Articles
- Page Path
- HOME > J Korean Fract Soc > Volume 37(2); 2024 > Article
- Original Article Comparison of the Radiological Outcomes of an Anatomical Quadrilateral Surface Plate with a Pelvic Reconstruction Plate in Acetabulum Fractures
- Sung Hyun Yoon, Hee Gon Park, Dong Uk Lee
-
Journal of The Korean Orthopaedic Trauma Association 2024;37(2):95-101.
DOI: https://doi.org/10.12671/jkfs.2024.37.2.95
Published online: April 30, 2024
- 872 Views
- 10 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
This study compared the radiological outcomes of fixation using an anatomical quadrilateral surface plate with those using a traditional pelvic reconstruction plate for fractures involving the quadrilateral surface or superomedial wall of the acetabulum.
Materials and Methods
From 2015 to 2022, 47 patients who met the inclusion and exclusion criteria were analyzed retrospectively. Internal fixation of an acetabular fracture was achieved with a pelvic reconstruction plate (n=28) or an anatomical quadrilateral surface plate (n=19). The ability to achieve immediate postoperative anatomical reduction and the long-term outcomes were assessed by confirming the arthritic changes. Immediate postoperative reduction quality and long-term radiological outcomes for post-traumatic arthritis were assessed using the Matta scoring system on standard radiographs.
Results
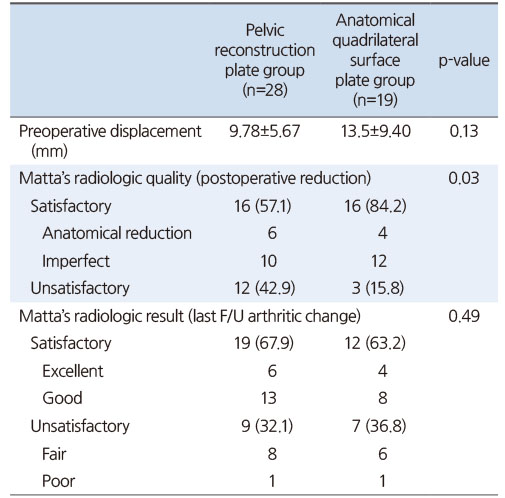
The assessment of immediate postoperative reduction in the pelvic reconstruction plate group was satisfactory in 16 patients (57.1%) and unsatisfactory in 12 patients (42.9%). In the anatomical quadrilateral surface plate group, the results were satisfactory in 16 patients (84.2%) and unsatisfactory in 3 patients (15.8%). When evaluating over an extended follow-up period in the pelvic reconstruction plate group, 19 patients (67.9%) demonstrated satisfactory, while 9 patients (32.1%) had unsatisfactory outcomes. In the anatomical quadrilateral surface plate group, 12 patients (63.2%) achieved satisfactory, and 7 patients (36.8%) had unsatisfactory outcomes. The immediate postoperative reduction quality was superior in the anatomical quadrilateral surface plate group (p=0.03). Comparing longterm results, the anatomical quadrilateral surface plate group did not have statistically more favorable outcomes (p=0.49).
Conclusion
In this study, the anatomical quadrilateral surface plate achieved sufficiently good radiological results without significant difference from the existing pelvic reconstruction plate. It was concluded that it is a useful option that can replace the existing metal plate in the selection of surgery for acetabular fractures.
Published online Apr 24, 2024.
https://doi.org/10.12671/jkfs.2024.37.2.95
Abstract
Purpose
This study compared the radiological outcomes of fixation using an anatomical quadrilateral surface plate with those using a traditional pelvic reconstruction plate for fractures involving the quadrilateral surface or superomedial wall of the acetabulum.
Materials and Methods
From 2015 to 2022, 47 patients who met the inclusion and exclusion criteria were analyzed retrospectively. Internal fixation of an acetabular fracture was achieved with a pelvic reconstruction plate (n=28) or an anatomical quadrilateral surface plate (n=19). The ability to achieve immediate postoperative anatomical reduction and the long-term outcomes were assessed by confirming the arthritic changes. Immediate postoperative reduction quality and long-term radiological outcomes for post-traumatic arthritis were assessed using the Matta scoring system on standard radiographs.
Results
The assessment of immediate postoperative reduction in the pelvic reconstruction plate group was satisfactory in 16 patients (57.1%) and unsatisfactory in 12 patients (42.9%). In the anatomical quadrilateral surface plate group, the results were satisfactory in 16 patients (84.2%) and unsatisfactory in 3 patients (15.8%). When evaluating over an extended follow-up period in the pelvic reconstruction plate group, 19 patients (67.9%) demonstrated satisfactory, while 9 patients (32.1%) had unsatisfactory outcomes. In the anatomical quadrilateral surface plate group, 12 patients (63.2%) achieved satisfactory, and 7 patients (36.8%) had unsatisfactory outcomes. The immediate postoperative reduction quality was superior in the anatomical quadrilateral surface plate group (p=0.03). Comparing long-term results, the anatomical quadrilateral surface plate group did not have statistically more favorable outcomes (p=0.49).
Conclusion
In this study, the anatomical quadrilateral surface plate achieved sufficiently good radiological results without significant difference from the existing pelvic reconstruction plate. It was concluded that it is a useful option that can replace the existing metal plate in the selection of surgery for acetabular fractures.
초록
목적
이 연구는 비구 내 사변형면 혹은 상내측 벽을 포함하는 골절에 대한 해부학적 사변형면 금속판과 골반 재건 금속판을 이용한 수술의 방사선학적 결과를 비교하기 위함이다.
대상 및 방법
비구 골절에 대한 내고정술에서 해부학적 사변형면 금속판과 골반 재건 금속판의 효과를 비교하기 위해 2015년 8월부터 2022년 10월까지 수술을 받은 총 47명의 환자들의 수술 후 방사선학적 결과를 평가했다.
결과
수술 직후 골절의 정복 정도를 평가할 때 해부학적 사변형면 금속판을 사용한 군이 골반 재건 금속판을 사용한 군에 비해 더 좋은 결과를 보였다(p=0.03). 그러나 수술 후 최소 6개월 이후에 외상 후 관절염을 평가한 방사선학적 결과는 두 군 간에 유의미한 차이가 없었다.
결론
이 연구에서 해부학적 사변형면 금속판은 기존의 골반 재건 금속판과 유의한 차이 없이 충분히 좋은 방사선학적 결과 수치를 얻었다. 비구 골절의 수술의 선택에서 기존의 금속판을 대치할 수 있는 유용한 선택지라는 결론을 얻었다.
Introduction
The involvement of the quadrilateral surface in acetabulum fractures has been considered as an important factor contributing to the complexity of surgical reconstruction.1) The acetabular fracture in the geriatric population is prone to the fracture with involvement of quadrilateral surface comminution, medialization of the femoral head, and superomedial roof impaction.2,3,4,5) These fracture characteristics have been associated with poorer patient outcomes and an increased likelihood of conversion to total hip arthroplasty but the principles of treatment for reduction and preservation of fixation have not been established.6,7,8,9,10) Because it is located on the inner surface of the acetabulum, where the position is deep, and the bone quality is thin, and it is adjacent to a large number of peripheral nerves and blood vessels,11) various surgical approaches with direct and indirect reduction techniques and implants have been used for reduction and fixation. Recently options available for surgical fixation to address the quadrilateral surface fracture or superomedial displaced fracture included a combination of suprapectineal reconstruction plates and column lag screw fixation or buttress screw fixation.12,13,14,15,16,17) Anatomical quadrilateral surface plate have been developed to buttress the quadrilateral plate in the management of these challenging, which a design can help in the reduction and fixation of acetabulum fractures.18) In the literatures, it had shown that quadrilateral surface buttress plating is biomechanically comparable to conventional fixation methods as measured by stiffness and ultimate strength, further validating its clinical use.19,20,21)
The aim of this study is to compare the radiological outcome of fixation strategies with anatomical quadrilateral surface plate and traditional pelvic reconstruction plate for acetabular fracture involving quadrilateral surface or superomedial wall of acetabulum.
Materials and Methods
We performed a retrospective analysis of prospectively collected data from patients with acetabular fractures performed at our institution. This study received approval from the Institutional Review Board (IRB) of Dankook University Hospital (IRB No. 2024-04-006) and the written informed consent was waived by the IRB due to the retrospective nature of the study. From August 2015 and October 2022, among 118 patients that performed internal fixation for acetabular fracture, 47 patients who met inclusion and exclusion criteria were retrospectively analyzed. Inclusion criteria were fractures involving quadrilateral surface in acetabulum. And patients treated with a procedure using the Stoppa approach and had at least 6 months of follow-up after surgery were included. Exclusion criteria were patients with a history of ipsilateral hip fracture or surgery and previous degenerative arthritis.
Of the 60 patients who met the inclusion criteria, 8 patients who were lost to follow-up, and 5 patients who had other surgical approach (ilioinguinal approach) were excluded. Finally, only 47 patients enrolled in the study. Of these patients, 28 patients (24 males, 4 females) with the mean age of 53.2 years (range, 16-81 years) were treated with pelvic reconstruction plate and 19 patients (17 males, 2 females) with mean age of 57.1 years (range, 29-84 years) were treated with anatomical quadrilateral surface plate. Mean follow-up duration was 24.9 months (range, 6-71 months) in pelvic reconstruction plate group, and 14.0 months (range, 6-34 months) in anatomical quadrilateral surface plate group. Demographic data, mechanism of trauma, associated injuries, time to surgery and surgery time were obtained from the patients’ medical records for comparison with the two plates.
Preoperatively, three standard plain radiographs including anteroposterior (AP) pelvis, obturator oblique, and iliac oblique views were obtained along with computed tomography (CT) scans to classify fracture according to Letournel and Judet’s classification system (type of acetabular fracture).22) On the basis of this classification, 22 patients had associated both column fractures while 18 patients had anterior column fractures and 7 patients had anterior column-posterior hemitransverse fractures. Quality of immediate postoperative reduction was evaluated and graded as anatomical (0 to 1 mm of displacement), imperfect (2 to 3 mm displacement) or poor (more than 3 mm displacement) according to the residual displacement as defined by the Matta classification.6) We divided into satisfactory group for anatomical and imperfect reduction and unsatisfactory group. All patients were followed in the outpatient clinic at 6 months after surgery and yearly and follow-up pelvis AP, iliac oblique and obturator oblique radiographs were obtained for radiologic evaluation. The evaluation of radiological outcome performed on last follow-up standard pelvic radiograph at least 6 months by the basis of the Matta criteria was as follows: excellent (normal-appearing hip joint), good (mild changes with minimal sclerosis and joint narrowing <1 mm), fair (intermediate changes with moderate sclerosis and joint narrowing <50%), and poor (advanced changes).23) Likewise as above, we divided into satisfactory group for excellent and good long-term outcome and unsatisfactory group for fair and poor long-term outcome.
All operations were performed by one hip and pelvis trauma surgeon with an experience of >20 years in pelvicacetabular fractures. The decision to proceed with acetabular internal fixation was made by taking into consideration, age, comorbidities, bone quality, pre-existing osteoarthritis and fracture characteristics.
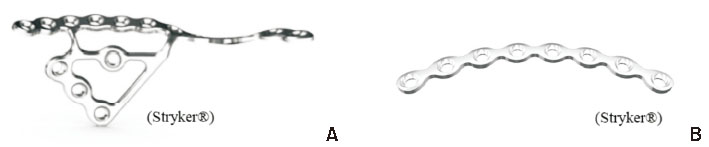
The modified Stoppa approach, as described by Cole and Bolhofner,24) was used in all patients. Internal fixation was done using either anatomical quadrilateral surface plate (Stryker®) and pelvic reconstruction plate (Stryker®) (Fig. 1).
Fig. 1
(A) Anatomical quadrilateral surface plate (Stryker®). (B) Pelvic reconstruction plate (Stryker®).
This was undertaken using IBM SPSS Statistics software (ver. 27.0; IBM Corp.). Descriptive statistics were used to describe the patients’ variables and radiological outcomes. Continuous variables between the groups were compared using Student’s t-test or analysis of variance, as appropriate. Categorical variables were analyzed using the chi-square test or Fisher’s exact test, as appropriate. Statistical significance was set at p<0.05.
Results
In comparing general demographic data between the two groups (pelvic reconstruction plate vs anatomical quadrilateral surface plate), there were no statistically significant differences such as age, sex, injury mechanisms, time to surgery (Table 1). Mean age was 53.2 years in the pelvic reconstruction plate group compared to 57.1 years in the anatomical quadrilateral buttress plate group (p=0.44). There were no sex differences (male/female: 24/4 vs 17/2) (p=0.54) or differences in mechanism of injury with regards low (6 vs 5) or high (22 vs 14) energy (p=0.48). The fracture patterns were similar between groups (p=0.05). All patients were followed up for a minimum of 6 months with a mean follow-up period of 20.5 months (6-71 months) and no differences between two group (p=0.14). The mean operative time was 128.3±33.2 minutes, there was no difference in operative time (130.5±36.8 vs 124.8±28.7) (p=0.57).
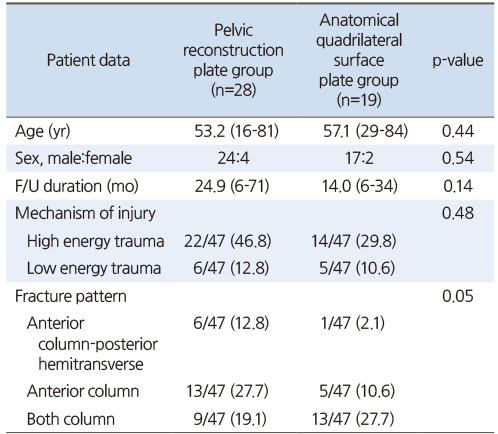
Table 1
Demographic Data
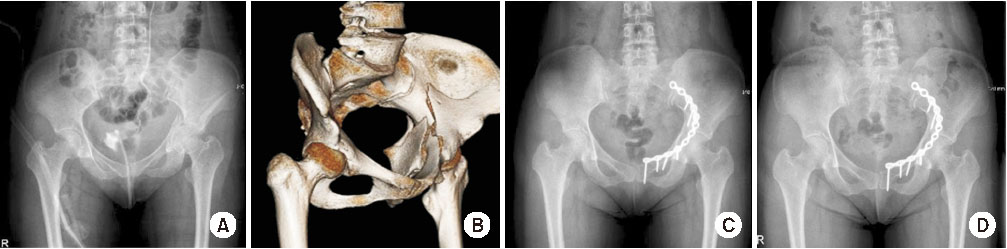
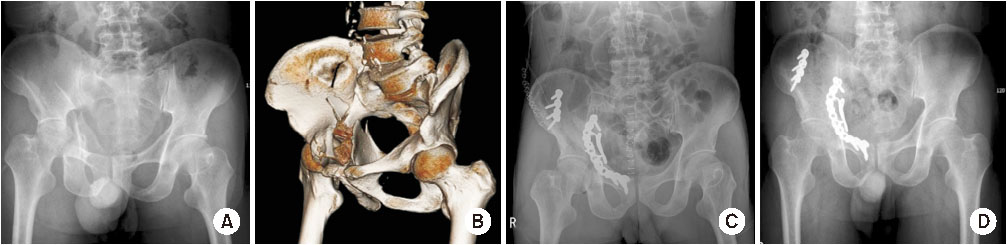
The quality of immediate postoperative reduction in the pelvic reconstruction plate group, it was satisfactory in 16 patients and unsatisfactory in 12 patients, whereas in the anatomical quadrilateral surface group was satisfactory (anatomical/imperfect) in 16 patients and unsatisfactory in 3 patients (Fig. 2,3). The long-term radiological results at least 6 months of the pelvic reconstruction plate group, there were 6 excellent cases, 13 good cases, 8 fair cases, and 1 poor case. In the anatomical quadrilateral surface plate group there were excellent in 4 cases, good in 8 cases, fair in 6 cases, and poor in 1 case. Only 2 poor cases with 1 patient from each plate group resulted in total hip arthroplasty at 1 year after surgery. Complications such as deep infection, surgical site infection or venous thromboembolism were not reported.
Fig. 2
Case A was a 34-year-old female patient. Preoperative X-ray and three-dimensional computed tomography (3D-CT) of the pelvis confirmed both column fractures. (A) Pelvis anteroposterior (AP) radiograph preoperatively. (B) 3D-CT, superomedially displaced acetabular fracture. (C) Pelvis AP radiograph immediate postoperative. (D) Pelvis AP radiograph after one year fixed with pelvic reconstruction plate.
Fig. 3
Case B was a 58-year-old male patient. Preoperative X-ray and three-dimensional computed tomography (3D-CT) of the pelvis confirmed both column fractures. (A) Pelvis anteroposterior (AP) radiograph preoperatively. (B) 3D-CT, superomedially displaced acetabular fracture. (C) Pelvis AP radiograph immediate postoperative. (D) Pelvis AP radiograph after one year fixed with anatomical quadrilateral plate.
The immediate postoperative reduction quality was notably superior in the anatomical quadrilateral surface plate group (p=0.03). Nevertheless, comparing long-term results, the anatomical quadrilateral surface plate group did not exhibit statistically more favorable outcomes (p=0.49) (Table 2).
Table 2
Radiologic Measurements of the Two Plate Groups
Discussion
Treating acetabulum fracture involving the quadrilateral surface is a demanding decision-making challenge.1) Although it is not a component located in the weight-bearing area, it affects outcome as it implies greater difficulty in reconstruction and its reduction is essential to achieve adequate joint congruency.5,25) In addition, quadrilateral surface involving fractures are frequently comminuted and are seen mainly in elderly patients who have accompany with comorbid medical conditions and osteoporosis, which could create additional challenges for the treatment.18) Treatments for comminuted or osteoporotic quadrilateral plate fractures with the traditional techniques may lead to instability of fixation or step off articular surface that leave residual protrusion of the femoral head and hip incongruence, which result in poor clinical outcomes despite otherwise anatomical reduction.10,26,27)
Recent advances in surgical approaches, including the emergence of less invasive intrapelvic approaches such as the modified Stoppa, pararectus, or supra-ilioinguinal approaches,19,24,28,29) provide improved access to the quadrilateral surface and the medial aspect of the posterior column.19,30) Less invasive surgical exposures with lower morbidity to the patient such as the anterior intrapelvic (modified Stoppa) approach were used to give access to the posterior column, quadrilateral surface, and anterior column through a single midline incision.19,24,28,29) With improved access to the quadrilateral surface and the medial aspect of the posterior column, more effective means of buttress plating the medial wall.12) Newer plate designs have been introduced that provide a buttress to the quadrilateral surface and prevent medial subluxation of the femoral head and span fixation from the posterior to the anterior column.16,30)
Zhang et al.31) investigated a kind of novel quadrilateral surface buttressing anatomical plate in the treatment of displaced acetabular fractures involving quadrilateral surface to solve the problem of difficulty in obtaining a satisfactory fixation effect using existing reconstruction plates. Of the patients, 26 patients underwent anatomical quadrilateral surface buttress fixation through the Stoppa approach. It was found by postoperative X-ray and CT scan that anatomical reduction and good reduction rates are 88.46% and 11.54%, respectively.31)
Likewise, in our study, there was no difference in the operation time and frequency of surgery-related complications between the two plate groups in using the modified Stoppa approach.31,32) In comparison the two plates, the anatomical quadrilateral surface plate demonstrated a statistically superior immediate postoperative reduction quality than the pelvic reconstruction plate. However, when assessing the final radiological results, no significant difference was observed between the two plates.
Studies on prognosis after fracture treatment investigated various factors that may affect the outcomes. Morison et al.33) previously suggested that posttraumatic arthritis may not only be a result of articular incongruities following reduction, but also result from the articular cartilage damage at the initial trauma.8,26,34,35) Lin et al.36) concluded age, initial articular and dome comminution were the prognostic indicators of advanced arthritis and poor functional scores after the anatomical reduction and internal fixation of acetabular wall fractures. Navarre et al.37) posed the poor bone quality and higher rate of fragment comminution and marginal impaction in elderly patients also contribute an unsecure fixation and lead to early implant failure.37,38) Comprehensively, anatomical reduction is crucial for prognosis and we should make effort to achieve better outcome.
It is our impression that the pre-contoured configuration of the anatomical quadrilateral surface plate has utility as a reduction tool. It could allow the surgeon to utilize the medial buttress effect of the surgical plate distributing force across the acetabulum’s quadrilateral surface and indirectly adjusting the position of the femoral head.24,28)
Our study has several limitations. The main limitations of this study are the retrospective design and short follow-up (including minimum 6 months). Delayed complications were probably underestimated due to the short follow-up. Additionally, studies on clinical outcomes were not included. However, we consider the results to be interesting because they provided a useful treatment option for the treatment of acetabular quadrilateral surface fracture.
Conclusion
In this study, the anatomical quadrilateral surface plate demonstrated a statistically superior immediate postoperative reduction quality compared to the pelvic reconstruction plate although when assessing the final radiological results, no significant difference was observed between the two plates. We could affirm that both plate groups achieved sufficiently good results, so we concluded that the anatomical quadrilateral surface plate is one of the valuable therapeutic options for acetabulum fractures.
Financial support:None.
Conflict of interests:None.
References
-
Sousa H, Dinis J, Seabra P, et al. Acetabular fracture involving the quadrilateral surface in the elderly treated with supra-pectineal buttress plate: a center experience. J Musculoskelet Disord Treat 2021;7:104
-
-
Andrés-Peiró JV, Teixidor-Serra J, Tomás-Hernández J, et al. Retrospective study of 16 acetabular fractures with involvement of the quadrilateral plate treated with an anterior intrapelvic modified Rives-Stoppa approach. Rev Esp Cir Ortop Traumatol (Engl Ed) 2019;63:416–423.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

