTM proximal femoral nailing system (TFNA) for the treatment of proximal femur fracture in a Chinese population
Lidan Zhang, Zhijun Pan, Xiaohui Zheng, Qiugen Wang, Peifu Tang, Fang Zhou, Fan Liu, Bin Yu, Frankie K. L. Leung, Alex Wu, Suzanne Hughson, Zhuo Chen, Michael Blauth, Anthony Rosner, Charisse Sparks, Manyi Wang
European Journal of Trauma and Emergency Surgery.2023; 49(3): 1561. CrossRef - Risk of shortening in operatively treated proximal femur fractures with cephalomedullary nails with dynamically versus statically locked helical blades
Nathan Cherian, Lasun Oladeji, Cole Ohnoutka, Dan Touhey, Madeline Sauer, Kyle A. Schweser, Mauricio Kfuri, James L. Cook, Gregory J. Della Rocca, Brett D. Crist
Injury.2023; 54(2): 669. CrossRef - GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
Seungcheol Kwon, Minjae Lee, Heeyeon Lee, Jihyo Hwang
Journal of Clinical Medicine.2023; 12(21): 6720. CrossRef - Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef - Analysis of Clinical and Functional Outcomes according to the Blood Sugar Control Status at the Time of Ankle Fractures Resulting from Rotational Injuries
Jun Young Lee, Dong Seop Lim, Seung Hyun Lee, Seo Jin Park
Journal of the Korean Fracture Society.2022; 35(4): 135. CrossRef - Conventional versus helical blade screw insertion following the removal of the femoral head screw: a biomechanical evaluation using trochanteric gamma 3 locking nail versus PFN antirotation
Hong Man Cho, Kwang Min Park, Tae Gon Jung, Ji Yeon Park, Young Lee
BMC Musculoskeletal Disorders.2021;[Epub] CrossRef - Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef
- Intermediate Length Cephalomedullary Nails in Proximal Femoral Fractures: Review of Indications and Outcomes
- 2,399 View
- 23 Download
- 10 Crossref

Review Article
- Current Concepts of Bone Healing
- Dong Hun Suh, Bong Mo Koo, Jong Woo Kang
- J Korean Fract Soc 2020;33(3):171-177. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.171
-
 Abstract
Abstract
 PDF
PDF - Bone injuries induce an inflammatory response that promotes bone healing. On the other hand, an aberrant process, where inflammation becomes chronic, can inhibit the healing of injured bone. At the first stage of the bone healing process, inflammatory cells, such as neutrophils and macrophages, are assembled and secrete various cytokines, chemokines, and growth factors. During callus formation, cells differentiated from mesenchymal stem cells, such as osteoblasts and chondrocytes, play leading roles in bone healing. Currently, various treatment modalities have been developed through the known mechanism of bone healing, and the clinical outcomes of bone defect and fracture nonunion have been good.
- 2,264 View
- 87 Download

Case Report
- Rendezvous Surgery for Peri-Implant Fractures around Locking Compression Plate on Anterolateral Bowed Femur - A Case Report -
- Hong Man Cho, Jiyeon Park
- J Korean Fract Soc 2020;33(3):159-163. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.159
-
 Abstract
Abstract
 PDF
PDF - An 84-year-old female visited with an intertrochanteric femoral fracture. The patient had undergone an open reduction and internal fixation with a compressive plate and elastic nail in an ipsilateral atypical diaphyseal femoral fracture in the past. Compressive plate and elastic nail remained, and anterolateral bowing was presented. To treat the periprosthetic trochanteric fracture, a proximal femoral nail was used without removing the previously inserted compressive plate. Under the “rendezvous” technique, using a combination of fixating intramedullary nail and compressive plate simultaneously, the distal screw was fixed, and a femoral head lag screw was inserted after reducing the fracture. Complete union of the fracture was achieved 16 months after the operation, and a decrease in mobility function was not found postoperatively. The authors report this case for the “rendezvous” technique as a treatment option for elderly patients with periprosthetic trochanteric fractures, who had previously undergone surgical treatment for ipsilateral atypical diaphyseal femoral fractures with anterolateral bowing.
- 476 View
- 3 Download

Original Article
- Does the Use of a Silicone Ring Tourniquet Help Reduce Bleeding in the Minimally Invasive Internal Fixation with Locking Plate for Distal Femoral Fractures?
- Ki-Bong Park, Hong-Ki Jin, Il-Yeong Hwang, Sung-Who Chang, Sung-Cheon Na
- J Korean Fract Soc 2020;33(3):148-153. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.148
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the usefulness of a silicone ring tourniquet by analyzing the changes in the perioperative hemoglobin (Hb) levels or amount of perioperative bleeding compared to those of a pneumatic tourniquet or no usage during minimally invasive plate fixation for distal femoral fractures.
Materials and Methods
From January 2017 to December 2019, 30 patients who underwent minimally invasive plate fixation using a locking compression plate for distal femoral fractures were evaluated and classified as a silicone ring tourniquet (Group 1), a pneumatic tourniquet (Group 2), and no usage (Group 3). The variables for analysis were age, sex, preoperative Hb (preHb), postoperative 72-hour Hb (postHb), differences between preHb and postHb (preHb-postHb), amount of intraoperative and overall transfusion, estimated unit of transfusion corrected by preHb-postHb and total transfusion (Hb-lost), amount of intraoperative and postoperative and total bleeding. One-way ANOVA was used to identify the differences between the groups.
Results
The age, sex, operation time, preHb, preHb-postHb, amount of intraoperative and overall transfusion and Hb-lost were similar in the two groups. The amount of intraoperative bleeding was significantly lower in Group 1 than Group 3 (p=0.004), but there was no difference in the amount of postoperative and total bleeding between the two groups.
Conclusion
The use of a silicone ring tourniquet in the minimally invasive plate fixation for distal femoral fractures decreased the amount of intraoperative bleeding compared to no use of a tourniquet. -
Citations
Citations to this article as recorded by- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
Tae sung Lee, Kwan Kyu Park, Byung Woo Cho, Woo-Suk Lee, Hyuck Min Kwon
BMC Musculoskeletal Disorders.2023;[Epub] CrossRef
- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
- 945 View
- 6 Download
- 1 Crossref

Review Article
- Periprosthetic Fractures following Total Knee Arthroplasty
- Byung Hoon Lee, Jae Ang Sim
- J Korean Fract Soc 2020;33(1):52-61. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.52
-
 Abstract
Abstract
 PDF
PDF - Recently, as the elderly population increases, the incidence of total knee arthroplasty has increased, with a concomitant increase in the frequency of periprosthetic fractures. To determine the treatment plan for fractures, the treatment method should be determined by the patient's age, osteoporosis, fixation status of the implant, and type of fracture. In recent years, operative treatment with reduction and stable fixation, rather than non-operative treatment, was used to promote early joint movement and gait. On the other hand, it is necessary to select an appropriate operative method to reduce complications of surgery, such as nonunion and infection, and expect a good prognosis. In this review, periprosthetic fractures were divided into femur, tibia, and patella fractures, and their causes, risk factors, classification, and treatment are discussed.
- 975 View
- 20 Download

Case Report
- Concurrent Posterolateral Corner Injury Associated with a Schatzker Type 2 Tibial Plateau Fracture: A Case Report
- Jae Cheon Sim, Choong Won Jung, Tae Seok Nam
- J Korean Fract Soc 2020;33(1):27-31. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.27
-
 Abstract
Abstract
 PDF
PDF - Isolated posterolateral corner (PLC) injury associated with a Schatzker type 2 fracture is a very rare combination of injuries. A male who was driving a motor vehicle was injured after a collision accident. The plain radiographs and computed tomography scans of the knee showed a Schatzker type 2 fracture of the tibial plateau, mostly in the anterolateral portion of tibial plateau, and an avulsion fragment on the fibular tip. Magnetic resonance imaging showed no injury to cruciate ligaments, medial collateral ligament, or any meniscal injury. We performed an open reduction operation and internal fixation for treating the fracture. Six months later, he complained of instability. At 11 months later after initial operation, we performed the second operation for stabilizing the PLC. We present here a rare case of an isolated PLC injury associated with a Schatzker type 2 fracture. We discuss the mechanism of injury and review similar cases.
- 905 View
- 4 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


