Abstract
-
Background
The purpose of this study was to retrospectively evaluate the radiographic and clinical results of a small single or double low-profile plate fixation of 2.0/2.4 mm locking compression plate (LCP) in treating isolated greater tuberosity (GT) fractures of the humerus.
-
Methods
From June 2015 to October 2022, patients who underwent LCP in treating isolated GT fractures of the humerus were included in this study. The radiological and clinical results were analyzed in 15 patients who underwent open reduction and internal fixation used 2.0/2.4 mm LCP.
-
Results
Bone union was achieved in 14 patients (93.3%) and one failed case was treated with a 2.4 mm single LCP fixation. Radiological union was achieved within 10–20 weeks. Complications occurred in two patients (13.3%), including the reduction failure and shoulder stiffness. At the final follow-up, the average clinical scores were as follows: a visual analog scale for pain of 2.1 (range, 0–5) and a University of California, Los Angeles score of 27.2 (range, 18–31). Regarding range of motion (ROM), the average active ROMs were 142° for forward flexion (range, 120°–150°), 147.1° for abduction (range, 120°–180°), and 59.3° for external rotation (range, 45°–80°). For internal rotation, the average was observed to reach the 10th thoracic vertebra (range, 1st lumbar vertebra–7th thoracic vertebra).
-
Conclusions
The clinical and radiologic outcomes of treating isolated GT fracture using 2.0/2.4 mm LCP were favorable, and double low-profile plate fixation may be beneficial for sufficient fracture stability if possible.
-
Level of Evidence
Level IV, case series.
-
Keywords: Shoulder, Shoulder fractures, Internal fracture fixation, Internal fixators, Bone plates
Introduction
Of proximal humeral fractures, isolated greater tuberosity (GT) fractures of humerus accounted for approximately 20% [
1]. For patients with proximal humeral fractures, 3.5 mm locking compression plate (LCP) Proximal Humeral Internal Locking System (PHILOS, DePuy Synthes) was commonly used for fixation. Geiger et al. [
2] reported that the PHILOS plate provided sufficient fracture stabilization for the treatment of proximal humeral fractures in elderly patients and that subacromial impingement occurred in approximately 20% of proximal humeral fractures treated with the PHILOS plate, which was mainly due to the superior position of the plate. For humerus avulsion type GT fracture with small fragments, the recommended placement of a locking plate relatively superiorly might provide more secure fixation of the fragments, but might increase impingement [
3]. To prevent secondary subacromial impingement and secure fixation in the treatment of isolated GT fractures of the humerus, several authors have proposed various techniques, including cannulated screw fixation, tension band wiring, and arthroscopic double-row suture anchor fixation [
3–
5]. However, complications such as cortical breakage and reduction loss, anchor pull-out failure, and rotator cuff damage have been reported in elderly patient with osteoporosis or osteopenia [
5–
7].
In a comparative biomechanical study using animals, Gaudelli et al. [
8] compared fixation of humerus split type GT fractures with a calcaneal locking plate (DePuy Synthes), a tension band, and a double row suture bridge and reported that a locking plate fixation provided the strongest and stiffest biomechanical fixation. Several authors have showed reliable stability and good clinical results in the fixation of isolated GT fractures using low-profile system, such as the one-third tubular plate, LCP mesh plate, LCP hook plate, or X-shaped midfoot locking plate [
9–
14]. Authors thought that 2.0/2.4 mm LCP miniplate (DePuy Synthes) might enable specific fragment fixation and enhance the low-profile advantage in isolated GT fractures. To the best of our knowledge, no studies have been reported fixation of 2.0/2.4 mm LCP in isolated GT fractures of humerus. The purpose of this study was the results of treating isolated GT fractures with open reduction and internal fixation (ORIF) using a 2.0/2.4 mm LCP.
Methods
Ethics Statement
The study was approved by the Institutional Review Board of Daegu Fatima Hospital (IRB No. 2024-10-001) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was waived.
Patient Selection
We retrospectively studied the records of patients with isolated GT fractures who underwent ORIF between June 2015 and October 2022 and could be followed up for more than 6 months. Among the 66 patients, we select the 15 patients who underwent ORIF used 2.0/2.4 mm LCP and evaluate the clinical and radiological outcomes. The surgical indication was an at least 5 mm displacement of the GT as observed in either simple radiography or three-dimensional computed tomography (CT) (
Fig. 1). All fractures were evaluated with the anteroposterior, Grashey and scapular Y view throughout the follow up period. All patients underwent CT scans to assess the pattern of fracture, degree of comminution and the morphological classification of the GT fragment (avulsion, split, or depression) according to Mutch et al. [
14]. All patients underwent magnetic resonance imaging scans to assess the rotator cuff and associated injuries.
Exclusion criteria encompassed (1) individuals without a minimum 6-month follow-up postsurgery; (2) those with a prior history of shoulder surgery; (3) participants with additional injuries necessitating separate surgical interventions; (4) individuals experiencing neurovascular injuries preoperatively; and (5) patients with nonunion of the GT fracture.
Surgical Technique
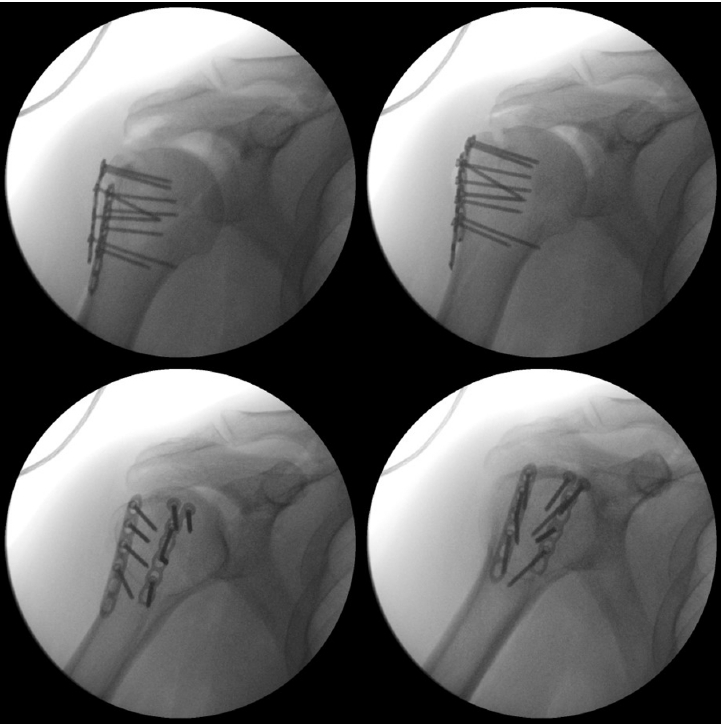
Under the general anesthesia, the patient was placed in beach chair position on the operation table. The fracture site was visualized using a deltopectoral approach, and the supraspinatus tendon attached to the displaced GT fragment was stabilized with Ethibond (Ethicon) sutures. We then pulled it downwards to achieve reduction of the fracture site, and confirmation of reduction was done using a C-arm. Subsequently, a 2.0/2.4 mm LCP miniplate was positioned on the fracture site and aligned with the contours of the fracture using bender. Temporary fixation was attempted using K-wires. In cases of severe comminution, additional anchors (Y-knot anchor or raptomite suture anchor) were used on the proximal fracture site before plating and passed the suture through the rotator cuff to reduce the GT fracture. Then double plates were applied to each fracture segment after aligning the contours. After confirming reduction of the fracture segments and plate position, screw fixation was performed (
Fig. 2). To provide appropriate tension to the rotator cuff, augmentation was performed using Ethibond or Fiberwire (Arthrex) through the empty holes of the 2.0/2.4 mm LCP. In some cases, tension band wires were used to increase the fixation strength and stability of the rotator cuff. In cases of poor bone quality, autograft or allograft bone grafting was performed in conjunction. Postoperative radiography was preformed to assess the fracture reduction and fixation.
All patients received standardized postoperative care, with the same treatment protocol applied regardless of the fracture type or degree of comminution. After the surgery, a shoulder immobilizing brace with an abduction pillow was used for a duration of 4 weeks. During the second week post-surgery, patients began gentle passive forward flexion arm exercises. At the 4-week mark, the brace and abduction pillow were removed, and patients initiated passive range of motion (ROM) exercises in all directions, as well as active mobilization.
Radiologic and Clinical Evaluation
We evaluated dual-energy X-ray absorptiometry to measure the lumbar spine and femoral bone mineral density. As a criterion for diagnosing osteoporosis, a T score of –1 to –2.5 was defined as osteopenia and below –2.5 was defined as osteoporosis. During the follow-up period, we evaluated the following radiological parameters: bone union and time to union. Time-to-union was determined as the point when cortical continuity was observed on one of the three planes of plain radiography (anteroposterior, Grashey, or scapular Y view), and when tenderness at the fracture site subsided. Anatomical reduction was defined as a distance between the GT and the humeral head of 4 to 10 mm at the final follow-up. Similarly, a loss of reduction was defined as a displacement greater than 3 mm at the final follow-up compared to the immediate postoperative radiograph. For all surgically treated patients, follow-up imaging was conducted at least up to 6 months postoperatively, with evaluations scheduled at 1-, 2-, 3-, and 6-month intervals. Clinical outcomes were assessed based on the degree of pain and the restoration of daily functional activities. At the final follow-up, the following clinical outcome parameters were evaluated: visual analog scale (VAS) score, ROM of the shoulder joint, and the Shoulder Rating Scale of the University of California, Los Angeles (UCLA) score. Postoperative complications were also carefully assessed.
Results
A total of 15 patients with isolated GT fractures underwent ORIF using 2.0/2.4 mm LCP. The average age of the patients was 63.8 years (range, 50–78 years), and the average follow-up period was 15.6 months (range, 6–78 months). Among the patients, five were male and 10 were female. Eight cases involved the right side, while seven cases involved the left side. The fractures occurred due to various mechanisms, including simple falls, motor vehicle accidents, being hit by a heavy object, falls from height, and idiopathic causes. Seven patients had accompanying anterior dislocation of the shoulder, and four patients had a combined fracture at a different site. Prior to the surgery, all patients were assessed and found to have intact rotator cuffs without any evidence of tears. The surgical treatment was performed, on average, 14 days after the trauma (range, 4–40 days). Important demographic data of the study group are shown in
Table 1.
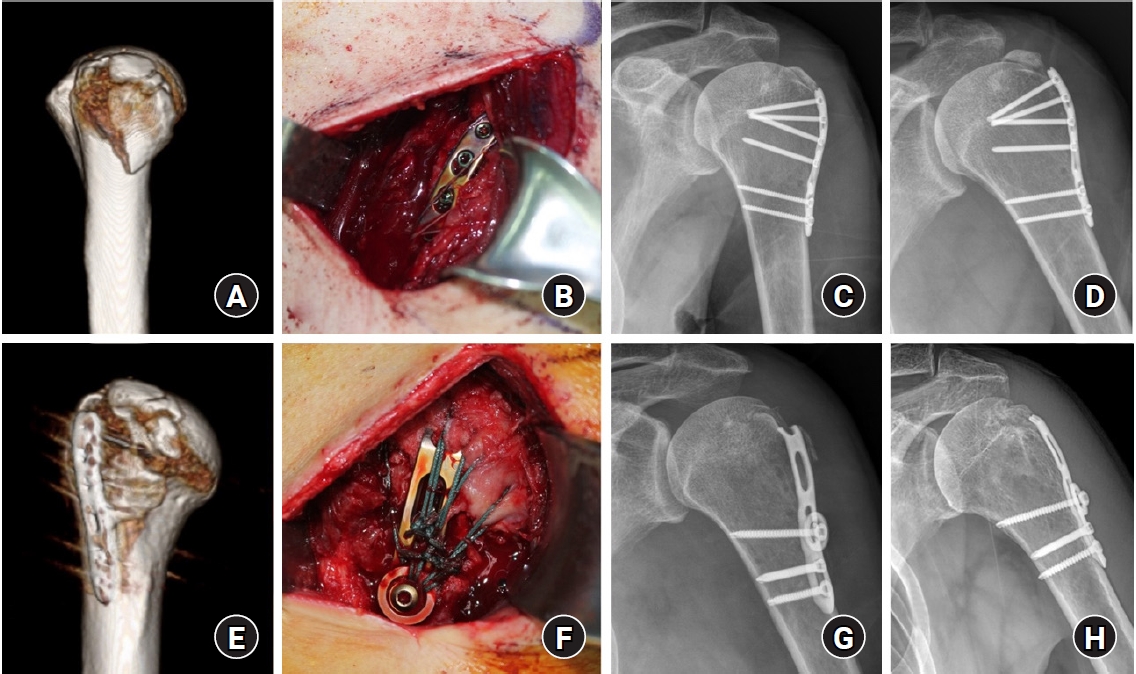
Radiological union was achieved within 10–20 weeks in all patients except one case of reduction failure. Although there was a reduction failure, bone union was confirmed through a subsequent reoperation using a 3.5 mm LCP hook plate (DePuy Synthes) (
Fig. 3). In all other patient groups, no displacement greater than 3 mm was observed, and anatomical reduction was achieved. At the final follow-up, the average clinical scores were as follows: a VAS for pain of 2.1 (range, 0–5) and a UCLA score of 27.2 (range, 18–31). Regarding ROM, the average active ROMs were 142° for forward flexion (range, 120°–150°), 147.1° for abduction (range, 120°–180°), and 59.3° for external rotation (range, 45°–80°). For internal rotation, the average was observed to reach the 10th thoracic vertebra (range, 1st lumbar vertebra–7th thoracic vertebra) (
Table 2).
No postoperative infections or neurovascular complications were observed in any of the patients. However, one patient experienced shoulder stiffness. At the sixth week after the operation, the affected shoulder showed limited passive ROM: 80° of forward flexion, 90° of abduction, and 10° of external rotation, indicating restricted mobility compared to the contralateral arm. To address this issue, we administered an intra-articular injection of steroids and initiated aggressive rehabilitation from the third postoperative month. After the final follow-up, significant improvements in the ROM were observed.
Discussion
This study aimed to evaluate the results of a small single or double 2.0/2.4 mm LCP miniplate fixation. Shin et al. [
9] reported that they modified a one-third tubular plate (DePuy Synthes) into a hook plate to fix isolated GT fractures and achieved fracture union in all cases, but performed a reoperation using the same method in one case where the metal failure. Even in small and comminuted fractures of isolated GT fractures, 3.5 mm LCP hook plate provided less subacromial impingement and sufficient stability and led to satisfactory clinical and radiologic results [
10,
11]. Bogdan et al. [
12] showed that the use of a variable angle LCP mesh plate (2.4/2.7 mm) (DePuy Synthes) to fix isolated GT fractures resulted in relatively good clinical results, demonstrating the benefit of a low-profile implant and no complication of impingement. Chen et al. [
13] reported satisfactory clinical results using a X-shaped midfoot locking plate (DePuy Synthes) for isolated GT fractures without complication such as subacromial impingement, nonunion, secondary displacement, and implant loosening. In our study, we demonstrated bone union in 14 out of 15 cases (93.3%) using small single or double low-profile LCP fixation for isolated GT fractures, and we believe that this technique can be considered a good alternative technique for small or comminuted isolated GT fractures in which conventional plates cannot be used.
Kim et al. [
1] reported that isolated GT fractures were more common in young and healthy male population, with a mean age of 42.8 years (range, 19–73 years), and that concomitant shoulder dislocation occurred in 6.9%. In our study, the mean age was 63.8 years (range, 50–78 years), the incidence was higher in women, 60% had osteoporosis and osteopenia, and 46.7% had concomitant shoulder dislocation. As society ages, the physical characteristics of patients were changing, and it was especially important to secure sufficient stability in isolated GT fractures in elderly patients with osteoporosis or osteopenia.
Lee et al. [
11] treated isolated GT fractures using a 3.5 mm LCP hook plate in 21 patients (mean age, 64 years), 15 of whom had osteoporosis and osteopenia, and reported adequate stability and satisfactory clinical and radiographic results. In a comparative biomechanical study of clavicle fracture fixation, Pastor et al. [
15] showed that low-profile 2.0/2.5 mm dual plates had significantly higher initial stiffness and similar fracture resistance compared to a single 3.5 mm locking plate. In our study, one case of reduction failure occurred after fixation of a single 2.4 mm LCP in isolated GT fractures, and bone union was achieved through reoperation using a 3.5 mm LCP hook plate. Although we were able to achieve bone union with single low-profile plate fixation, we believe that double low-profile plate fixation would be more effective than single low-profile plate fixation for sufficient fracture stability.
Lee et al. [
11] reported that two patients (9.5%) had bursal side partial thickness rotator cuff tears due to hook irritation, and these patients were repaired using a simple transosseous technique. In our study, a small single or double 2.0/2.4 mm LCP miniplate fixation was feasible for isolated GT fractures without accessing the rotator cuff as much as a hook plate.
The present study has certain limitations that should be acknowledged. Firstly, the small number of included patients underscores the necessity for future comparative studies with a larger sample size and extended follow-up periods. Secondly, the absence of a comparative group is a result of introducing a new technique for isolated GT fractures in this study. Currently, the authors are in the process of gathering and evaluating data for comparison, especially with the 3.5 LCP hook plate, in the context of the next research study. Thirdly, the absence of biomechanical studies is also a challenge that needs to be addressed. Fourth, it is important to note that the present study is retrospective. However, the strength of this study is that the surgeries were performed at a single center using the same surgical technique and products from the same company, although the number of fixation plates varied.
In summary, the authors experienced good clinical and radiological outcomes of ORIF using 2.0/2.4 mm LCP for isolated GT fractures. This fixation methods maximize the advantages of a low-profile system compared to using a 3.5 mm LCP. It further reduces the risk of subacromial impingement and provides better fixation for small or comminuted fractures, enabling fragment-specific fixation and facilitating anatomical reduction. If possible, double low-profile plate fixation would be more effective than single low-profile plate fixation for sufficient fracture stability. Moreover, it offers a solution to the previously reported complication of rotator cuff damage caused by the Hook plate. Therefore, it is suggested that the 2.0/2.4 mm LCP serves as an effective approach for addressing and preventing rotator cuff injuries, making it a beneficial fixation method in both radiological and clinical settings.
Conclusions
The 2.0/2.4 mm LCP fixation for isolated GT fractures serves as an effective approach for addressing and preventing rotator cuff injuries, making it a beneficial fixation method in both radiological and clinical settings. If possible, double low-profile plate fixation would be more effective than single low-profile plate fixation for sufficient fracture stability.
Article Information
-
Author contributions
Conceptualization: SC. Data curation: SC, DS. Formal analysis: BHK. Investigation: SC, DS, SK. Supervision: DS, BHK. Visualization: SK, BHK. Writing-original draft: BHK. Writing-review & editing: SC, DS, SK, BHK. All authors read and approved the final manuscript.
-
Conflict of interest
None.
-
Funding
None.
-
Data availability
Contact the corresponding author for data availability.
Fig. 1.A shoulder anteroposterior (A) three-dimensional computed tomography (B) of the right shoulder of a 58-year-old male patient with a displaced and comminuted isolated fracture of the greater tuberosity of the humerus.

Fig. 2.An immediate postoperative C-arm showing open reduction and internal fixation using dual 2.4 mm locking compression plate for a displaced and comminuted isolated fracture of the greater tuberosity of the humerus.

Fig. 3.(A) Three-dimensional computed tomography (CT) of a 60-year-old male patient showed a split ftype comminuted isolated fracture of the greater tuberosity of the humerus on left shoulder. (B, C) A single 2.4 mm locking compression plate (LCP) with augmentation anchor suture fixation was performed. (D, E) Postoperative 1 week shoulder anteroposterior (AP) radiograph and three-dimensional CT showed reduction loss. (F, G) A 3.5 mm LCP hook plate with augmentation tension-band suture fixation was performed. (H) Postoperative 6 months AP radiograph showed complete union of the fracture.

Table 1.Summary of demographic data
|
Patient no. |
Age (yr) |
Sex |
Affected side |
BMD |
Injury mechanism |
Dislocation |
Classification |
Combined injury |
Time to surgery (day) |
Union time (wk) |
No. of plate |
Augmentation
|
Bone graft |
Complication |
|
Tension suture |
Suture anchor |
|
1 |
73 |
Male |
Lt |
Osteopenia |
Hit by mass |
O |
Avulsion |
- |
16 |
10 |
Dual |
2.4+2.0 |
1 |
- |
- |
- |
|
2 |
72 |
Female |
Rt |
Osteoporosis |
Simple fall |
O |
Depression |
- |
21 |
10 |
Dual |
2.4+2.4 |
3 |
- |
Autograft |
- |
|
3 |
58 |
Male |
Lt |
- |
Idiopathic |
- |
Avulsion |
- |
25 |
16 |
Dual |
2.4+2.4 |
1 |
- |
Autograft |
- |
|
4 |
63 |
Female |
Rt |
Osteopenia |
Simple fall |
O |
Avulsion |
- |
6 |
12 |
Dual |
2.4+2.4 |
1 |
- |
- |
- |
|
5 |
65 |
Female |
Lt |
Osteopenia |
MVA |
O |
Split |
Rt 1st MC neck fx |
6 |
12 |
Dual |
2.4+2.4 |
3 |
- |
- |
- |
|
Multiple rib fx |
|
6 |
70 |
Male |
Rt |
Osteopenia |
Fall from height |
O |
Avulsion |
- |
11 |
12 |
Dual |
2.0+2.0 |
2 |
- |
- |
- |
|
7 |
52 |
Female |
Rt |
Osteopenia |
Simple fall |
- |
Split |
- |
13 |
17 |
Single |
2.4 |
1 |
- |
Allograft |
- |
|
8 |
73 |
Female |
Lt |
Osteopenia |
Simple fall |
- |
Avulsion |
- |
7 |
20 |
Single |
2.4 |
- |
- |
Allograft |
- |
|
9 |
50 |
Female |
Lt |
- |
Hit by mass |
|
Avulsion |
- |
9 |
20 |
Single |
2.4 |
1 |
- |
- |
- |
|
10 |
68 |
Female |
Rt |
- |
Simple fall |
O |
Split |
- |
18 |
16 |
Single |
2.4 |
3 |
1 |
Autograft |
- |
|
11 |
59 |
Male |
Rt |
- |
Hit by mass |
O |
Split |
Rt 4th finger distal phalanx fx |
12 |
20 |
Single |
2.4 |
- |
1 |
- |
Stiffness |
|
12 |
66 |
Female |
Rt |
Osteoporosis |
MVA |
- |
Split |
- |
40 |
20 |
Single |
2.0 |
- |
1 |
Autograft |
- |
|
13 |
60 |
Male |
Lt |
- |
MVA |
- |
Spllt |
Rt tibiofibular open fx |
11 |
|
Single |
2.4 |
- |
1 |
- |
Reduction failure |
|
14 |
50 |
Female |
Rt |
- |
MVA |
- |
Avulsion |
Lt Proximal humerus fx |
4 |
16 |
Single |
2.0 |
- |
1 |
- |
- |
|
Rt tibia plateau fx |
|
15 |
78 |
Female |
Lt |
Osteoporosis |
Simple fall |
- |
Split |
- |
11 |
16 |
Single |
2.0 |
- |
1 |
- |
- |
Table 2.Clinical outcomes at the final follow-up
|
Variable |
Mean (range) |
|
VAS pain score |
2.1 (0–5) |
|
Range of motion |
|
|
Forward flexion (°) |
142 (120–150) |
|
Abduction (°) |
147.1 (120–180) |
|
External rotation (°) |
59.3 (45–80) |
|
Internal rotation (level of spine) |
T10 (L1–T7) |
|
Functional score |
|
|
UCLA |
27.2 (18–31) |
References
- 1. Kim E, Shin HK, Kim CH. Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci 2005;10:441-4.ArticlePubMed
- 2. Geiger EV, Maier M, Kelm A, Wutzler S, Seebach C, Marzi I. Functional outcome and complications following PHILOS plate fixation in proximal humeral fractures. Acta Orthop Traumatol Turc 2010;44:1-6.ArticlePubMed
- 3. Liao W, Zhang H, Li Z, Li J. Is arthroscopic technique superior to open reduction internal fixation in the treatment of isolated displaced greater tuberosity fractures. Clin Orthop Relat Res 2016;474:1269-79.ArticlePubMedPMCPDF
- 4. Cornell CN, Levine D, Pagnani MJ. Internal fixation of proximal humerus fractures using the screw-tension band technique. J Orthop Trauma 1994;8:23-7.ArticlePubMed
- 5. Green A, Izzi J Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg 2003;12:641-9.ArticlePubMed
- 6. Nóbrega Catelas D, Correia L, Adan E Silva F, Ribau A, Claro R, Barros LH. Greater tuberosity fractures of the humerus: complications and long-term outcomes after surgical treatment. Eur J Orthop Surg Traumatol 2024;34:2541-7.ArticlePubMedPMCPDF
- 7. Ji JH, Shafi M, Song IS, Kim YY, McFarland EG, Moon CY. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy 2010;26:600-9.ArticlePubMed
- 8. Gaudelli C, Ménard J, Mutch J, Laflamme GY, Petit Y, Rouleau DM. Locking plate fixation provides superior fixation of humerus split type greater tuberosity fractures than tension bands and double row suture bridges. Clin Biomech (Bristol) 2014;29:1003-8.Article
- 9. Shin DJ, Byun YS, Chang SA, Yun HM, Park HW, Park JY. The surgical outcomes of isolated greater tuberosity fractures of the proximal humerus fixed with the spring plate. J Korean Fract Soc 2009;22:159-65.Article
- 10. Lee KR, Bae KC, Yon CJ, Cho CH. Hook plate fixation for isolated greater tuberosity fractures of the humerus. Clin Should Elbow 2017;20:222-9.ArticlePDF
- 11. Lee WY, Shin HD, Kim KC, Cha SM, Jeon YS, Kim DH. Open reduction and stable internal fixation using a 3.5-mm locking hook plate for isolated fractures of the greater tuberosity of the humerus: a 2-year follow-up study using an innovative fixation method. Clin Orthop Surg 2021;13:293-300.ArticlePubMedPMCPDF
- 12. Bogdan Y, Gausden EB, Zbeda R, Helfet DL, Lorich DG, Wellman DS. An alternative technique for greater tuberosity fractures: use of the mesh plate. Arch Orthop Trauma Surg 2017;137:1067-70.ArticlePubMedPDF
- 13. Chen YF, Zhang W, Chen Q, Wei HF, Wang L, Zhang CQ. AO X-shaped midfoot locking plate to treat displaced isolated greater tuberosity fractures. Orthopedics 2013;36:e995-9.ArticlePubMed
- 14. Mutch J, Laflamme GY, Hagemeister N, Cikes A, Rouleau DM. A new morphological classification for greater tuberosity fractures of the proximal humerus: validation and clinical implications. Bone Joint J 2014;96:646-51.PubMed
- 15. Pastor T, Knobe M, van de Wall BJ, et al. Low-profile dual mini-fragment plating of diaphyseal clavicle fractures: a biomechanical comparative testing. Clin Biomech (Bristol) 2022;94:105634.Article
 , Dongju Shin, MD2
, Dongju Shin, MD2 , Sangwoo Kim, MD1
, Sangwoo Kim, MD1 , Byung Hoon Kwack, MD1
, Byung Hoon Kwack, MD1






 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

