Articles
- Page Path
- HOME > J Korean Fract Soc > Volume 37(2); 2024 > Article
- Review Article Treatment of Avulsion Fractures around the Knee
- Sumin Lim
-
Journal of The Korean Orthopaedic Trauma Association 2024;37(2):117-124.
DOI: https://doi.org/10.12671/jkfs.2024.37.2.117
Published online: April 30, 2024

- 1,041 Views
- 9 Download
- 0 Crossref
- 0 Scopus
Abstract
Avulsion fractures are common in athletes and result from high-impact or sudden, forceful movements involving the separation of a bone fragment at the ligament or tendon attachment site. The key focus areas include the anterior and posterior cruciate ligaments, medial collateral ligament, anterolateral complex, arcuate complex, medial patellofemoral ligament, patellar tendon, and quadriceps tendon. Diagnostic approaches combine radiography with advanced imaging techniques, such as computed tomography and magnetic resonance imaging, to elucidate the extent of injury and guide treatment decisions. Treatment ranges from conservative management for non-displaced fractures to surgical intervention for displaced fractures, with strategies customized based on the specific ligament involved and the nature of the fracture.
Published online Apr 24, 2024.
https://doi.org/10.12671/jkfs.2024.37.2.117
 , M.D.
, M.D.
Abstract
Avulsion fractures are common in athletes and result from high-impact or sudden, forceful movements involving the separation of a bone fragment at the ligament or tendon attachment site. The key focus areas include the anterior and posterior cruciate ligaments, medial collateral ligament, anterolateral complex, arcuate complex, medial patellofemoral ligament, patellar tendon, and quadriceps tendon. Diagnostic approaches combine radiography with advanced imaging techniques, such as computed tomography and magnetic resonance imaging, to elucidate the extent of injury and guide treatment decisions. Treatment ranges from conservative management for non-displaced fractures to surgical intervention for displaced fractures, with strategies customized based on the specific ligament involved and the nature of the fracture.
초록
견열 골절은 인대 또는 힘줄 부착 부위에서 뼈 조각이 분리되는 골절로, 큰 충격이나 갑작스럽고 강한 움직임으로 인해 발생하며 운동선수에게 흔히 발생한다. 본 논문에서는 무릎 주위 견열 골절의 진단 및 치료에 대해 다룰 것이다. 주요 초점은 전방 및 후방 십자 인대, 내측 측부 인대, 전외측 복합체, 궁형 복합체, 내측 슬개대퇴 인대, 슬개건, 대퇴사두건 등에 맞추어 다룰 것이다. 진단 접근법은 기본적인 방사선 촬영과 컴퓨터 단층촬영, 자기공명영상을 결합하여 부상의 정도를 평가하고 치료 결정에 도움을 줄 수 있다. 치료는 비전위성 골절에 대한 보존적 치료에서 전위성 골절에 대한 수술적 치료에 이르기까지 다양하며, 특정 인대와 골절의 종류에 기반한 맞춤형 전략을 사용한다.
Introduction
An avulsion fracture is a type of bone injury where a fragment of the bone is separated from its main structure. This injury can occur in any area where soft tissue is attached to bone,1) and it is particularly common among individuals engaged in organized sports, especially adolescent athletes.2)
Avulsion fractures typically result from a sudden, forceful pull on the bone during an acute incident that cause a section of the bone to detach. In the knee, avulsion fractures can involve various anatomical structures, including the cruciate ligaments, collateral ligaments, the arcuate ligament complex, the iliotibial band, and the tendons of the patella and quadriceps, along with the retinaculum.3)
Initial evaluations often use radiographs to identify subtle signs of avulsion fractures, such as tiny bone fragments at normal attachment sites.4) Advanced imaging methods like computed tomography (CT) and magnetic resonance imaging (MRI) provide additional valuable information on the extent of the injury.5) This article will discuss the types and treatments of avulsion fractures around the knee.
Anterior Cruciate Ligament (ACL) Avulsion Fracture
These are more common in children than in adults due to the relative weakness of the apophysis compared to the ligament.5) Avulsion fractures of the ACL mainly occur at the tibial attachment, but in some cases, they can also occur at the lateral femoral condyle.6) The common mechanisms include pivot shift injury which involves valgus stress and internal rotation in a flexed knee and hyperextension injury.4) While conventional radiographs may not always clearly reveal these fractures, CT and MRI can provide a detailed evaluation, allowing for the assessment of ACL continuity and associated structures. MRI is particularly advantageous for evaluating potential accompanying injuries, such as meniscus tears, necessitating appropriate treatment.4,7) The Meyers and McKeever classification system outlines four subtypes of tibial spine fractures.8) Type I, which is non-displaced, can be treated conservatively (Fig. 1). The treatment for Type II, which are partially displaced, remains controversial. However, displaced fractures, such as types III and IV, require reduction and fixation, which can be performed arthroscopically or through open surgery.9,10)
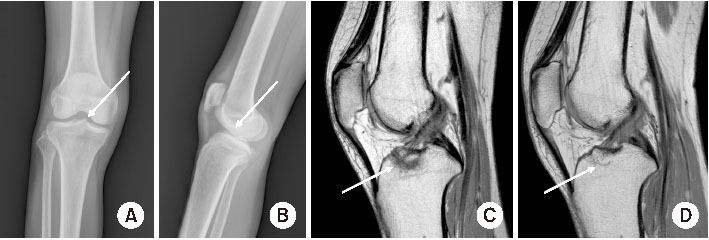
Fig. 1
A 37-year-old female patient sustained an injury from a fall from the third floor. The plain anteroposterior (A) and lateral (B) radiographs revealed a non-displaced anterior cruciate ligament (ACL) avulsion fracture (arrows). (C) The sagittal PD (proton density)-weighted magnetic resonance imaging (MRI) showed a non-displaced ACL avulsion fracture (arrow) and intact ACL continuity. (D) Conservative treatment was administered, and a follow-up MRI after six months confirmed bone union (arrow).
Posterior Cruciate Ligament (PCL) Avulsion Fracture
The injury mechanism for PCL avulsion fractures is similar to intrasubstance PCL tears, often resulting from motor vehicle or motorcycle accidents.11) Such injuries typically happen when a posteriorly directed force impacts the proximal tibia while the knee is flexed. The most common type of these fractures is the tibial-sided PCL avulsion.12) While plain radiographs are the initial diagnostic tool, the lateral view is the most informative. If an avulsion fracture is suspected but not clear on radiographs, CT or MRI can be helpful. Concomitant injuries are common, making MRI a recommended diagnostic step.11,13) For displaced PCL avulsion fractures, surgical reduction and fixation are essential to ensure joint stability and prevent nonunion, whereas conservative treatment has been shown to yield favorable outcomes for non-displaced fractures (Fig. 2). Zhao et al.14) reported that up to 5 mm displacement can be successfully treated with non-operative treatment. Recently, Yoon et al.15) suggested that acute PCL avulsion fractures with displacements up to 6.7 mm can be considered for non-operative treatment. The surgical interventions for these fractures may include a variety of techniques involving screws, K-wires, anchors, or sutures, which can be performed either through open surgery or arthroscopically.11,12)
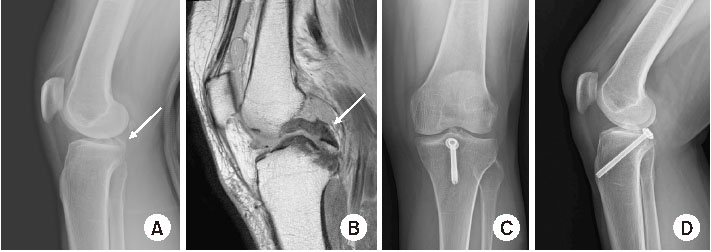
Fig. 2
A 57-year-old female patient was admitted following a motorcycle accident. (A) A posterior cruciate ligament (PCL) avulsion was noted on the knee lateral radiograph (arrow). (B) On the sagittal PD (proton density)-weighted magnetic resonance imaging, a displaced PCL avulsion fracture was observed, but the continuity was intact (arrow). (C, D) Bone union was achieved one year after surgical treatment.
Segond Fracture
The Segond fracture was first identified by Segond16) through cadaver studies, where he described it as a small avulsion fracture at the proximolateral aspect of the tibia. Following this initial identification, Kaplan17) highlighted its association with an avulsion fracture of the iliotibial band. This understanding was expanded upon by Terry et al.,18) who identified the deep capsulo-osseous fibers of the iliotibial band as being involved in the pathology of the Segond fracture. In 2013, the concept of the anterolateral ligament (ALL) was introduced, suggesting that avulsion fractures of this ligament could be central to the pathogenesis of the Segond fracture.19) Recently, in 2017, the anterolateral complex (ALC) Consensus Group stated that multiple structures, including the ALL, deep iliotibial band, and biceps aponeurosis, attach in the region of the Segond fracture, and it remains unclear which may be responsible for this lesion.20) While the specific injury mechanism remains somewhat unclear, it is generally believed that the fracture is associated with internal rotation of the tibia. The relationship between Segond fractures and ACL tears has been well-documented,21,22,23) with numerous reports also indicating an association with meniscus tears.24,25,26) Segond fracture can be easily diagnosed through radiographic imaging, but since it is rarely an isolated injury, further evaluation with MRI is necessary (Fig. 3). Regarding treatment, the focus should be on the associated injuries rather than the Segond fracture itself. The Segond fracture is considered a pathognomonic finding for ACL injuries, often necessitating ACL reconstruction. However, there is a lack of evidence to support the surgical fixation of Segond fractures. If the ALC complex is damaged and does not heal, it will adversely affect the stability and function of the knee. Generally, indications for additional lateral augmentation, such as ALL reconstruction or lateral extra-articular tenodesis, include a Segond fracture, chronic ACL lesion, grade III pivot shift, high level of sporting activity, participation in pivoting sports, or ACL revision surgery.20,27,28,29,30) However, recent systematic reviews have reported that the presence of a Segond fracture does not provide a disadvantage in ACL reconstruction, as it was not a significant predictor of high-grade Lachman or pivot-shift grades.31) Further research is needed regarding the treatment of Segond fractures.
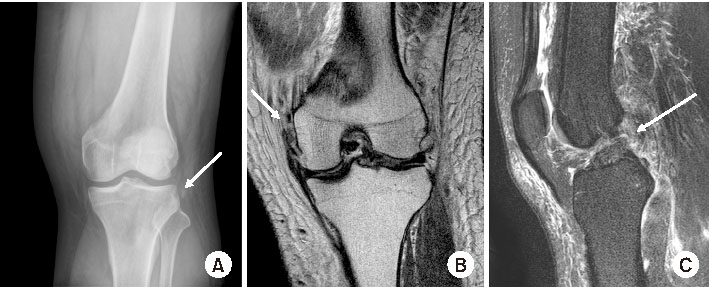
Fig. 3
A 29-year-old male patient was injured while skiing. (A) A Segond fracture was observed on the knee anteroposterior radiograph (arrow). (B) An associated proximal medial collateral ligament rupture was noted on the coronal T2-weighted magnetic resonance imaging (MRI) (arrow), and (C) an anterior cruciate ligament rupture was observed on the sagittal T2-weighted MRI (arrow).
Medial Collateral Ligament (MCL) Avulsion Fracture
The MCL of the knee comprises two distinct layers: the more robust superficial MCL (sMCL) and the less sturdy deep MCL (dMCL).32) The sMCL acts as the primary barrier against valgus stress and internal rotation when the knee is flexed, additionally offering secondary support against sagittal movements. Conversely, the dMCL provides secondary resistance to valgus stress, especially when the knee is extended. Tears in the sMCL typically occur at its proximal attachment to the medial femoral condyle, although injuries can also present distally. Avulsion fractures, where the ligament pulls off a bone fragment at its attachment point, are relatively rare. These fractures can happen at the dMCL’ s tibial attachment (known as a reverse Segond fracture) or at the MCL’s femoral attachment, a phenomenon first identified by Stieda33) in 1908. Hall and Hochman34) first described the reverse Segond fracture in 1997, also calling it a medial Segond fracture. This injury is an avulsion fracture of the medial tibial plateau, often linked with PCL and medial meniscus injuries. It usually results from high-energy knee trauma and is most commonly seen in young adults. Further research has connected reverse Segond fractures with ACL and MCL injuries.35) Stieda fractures mainly affect the deep MCL’s meniscofemoral fibers and might also involve nearby retinacular structures or the posteromedial oblique ligament, with potential concurrent injuries to the ACL, PCL, and meniscus.32) In cases where there are additional ligament injuries, early surgical repair is often recommended for Stieda fractures.36,37) For reverse Segond fractures, small bony avulsion fragments typically do not require fixation. However, if the fragment is large and impacts anteromedial knee stability or meniscal function, surgical fixation is advised.38,39) When no other injuries are involved, the treatment is similar to that for MCL injuries. Conservative treatment is possible for grades I, II, and even grade III injuries (Fig. 4). However, surgical intervention is typically recommended for isolated grade III MCL tears that exhibit significant valgus malalignment or MCL entrapment over the pes anserinus (Stener lesion), or in cases of intra-articular or bony avulsion. Consequently, avulsion fractures with grade III instability may require acute repair.
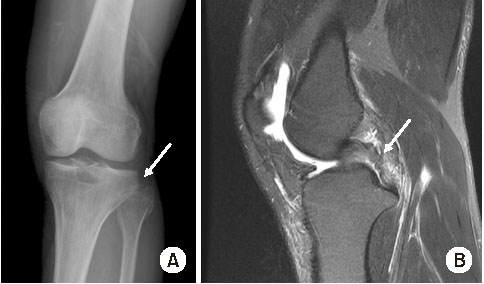
Fig. 4
(A) A 50-year-old male patient was injured in a pedestrian traffic accident, and a Stieda fracture was observed on the anteroposterior radiograph (arrow). (B) On the coronal T2-weighted magnetic resonance imaging, the medial collateral ligament continuity is intact, and there is no displacement of the Stieda fracture (arrow). (C) Bone union was confirmed at six months of conservative treatment (arrow).
Arcuate Ligament Avulsion Fracture
The “arcuate sign” refers to an avulsion fracture of the fibula head, as seen on knee radiographs, and it is associated with injuries to the posterolateral corner (PLC) of the knee.40) The PLC includes the lateral collateral ligament, biceps femoris tendon, popliteus tendon, and the arcuate complex, which consists of the popliteofibular ligament, the arcuate ligament, and the fabellofibular ligament.41) The most common mechanisms of injury involve a direct force to the anteromedial knee with the tibia externally rotated or a hyperextension force with the tibia internally rotated. Most avulsion fractures occur on the fibula side.42) Isolated PLC injuries are rare and are more often associated with ruptures of the ACL, PCL, or both (Fig. 5).43) While fractures can easily be identified on radiographic exams, further MRI is recommended to thoroughly evaluate any accompanying injuries. Regarding treatment, conservative approaches are typically favored for grade I-II PCL injuries,44) whereas surgery may be an option for grade III injuries.45) While there is limited literature on fixation methods for avulsion fractures, strategies employing k-wires, hook plates, and suture anchors have been discussed.46,47,48,49) However, due to the prevalence of associated injuries, it is crucial to develop a patient-specific treatment plan after a comprehensive assessment.
Fig. 5
A 37-year-old male patient was injured in an in-car traffic accident. (A) An arcuate sign is observed on the plain anteroposterior radiograph (arrow). (B) A sagittal T2-weighted magnetic resonance imaging showed an accompanying posterior cruciate ligament rupture (arrow).
Medial Patellofemoral Ligament (MPFL) Avulsion Fracture
The MPFL serves as the primary ligamentous restraint against lateral dislocation of the patella and is commonly injured during acute patellar dislocations.50,51) According to previous studies, 40% to 90% of MPFL disruptions occur at the ligament’s femoral attachment.52,53) Additionally, anatomical factors such as trochlear dysplasia, an increased tibial tubercle-trochlear groove (TT-TG) distance, and patella alta are known risk factors for patellar dislocation.54) Due to the high rate of associated pathology, knee MRI is recommended for all patients with acute patellar dislocation.52) Numerous studies indicate that surgical intervention does not provide substantial advantages over nonsurgical methods for managing primary patellar dislocations (Fig. 6).55,56,57) However, due to the risk of instability, primary repair is advised for avulsion fractures on the femoral side.53) Additionally, surgical intervention is considered for avulsion fractures that occur with osteochondral fractures of the patella to restore joint congruency.51)
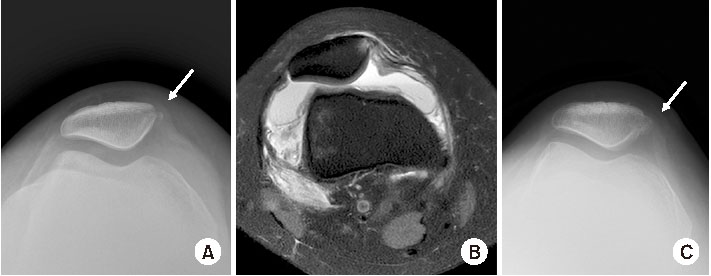
Fig. 6
(A) In an 18-year-old female with a patella dislocation, a medial patellofemoral ligament avulsion fracture is observed on a knee merchant radiograph (arrow). (B) The displacement is minimal, and no chondral injury is observed. (C) Bone union was achieved after six months of conservative treatment (arrow).
Patella Tendon, Quadriceps Tendon Avulsion Fracture
The patella is a critical bone in the articulation between the quadriceps and patellar tendons and serves as the lever for the extensor mechanism of the knee.58) Patellar avulsion fractures are relatively rare compared to other types of patellar fractures. These are often occurred in adolescents and young adults, with a higher prevalence in males due to an increased ratio of the strength of tendon and muscle to osseocartilaginous structures.59,60) The injury mechanism usually involves a rapid contraction of the quadriceps muscle while the knee is flexed, often leading to these fractures. MRI is one of the most useful tools for diagnosis because these injuries can be easily missed on plain X-rays due to the small bony components.61) Conservative treatment is usually recommended for fractures with minimal displacement and an intact extensor mechanism.3,5) In contrast, displaced fractures, indicative of a ruptured extensor mechanism, require surgical intervention to restore the extensor mechanism. Various surgical techniques have been developed for anatomical reduction and rigid fixation, including tension band wiring, transosseous sutures, intraosseous anchor sutures, and wire fixation, which are chosen based on the size and nature of the osteochondral fragment.59,60,61)
Conclusion
There are various types of avulsion fractures that can occur in the knee depending on the mechanism of injury. The severity of the damage can range from mild to multiligament injuries, and an avulsion fracture may be just one finding among many injuries. Since most fractures are accompanied by damage to other structures, MRI examinations should be performed whenever a fracture is suspected or diagnosed. Treatment should be tailored individually based on the extent of the associated injuries.
Financial support:None.
Conflict of interests:None.
References
-
McCoy JS, Nelson R. Avulsion fractures. In: StatPearls. Stat-Pearls Publishing; 2024.
-
-
Segond P. In: Recherches cliniques et expérimentales sur lesépanchements sanguins du genou par entorse. Aux bureaux du Progrès médical; 1879.French.
-
-
Stieda A. Uber eine typische verletzung am unteren femurende. Arch Klin Chir 1908;85:815–826.German.
-
-
Gupta R, Singh J, Khatri K, Bither N. Common peroneal nerve laceration in closed fibular head avulsion fracture: a case report. J Orthop Case Rep 2016;6:23–26.
-
- Related articles
-
- Current concepts in the management of phalangeal fractures in the hand
- Treatment of avulsion fractures around the knee
- Avulsion fractures around the hip joint and pelvis
- Avulsion Fractures around the Hip Joint and Pelvis
- Complications of Hand Fractures and Its Prevention
- Avulsion Fractures in the Ankle and Foot

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

