Search
- Page Path
- HOME > Search
Original Articles
- Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
- Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
- J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00276
-
 Abstract
Abstract
 PDF
PDF - Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
Methods
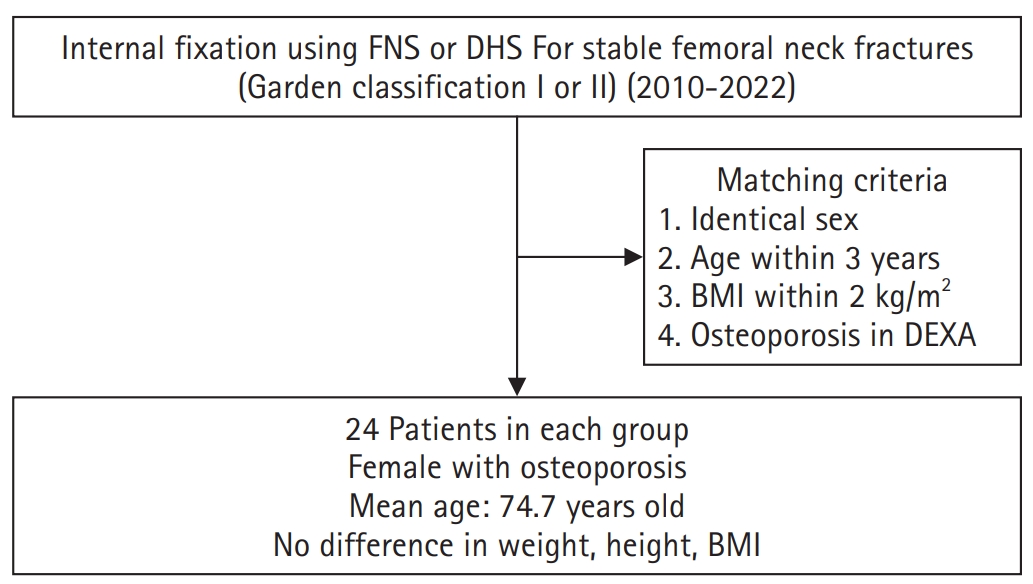
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results. Level of evidence: IV.
- 1,221 View
- 17 Download

- Hook plate versus periarticular-type volar locking plate for distal radius fractures involving the volar lunate facet in Korea: a retrospective cohort study
- Hyun-Jae Park, Joo-Hak Kim
- J Musculoskelet Trauma 2025;38(4):221-228. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00241
-
 Abstract
Abstract
 PDF
PDF - Background
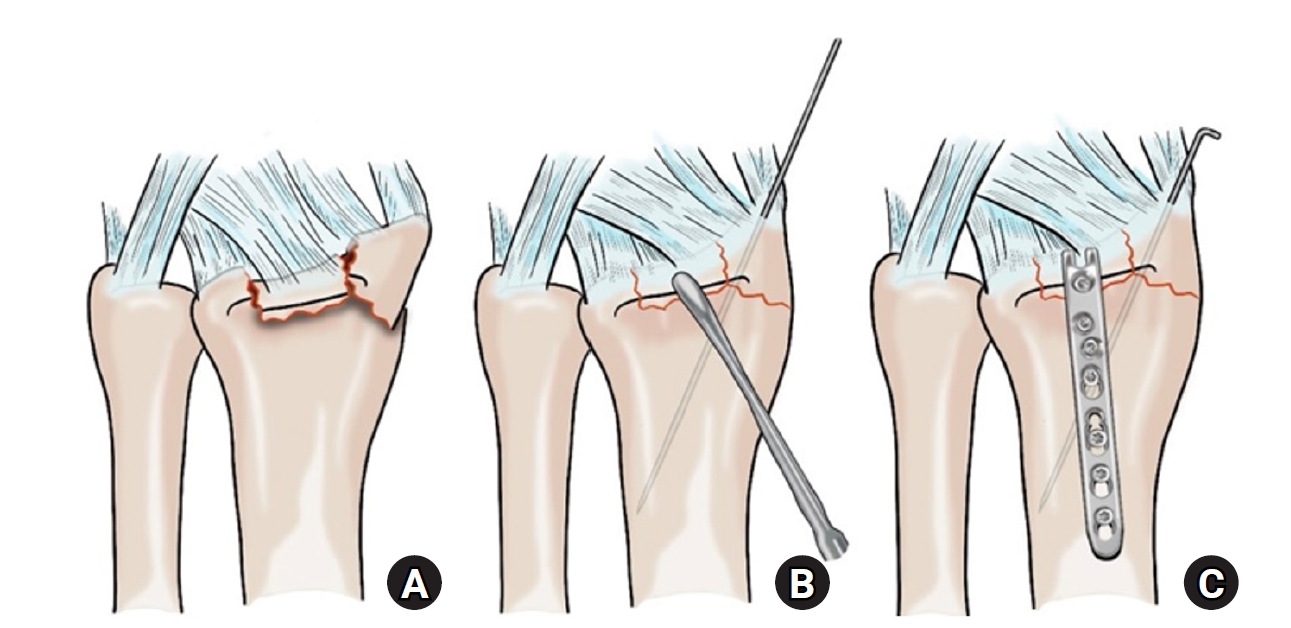
This study investigated the clinical and radiographic outcomes of hook plate (HP) fixation for volar lunate facet fractures, comparing them with periarticular-type volar locking plates (PVLPs).
Methods
A retrospective review was conducted on 24 patients with distal radius fractures involving volar lunate facet fragments who underwent surgery between January 2016 and April 2021. Patients were divided into two groups: HP (n=12) and PVLP (n=12). Radiographic union, wrist range of motion, Disabilities of the Arm, Shoulder and Hand (DASH) scores, and implant-related complications were compared. Statistical analyses included the Mann-Whitney U test and Fisher exact test.
Results
Radiographic union was achieved in all patients (100%), without secondary displacement or hardware failure. No significant differences were observed between the two groups in wrist flexion (P=0.152), extension (P=0.832), pronation (P=0.792), or supination (P=0.328). The mean DASH scores were 12.8±5.5 in the HP group and 14.6±6.0 in the volar plate group (P=0.449). One patient in the HP group experienced mild flexor tendinopathy that resolved with conservative management. No cases of tendon rupture or early reoperation were reported.
Conclusions
Fixation of volar lunate facet fractures using a HP yielded clinical and radiographic outcomes comparable to those of PVLPs, with a low rate of complications and reliable bony union. Due to its mechanical stability, compatibility with standard surgical approaches, and low risk of flexor tendon irritation, the HP may serve as a valuable alternative for managing volar lunate facet fractures. Level of evidence: IV.
- 252 View
- 9 Download

Review Article
- Atypical ulnar fractures: a narrative review of current concepts and a case of bilateral surgical management
- Chi-Hoon Oh, Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):124-132. Published online July 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00227
-
 Abstract
Abstract
 PDF
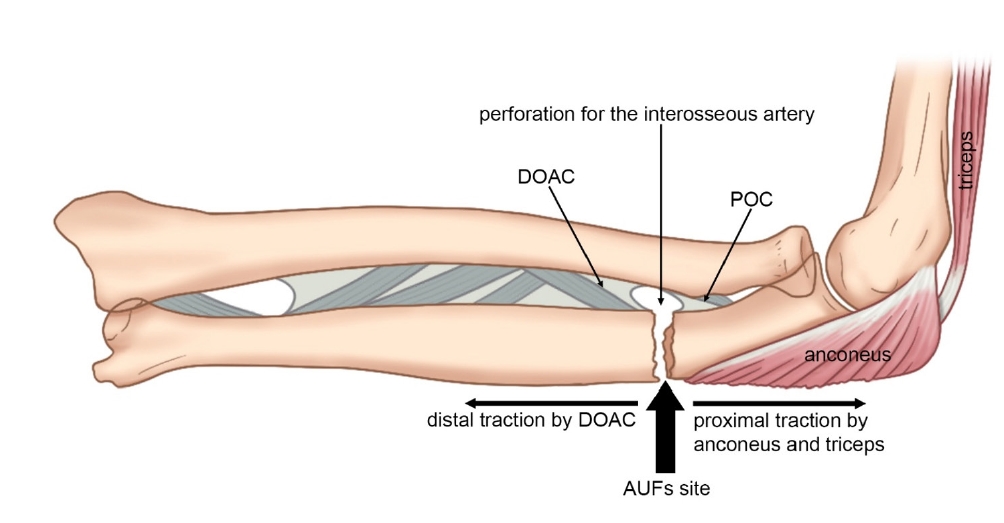
PDF - Atypical ulnar fractures (AUFs) are rare complications that are often linked to long-term antiresorptive therapy. Although atypical femoral fractures are well-studied, AUFs lack standardized diagnostic and treatment protocols. This review summarizes current knowledge on AUFs, including their pathophysiology, diagnostic criteria, and management. A case of bilateral AUFs treated with two distinct osteosynthesis methods is presented, emphasizing the principles of biological healing and mechanical stabilization.
- 1,397 View
- 39 Download

Original Articles
- Computational simulation of coracoclavicular screw insertion through the superior distal clavicular plate for clinical applications in Korean cadavers
- Hyung-Lae Cho, Ji Han Choi, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):143-151. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00122
-
 Abstract
Abstract
 PDF
PDF - Background
The study was conducted to determine the practical area for inserting the coracoclavicular (CC) screw through the plate by analyzing three-dimensional (3D) shoulder models featuring virtually implanted, actual-size plates and screws.
Methods
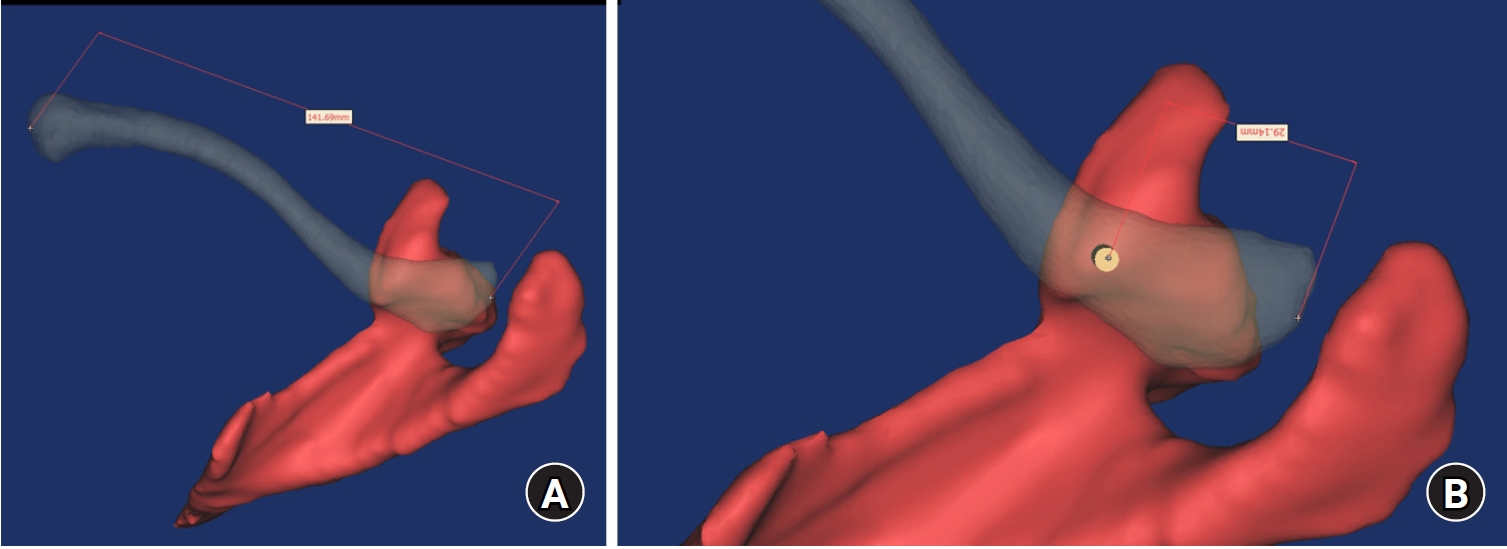
Ninety cadaveric shoulders (41 males and 49 females) underwent continuous 1.0-mm slice computed tomography scans. The data were imported into image-processing software to generate a 3D shoulder model, including the scapula and clavicle. The overlapping area between the clavicle and the horizontal portion of the coracoid process (horizontal portion_CP) was analyzed in the cranial view. A curved pelvic recon plate was virtually placed on the upper surface of the distal clavicle, and an actual-size (3.5 mm) CC screw was inserted through the plate.
Results
The distal clavicle directly overlapped with the horizontal portion_CP in the vertical direction. The overlapping area was sufficient to place the 3.5 mm and 4.5 mm-sized screws. In all shoulder models, the CC screw could be inserted through the plate into the vertical direction, with an average length of 35.5 mm (range, 26.2–62.5 mm; standard deviation, 1.2 mm). In 87 models, the CC screw was inserted through the third hole from the lateral end of the plate. Two models were inserted through the second hole, and one model through the fourth hole.
Conclusions
The upper surface of the clavicle has sufficient overlapping area to place CC screws through the plate in the vertical direction in the corresponding hole. Supplemental CC screw fixation through the plate can be performed without additional or special equipment. Level of evidence: IV
- 545 View
- 19 Download

- Biomechanical finite element analysis of a femoral neck system fixation construct for femur neck fractures and clinical implications
- Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):133-142. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00108
-
 Abstract
Abstract
 PDF
PDF - Background
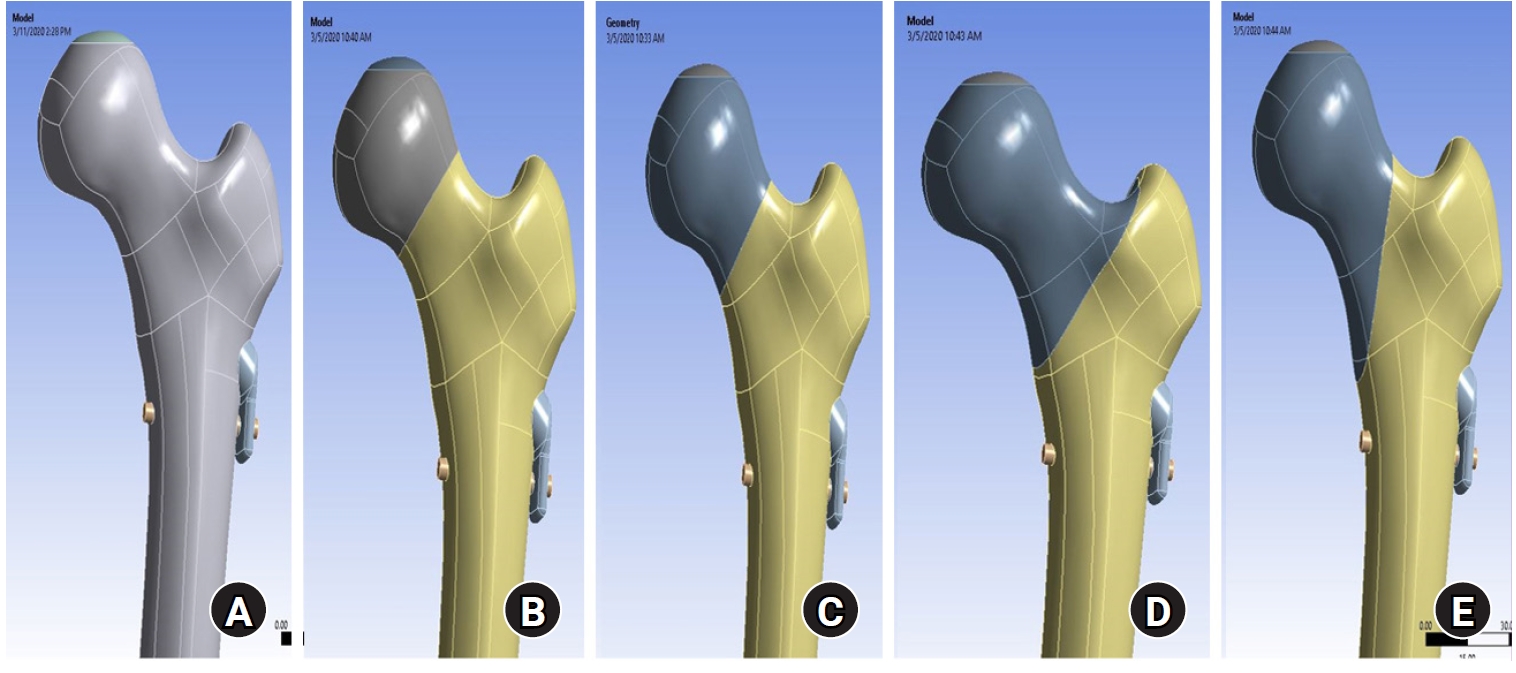
This study assessed the structural/mechanical stability of fixation constructs with a femoral neck system (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications.
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital, 68.56 MPa for a transcervical, 344.54 MPa for a basicervical, and 130.59 MPa for a vertical model. The maximum VMS of FNS was 840.34 MPa for a subcapital, 637.37 MPa for a transcervical, 464.07 MPa for a basicervical, and 421.01 MPa for a vertical model. The stress distribution of basicervical and vertical fractures differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
FNS fixation should be performed with consideration the osseous anchorage in the femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution. Level of evidence: IV.
- 1,709 View
- 77 Download

Review Article
- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
- Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(2):74-85. Published online March 31, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00024

-
 Abstract
Abstract
 PDF
PDF - Distal tibial metaphyseal fractures are commonly caused by high-energy injuries in young men and osteoporosis in older women. These fractures should be clearly distinguished from high-energy pilon fractures. Although the optimal surgical intervention methods for distal tibial metaphyseal fractures remain uncertain and challenging, surgical treatments for nonarticular distal tibia fractures can be broadly divided into two types: plate fixation and intramedullary nail (IMN) fixation. Once functional reduction is achieved using an appropriate technique, distal tibial nailing might be slightly superior to plate fixation in reducing postoperative complications. Thus, the surgical strategy should focus on functional realignment and proceed in the following sequence: (1) restoring the original tibial length, regardless of whether fibular fixation is to be done; (2) making the optimal entry point through an anteroposterior (AP) projection based on the overlapping point between the fibular tip and lateral plateau margin; (3) placing Kirschner wires (Ø2.4 mm) as blocking pins (in the AP orientation for coronal control and in the mediolateral [ML] orientation for sagittal control) as close to the upper locking hole as possible without causing further comminution on the concave aspect of the short fragment; and (4) making the the distal fixation construct with at least two ML and one AP interlocking screw or two ML interlocking screws and blocking screws. After the IMN is adequately locked, blocking pins (Ø2.4 mm) need to be replaced by a 3.5 mm screw.
-
Citations
Citations to this article as recorded by- Impact of Foot Width on Patient-Reported Outcomes Assessed by 3-Dimensional Foot Morphometry in Hallux Valgus
Jungtae Ahn, Dae-Cheol Nam, Gu-Hee Jung
Clinics in Orthopedic Surgery.2025; 17(6): 1062. CrossRef
- Impact of Foot Width on Patient-Reported Outcomes Assessed by 3-Dimensional Foot Morphometry in Hallux Valgus
- 2,430 View
- 43 Download
- 1 Crossref

Original Articles
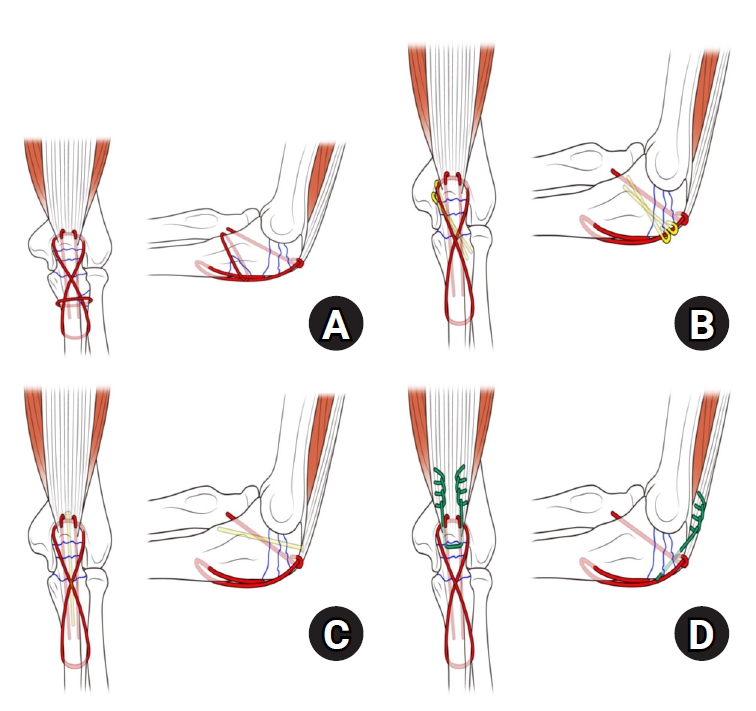
- Comparison of outcomes of reinforced tension band wiring and precontoured plate and screw fixation in the management of Mayo type IIIB olecranon fractures
- Hyun Goo Kang, Tong Joo Lee, Samuel Jaeyoon Won
- J Musculoskelet Trauma 2025;38(2):96-101. Published online February 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00059
- Correction in: J Musculoskelet Trauma 2025;38(3):168
-
 Abstract
Abstract
 PDF
PDF - Background
Mayo type IIIB olecranon fractures are characterized by significant displacement and comminution, presenting a challenge in selecting the appropriate fixation technique. This study compared the clinical and radiographic outcomes, complications, and reoperation rates of reinforced tension band wiring (TBW) and precontoured plate and screw fixation (PF) in the surgical treatment of Mayo type IIIB olecranon fractures.
Methods
This retrospective review analyzed 24 patients diagnosed with Mayo type IIIB olecranon fractures, who were treated between 2005 and 2023. Of these, 11 patients underwent reinforced TBW, and 13 received precontoured PF. Clinical outcomes were assessed using Disabilities of the Arm, Shoulder, and Hand (DASH) scores and the Mayo Elbow Performance Score (MEPS). Radiographic outcomes focused on fracture union. Operative times, complication rates, and reoperation rates were compared between the groups.
Results
Both the reinforced TBW and PF groups achieved satisfactory clinical outcomes, with no significant between-group differences in DASH and MEPS scores (P>0.05). Radiographic union was achieved in all patients. The reinforced TBW group demonstrated a significantly shorter operative time than the PF group (93.6±7.4 min vs. 132.3±13.7 min; P<0.001). Complication rates were similar between the two groups (reinforced TBW, 38.4%; PF, 36.3%), but hardware-related irritation occurred more frequently in the reinforced TBW group. Reoperations were required in 15.8% of the reinforced TBW group due to hardware irritation, whereas no reoperations were necessary in the PF group.
Conclusions
Reinforced TBW and PF are both effective surgical options for managing Mayo type IIIB olecranon fractures, yielding comparable clinical and radiographic outcomes. While reinforced TBW offers shorter operative times and lower costs, PF is associated with fewer hardware-related complications. Further prospective studies are needed to optimize treatment strategies for these complex fractures. Level of Evidence: Level III. -
Citations
Citations to this article as recorded by- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
Reva Qiu, Mallika Makkar, Richard Buckley
Injury.2025; 56(11): 112769. CrossRef
- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
- 2,039 View
- 46 Download
- 1 Crossref

- Outcomes of open reduction and internal fixation using 2.0/2.4 mm locking compression plate in isolated greater tuberosity fractures of humerus
- Sung Choi, Dongju Shin, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2025;38(1):32-39. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00005

-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to retrospectively evaluate the radiographic and clinical results of a small single or double low-profile plate fixation of 2.0/2.4 mm locking compression plate (LCP) in treating isolated greater tuberosity (GT) fractures of the humerus. Methods: From June 2015 to October 2022, patients who underwent LCP in treating isolated GT fractures of the humerus were included in this study. The radiological and clinical results were analyzed in 15 patients who underwent open reduction and internal fixation used 2.0/2.4 mm LCP. Results: Bone union was achieved in 14 patients (93.3%) and one failed case was treated with a 2.4 mm single LCP fixation. Radiological union was achieved within 10–20 weeks. Complications occurred in two patients (13.3%), including the reduction failure and shoulder stiffness. At the final follow-up, the average clinical scores were as follows: a visual analog scale for pain of 2.1 (range, 0–5) and a University of California, Los Angeles score of 27.2 (range, 18–31). Regarding range of motion (ROM), the average active ROMs were 142° for forward flexion (range, 120°–150°), 147.1° for abduction (range, 120°– 180°), and 59.3° for external rotation (range, 45°–80°). For internal rotation, the average was observed to reach the 10th thoracic vertebra (range, 1st lumbar vertebra–7th thoracic vertebra). Conclusions: The clinical and radiologic outcomes of treating isolated GT fracture using 2.0/2.4 mm LCP were favorable, and double low-profile plate fixation may be beneficial for sufficient fracture stability if possible. Level of evidence: Level IV, case series.
- 1,729 View
- 54 Download

- Restoration of Lateral Tibial Plateau Widening and Articular Depression Is Necessary to Prevent Valgus Deformities after Arthroscopic Reduction and Internal Fixation in AO/OTA 41.B2 or B3 Fractures
- Jun-Ho Kim, Kang-Il Kim, Sang-Hak Lee, Gwankyu Son, Myung-Seo Kim
- J Korean Fract Soc 2024;37(3):125-136. Published online July 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.3.125
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the factors affecting valgus deformities after arthroscopic reduction and internal fixation (ARIF) in lateral joint-depression tibial plateau fractures.
Materials and Methods
Patients with lateral joint-depression tibial plateau fractures treated with ARIF were assessed retrospectively. The radiological evaluations included the articular depression distance (ADD) and the lateral plateau widening distance (LPWD) on preoperative and postoperative computed tomography. A postoperative valgus deformity was defined as valgus malalignment (mechanical axis ≥3°) and valgus deviation (Δmechanical axis of the operated knee from the healthy knee of ≥5°). Subgroup analyses based on a postoperative valgus deformity were performed to compare the clinical outcomes, including the range of motion, patient-reported outcomes measures, and failure and osteoarthritis progression. Furthermore, factors affecting the postoperative mechanical and Δmechanical axes were assessed.
Results
Thirty-nine patients were included with a mean follow-up of 44.6 months (range, 24-106 months). Valgus malalignment and valgus deviation were observed after ARIF in 10 patients (25.6%) and five patients (12.8%), respectively. The clinical outcomes were similar in patients with and without a postoperative valgus deformity. On the other hand, lateral compartment osteoarthritis progression was significantly higher in the valgus deformity group than in the non-valgus deformity group (valgus malalignment group: 50.0% vs 6.9%, p=0.007; valgus deviation group: 60.0% vs 11.8%, p=0.032). One patient with valgus deformity underwent realignment surgery at postoperative five years. The preoperative ADD and postoperative LPWD were significantly associated with the postoperative mechanical (both, p<0.001) and Δmechanical (ADD, p=0.001; LPWD, p=0.025) axes. Moreover, the lateral meniscectomized status during ARIF was significantly associated with the Δmechanical axis (p=0.019).
Conclusion
Osteoarthritis progression was highly prevalent in patients with postoperative valgus deformity. Thus, the restoration of lateral plateau widening and articular depression and preservation of the meniscus are necessary to prevent a valgus deformity after ARIF in lateral joint-depression tibial plateau fractures.
- 2,487 View
- 39 Download

- Comparison of the Radiological Outcomes of an Anatomical Quadrilateral Surface Plate with a Pelvic Reconstruction Plate in Acetabulum Fractures
- Sung Hyun Yoon, Hee Gon Park, Dong Uk Lee
- J Korean Fract Soc 2024;37(2):95-101. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.95
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the radiological outcomes of fixation using an anatomical quadrilateral surface plate with those using a traditional pelvic reconstruction plate for fractures involving the quadrilateral surface or superomedial wall of the acetabulum.
Materials and Methods
From 2015 to 2022, 47 patients who met the inclusion and exclusion criteria were analyzed retrospectively. Internal fixation of an acetabular fracture was achieved with a pelvic reconstruction plate (n=28) or an anatomical quadrilateral surface plate (n=19). The ability to achieve immediate postoperative anatomical reduction and the long-term outcomes were assessed by confirming the arthritic changes. Immediate postoperative reduction quality and long-term radiological outcomes for post-traumatic arthritis were assessed using the Matta scoring system on standard radiographs.
Results
The assessment of immediate postoperative reduction in the pelvic reconstruction plate group was satisfactory in 16 patients (57.1%) and unsatisfactory in 12 patients (42.9%). In the anatomical quadrilateral surface plate group, the results were satisfactory in 16 patients (84.2%) and unsatisfactory in 3 patients (15.8%). When evaluating over an extended follow-up period in the pelvic reconstruction plate group, 19 patients (67.9%) demonstrated satisfactory, while 9 patients (32.1%) had unsatisfactory outcomes. In the anatomical quadrilateral surface plate group, 12 patients (63.2%) achieved satisfactory, and 7 patients (36.8%) had unsatisfactory outcomes. The immediate postoperative reduction quality was superior in the anatomical quadrilateral surface plate group (p=0.03). Comparing longterm results, the anatomical quadrilateral surface plate group did not have statistically more favorable outcomes (p=0.49).
Conclusion
In this study, the anatomical quadrilateral surface plate achieved sufficiently good radiological results without significant difference from the existing pelvic reconstruction plate. It was concluded that it is a useful option that can replace the existing metal plate in the selection of surgery for acetabular fractures.
- 808 View
- 9 Download

- Effect of Additional Medial Locking Plate Fixation and Autogenous Bone Graft for Distal Femur Nonunion after Lateral Locking Plate Fixation
- Ho Min Lee, Jong Pil Kim, In Hwa Baek, Han Sol Moon, Sun Kyo Nam
- J Korean Fract Soc 2024;37(1):30-38. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.30
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the outcomes of additional medial locking plate fixation and autogenous bone grafting in the treatment of nonunions that occurred after initial fixation for distal femoral fractures using lateral locking plates.
Materials and Methods
The study involved eleven patients who initially underwent minimally invasive lateral locking plate fixation for distal femoral fractures between January 2008 and December 2020. The initial procedure was followed by additional medial locking plate fixation and autogenous bone grafting for clinically and radiographically confirmed nonunions, while leaving the stable lateral locking plate in situ. A clinical evaluation of the bone union time, knee joint range of motion, visual analog scale (VAS) pain scores, presence of postoperative complications, and functional evaluations using the lower extremity functional scale (LEFS) were performed.
Results
In all cases, bone union was achieved in an average of 6.1 months after the secondary surgery. The range of knee joint motion, weight-bearing ability, and VAS and LEFS scores improved at the final follow-up compared to the preoperative conditions. All patients could walk without walking assistive devices and did not experience pain at the fracture site. On the other hand, three patients complained of pain in the lateral knee joint caused by irritation by the lateral locking plate; hence, lateral hardware removal was performed. One patient complained of mild paresthesia at the anteromedial incision site. Severe complications, such as deep infection or metal failure, were not observed.
Conclusion
For nonunion with stable lateral locking plates after minimally invasive lateral locking plate fixation of distal femur fractures, additional medial locking plate fixation and autogenous bone grafting, while leaving the lateral locking plate intact, can achieve successful bone union.
- 335 View
- 5 Download

- Risk Factors of Fixation Failure in Femoral Neck Fractures
- Sung Hyun Yoon, Kyu Beom Kim, Hyung Jun Lee, Kyung Wook Kim
- J Korean Fract Soc 2023;36(4):118-124. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.118
-
 Abstract
Abstract
 PDF
PDF - Purpose
Internal fixation after a femoral neck fracture (FNF) is one of the conventional treatment options for the young and active elderly patients. However, fixation failure of internal fixation is a probable complication. The treatment of fixation failure after a primary internal fixation of the FNF remains a challenge.
Materials and Methods
Between July 2002 and March 2017, 83 patients who underwent internal fixation after FNF were retrospectively analyzed. Radiological assessments, including Pauwels’ angle, fracture level, reduction quality, and bone union, were measured, preoperatively and postoperatively. Moreover, intraoperative variables such as time to surgery, surgical time, and estimated blood loss were also evaluated.
Results
The patients were divided into the fixation failure and the non-failure groups. Among the 83 patients, 17 cases (20.5%) of fixation failure after the primary internal fixation of the FNF were identi-fied. When comparing the two groups according to the radiographic data, Pauwels’ angle and the reduction quality based on Garden’s angle showed significant differences (p<0.001). Moreover, when comparing the intraoperative variables, unlike the surgical time and estimated blood loss, significant differences were noted in the time interval from injury to surgery and specifically in whether the surgery was performed within 12 hours after injury (p<0.001).
Conclusion
Pauwels’ angle, reduction quality, and time to surgery are the major factors that can predict the possibility of internal fixation failure of the FNF. Early and accurate anatomical reduction is needed to decrease complications after the internal fixation of the FNF.
- 2,395 View
- 27 Download

Case Report
- Single Percutaneous Retrograde Anterior Column Screw Fixation in a Minimally Displaced Transverse Acetabular Fracture - A Case Report -
- Seungyup Shin, Jinkyu Park, Sungho Lee
- J Korean Fract Soc 2023;36(2):57-61. Published online April 30, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.2.57
-
 Abstract
Abstract
 PDF
PDF - According to the Letournel classification, a transverse fracture is the only elementary fracture pattern that breaks both the anterior and posterior border of the innominate bone. A transverse acetabular fracture separates the innominate bone into two segments: the iliac segment and the ischiopubic segment. Therefore, minimally displaced transverse fractures can be stabilized by purchasing both segments with a large-diameter single screw. Although it is not a stable internal fixation construct compared with plates and screws, it provides sufficient stability to promote early mobilization and early weight-bearing while minimizing the risk of secondary displacement and preventing secondary complications associated with prolonged bed rest and immobilization. The authors successfully treated a case of minimally displaced transverse acetabular fracture with percutaneous column fixation using a retrograde fashion of a single anterior column screw. This report discusses the case with a literature review and deliberates the usefulness of the procedure.
- 446 View
- 9 Download

Review Article
- Fragility Fractures of the Pelvis and Sacrum
- Se-Won Lee, Ju-Yeong Kim
- J Korean Fract Soc 2023;36(1):29-38. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.29
-
 Abstract
Abstract
 PDF
PDF - The incidence of fragility fractures of the pelvis (FFP) has increased significantly due to the aging popu-lation and improved diagnostic modalities. The evaluation and treatment of these patients differ from that of high-energy pelvic ring injuries typically seen in younger patients. Therefore, it is important to classify the FFP by patterns of the classification system to standardize optimal treatment criteria and appropriate treatment strategy. However, some cases are not classifiable according to the FFP classifi-cation. A newly proposed classification that can be verified by comparing existing FFP classifications is needed to overcome the weak points. Non-operative treatment is usually considered first and should focus on early mobilization. Operative fixation should focus on stabilizing the minimally invasive pelvic ring than the reduction of fractures to facilitate early mobilization and avoid complications that can arise from comorbidities associated with immobility.
- 1,679 View
- 24 Download

Technical Note
- Usefulness of Reduction and Internal Fixation Using a 2.4 mm Hand Plating System in Type AO 33-A3 Distal Femur Fracture - Technical Note -
- Bong-Ju Lee, Ja-Yeong Yoon, Seungha Woo
- J Korean Fract Soc 2023;36(1):25-28. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.25
-
 Abstract
Abstract
 PDF
PDF - Open reduction in an AO 33-A3 class distal femur transverse and comminuted fracture is often difficult due to frequent reduction loss during surgery, leading to longer operative time and increased blood loss intra-operation. In this study, the authors report a case in which the use of an offset grid plate (OsteoMed, USA) using 2.4 mm HPS (hand plating system) eased the process of fracture reduction and achieved a stable internal fixation, ultimately leading to successful osteosynthesis. The authors experienced no need for temporary fixation devices such as K-wires or screws, which are otherwise required to stabilize the reduction. The fracture reduction was stable throughout the primary fixation of the fracture using a locking plate and screws. The authors report that the advantage of the HPS plate is fitting into the cortical contour and providing stable maintenance of fracture reduction intra-operation, which would be beneficial in certain distal femoral fracture patterns.
- 468 View
- 9 Download

Original Article
- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
- Ju-Yeong Kim
- J Korean Fract Soc 2023;36(1):1-9. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
To identify the biomechanical features for clinical applications through a computational simulation of the fixation of the Femoral Neck System (FNS) with additional cannulated screws for a Pauwels type III femoral neck fractures.
Materials and Methods
Thirty cadaveric femurs underwent computed tomography, and the images were transferred to the Mimics ® program, resulting in three-dimensional proximal femur models. A three-dimensional scan of the FNS and 6.5 mm and 7.0 mm cannulated screws was performed to enable computerized virtual fixation of FNS with additional cannulated screws for unstable femoral neck fractures. Furthermore, the cannulated screw used for additional fixation was modeled and used as a cylinder within the Ansys program. The biomechanical characteristics of these models were investigated by applying a physiological load virtually.
Results
The maximum von Mises stress value at bone was 380.14 MPa in FNS and 297.87 MPa in FNS+7.0 mm full-thread cannulated screw. The maximum von Mises stress value at FNS was 786.83 MPa in FNS and 435.62 MPa in FNS+7.0 mm full-thread cannulated screw. The FNS group showed the highest maximum von Mises stress values at bone and FNS. For total deformation, the maximum deformation value was 10.0420 mm in FNS and 9.2769 mm in FNS+7.0 mm full-thread cannulated screws. The FNS group represented the highest maximum deformation compared to the other groups.
Conclusion
Considering the anatomical spatiality and biomechanical characteristics of the FNS in unstable femoral neck fractures, when one 7.0 mm full thread cannulated screw was also fixed to the anterosuperior portion of the FNS, significant biomechanical stability was demonstrated.
- 674 View
- 8 Download

Review Article
- Current Concepts in Management of Phalangeal Fractures
- Yohan Lee, Sunghun Park, Jun-Ku Lee
- J Korean Fract Soc 2022;35(4):169-181. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.169
-
 Abstract
Abstract
 PDF
PDF - This review focused on the research published to date on the treatment of phalangeal fractures according to the anatomical location of the finger bones, excluding the thumb. In many finger fracture cases, conservative treatment should be prioritized over surgical treatment. The three determinants of surgical treatment are the presence of an intra-articular fracture, the stability of the fracture itself, and the degree of damage to the surrounding soft tissues. Surgical treatment is recommended when bone fragments of 3 mm or more and distal phalanx subluxation are present in the bony mallet finger, and the main surgical treatment is closed reduction and extension block pin fixation. It is essential to pay attention to rotational deformation asf ractures occur proximally. Since intra-articular fractures can cause stiffness and arthritis in the future, a computed tomography scan is recommended to confirm the fracture pattern. These fractures require anatomical reduction of the bone fragments within the joint, and the instability of the joint itself must be corrected. There are no superior surgical treatment methods. It is therefore advantageous for the surgeon to select a surgical method that he is familiar with and confident of performing, considering the fracture itself and various patient-related clinical factors. Nonunion is rare as a complication of a finger fracture, and finger stiffness is the most common complication. Ensuring rapid joint movement as soon as possible can reduce finger stiffness.
- 757 View
- 16 Download

Original Articles
- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- Min Sung Kwon, Young Bok Kim, Gyu Min Kong
- J Korean Fract Soc 2022;35(4):162-168. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.162
-
 Abstract
Abstract
 PDF
PDF - Purpose
Trochanteric fixation nail advanced (TFNA) was modified to compensate for the shortcomings of proximal femoral nail antirotation-II (PFNA-II). The clinical and radiological outcomes of surgeries us-ing the PFNA-II and TFNA for femoral intertrochanteric fractures were compared.
Materials and Methods
Eighty-two patients who underwent surgeries using PFNA-II or TFNA were analyzed. Only those who were followed up for more than a year were enrolled. Bone union, shortening of the femoral neck, and the tip–apex distance of the intramedullary nail were compared in the radiological findings. Clinical outcomes, including the frequency of complications and gait ability (Koval score), were also assessed.
Results
The mean follow-up periods were 22 and 19 months for the PFNA-II and TFNA groups, re-spectively. In the PFNA-II group, two cases of femoral head cut-out and one case of varus collapse were observed. In the TFNA group, only one case of femoral head cut-out was observed; however, there was no significant difference in the frequency of complications between the two groups (p=0.37). Ad-ditionally, both the shortening of the femoral neck and the decrease in gait ability after surgery showed relative improvement in the TFNA group compared to the PFNA-II group; however, there was no sig-nificant difference between the two groups.
Conclusion
The use of both TFNA and PFNA-II was associated with satisfactory outcomes. In patients who underwent surgeries using TFNA, the recovery of gait ability, frequency of complications, and short-ening of the femoral neck were not significantly different from PFNA-II, suggesting that both are suitable instrument choices for intertrochanteric fracture treatment. However, the clinical significance must be further assessed using a larger group of patients over a longer follow-up period in future studies. -
Citations
Citations to this article as recorded by- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
Jee Young Lee, Gyu Min Kong
Journal of Orthopaedic Trauma.2025; 39(7): 352. CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef
- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
- 3,043 View
- 46 Download
- 2 Crossref

- Is It Essential to Apply Tension Band Wire Fixation in Non-Comminuted Displaced Transverse Fractures of the Olecranon (Mayo Type 2A)?
- In-Tae Hong, Cheungsoo Ha, Seongmin Jo, Wooyeol Ahn, Soo-Hong Han
- J Korean Fract Soc 2022;35(3):97-102. Published online July 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.3.97
-
 Abstract
Abstract
 PDF
PDF - Purpose
Various problems have been reported with tension-band wire (TBW) fixation. With the devel-opment of anatomical plates and the improvement of fixation forces, plate fixation is currently being performed for non-comminuted, displaced, transverse olecranon fractures (Mayo Type 2A). This study compared the usefulness of the above two procedures applied in non-comminuted, displaced, transverse olecranon fractures.
Materials and Methods
Fifty-three patients with Mayo Type 2A were studied retrospectively. Twenty-nine patients underwent TBW fixation, while the other 24 underwent plate fixation. The averageoutpatient follow-up period was 10 months for both groups. Both groups were analyzed radiologically and clinically. The radiological assessment included the time to bone union, joint stability, and presence of traumatic osteoarthritis at the final follow-up. The clinical assessment included the operation time,range of motion of the elbow joint, Mayo Elbow Performance Score (MEPS), Disability of the Arm, Shoulder and Hand (DASH) score, and the presence of postoperative complications.
Results
Both groups showed stable elbow joints, proper union of fractures, and no traumatic osteo-arthritis at the final follow-up. The range of motion for the TBW fixation group was 142° (range, 3°-145°), while that of the plate fixation group was 135° (range, 4°-139°) at the final follow-up (p=0.219). The MEPS was 98.2 and 97.7 for the TBW fixation and plate fixation groups, respectively (p=0.675). The DASH score was 10.7 and 13.9 for the TBW fixation and plate fixation groups, respectively. Both groups showed excellent results, and the differences were not statistically significant (p=0.289).
Conclusion
TBW fixation and plate fixation were compared in non-comminuted, displaced, transverse olecranon fractures, and good results were obtained without significant differences between the two groups. Hence, surgeons should choose a technique they are more confident with and can be applied more efficiently.
- 340 View
- 2 Download

Review Article
- Surgical Treatment of Distal Radius Fractures and Treatment of Common Accompanying Lesions
- Joo-Hak Kim
- J Korean Fract Soc 2022;35(3):120-127. Published online July 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.3.120
-
 Abstract
Abstract
 PDF
PDF - There have been major advances in the treatment of distal radius fractures over the past 20 years. Specifically, the development of the volar locking plate in 2001 and the subsequent improvements in its design and performance have enabled the treatment of distal radius fractures that were previously considered difficult to treat. The volar plate is used for fractures and shows good results with anatomical reduction and firm fixation. However, when trying to apply it to more complex fractures, there are still difficulties related to the unique anatomical structure of the distal radius, and there are also several factors that can impair joint function and cause pain after surgery. In this review, the factors to be considered to ensure better outcomes during ORIF (open reduction and internal fixation), and external fixation in the treatment of distal radial fractures are described. The review also details the common accompanying injuries and management methods.
- 662 View
- 16 Download

Original Articles
- Minimal Invasive Fixation Methods for the Metacarpal Fracture
- Ki Youn Kwon, Jin Rok Oh, Ji Woong Kwak
- J Korean Fract Soc 2022;35(1):9-15. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.9
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the radiologic and clinical outcomes of metacarpal fractures treated with two minimally invasive surgical techniques: Kirschner wire (K-wire) fixation and headless screw fixation.
Materials and Methods
This study included 52 patients (46 males and 6 females; age 18-55 years) with distal metacarpal fractures (middle and distal shaft, including the neck) who had undergone K-wire fixation or headless screw fixation. All subjects were followed up for at least six months. The radiologic assessments were performed to evaluate the angular deformity and shortenings. The total active motion (TAM), grip strength, and patients’ subjective functional assessment were measured to evaluate the hand function. The time taken to return to work (RTW) and adverse events were analyzed.
Results
Of the 52 cases, metacarpal fractures treated with headless screw fixation and K-wire fixation showed a significant difference associated with early RTW (p<0.05). There were no significant differences between the subjects treated with K-wire fixation and those with headless screw fixation in terms of the radiologic measurement, hand function examinations, complications, and adverse events (p>0.05).
Conclusion
After a six-month follow-up, minimally invasive K-wire fixation and headless screw fixation produced similar clinical and radiologic outcomes in subjects with metacarpal fractures. Compared to K-wire fixation, however, headless screw fixation led to earlier functional recovery and might be a better option for treating metacarpal fractures in this regard.
- 491 View
- 4 Download

- Surgical Treatment of AO/OTA 33-C Intra-Articular Distal Femoral Fractures through Parapatellar Approach
- Suk Kyu Choo, Sung Tan Cho, Hyoung Keun Oh
- J Korean Fract Soc 2022;35(1):1-8. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
To report the surgical results of the parapatellar approach for AO/OTA 33-C distal femoral intra-articular fractures.
Materials and Methods
Twenty-one patients with AO/OTA 33-C distal femoral intra-articular fracture were included. There were 11 cases of C2 and 10 cases of C3 fractures. The time of union and the coronal alignment were radiographically investigated. The complications related to surgery were clinically investigated, and a functional evaluation using the range of motion and Oxford knee score was performed to compare the surgical results according to fracture classification.
Results
In all cases, sufficient articular exposure and anatomical reduction were achieved with the parapatellar approach. No cases of coronal malalignment, loss of reduction, and plate failure were noted. On the other hand, in four cases (19.0%), an autogenous bone graft was performed due to delayed union on the meta-diaphyseal fracture site. There were no differences in the radiological and clinical outcomes of the C2 and C3 fractures. The knee joint pain and Oxford knee score were poorer in the delayed union group than the normal union group.
Conclusion
The parapatellar approach is useful for achieving an anatomical reduction of the articular surface of the distal femur and minimally invasive plating technique. Although satisfactory surgical results could be obtained regardless of the degree of articular comminution, a study of the risk factors of delayed metaphyseal fusion may be necessary.
- 459 View
- 3 Download

- Comparing Outcomes of Retrograde Intramedullary Nail and Locking Plate Fixation in Distal Femoral Fractures
- Byung-Ho Yoon, Bo Kwon Hwang, Hyoung-Keun Oh, Suk Kyu Choo, Jong Min Sohn, Yerl-Bo Sung
- J Korean Fract Soc 2021;34(4):131-136. Published online October 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.4.131
-
 Abstract
Abstract
 PDF
PDF - Purpose
We compared the radiological and clinical results of fixation for distal femoral fracture (DFF) using a locking compression plate (LCP) or a retrograde intramedullary nail (RIN).
Materials and Methods
From October 2003 to February 2020, 52 cases of DFF with a minimum 1-year follow-up (with a mean follow-up of 19.1 months) were included: 31 were treated with LCP and 21 with RIN. The operation time, blood loss, and hospitalization period were compared, and the incidence of postoperative nonunion, malunion, delayed union and metal failure and other post-operative complications were evaluated and compared.
Results
There was no significant difference in the operating time between the two groups, but the mean blood loss was significantly higher in the LCP group (LCP 683.5 ml vs RIN; 134.9 ml; p=0.015). In 49 out of 52 cases, bone union was achieved without additional surgery in an average of 6.8 months, and a complete union was achieved after additional surgery in three cases of nonunion (LCP 2 cases vs RIN 1 case; p=0.065). One case of malunion and superficial infection was confirmed in each group.
Conclusion
Internal fixation using LCP and RIN give good outcomes with a low complication rate and can therefore be considered useful surgical treatments for DFF.
- 419 View
- 4 Download

- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
- J Korean Fract Soc 2021;34(3):105-111. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.105
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the clinical and radiological outcomes of TFNA (Trochanteric Fixation NailAdvanced; Depuy Synthes) for the treatment of proximal femur fractures.
Materials and Methods
This was a retrospective study of 64 patients diagnosed with a proximal femur fracture from January 2019 to November 2019. The patient’s demographic data, preoperatively and postoperatively Koval grade, modified Harris hip score, EQ-5D (Euro-Qol-5 Dimension), sliding and advancement of the blade, radiologic outcome, and complications were investigated.
Results
Fifty patients were available for evaluation at one year postoperatively. The patients reported the following: the Koval grade decreased after surgery; the modified Harris hip score decreased from 78.56±8.88 to 72.74±6.59 (p=0.149); the mean EQ-5D decreased from 0.75±0.09 to 0.72±0.06 (p=0.000). Satisfactory reduction was achieved on a postoperative radiographic examination in 47 patients in six months. Complications occurred in seven cases.
Conclusion
TFNA is considered an appropriate implant for treating intertrochanteric fractures of the femur with a minimum follow-up of one year. -
Citations
Citations to this article as recorded by- Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
Ramprasad Jasti, Prithvi Mohandas, Mahesh K Ragavan, Sunil D Magadam, Umesh Kannadasan
Cureus.2025;[Epub] CrossRef - GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
Seungcheol Kwon, Minjae Lee, Heeyeon Lee, Jihyo Hwang
Journal of Clinical Medicine.2023; 12(21): 6720. CrossRef - Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef
- Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
- 910 View
- 14 Download
- 3 Crossref

- Comparing Outcomes of Screw Fixation and Non-Fixation for Small-Sized Posterior Malleolar Fragment in Ankle Trimalleolar Fractures
- Jee-Wook Ko, Gun-Woo Lee, Keun-Bae Lee
- J Korean Fract Soc 2021;34(1):8-15. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.8
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study was undertaken to compare outcomes of screw fixation and non-fixation of a small-sized posterior malleolar fragment involving less than 25% articular surface in ankle trimalleolar fractures. Materials and Methods: A total of 32 consecutive ankles (32 patients), with posterior malleolar fragment involving 15%-25% of the joint surface, were enrolled in the study. Patients were divided into 2 groups according to whether the fragment was fixed or not (fixed: 20 ankles, non-fixed: 12 ankles). The minimum follow-up period was 12 months. Median size of the posterior malleolar fragment in the fixed and non-fixed groups were 24.6% (range, 22.3%-25.0%) and 22.1% (range, 17.4%-24.3%), respectively. Complications as well as clinical and radiographic outcomes were compared and analyzed between the two groups. Results: Clinical outcomes, including American Orthopaedic Foot & Ankle Society (p=0.501), visual analogue scale (p=0.578), and ankle range of motion (p=0.552), showed no difference between groups at the final follow-up. No differences were obtained in the radiographic outcomes, including joint stepoff (p=0.289) and fragment gap (p=0.289). Complications, including 1 case of delayed union and 1 case of wound infection, were reported in the fixed group. Conclusion: Clinical outcomes and radiographic outcomes of the non-fixation group were satisfactory and comparable to the fixation group. Our results indicate that anatomical reduction with small-sized posterior malleolar fragment in ankle trimalleolar fractures is sufficient for satisfactory outcomes, without the need for additional internal fixation.
- 694 View
- 8 Download

Review Article
- Pediatric Femoral Neck Fracture
- Joo Hyung Han, Hoon Park
- J Korean Fract Soc 2021;34(1):34-43. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.34
-
 Abstract
Abstract
 PDF
PDF - Pediatric femoral neck fracture is an uncommon injury with a high complication rate, regardless of the appropriate diagnosis and management. The bony anatomy and blood supply of the proximal femur in a skeletally immature patient differ from those in adult patients. Generally, these fractures result from high-energy trauma, but pathologic hip fractures also occur, usually from low-energy trauma. Pediatric femoral neck fractures are categorized using the Delbet classification system. This classification guides management and aids clinicians in determining the risk of avascular osteonecrosis. The ideal surgical treatment is determined by the fracture type and the age of the patient. Reduction, which is achieved using a closed or open procedure, combined with stable fixation and/or cast immobilization, is recommended for most of these fractures. Anatomical reduction within 24 hours from the injury may result in a good surgical outcome. Although the effects of capsular decompression after reduction and fixation have not been established, decompression is easy to perform and may reduce the risk of avascular necrosis. Despite appropriate management, osteonecrosis can occur after all types of pediatric femur neck fractures. Other complications include coxa vara, nonunion, and premature physeal arrest.
- 1,217 View
- 23 Download

Original Articles
- Primary Open Reduction and Plate Fixation in Open Comminuted Intra-Articular Distal Radius Fracture
- Jun-Ku Lee, Soonchul Lee, Weon Min Cho, Minkyu Kil, Soo-Hong Han
- J Korean Fract Soc 2021;34(1):16-22. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.16
-
 Abstract
Abstract
 PDF
PDF - Purpose
There are no standard surgical treatments for open distal radius fractures (DRFs), and the fracture fixator is chosen by the surgeon’s own experience. This study compared the outcomes of open reduction and volar locking plating (OR VLP) between closed and open AO-OTA type C3 DRFs. Materials and Methods: Patient data were retrospectively collected between January 2010 and December 2018. Only patients aged >18 years with AO-OTA C3 DRFs were included. After further exclusion, the patients with DRFs were divided into two groups: 13 patients with open DRFs in Group 1 and 203 patients with closed DRFs in Group 2. Data on the patient characteristics and treatment-related factors were further investigated. For the radiological evaluation, the radial height, volar height, and volar titling were measured based on the final plain radiography, and the union time was measured. The wrist range of motion (ROM), pain visual analogue scale score, and modified Mayo wrist score for function were measured at the final outpatient follow-up. Finally, the complications associated with OR VLP fixa-tion were investigated. Results: In the demographic comparison, the patients with open fractures were older (mean age, 62years) than those with closed fractures (mean age, 57 years), without a statistically significant differ-ence. The patients with open DRFs had longer antibiotic therapy and hospital stay durations. Although they presented a higher radial inclination, with statistical significance, the clinical implication was low with a mean difference of 3°. No significant differences were observed for the remaining radiological parameters, wrist ROM, and functional scores. An open DRF did not increase the complication rates,including deep infection. Conclusion: Depending on the expertise of the operating surgeon, the primary OR VLP fixation in open intra-articular comminuted DRF did not increase the incidence of deep infections and yielded similar outcomes to a closed intra-articular comminuted DRF.
- 964 View
- 10 Download

- Treatment of Proximal Femur Fracture with a Newly Designed Nail: Trochanteric Fixation Nail-Advanced (TFNA)
- Jae Youn Yoon, Ji Wan Kim
- J Korean Fract Soc 2020;33(4):189-195. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.189
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the clinical results and implant safety of a newly developed implant, Trochanteric Fixation Nail-Advanced (TFNA; DePuy Synthes), in the treatment of proximal femur fractures.
Materials and Methods
This was a retrospective cohort study of 26 patients diagnosed with proximal femur fracture and treated surgically with TFNA. The patients’ demographic data, surgical data, radiologic findings, and functional outcomes, including complications, were evaluated.
Results
The mean age of the patients was 71.2 years (95% confidence interval [CI], 68.2-74.2); 65.4% were female. The mean Carlson comorbidity index score was 5.4, and the mean Koval grade before fracture was 2.1. Fracture classification included four cases of AO/OTA 31.A1, nine cases of A2, six cases of A3, and seven cases of 32A including six cases of atypical femoral fractures. The mean operating time was 53.3 minutes (95% CI, 43.6-63.1). There were no early postoperative complications, such as postoperative infection, deep vein thrombosis, pulmonary embolism, or in-hospital death, except one case of pneumonia. The mean Koval score at the postoperative six-month follow-up was 2.9. EuroQol-5 Dimension (EQ-5D) increased from 0.05 to 0.54 after three months and 0.72 at six months postoperatively. Bone union was observed in all cases with a mean union time of 12.9 weeks. No implant failure occurred, and no cases required secondary revision surgery.
Conclusion
A new intramedullary nail system, TFNA, showed excellent outcomes and safety in the surgical treatment of proximal femur fractures. -
Citations
Citations to this article as recorded by- Intermediate Length Cephalomedullary Nails in Proximal Femoral Fractures: Review of Indications and Outcomes
Daniel Scott Horwitz, Ahmed Nageeb Mahmoud, Michael Suk
Journal of the American Academy of Orthopaedic Surgeons.2025; 33(19): 1071. CrossRef - Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
Ramprasad Jasti, Prithvi Mohandas, Mahesh K Ragavan, Sunil D Magadam, Umesh Kannadasan
Cureus.2025;[Epub] CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef - Prospective randomized multicenter noninferiority clinical trial evaluating the use of TFN-advancedTM proximal femoral nailing system (TFNA) for the treatment of proximal femur fracture in a Chinese population
Lidan Zhang, Zhijun Pan, Xiaohui Zheng, Qiugen Wang, Peifu Tang, Fang Zhou, Fan Liu, Bin Yu, Frankie K. L. Leung, Alex Wu, Suzanne Hughson, Zhuo Chen, Michael Blauth, Anthony Rosner, Charisse Sparks, Manyi Wang
European Journal of Trauma and Emergency Surgery.2023; 49(3): 1561. CrossRef - Risk of shortening in operatively treated proximal femur fractures with cephalomedullary nails with dynamically versus statically locked helical blades
Nathan Cherian, Lasun Oladeji, Cole Ohnoutka, Dan Touhey, Madeline Sauer, Kyle A. Schweser, Mauricio Kfuri, James L. Cook, Gregory J. Della Rocca, Brett D. Crist
Injury.2023; 54(2): 669. CrossRef - GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
Seungcheol Kwon, Minjae Lee, Heeyeon Lee, Jihyo Hwang
Journal of Clinical Medicine.2023; 12(21): 6720. CrossRef - Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef - Analysis of Clinical and Functional Outcomes according to the Blood Sugar Control Status at the Time of Ankle Fractures Resulting from Rotational Injuries
Jun Young Lee, Dong Seop Lim, Seung Hyun Lee, Seo Jin Park
Journal of the Korean Fracture Society.2022; 35(4): 135. CrossRef - Conventional versus helical blade screw insertion following the removal of the femoral head screw: a biomechanical evaluation using trochanteric gamma 3 locking nail versus PFN antirotation
Hong Man Cho, Kwang Min Park, Tae Gon Jung, Ji Yeon Park, Young Lee
BMC Musculoskeletal Disorders.2021;[Epub] CrossRef - Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef
- Intermediate Length Cephalomedullary Nails in Proximal Femoral Fractures: Review of Indications and Outcomes
- 2,148 View
- 20 Download
- 10 Crossref

- Does the Use of a Silicone Ring Tourniquet Help Reduce Bleeding in the Minimally Invasive Internal Fixation with Locking Plate for Distal Femoral Fractures?
- Ki-Bong Park, Hong-Ki Jin, Il-Yeong Hwang, Sung-Who Chang, Sung-Cheon Na
- J Korean Fract Soc 2020;33(3):148-153. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.148
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the usefulness of a silicone ring tourniquet by analyzing the changes in the perioperative hemoglobin (Hb) levels or amount of perioperative bleeding compared to those of a pneumatic tourniquet or no usage during minimally invasive plate fixation for distal femoral fractures.
Materials and Methods
From January 2017 to December 2019, 30 patients who underwent minimally invasive plate fixation using a locking compression plate for distal femoral fractures were evaluated and classified as a silicone ring tourniquet (Group 1), a pneumatic tourniquet (Group 2), and no usage (Group 3). The variables for analysis were age, sex, preoperative Hb (preHb), postoperative 72-hour Hb (postHb), differences between preHb and postHb (preHb-postHb), amount of intraoperative and overall transfusion, estimated unit of transfusion corrected by preHb-postHb and total transfusion (Hb-lost), amount of intraoperative and postoperative and total bleeding. One-way ANOVA was used to identify the differences between the groups.
Results
The age, sex, operation time, preHb, preHb-postHb, amount of intraoperative and overall transfusion and Hb-lost were similar in the two groups. The amount of intraoperative bleeding was significantly lower in Group 1 than Group 3 (p=0.004), but there was no difference in the amount of postoperative and total bleeding between the two groups.
Conclusion
The use of a silicone ring tourniquet in the minimally invasive plate fixation for distal femoral fractures decreased the amount of intraoperative bleeding compared to no use of a tourniquet. -
Citations
Citations to this article as recorded by- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
Tae sung Lee, Kwan Kyu Park, Byung Woo Cho, Woo-Suk Lee, Hyuck Min Kwon
BMC Musculoskeletal Disorders.2023;[Epub] CrossRef
- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
- 820 View
- 4 Download
- 1 Crossref

- Three-Dimensional Analysis of the Morphological Features in the Femur of Atypical Fracture and Practical Implications of Intramedullary Nailing
- Yong Uk Kwon, Kyung-Jae Lee, Joo Young Choi, Gu-Hee Jung
- J Korean Fract Soc 2020;33(2):87-95. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.87
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study analyzed the morphological features of the contralateral femur without an atypical fracture by constructing a three-dimensional model with an actual size medullary canal.
Materials and Methods
Lateral and anterior bowing of the shaft were measured for 21 models, and the shape of the medullary canal was analyzed. To eliminate the projection error, the anteroposterior (AP) femur was rotated internally to the extent that the centerline of the head and neck, which is the ideal position of cephalomedullary nail screw, was neutral, and the lateral femur matched the medial and lateral condyle exactly.
Results
The lateral bowing and anterior bowing was an average of 5.5° (range, 2.8°-10.7°; standard deviation [SD], 2.4°) and 13.1° (range, 6.2°-21.4°; SD, 3.2°), respectively. In the area where lateral bowing increased, the lateral cortex became thicker, and the medullary canal was straightened. On the lateral femur, the anterior angle was increased significantly, and the diameter of curvature averaged 1,370.2 mm (range, 896-1,996 mm; SD, 249.5 mm).
Conclusion
Even if the anterolateral bowing increases in the atypical femur, the medullary canal tends to be straightened in the AP direction. So, it might be considered as a reference to the modification of an intramedullary nail to increase the conformity.
- 422 View
- 4 Download

- Treatment of Isolated Lateral Malleolar Fractures Using Locking Compression Plate Fixation and Tension Band Wiring Fixation
- Woojin Shin, Seondo Kim, Jiyeon Park
- J Korean Fract Soc 2020;33(1):16-21. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.16
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to compare the clinical and radiological outcomes of locking compression plate (LCP)-screw fixation and tension band wiring (TBW) fixation in isolated lateral malleolar fractures.
MATERIALS AND METHODS
From May 2016 to August 2018, 52 patients with isolated lateral malleolar fracture were retrospectively reviewed. They were divided into 30 cases of the LCP fixation group (Group I) and 22 cases of the TBW fixation group (Group II). The clinical and radiological results of those groups were compared. Pearson chi-square tests and independent t-tests were used in the statistical analysis.
RESULTS
The mean length of the surgical incision was 8.3 cm in Group I and 4.9 cm in Group II. Radiological union was obtained at a mean of 8.4 weeks in both groups. The mean American Orthopaedic Foot and Ankle Society score was 90 (range, 85–97) and 92 (range, 85–100) in Groups I and II, respectively, at the last follow up.
CONCLUSION
Both the LCP-screw and TBW techniques revealed excellent results in isolated lateral malleolar fractures. The tension band technique may be a fine alternative method of fixation in the treatment of isolated lateral malleolar fracture.
- 882 View
- 7 Download

- Comparison of Percutaneous versus Open Pedicle Screw Fixation for Treating Unstable Thoracolumbar Fractures
- Jin Young Han, Ki Youn Kwon
- J Korean Fract Soc 2020;33(1):1-8. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study compared the clinical and radiological results between two groups of patients with percutaneous fixation or conventional fixation after hardware removal.
MATERIALS AND METHODS
The study analyzed 68 patients (43 open fixation and 43 percutaneous screw fixation [PSF] 25) who had undergone fixation for unstable thoracolumbar fractures. The radiologic results were obtained using the lateral radiographs taken before and after the fixation and at the time of hardware removal. The clinical results included the time of operation, blood loss, time to ambulation, duration of the hospital stay and the visual analogue scale.
RESULTS
The percutaneous pedicle screw fixation (PPSF) group showed better results than did the conventional posterior fixation (CPF) group (p<0.05) in regard to the perioperative data such as operation time, blood loss, and duration of the hospital stay. There were no significant differences in wedge angle, local kyphotic angle, and the ΔKyphotic angle on the postoperative plane radiographs between the two groups (p>0.05). There were no significant differences in the wedge angle and local kyphotic angle after implant removal (p>0.05) between the two groups as well. However, there were significant differences in the segmental montion angle (p<0.001), and the PPSF group showed a larger segmental motion angle than did the CPF group (CPF 1.7°±1.2° vs PPSF 5.9°±3.2°, respectively).
CONCLUSION
For the treatment of unstable thoracolumbar fractures, the PPSF technique could achieve better clinical results and an improved segmental motion angle after implant removal within a year than that of the conventional fixation method. -
Citations
Citations to this article as recorded by- A Comparison of 2 Surgical Treatments for Thoracolumbar Burst Fractures: Temporary Osteosynthesis and Arthrodesis
Halil Ibrahim Süner, Rafael Luque Pérez, Daniel Garríguez-Pérez, Marta Echevarría Marín, Jose Luis Pérez, Ignacio Domínguez
World Neurosurgery.2022; 166: e419. CrossRef
- A Comparison of 2 Surgical Treatments for Thoracolumbar Burst Fractures: Temporary Osteosynthesis and Arthrodesis
- 1,329 View
- 21 Download
- 1 Crossref

Review Article
- Fixation Options of Unstable Posterior Pelvic Ring Disruption: Ilio-Sacral Screw Fixation, S2AI Fixation, Posterior Tension Band Plate Fixation, and Spino-Pelvic Fixation
- Dong Hee Kim, Jae Hoon Jang, Myungji Shin, Gu Hee Jung
- J Korean Fract Soc 2019;32(4):240-247. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.240
-
 Abstract
Abstract
 PDF
PDF - The fixation methods that can be used for unstable posterior pelvic ring injuries have undergone many innovative changes due to the recent development of surgical and imaging techniques. After understanding the appropriate indications of first and second sacroiliac screw fixation and spinopelvic fixation, innovative methods, including the trans-sacral screw fixation, posterior tension-band plate fixation, and the S2AI screw, would be chosen and applied. Considering the anatomical complexity and proximity to the surrounding vessels and nerves in the posterior fixation, the safe zone according to the fixation options should be well understood in preoperative planning. Moreover, the functional reduction of the posterior pelvic ring through the reduction and fixation of the anterior lesion should be achieved before placing the implant to reduce the number of malposition-related complications.
-
Citations
Citations to this article as recorded by- Clinical Research through Computational Anatomy and Virtual Fixation
Ju Yeong Kim, Dong-Geun Kang, Gu-Hee Jung
Journal of the Korean Orthopaedic Association.2023; 58(4): 299. CrossRef
- Clinical Research through Computational Anatomy and Virtual Fixation
- 888 View
- 10 Download
- 1 Crossref

Original Articles
- Open Reduction and Internal Fixation in Comminuted Radial Head Fracture
- Jun Ku Lee, Tae Ho Kim, Choongki Kim, Soo Hong Han
- J Korean Fract Soc 2019;32(4):173-180. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.173
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Radial head fractures, which account for 33% of all fractures, are treated depending on the Mason classification. In comminuted type 3 fractures, open reduction internal fixation (ORIF), and radial head arthroplasty are the treatment options. This study examined the clinical outcome of modified Mason type 3 radial head fractures using ORIF with a plate.
MATERIALS AND METHODS
The medical records and image of 33 patients, who underwent ORIF for modified Mason type 3 radial head fractures, were reviewed retrospectively. The preoperative plain radiographs and computed tomography images were used to examine the location of the fracture of the radial head, the number of fragments, union, joint alignment, and traumatic arthritis at the final follow-up. The range of motion (ROM) of the elbow at the last follow-up, pain score (visual analogue scale), modified Mayo elbow score (MMES), and complications were analyzed for the clinical outcome.
RESULTS
Of the 33 cases, 14 were men and 19 were women. The mean age was 41.8 years and the average follow-up period was 19 months. The functional ROM was divided into three groups according to the number of bone fragments: 141.2°±9.3° of 3 (n=20), 123.8°±18.5° of 4 (n=7), 100.7°±24.4° of more than 4 (n=6). Furthermore, the MMES were 88.2±2.9, 83.7±4.3, and 77.3±8.4, respectively (p=0.027). Depending on the radial head fracture location, the ROM and MMES were 130.7°±7.5° and 82.1±4.7, respectively, with poor outcomes on the ulnar aspect compared to 143.1°±3.8° and 89.9±3.2 on the radial aspect.
CONCLUSION
Various factors, such as the degree of crushing and location involved in the clinical outcome. In particular, the result was poor in the case of more than four comminuted fragments or chief position located in the ulnar aspect. In this case, radial head arthroplasty may be considered in the early stages. -
Citations
Citations to this article as recorded by- Does the coronoid fracture in terrible triad injury always need to be fixed?
Yeong-Seub Ahn, Seong-Hwan Woo, Sungmin Kim, Jun-Hyuk Lim, Tae-Hoon An, Myung-Sun Kim
BMC Surgery.2024;[Epub] CrossRef - Results of the Use of Bioabsorbable Magnesium Screws for Surgical Treatment of Mason Type II Radial Head Fractures
Chul-Hyung Lee, Seungha Woo, Hyun Duck Choi
Clinics in Orthopedic Surgery.2023; 15(6): 1013. CrossRef
- Does the coronoid fracture in terrible triad injury always need to be fixed?
- 878 View
- 5 Download
- 2 Crossref

- Percutaneous Iliosacral Screw Fixation with Cement Augmentation in Osteoporotic Sacral Fracture
- Cheol hwan Kim, Young yool Chung, Seung woo Shim, Sung nyun Baek, Choong young Kim
- J Korean Fract Soc 2019;32(4):165-172. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.165
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The prevalence of osteoporotic sacral fractures is increasing. Traditionally, conservative treatment is the 1st option, but it can increase the risk of comorbidity in the elderly. To reduce the complications and allow early mobility, iliosacral screw fixation with cement augmentation will be one of the treatment options for patients with osteoporotic sacral fractures.
MATERIALS AND METHODS
This study reviewed 25 patients (30 cases) who had undergone percutaneous iliosacral screw fixation with cement augmentation for osteoporotic sacral fractures from July 2012 to December 2018 with a minimum follow up of six months. The clinical outcomes were assessed using the measures of pain (visual analogue scale [VAS] score), hospital stay and the date when weight-bearing started. All patients were evaluated radiologically for pull-out of screw, bone-union, and cement-leakage.
RESULTS
Bone union was achieved in 30 cases (100%). The mean duration of the hospital stay was 24 days (4–66 days); weight-bearing was performed on an average nine days after surgery. The VAS scores immediately (3.16) and three months after surgery (2.63) were lower than that of the preoperative VAS score (8.3) (p<0.05). No cases of cement-leakage or neurologic symptoms were encountered. Two patients (6.7%) experienced a pulling-out of the screw, but bone-union was accomplished without any additional procedures.
CONCLUSION
Percutaneous iliosacral fixation with cement augmentation will be an appropriate and safe surgical option for osteoporotic sacral fractures in the elderly in terms of early weight-bearing, pain reduction, and bone-union. -
Citations
Citations to this article as recorded by- Role of Augmentation in the Fixation of Osteoporotic Fractures
Chinmoy Das, Partha Pratim Das
Indian Journal of Orthopaedics.2025; 59(3): 294. CrossRef
- Role of Augmentation in the Fixation of Osteoporotic Fractures
- 858 View
- 4 Download
- 1 Crossref

- Treatment of the Proximal Femoral Fracture Using the New Design Cephalomedullary Nail: Prospective Outcomes Study
- Young Ho Roh, Joseph Rho, Kwang Woo Nam
- J Korean Fract Soc 2019;32(1):35-42. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.35
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study is to investigate the clinical performance and safety of Zimmer® natural nail cephalomedullary nail (ZNN CM nail) in the treatment of proximal femur fractures.
MATERIALS AND METHODS
The following research was conducted as a prospective, non-comparative, single center outcome study. Upon providing written informed consent, enrolled patients' data were collected and analyzed. Postoperative follow-up visits were scheduled at 6 weeks, 3 months, 6 months, and 1 year. Follow-up evaluation included radiographic assessment, physical examination, and quality of life and adverse events reports.
RESULTS
Thirty-nine patients were available for evaluation at one year postoperative. The patients reported the mean EuroQol-5 Dimension score increased after surgery: from 0.4 points at discharge (n=49) to 0.6 points at 1-year post-surgery (n=39). The mean Harris hip score also increased after surgery: from 56.3 points at discharge (n=49) to 72.1 points at 1 year (n=12). Bone union was seen in 64% (n=16) in 6 months and 95% (n=37) in 1 year.
CONCLUSION
The results of this 1-year follow-up study affirmed the effectiveness and safety of the ZNN CM nail in the treatment of proximal femur fractures. -
Citations
Citations to this article as recorded by- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef - Treatment of Proximal Femur Fracture with a Newly Designed Nail: Trochanteric Fixation Nail-Advanced (TFNA)
Jae Youn Yoon, Ji Wan Kim
Journal of the Korean Fracture Society.2020; 33(4): 189. CrossRef
- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- 754 View
- 0 Download
- 2 Crossref

- Surgical Results of Minimally Invasive Percutaneous Plate Fixation in the Treatment of Clavicle Shaft Fracture
- Seong Ho Yoo, Suk Woong Kang, Jae Seung Seo
- J Korean Fract Soc 2019;32(1):21-26. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.21
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study analyzed the results of the midclavicle fracture treatment using the minimally invasive percutaneous plate osteosynthesis (MIPO) technique in a retrospective manner.
MATERIALS AND METHODS
Between March 2013 and March 2017, this study analyzed 40 patients who received MIPO surgery. Excluding 1 patient who underwent surgery on another body part injury, and 4 patients who were lost to follow-up over 1 year, 40 patients were analyzed for their operation time, bone union, functional American Shoulder and Elbow Surgeons score, scar lengths, pain relief (visual analogue scale), and complications.
RESULTS
All patients over a 1 year of follow-up achieved bone union, and American Shoulder and Elbow Surgeons score 97.6 (94–100) on their shoulder functional scores. Their average operation time was 42.7 minutes, and the average scar length was 6.1 cm. Eighteen patients successfully received metal removal using the previous scar without additional incision. The clavicle length was similar in the normal and operated group.
CONCLUSION
Despite its small sample size, clavicle fixation using the MIPO technique can be considered an effective treatment because of its limited number of complications, such as nonunion and rotational angulations. -
Citations
Citations to this article as recorded by- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
Woo Jin shin, Young Woo Chung, Seon Do Kim, Ki-Yong An
Clinics in Shoulder and Elbow.2020; 23(4): 205. CrossRef
- Additional fixation using a metal plate with bioresorbable screws and wires for robinson type 2B clavicle fracture
- 855 View
- 1 Download
- 1 Crossref

Review Article
- Atypical Femoral Fractures: What Do We Know about Them?
- Beom Seok Lee, Young Kyun Lee, Heejae Won, Hyungkook Kim, Kyung Hoi Koo
- J Korean Fract Soc 2018;31(4):159-164. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.159
-
 Abstract
Abstract
 PDF
PDF - Recently, atypical femoral fractures (AFFs) have been found in patients who were prescribed bisphosphonate to prevent osteoporotic fractures. Although the occurrence of AFF is rare, there are some concerns, such as a higher risk of delayed or non-union of AFF. This paper reviews the treatment of AFF and suggests some considerations during surgery.
-
Citations
Citations to this article as recorded by- How to Improve Fracture Healing in Atypical Femoral Fractures
Sang-Jin Jeong, Chan-Woo Park, Seung-Jae Lim
Journal of the Korean Orthopaedic Association.2024; 59(1): 9. CrossRef - Atypical Femoral Fracture Occurring at a Proximal Screw Insertion Site after Plate Removal in a Distal Femoral Fracture
Jin Woo Jin, Sung Jin Shin, Jong Min Jeon
Journal of the Korean Orthopaedic Association.2024; 59(4): 314. CrossRef - Position Statement: Atypical Femoral Fracture from the Korean Society for Bone and Mineral Research in 2023
Jae-Hwi Nho, Byung-Woong Jang, Dong Woo Lee, Jae-Hyun Kim, Tae Kang Lim, Soo Min Cha, Dong-Kyo Seo, Yong-Geun Park, Dong-Geun Kang, Young-Kyun Lee, Yong-Chan Ha
Journal of Bone Metabolism.2023; 30(3): 209. CrossRef
- How to Improve Fracture Healing in Atypical Femoral Fractures
- 499 View
- 5 Download
- 3 Crossref

Case Report
- Spino-Pelvic Fixation in Unstable Sacral Fracture: A Case Report
- Jung Hwan Choi, Kyu Tae Hwang, Seung Gun Lee, Chang Nam Kang
- J Korean Fract Soc 2018;31(4):145-148. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.145
-
 Abstract
Abstract
 PDF
PDF - A 22-year-old female patient visited the emergency room (ER) after a pedestrian traffic accident in a drunken state. An examination at the ER revealed fractures at the right side of the sacral ala, sacral foramina, left anterior acetabulum, right inferior ramus, and right superior articular process of S1. She underwent spino-pelvic fixation and iliosacral (IS) screw fixation. One year later, bone union was completed and implant removal was performed and the treatment was completed without complications. The authors recommend spino-pelvic fixation and IS screw fixation for unstable sacral fractures as one of the excellent methods for obtaining posterior stability of the pelvis among the various treatments of unstable sacral fractures.
- 288 View
- 1 Download

Original Articles
- A Comparison of the Results between Internal Fixation and External Fixation in AO C Type Distal Radius Fractures
- Yoon min Lee, Hwa Sung Lee, Seok Whan Song, Jae Hoon Choi, Jong Tae Park
- J Korean Fract Soc 2018;31(3):87-93. Published online July 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.3.87
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to evaluate the radiological and clinical results of plate fixation and external fixation with additional devices for treating distal radius fracture in AO type C subtypes, and propose a treatment method according to the subtypes.
MATERIALS AND METHODS
Two hundred and one AO type C distal radius fracture patients were retrospectively reviewed. Eighty-five patients in group 1 were treated with volar or dorsal plate, and 116 patients in group 2, were treated with external fixation with additional fixation devices. Clinical (range of mtion, Green and O'Brien's score) and radiological outcomes were evaluated.
RESULTS
At the 12-month follow-up, group 1 showed flexion of 64.4°, extension of 68.3°, ulnar deviation of 30.6°, radial deviation of 20.8°, supination of 76.1°, and pronation of 79.4° in average; group 2 showed flexion of 60.5°, extension of 66.9°, ulnar deviation of 25.5°, radial deviation of 18.6°, supination of 73.5°, and pronation of 75.0° in average. The mean Green and O'Brien score was 92.2 in group 1 and 88.6 in group 2. The radial height of group 1 and group 2 was 11.6/11.4 mm; radial inclination was 23.2°/22.5°; volar tilt was 11.6°/8.7°; and the ulnar displacement was 1.27/0.93 mm.
CONCLUSION
Judicious surgical techniques during device application and tips for postoperative management during external fixation can produce similar clinical results compared with internal fixation patients. -
Citations
Citations to this article as recorded by- Intra-articular fracture distal end radius external fixation versus locking volar radius plate: A comparative study
S.P.S Gill, Manish Raj, Santosh Singh, Ajay Rajpoot, Ankit Mittal, Nitin Yadav
Journal of Orthopedics, Traumatology and Rehabilitation.2019; 11(1): 31. CrossRef
- Intra-articular fracture distal end radius external fixation versus locking volar radius plate: A comparative study
- 447 View
- 1 Download
- 1 Crossref

- How Difficult Is It to Surgically Treat AO-C Type Distal Humerus Fractures for Inexperienced Orthopedic Surgeons?
- Seong Ho Yoo, Suk Woong Kang, Moo Ho Song, Young Jun Kim, Hyuck Bae
- J Korean Fract Soc 2018;31(2):45-49. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.45
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Twenty early surgical management cases of distal humerus type-C fractures were analyzed.
MATERIALS AND METHODS
This study analyzed 20 early patients, who received surgical management of distal humerus type-C fractures, and could be followed-ups for more than one year between March of 2013 and May of 2015. The operative time, bone union time, and elbow range of motion were analyzed. The Mayo's functional score was used to evaluate their postoperative function. The primary and secondary complications of each patient immediately after each of their surgery were also reviewed.
RESULTS
All patient groups achieved bone union within an average period of 16.4 weeks. Based on the Mayo functional score, 6, 10, and 4 patients scored excellent, good, and fair, respectively. The average range of motion was a flexion contracture of 14.5° with a follow-up improvement averaging 120.7°. Six patients received nine revision operations due to major and minor complications. Two patients received revision fixation from an inadequate fixating power, and another patient received an ulnar nerve transposition. Other complications included olecranon osteotomy site displacement, superficial operational site infection, and pin loosening.
CONCLUSION
Distal humerus fractures of the AO-C type can cause a range of complications and has a very high rate of revision due to its difficult nature of surgical manageability. Therefore, it is imperative for a surgeon to expect various complications beforehand and a careful approach to their postoperative rehabilitation is essential.
- 238 View
- 0 Download

- Computational Simulation of Multiple Cannulated Screw Fixation for Femoral Neck Fractures and the Anatomic Features for Clinical Applications
- Jin Hoon Jeong, Gu Hee Jung
- J Korean Fract Soc 2018;31(2):37-44. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.37
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To identify the anatomic features for clinical applications through a computational simulation of the fixation of three cannulated screws for a femoral neck fracture.
MATERIALS AND METHODS
Thirty cadaveric femurs underwent computed tomography and the images were transferred to the Mimics® program, resulting in three-dimensional proximal femur models. A three-dimensional scan of the 7.0 mm cannulated screw was performed to enable computerized virtual fixation of multiple cannulated screws for femoral neck fractures. After positioning the screws definitively for cortical support, the intraosseous position of the cannulated screws was evaluated in the anteroposterior image and axial image direction.
RESULTS
Three cannulated screws located at the each ideal site showed an array of tilted triangles with anterior screw attachment and the shortest spacing between posterior and central screws. The central screw located at the lower side was placed in the mid-height of the lesser trochanter and slightly posterior, and directed toward the junction of femoral head and neck to achieve medial cortical support. All the posterior screws were limited in height by the trochanteric fossa and were located below the vastus ridge, but the anterior screws were located higher than the vastus ridge in 10 cases. To obtain the maximum spacing of the anterior and posterior screws on the axial plane, they should be positioned parallel to the cervical region nearest the cortical bone at a height not exceeding the vastus ridge.
CONCLUSION
The position of cannulated screws for cortical support were irregular triangular arrangements with the anterosuperior apex. The position of the ideal central screw in the anteroposterior view was at the mid-height of the lesser trochanter toward the junction of the femoral head and neck, and the anterior and posterior screws were parallel to the neck with a maximal spread just inferior to the vastus ridge. -
Citations
Citations to this article as recorded by- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
Ju-Yeong Kim
Journal of the Korean Fracture Society.2023; 36(1): 1. CrossRef
- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
- 583 View
- 0 Download
- 1 Crossref

- Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
- Kwang Hee Yeo, Nam Hoon Moon, Jae Min Ahn, Jae Yoon Jeong, Jae Hoon Jang
- J Korean Fract Soc 2018;31(1):9-17. Published online January 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.1.9
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Iliosacral screw fixation is an effective and less invasive method that is used widely for the definitive treatment of unstable pelvic ring injuries. On the other hand, fixation failures after iliosacral screw fixation have been reported in vertically unstable pelvic ring injuries. This study examined the surgical outcomes of posterior pelvic fixation using S1 and S2 screws in vertically unstable pelvic ring injuries.
MATERIALS AND METHODS
Between January 2011 and April 2016, 17 patients with vertically unstable pelvic ring injuries who met the minimum 1 year follow-up criteria were treated with internal fixation using posterior pelvic S1 and S2 screws. Their mean age was 43.9 years. According to the AO/OTA classification, 10 patients had C1, 6 had C2, and 1 had C3 injuries. Surgical treatments of single or multiple steps, where necessary, were performed by two surgeons. The clinical and radiologic outcomes were assessed retrospectively using radiographs and medical records.
RESULTS
Overall, 16 patients had bone healing without screw loosening; however, one patient could not maintain anterior pelvic fixation because of an open fracture and deep infection in the anterior pelvic ring. Of five patients who complained of neurological symptoms after injury, three had partially recovered from their neurological deficit. At the last follow-up, the clinical outcomes according to the Majeed score were excellent in 5, good in 6, fair in 4, and poor in 2 patients. The postoperative radiologic outcomes by Matta and Tornetta's method were excellent in 5, good in 8, and fair in 4 patients. Malposition of the S2 screw was identified in one case. The mean time to union was 14.6 weeks after surgery.
CONCLUSION
S1 and S2 screw fixation can be an effective treatment option for posterior pelvic stabilization in vertically unstable pelvic ring injuries when considering the surgical outcomes, such as screw loosening and loss of reduction. -
Citations
Citations to this article as recorded by- Fixation Options of Unstable Posterior Pelvic Ring Disruption: Ilio-Sacral Screw Fixation, S2AI Fixation, Posterior Tension Band Plate Fixation, and Spino-Pelvic Fixation
Dong-Hee Kim, Jae Hoon Jang, Myungji Shin, Gu-Hee Jung
Journal of the Korean Fracture Society.2019; 32(4): 240. CrossRef
- Fixation Options of Unstable Posterior Pelvic Ring Disruption: Ilio-Sacral Screw Fixation, S2AI Fixation, Posterior Tension Band Plate Fixation, and Spino-Pelvic Fixation
- 482 View
- 3 Download
- 1 Crossref

Case Report
- Arthroscopic Assisted Bioabsorbable Screw Fixation for Radial Head Fractures: A Report of Two Cases
- Bong Ju Park, Ki Yong An, Yong Suk Choi
- J Korean Fract Soc 2017;30(1):35-39. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.35
-
 Abstract
Abstract
 PDF
PDF - Most radial head fractures occur as the result of low-energy mechanisms, such as a trip or fall on the outstretched hand. These fractures typically occur when an axial load is applied to the forearm, causing the radial head to hit the capitellum of the humerus. Good results are shown with nonsurgical treatments for Mason type 2 fractures. However, if there is a limitation of elbow joint exercise or displacement of more than 2 mm, an operative treatment should be considered. We treated two patients with arthroscopic assisted bioabsorbable screw (K-METâ„¢; U&I Corporation, Uijeongbu, Korea) fixation for radial head fractures to prevent complications of open reduction and minimize radiation exposure.
-
Citations
Citations to this article as recorded by- Bioabsorbable Screws Used in Hallux Valgus Treatment Using Proximal Chevron Osteotomy
Woo-Jin Shin, Young-Woo Chung, Ki-Yong An, Jae-Woong Seo
Journal of Korean Foot and Ankle Society.2018; 22(4): 181. CrossRef
- Bioabsorbable Screws Used in Hallux Valgus Treatment Using Proximal Chevron Osteotomy
- 599 View
- 3 Download
- 1 Crossref

Original Articles
- Use of Composite Wiring on Surgical Treatments of Clavicle Shaft Fractures
- Kyung Chul Kim, In Hyeok Rhyou, Ji Ho Lee, Kee Baek Ahn, Sung Chul Moon
- J Korean Fract Soc 2016;29(3):185-191. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.185
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To introduce the technique of reducing displaced or comminuted clavicle shaft fracture using composite wiring and report the clinical results.
MATERIALS AND METHODS
Between March 2006 and December 2013, 31 consecutive displaced clavicle fractures (Edinburgh classification 2B) treated by anatomic reduction and internal fixation using composite wiring and plates were retrospectively evaluated. The fracture fragments were anatomically reduced and fixed with composite-wiring. An additional plate was applied. Radiographic assessments for the numbers of fragments, size of each fragment and amount of shortening and displacement were performed. The duration for fracture union and complications were investigated retrospectively. The mean fallow-up duration was 15.9 months.
RESULTS
The mean number of fragments was 1.7 (1-3) and the mean width of fracture fragment was 7.1 mm (4.5-10.6 mm). The mean shortening of the clavicle was 20.5 mm (10.3-36.2 mm). The mean number of composite wires used in fixation was 1.9 (1-3). Radiographic union was achieved in all patients with a mean time to union of 11.6 weeks. There were no complications including metal failure, pin migration, nonunion, or infection.
CONCLUSION
The composite wiring was suitable for fixation of small fracture fragment and did not interfere with the union, indicating that it is useful for treatment of clavicle shaft fracture.
- 313 View
- 1 Download

- Orthogonal Locking Compression Plate Fixation for Distal Humeral Intraarticular Fractures
- Hyoung Keun Oh, Suk Kyu Choo, Kyoung Hwan Koh, Ji Woong Yeom
- J Korean Fract Soc 2016;29(3):178-184. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.178
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To investigate the surgical outcomes of orthogonal locking compression plate fixation for distal humeral intraarticular fractures.
MATERIALS AND METHODS
This study included 18 patients presenting a distal humeral intraarticular fracture who were treated with orthogonal locking compression plate fixation. According to the AO/OTA classification, there were eight C2 and ten C3 fractures. We evaluated radiologic outcomes, clinical results with range of motion, operation-related complications, and functional score by Mayo elbow performance score (MEPS).
RESULTS
The a verage u nion t ime was 3.5 months, and there was no c ase of r eduction l oss of a rticular f racture at t he last follow-up. Additional surgical procedures were needed in the three cases of C3 fractures. There was one case of heterotrophic ossification and one case of K-wire irritation. The average range of motion of elbow joint was 7° to 122°, and functional results were graded as 14 excellent, three good, and one fair by MEPS.
CONCLUSION
Anatomical reduction and internal fixation with orthogonal locking compression plate could provide satisfactory surgical outcomes for the treatment of distal humeral intraarticular fracture.
- 346 View
- 0 Download

- Hypoesthesia after Open Reduction and Plate Fixation of Clavicular Midshaft Fractures: Correlation with Plate Location and Clinical Features of Hypoesthesia
- Seong Hun Kim, Joon Yub Kim, Kyoung Hwan Koh, Myung Gon Jung, Jae Ho Cho
- J Korean Fract Soc 2016;29(2):121-127. Published online April 30, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.2.121
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study is to evaluate the correlation between the location of the plate and the incidence of clavicular hypoesthesia and the clinical features of patients with clavicular hypoesthesia after open reduction and internal fixation of clavicular midshaft fractures.
MATERIALS AND METHODS
Seventy-eight patients who underwent open reduction and plate fixation for clavicle midshaft fractures between March 2013 and October 2014 were assessed for eligibility. The total clavicular length (A), the distance to the medial end of the plate from the sternoclavicular joint (B), and the distance to the lateral end of the plate from the sternoclavicular joint (C) were measured. Correlation between the location of the clavicular plate and the incidence of clavicular hypoesthesia was evaluated. In addition, the severity, and recovery of hypoesthesia were evaluated. Patient satisfaction, pain visual analogue scale were evaluated regarding hypoesthesia.
RESULTS
The incidence of hypoesthesia was 32.1% (25/78 patients). No correlation was observed with respect to the location of the clavicular plate and the incidence of clavicular hypoesthesia (p=0.666 at the medial end, p=0.369 at the lateral end). Recovery from hypoesthesia was observed in 23 out of 25 patients (p=0.008). Patient satisfaction and pain showed negative correlation with the incidence of hypoesthesia (p=0.002 and p=0.022).
CONCLUSION
There was no correlation between clavicular hypoesthesia and the plate location. Although most cases of hypoesthesia were recovered, we should try to avoid hypoesthesia due to the negative 'correlation' with patient satisfaction and pain.
- 396 View
- 0 Download

Case Report
- Medial and Lateral Dual Plate Fixation for Osteoporotic Proximal Humerus Comminuted Fracture: 2 Case Reports
- Sam Guk Park
- J Korean Fract Soc 2016;29(1):61-67. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.61
-
 Abstract
Abstract
 PDF
PDF - Some proximal humeral fractures in elderly patients are accompanied by medial metaphyseal comminution and quality of the bone is so poor that head preserving osteosynthesis seems to be amenable. In cases of medial metaphyseal comminution, lateral locking compression plate (LCP) fixation also has a tendency to become a matter of screw cut out or loss of fixation. The author reports on successful treatment of two osteoporotic proximal humeral fractures combined with medial meta-physeal comminution, with application of additional direct medial supporting plate fixation. Medial plate fixations were added when the fractures were still unstable after the conventional lateral LCP fixation and anterior circumflex humeral arteries had been ruptured before. The fixations were stable enough to start exercise immediately after surgery. The inclinations of the humeral neck were not changed until the last follow-up and clinical results were satisfactory without humeral head osteonecrosis which was a concern.
-
Citations
Citations to this article as recorded by- Dual-Plate Fixation for Proximal Humerus Fractures With Unstable Medial Column in Patients With Osteoporosis
Hyun-Gyu Seok, Sam-Guk Park
Journal of Orthopaedic Trauma.2023; 37(10): e387. CrossRef - The plate fixation strategy of complex proximal humeral fractures
Qi Sun, Xiaoming Wu, Lei Wang, Ming Cai
International Orthopaedics.2020; 44(9): 1785. CrossRef - Biomechanical evaluation of a novel dualplate fixation method for proximal humeral fractures without medial support
Yu He, Yaoshen Zhang, Yan Wang, Dongsheng Zhou, Fu Wang
Journal of Orthopaedic Surgery and Research.2017;[Epub] CrossRef
- Dual-Plate Fixation for Proximal Humerus Fractures With Unstable Medial Column in Patients With Osteoporosis
- 600 View
- 6 Download
- 3 Crossref

Original Articles
- The Usefulness of Poller Screw with Antegrade Nailing in the Initial Treatment of Infraisthmal Femur Shaft Fracture
- Jeong Hyun Yoo, Hyoung Soo Kim, Chang Geun Kim, Ho Il Kwak, Sang Heon Song
- J Korean Fract Soc 2015;28(4):230-236. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.230
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to evaluate the radiologic and clinical outcomes after intramedullary nailing with Poller screw insertion at initial stage in infraisthmal femur shaft fractures.
MATERIALS AND METHODS
Seven consecutive patients (7 femurs) treated with antegrade intramedullary nailing with Poller screw insertion for the infraisthmal femur shaft fracture were reviewed retrospectively. There were 4 male and 3 female patients. Mean age was 46.1 years (20-72 years). Operative time including Poller screw insertion, time for union, malalignment, and range of motion were evaluated.
RESULTS
All 7 cases had primarily healed successfully. Mean time for radiologic union was 19.1 weeks (16-24 weeks) postoperatively. One case had 5 degree valgus malalignment. One case of 15 mm shortening was reported and he required shoe lift orthosis. All cases had a full range of motion in hip and knee joint.
CONCLUSION
Antegrade intramedullary nailing with Poller screw insertion is useful in the initial treatment of infraisthmal femur shaft fracture, because it could provide additional stability. An additional 20 minutes were required but a Poller screw should be considered according to the anatomic location of a femur shaft fracture.
- 432 View
- 2 Download

- Analysis of Low-Energy Trochanter Fracture Using the Multiplanar Computed Tomography Image: Application for Intramedullary Nail Fixation
- Gu Hee Jung, Sung Keun Heo, Hyun Je Seo
- J Korean Fract Soc 2015;28(3):155-162. Published online July 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.3.155
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this radiologic study was to evaluate the geographic patterns of low-energy trochanteric fractures using multiplanar computed tomography (CT) images for application of intramedullary nailing.
MATERIALS AND METHODS
In this study, 117 trochanteric fractures (stable fracture, 39 cases, unstable fractures, 78 cases) sustained from simple slip-down were assessed. The mean age was 78.4 years (range, 60-96 years). Multiplanar CT images were assessed for evaluation of geographic features of trochanteric fracture, and the fracture exit and geographic patterns were analyzed.
RESULTS
The medial and lateral exit of the trochanteric fracture showed no statistical difference by age, bone density, and comorbid disease. The exit was located at an average distance of 10.2 mm (range, 1.0-22.2 mm) from the tip of the greater trochanter (GT), and the medial exit, average distance of 8.1 mm (range, 0.0-18.3 mm) from the tip of the lesser trochanter. It was also found that there was no comminution around the anteromedial cortex of the fracture, and its contact loss was from fracture deformity.
CONCLUSION
Because of no comminution, the contact restoration of the anteromedial cortex resulted in correction of fracture deformity and reduction. Trochanteric nailing by GT tip could be fixed through the proximal fragment of the fracture because the lateral exit is placed at an average distance of 10.2 mm from the GT tip.
- 311 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


