Articles
- Page Path
- HOME > J Korean Fract Soc > Volume 37(3); 2024 > Article
- Original Article Restoration of Lateral Tibial Plateau Widening and Articular Depression Is Necessary to Prevent Valgus Deformities after Arthroscopic Reduction and Internal Fixation in AO/OTA 41.B2 or B3 Fractures
- Jun-Ho Kim, Kang-Il Kim, Sang-Hak Lee, Gwankyu Son, Myung-Seo Kim
-
Journal of The Korean Orthopaedic Trauma Association 2024;37(3):125-136.
DOI: https://doi.org/10.12671/jkfs.2024.37.3.125
Published online: July 31, 2024
- 2,910 Views
- 44 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
This study examined the factors affecting valgus deformities after arthroscopic reduction and internal fixation (ARIF) in lateral joint-depression tibial plateau fractures.
Materials and Methods
Patients with lateral joint-depression tibial plateau fractures treated with ARIF were assessed retrospectively. The radiological evaluations included the articular depression distance (ADD) and the lateral plateau widening distance (LPWD) on preoperative and postoperative computed tomography. A postoperative valgus deformity was defined as valgus malalignment (mechanical axis ≥3°) and valgus deviation (Δmechanical axis of the operated knee from the healthy knee of ≥5°). Subgroup analyses based on a postoperative valgus deformity were performed to compare the clinical outcomes, including the range of motion, patient-reported outcomes measures, and failure and osteoarthritis progression. Furthermore, factors affecting the postoperative mechanical and Δmechanical axes were assessed.
Results
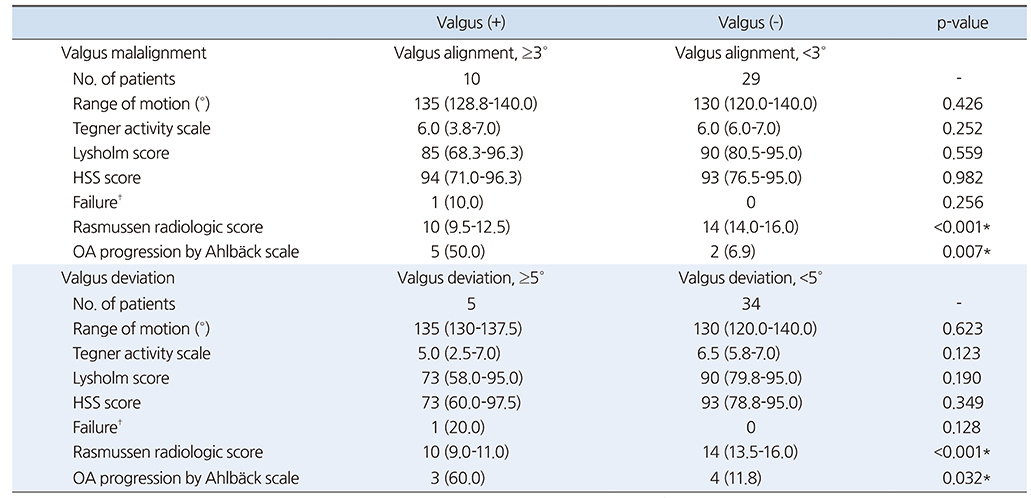
Thirty-nine patients were included with a mean follow-up of 44.6 months (range, 24-106 months). Valgus malalignment and valgus deviation were observed after ARIF in 10 patients (25.6%) and five patients (12.8%), respectively. The clinical outcomes were similar in patients with and without a postoperative valgus deformity. On the other hand, lateral compartment osteoarthritis progression was significantly higher in the valgus deformity group than in the non-valgus deformity group (valgus malalignment group: 50.0% vs 6.9%, p=0.007; valgus deviation group: 60.0% vs 11.8%, p=0.032).
One patient with valgus deformity underwent realignment surgery at postoperative five years. The preoperative ADD and postoperative LPWD were significantly associated with the postoperative mechanical (both, p<0.001) and Δmechanical (ADD, p=0.001; LPWD, p=0.025) axes. Moreover, the lateral meniscectomized status during ARIF was significantly associated with the Δmechanical axis (p=0.019).
Conclusion
Osteoarthritis progression was highly prevalent in patients with postoperative valgus deformity. Thus, the restoration of lateral plateau widening and articular depression and preservation of the meniscus are necessary to prevent a valgus deformity after ARIF in lateral joint-depression tibial plateau fractures.
Published online Jul 25, 2024.
https://doi.org/10.12671/jkfs.2024.37.3.125
 , M.D., Ph.D.,
Kang-Il Kim
, M.D., Ph.D.,
Kang-Il Kim , M.D., Ph.D.,
Sang-Hak Lee
, M.D., Ph.D.,
Sang-Hak Lee , M.D., Ph.D.,
Gwankyu Son
, M.D., Ph.D.,
Gwankyu Son , M.D.
and Myung-Seo Kim
, M.D.
and Myung-Seo Kim , M.D., Ph.D.
, M.D., Ph.D.
Abstract
Purpose
This study examined the factors affecting valgus deformities after arthroscopic reduction and internal fixation (ARIF) in lateral joint-depression tibial plateau fractures.
Materials and Methods
Patients with lateral joint-depression tibial plateau fractures treated with ARIF were assessed retrospectively. The radiological evaluations included the articular depression distance (ADD) and the lateral plateau widening distance (LPWD) on preoperative and postoperative computed tomography. A postoperative valgus deformity was defined as valgus malalignment (mechanical axis ≥3°) and valgus deviation (Δmechanical axis of the operated knee from the healthy knee of ≥5°). Subgroup analyses based on a postoperative valgus deformity were performed to compare the clinical outcomes, including the range of motion, patient-reported outcomes measures, and failure and osteoarthritis progression. Furthermore, factors affecting the postoperative mechanical and Δmechanical axes were assessed.
Results
Thirty-nine patients were included with a mean follow-up of 44.6 months (range, 24-106 months). Valgus malalignment and valgus deviation were observed after ARIF in 10 patients (25.6%) and five patients (12.8%), respectively. The clinical outcomes were similar in patients with and without a postoperative valgus deformity. On the other hand, lateral compartment osteoarthritis progression was significantly higher in the valgus deformity group than in the non-valgus deformity group (valgus malalignment group: 50.0% vs 6.9%, p=0.007; valgus deviation group: 60.0% vs 11.8%, p=0.032). One patient with valgus deformity underwent realignment surgery at postoperative five years. The preoperative ADD and postoperative LPWD were significantly associated with the postoperative mechanical (both, p<0.001) and Δmechanical (ADD, p=0.001; LPWD, p=0.025) axes. Moreover, the lateral meniscectomized status during ARIF was significantly associated with the Δmechanical axis (p=0.019).
Conclusion
Osteoarthritis progression was highly prevalent in patients with postoperative valgus deformity. Thus, the restoration of lateral plateau widening and articular depression and preservation of the meniscus are necessary to prevent a valgus deformity after ARIF in lateral joint-depression tibial plateau fractures.
초록
목적
본 연구는 경골 외측 고평부 관절면 함몰 골절로 관절경 정복을 이용한 수술적 치료를 시행한 환자들에게 발생하는 외반 변형의 결과 및 발생 원인에 대해 알아보고자 한다.
대상 및 방법
2011년 5월부터 2019년 12월까지 관절면의 함몰이 동반된 AO/OTA 41.B2 및 B3에 해당하는 골절에 대해 관절경 정복 및 내고정술을 시행하고 최소 24개월 이상 추시가 가능한 39예의 환자를 대상으로 하였다. 수술 전, 후 CT 검사에서 ADD 및 LPWD를 측정하였다. 단순 방사선 검사상 수술 후 외반 변형 여부를 평가하였으며 관절염의 진행 여부를 평가하였다. 또한 수술 후 외반을 일으키는 원인을 분석해 보았다.
결과
술 후 외반 변형은 10예에서 확인되었고, 관절염이 악화된 환자는 외반 변형된 군에서 유의하게 높게 나타났다. 다중선형 회귀분석 검사상 수술 전 ADD가 큰 경우, 수술 시 외측 연골판 절제술을 같이 시행한 경우, 수술 후 LPWD가 클수록 수술 후 유의하게 외반 변형을 일으키는 인자로 확인되었다.
결론
경골 외측 고평부 관절면 함몰 골절의 수술적 치료 후 발생하는 외반 변형은 관절염의 악화를 초래할 수 있어 주의해야 하며, 수술 시 정확한 관절면의 정복뿐 아니라 경골 고평부의 너비 정복에도 유의해야 할 것으로 생각된다.
Introduction
The optimal goal of the treatment of tibial plateau fracture is the satisfactory recovery of function and prevention of malalignment and osteoarthritic progression.1,2,3) Successful treatment depends on the anatomical reduction of the articular surface, restoration of the mechanical axis, and treatment of concomitant injuries.1,2) Arthroscopic reduction and internal fixation (ARIF) has recently been suggested especially for lateral joint depression tibial plateau fractures such as Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association (AO/OTA) 41.B2 or B3 fractures.4,5) Under direct visualization of intra-articular fractures and concomitant injuries via arthroscopy, surgeons could achieve accurate reductions of the articular depressions of fracture fragments and proper management of combined injuries such as lateral meniscus (LM) tears.4,5) Owing to these advantages, a recent study showed that ARIF led to better radiologic results than open reduction and internal fixation (ORIF).6) Therefore, ARIF has been deemed a reliable, effective, and safe treatment for lateral joint depression tibial plateau fractures.7)
Meanwhile, preoperative articular depression distance (ADD) and lateral meniscectomized status are known factors for valgus deformity and subsequent osteoarthritis in lateral joint depression tibial plateau fracture after ORIF.8,9,10) Thus, much attention has recently been directed toward the restoration of the joint depression to minimize intra-articular step-off and meniscal repair of LM tears during ARIF.4,11,12) Despite these efforts, valgus deformity and subsequent osteoarthritis progression may occasionally develop in lateral joint depression tibial plateau fracture after ARIF.4,7) However, there is a lack of evidence regarding valgus deformity and investigating factors affecting valgus deformity after ARIF. Moreover, limited studies have evaluated both preoperative and postoperative findings of computed tomography (CT), which may be a more accurate and reliable radiological method.
Thus, the current study retrospectively assessed lateral joint depression tibial plateau fractures to determine the factors affecting valgus deformity after ARIF using preoperative and postoperative CT evaluations. The proposed hypothesis was that the restoration of lateral plateau widening as well as articular surface and preservation of the LM would be necessary to prevent valgus deformity after ARIF in lateral joint-depression tibial plateau fractures as both joint depression and widening could lead to joint incongruity resulting in the disruption of joint mechanics.13,14)
Materials and Methods
1. Study design and patient selection
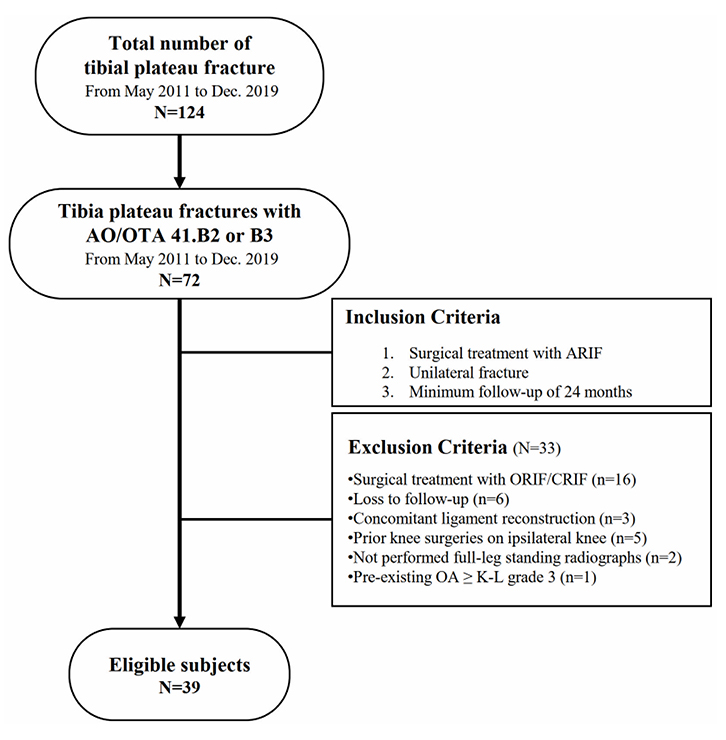
From May 2011 to December 2019, a total of 124 consecutive tibia plateau fractures at a single institution were retrospectively assessed for eligibility. Of 124 fractures, 72 were AO/OTA 41.B2 or B3 fractures (tibial plateau fractures of Schatzker type 2 or 3) and assessed for eligibility. The inclusion criteria of the current study were as: (1) patients who underwent ARIF, (2) unilateral lower limb fracture; and (3) a minimum follow-up of 24 months. Of 72 fractures, 33 were excluded for (1) surgical treatment with ORIF or closed reduction and internal fixation (n=16), (2) follow-up of <24 months (n=6), (3) concomitant ligament reconstruction (n=3), (4) prior knee surgeries on ipsilateral knee (n=5), (5) absence of full-leg standing radiographs (n=2), and (6) pre-existing osteoarthritis of Kellgren–Lawrence (K-L) grade 3 or 4 (n=1). Finally, the current study enrolled 39 patients (Fig. 1). The data collected from the patients’ medical records included (1) demographic characteristics such as age, sex, and body mass index and (2) mean follow-up period. This study has been approved from the Institutional Review Board of Kyung Hee University Hospital at Gangdong (approval No. KHNMC 2022-02-010), and the written informed consent was obtained from all patients.
Fig. 1
Flow diagram illustrating patient enrolment. AO/OTA: Arbeitsgemeinschaft für Osteosynthesefragen/Orthopedic Trauma Association, ARIF: arthroscopic reduction and internal fixation, ORIF: open reduction and internal fixation, CRIF: closed reduction and internal fixation, OA: osteoarthritis, K-L: Kellgren–Lawrence.
2. Surgical technique and rehabilitation protocol
All surgeries were performed by two experienced knee specialists (K.I.K. and S.H.L., with >25 years and >15 years, respectively). The detailed surgical technique of ARIF for lateral joint depression tibial plateau fractures was performed as previously described.4) During diagnostic arthroscopy, the precise morphology of intra-articular fractures and combined injuries were identified after removing the hematoma and small fragments around the fracture site. A meniscal retractor or probe was then used to clearly visualize the fracture site. To elevate the depressed fragment, a 2.4-mm guide pin was inserted at the center to the posterior region of the depressed main fragment. With a guide for anterior cruciate ligament reconstruction, a 7- or 8-mm reamer was used to create a cortical window at the anterior tibial cortex. A bone impactor was subsequently inserted through the cortical window to elevate the depressed fragments under arthroscopic and fluoroscopic guidance. If the reduction was acceptable, large reduction forceps were deployed to grab both tibial condyles to maintain the stable reduction of the split fracture fragment. Then, the bony defect was filled with allogenous cancellous bone graft and the reduced fracture was fixed with a locking compression plate (angular stable plate; AO Synthes) via the anterolateral approach. After ARIF of the fracture, the combined intra-articular injuries were managed according to their conditions. In cases of LM tears with peripheral longitudinal tears, LM repair was mostly performed with the inside-out or modified outside-in technique using a suture hook (Linvatec) with a straight neck and a spinal needle using absorbable suture material (polydioxanone suture, PDS; Ethicon).15)
The same postoperative rehabilitation protocol was applied in all cases, although two surgeons performed the ARIF. A splint was applied for 1 week to maintain knee extension. Then, passive range of motion (ROM) was allowed with a limitation of a knee flexion of 90° under a hinged brace until 4 weeks postoperatively. After 4 weeks, the patients were gradually allowed to achieve a wide ROM. Non–weight-bearing with a crutch was allowed at least 4 postoperative weeks. Partial weight-bearing was additionally permitted during postoperative weeks 4-8, then full weight-bearing was allowed. Quadriceps muscle-setting exercises were encouraged after surgery when the postoperative pain had subsided.
3. Radiological evaluation
Preoperative anteroposterior (AP) and lateral radiographs were obtained. Preoperative and postoperative CT scans were performed within 1 week after surgery in all patients to assess the fracture pattern, amount of joint depression, and postoperative reduction status. The patients were followed up at 4 weeks and 3, 6, and 12 months, and then every year postoperatively. Simple AP, lateral, and full-leg standing AP were routinely obtained when full weight-bearing was allowed after surgery. Bone union was defined as the formation of a bridging callus on four cortices across the fracture line and was assessed on serial AP and lateral radiographs of the knee joint.16)
The radiological measurements included ADD and lateral plateau widening distance (LPWD) on preoperative and postoperative CT scans (Fig. 2). ADD was measured between the joint line of the unaffected contralateral plateau and the maximal articular depression point on coronal CT images.11,12,17,18) LPWD was measured between two perpendicular lines to the joint line on coronal CT images, which were the lateral femoral epicondyle and the most lateral point of the lateral tibial plateau, showing maximal widening distance on coronal CT images.17) The reduction rates of the ADD and LPWD were calculated as follows: ([preoperative value–postoperative value]/preoperative value)×100. Four-column and nine-segment classifications were assessed on preoperative CT, including anterolateral and posterolateral fragments.19) The degree of osteoarthritis was evaluated using the Rasmussen radiologic system20) and the Ahlbäck scale.21) The grades of the Rasmussen radiologic system were classified as excellent (18), good (12-17), fair (6-11), and poor (<6).20) For lower limb alignment, the mechanical axis of the operated knee and the Δmechanical axis (operated knee–healthy knee) were evaluated using the hip-knee-ankle angle (HKAA) on the latest full-leg standing radiography.22) Valgus deformity was assessed based on valgus malalignment and deviation. Valgus malalignment was defined as a mechanical axis of +3° (HKAA, 183°) or more23) while valgus deviation was defined as a Δmechanical axis of ≥5°.24) Subgroups were defined according to the presence of valgus deformities. Two orthopedic surgeons (J.H.K. and G.S.) evaluated the radiological variables in a blinded manner.
Fig. 2
Radiological measurements including articular depression distance (ADD) and lateral plateau widening distance (LPWD) on preoperative and postoperative computed tomography (CT) scans. (A) ADD was measured between the joint line of the unaffected contralateral plateau and the maximal articular depression point on coronal CT images. (B) LPWD was measured between two perpendicular lines to the joint line on coronal CT images, which were the lateral femoral epicondyle and the most lateral point of the lateral tibial plateau, showing maximal widening distance on coronal CT images.
4. Clinical evaluation
The clinical evaluations included the Tegner activity scale,25) Lysholm knee score,26) and hospital for special surgery (HSS) score27) at the latest follow-up. The Tegner activity scale was obtained for both pre-injury status and at the latest follow-up. Patients who did not regularly visit were contacted by telephone. The complications included infection, symptomatic deep vein thrombosis, compartment syndrome, and neural palsy. Failure was defined as the need for additional surgery on the operated knee, including arthroscopic, realignment, or arthroplasty surgeries. The clinical outcomes were compared between subgroups, depending on the valgus alignment or deviation.
5. Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows (ver. 23.0; IBM Corp.) and G-power version 3.1.5 (University Düsseldorf). Continuous data are presented as mean±standard deviation (range) or median (interquartile range). All dependent variables were tested for the normality of the distributions and equality of variance using Kolmogorov–Smirnov tests and analyzed using parametric or nonparametric tests, as appropriate. Continuous variables were analyzed using Student’s t-test or Mann–Whitney U tests, depending on the number of groups and the normality of the distributions. Categorical variables were analyzed using chi-squared or Fisher’s exact tests. Paired t-test or Wilcoxon signed-rank tests were performed to analyze the changes between preoperative and postoperative values. A univariable simple regression analysis was performed to determine the factors affecting the mechanical or Δmechanical axes. The eligibility criterion for the multivariate linear regression was a p-value of <0.10. Multiple linear regression with a stepwise method was performed using the selected significant factors. Statistical significance was set at p<0.05.
A post-hoc power analysis was performed to calculate the sample power of the valid equations by adopting an α error of 5% for a sample size of 39 patients. The sample power ranged from 0.86 to 0.97 for the two equations used in the current study, which was deemed acceptable.
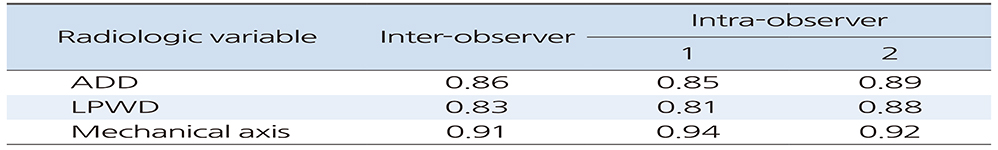
Cohen’s kappa (κ) values were calculated to assess inter- and intra-observer reliabilities.28) The κ values were interpreted as follows: ≤0, no agreement; 0.01-0.20, none to slight; 0.21-0.40, fair; 0.41-0.60, moderate; 0.61-0.80, substantial; and 0.81-1.00, almost perfect agreement.28)
Results
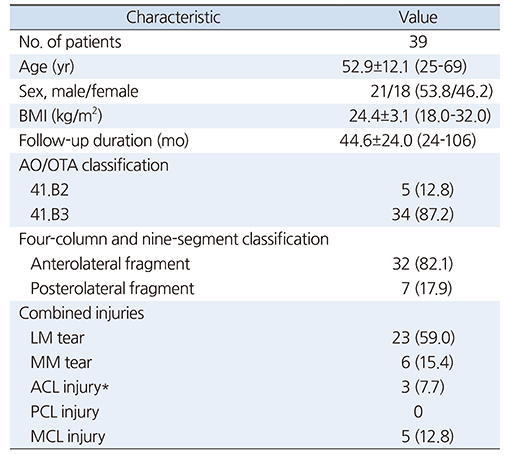
LM tears were the most common combined injuries (n=23, 59.0%) (Table 1). Among LM tears, meniscal repair, partial meniscectomy, and subtotal meniscectomy were performed in 18, four, and one patient, respectively. The amounts of ADD and LPWD seen observed on CT was significantly decreased, shifting from 10.2±5.1 mm (ADD) and 6.0±3.9 mm (LPWD) preoperatively to 1.4±1.9 mm (ADD, p<0.001) and 4.1±2.6 mm (LPWD, p<0.001) postoperatively (Table 2). The reduction rates were 85.5%±19.5% for ADD and 35.5%±30.5% for LPWD. Overall, osteoarthritis progression was noted in five patients (12.8%) based on the Ahlbäck scale. Clinically, the Tegner activity scale did not differ between the preoperative and postoperative values. All patients had bone union within 6 months postoperatively, but one patient (2.6%) underwent realignment surgery 5 years postoperatively due to valgus deformity with lateral compartment osteoarthritis.
Table 1
Demographic Characteristics
Table 2
Radiological and Clinical Results
The mean mechanical and Δmechanical axes axis of the operated knees was –0.2°±3.6° and the mean was 2.5°±3.4°. Valgus malalignment was observed in 10 patients (25.6%), and valgus deviation was observed in five patients (12.8%) (Table 2). The degree of osteoarthritis was significantly more severe in the valgus deformity groups based on the Rasmussen radiologic score (p<0.001). Furthermore, osteoarthritis progression according to the Ahlbäck scale was significantly higher in the valgus deformity groups (valgus malalignment group: 50.0% vs 6.9%, p=0.007; valgus deviation group: 60.0% vs 11.8%, p=0.032) compared to that in the non-valgus deformity group (Table 3).
Table 3
Comparison of Clinical Outcomes Based on Valgus Deformity
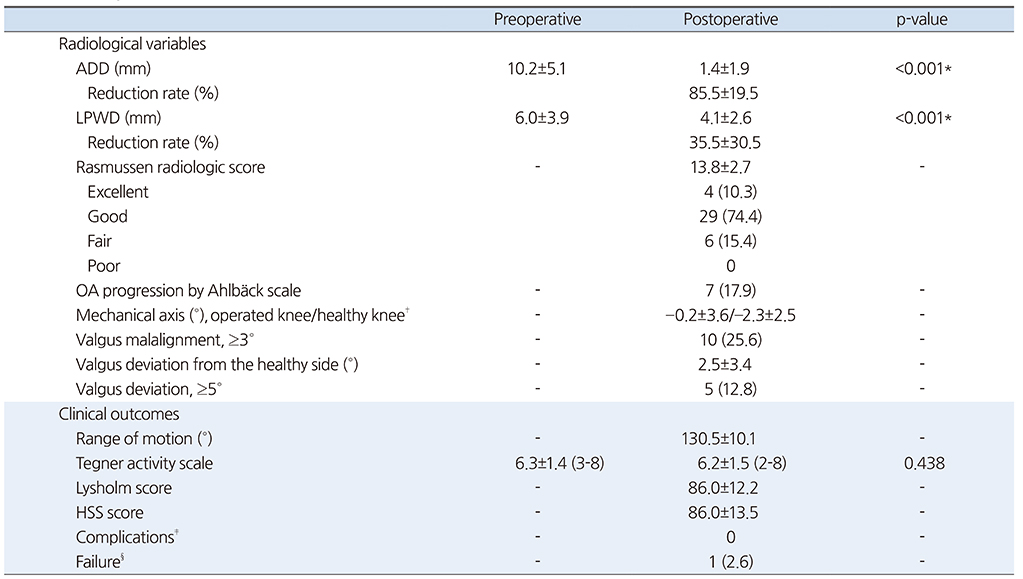
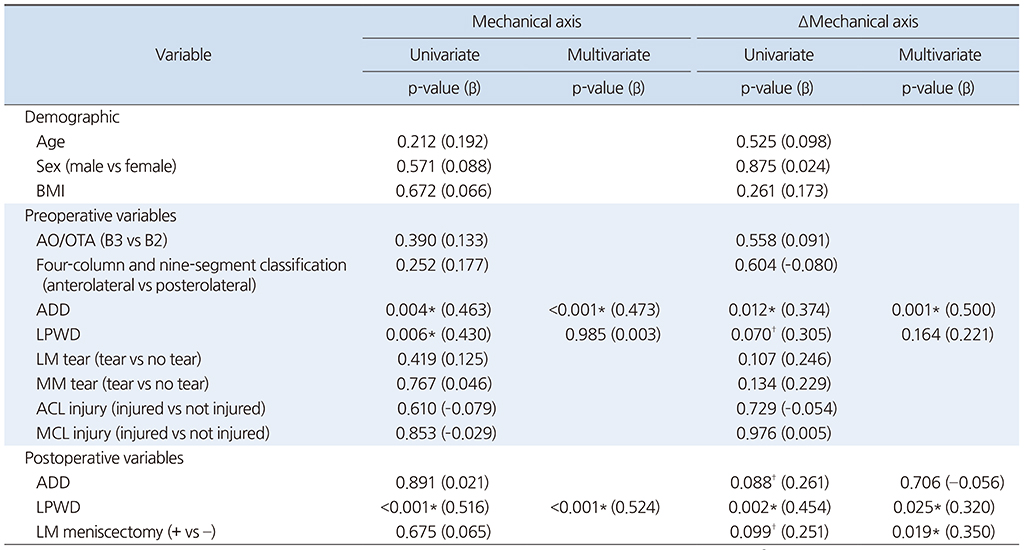
According to multivariate regression analysis, preoperative ADD (β=0.473; p<0.001) and postoperative LPWD (β=0.524; p<0.001) were significantly associated with postoperative mechanical axis (Table 4). In addition, preoperative ADD (β=0.500; p=0.001), postoperative LPWD (β=0.320; p=0.025), and lateral meniscectomized status (β=0.350; p=0.019) were significantly associated with the postoperative Δmechanical axis (Fig. 3).
Fig. 3
Right knee of a 27-year-old male patient with a lateral tibial plateau fracture showing joint depression and lateral plateau widening on a preoperative anteroposterior radiograph (A) and computed tomography (CT) (C). After arthroscopic reduction with allogenic cancellous bone graft and internal fixation with a locked plate, postoperative anteroposterior radiographs (B) and CT (D) show an acceptable reduction of joint depression, but some lateral plateau widening remains. (E) A full-leg standing anteroposterior radiograph shows a valgus of nine degrees on the right knee and a varus of one degree on the left knee at postoperative three years, as evaluated by mechanical axis using hip-knee-ankle angle.
Table 4
Factors for the Progression of Valgus Deformity after ARIF in AO/OTA 41.B2 or 41.B3 Fractures
Meanwhile, the inter- and intra-observer reliabilities for the radiological variables showed substantial to almost perfect agreement, with κ values ranging from 0.81 to 0.94 (Appendix).
Discussion
The results of the current study demonstrated that preoperative ADD, postoperative LPWD, and LM meniscectomized status were significantly associated with valgus deformity after ARIF in lateral joint depression tibial plateau fractures. Although comparable clinical outcomes were observed in patients regardless of valgus deformity, osteoarthritis progression was significantly more prevalent in patients with valgus deformity than in those without valgus deformity, with a mean follow-up of 44.6 months.
Although most previous studies reported that postoperative valgus deformity did not significantly affect postoperative clinical outcomes, relevant literature contains conflicting data regarding the influence of valgus deformity on osteoarthritis progression in patients with lateral joint depression tibial plateau fractures after ORIF.9,10,29) Meanwhile, no studies have assessed this topic after ARIF; thus, the current study was performed to focus on valgus deformity after ARIF. The results of the current study showed comparable postoperative clinical outcomes in patients with and without valgus deformity, whereas the osteoarthritis progression was significantly higher in the valgus deformity group (valgus malalignment group, 50.0%; valgus deviation group, 60.0%) than in the non-valgus deformity group after ARIF (non-valgus malalignment group: 6.9%; non-valgus deviation group: 11.8%). Although the incidence of osteoarthritic progression ranged from 3.2% to 63.0% in a recent systematic review,7) it was highly prevalent in the valgus deformity group based on subgroup analyses in the present study. Valgus deformity theoretically leads to osteoarthritic progression because it changes the load distribution of the joint and increases the maximal contact pressure of the lateral compartment.8,30) Despite this, several previous studies have maintained that postoperative valgus deformity in tibial plateau fractures would not affect osteoarthritic progression because there is a high prevalence of underlying advanced osteoarthritis with varus malalignment in elderly patients, of which the medial compartment would be unloaded by postoperative valgus progression, similar to high tibial osteotomy.10,31) To avoid this confounding factor, the current study excluded patients with underlying osteoarthritis with K-L grades 3 or 4. The results of the current study suggest that surgeons should take care to avoid valgus deformity in lateral joint-depression tibial plateau fracture after ARIF and should recognize preoperative and postoperative factors affecting the valgus deformity to prevent subsequent osteoarthritic aggravation.
In the current study, preoperative ADD and postoperative LPWD were significantly associated with valgus deformity in lateral joint depression tibial plateau fractures after ARIF. In the multivariate regression analysis, preoperative ADD was a significant factor for valgus deformity, which seems plausible as the amount of ADD may reflect the amount of energy absorbed at the time of injury resulting from valgus force.11,17,31) Unexpectedly, postoperative ADD was not a significant factor for valgus deformity after ARIF, although restoration of intra-articular step-off has been well emphasized for the surgical treatment of lateral joint depression tibial plateau fractures to prevent the valgus deformity, osteoarthritic aggravation, and functional impairment.7,8,9,29) Because the primary goal of ARIF is to minimize intra-articular step-off under direct visualization, it would be difficult to show a statistical difference in postoperative ADD values after ARIF in the multivariate regression analysis of valgus deformity. In the present study, the mean postoperative ADD was 1.4±1.9 mm and the mean reduction rate of ADD was 85.5%±19.5%, which were deemed acceptable and successful. Meanwhile, postoperative LPWD was a significant factor for valgus deformity after ARIF. Although several studies reported that LPWD was associated with LM tear,7,11) there is little evidence reporting that postoperative LPWD was significantly associated with valgus deformity in tibial plateau fractures after surgical treatment. It may be cautiously postulated that surgeons tend to concentrate on restoring intra-articular step-off by elevating the depressed fragment and filling the bone graft at the defect area during ARIF. They may tend to overlook the restoration of LPWD by compressing both tibial condyles with a reduction clamp. In particular, it would be more difficult to reduce LPWD if the bone graft was performed before compressing both tibial condyles. In our series, the mean postoperative LPWD was 4.1±2.6 mm and the mean reduction rate was 35.5%±30.5%, which seemed a somewhat insufficient reduction despite the sensitive evaluation of postoperative CT. Accordingly, widening of the lateral tibial plateau may lead to joint incongruency and provide more space for the lateral femoral condyle to glide on the coronal plane, resulting in valgus deformity as medial laxity progresses. Moreover, the hidden injury of medial collateral ligament might lead to progressive medial laxity resulting in valgus deformity in addition to the postoperative widening of lateral tibial plateau. The results of the current study indicate the need for the restoration of LPWD and ADD for the treatment of lateral joint depression tibial plateau fractures, especially after ARIF. A recent study supported the result of current study that postoperative ADD more than 4 mm and postoperative LPWD more than 5 mm were significant risk factors for conversion to total knee arthroplasty because of joint incongruency leading to progressive postoperative arthritis.32)
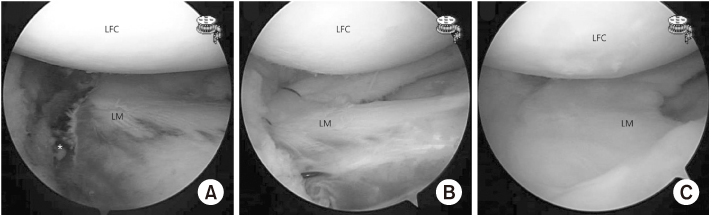
Previous studies reported that LM tears were the most common concomitant injury in lateral joint depression tibial plateau fractures.4,7,11,12) As the injury mechanism of valgus and axial compressive force and fracture patterns, the LM is occasionally entrapped between lateral femoral and tibial condyles. Furthermore, when the load propagates, the entrapped LM might be pulled medially and inferiorly, leading to longitudinal tears.7,11) In the current study, LM tear was observed in 59.0% of the study cohort, most commonly longitudinal tears. As neglected LM tear and LM meniscectomized status lead to the progression of valgus deformity and subsequent osteoarthritis, great efforts have recently been made to detect LM tears preoperatively and to preserve LM as much as possible.4,11,12,17,18) Consistent with previous studies,8,30) the current study found that LM meniscectomy was significantly associated with valgus deformity, especially valgus deviation (Δmechanical axis). Thus, LM tears should be thoroughly assessed in lateral joint depression tibial plateau fractures and it is important to preserve LM as much as possible during ARIF (Fig. 4).
Fig. 4
(A) Right knee of a 49-year-old male patient with lateral joint depression tibial plateau fracture showing concomitant lateral meniscus (LM) longitudinal tear (asterisk) at the menisco-capsular junction from the anterior horn to mid-body. (B) After the reduction of the articular surface of the joint depression, the LM was repaired with proper tension using a modified outside-in technique. (C) Second-look arthroscopic finding at the time of plate removal showing the well-healed LM repair at one year postoperatively. LFC: lateral femoral condyle
The current study had several limitations. First, it was a retrospective case series with a relatively small sample size. Moreover, the small sample size of meniscectomized compared with meniscal repair and progression of osteoarthritis might be a potential selection bias for the result. However, it seemed inevitable to perform a retrospective study to identify the factors for valgus deformity after ARIF. Furthermore, the posthoc power calculation for the primary aim of the current study was >80%, which seemed acceptable power for the sample size. Second, the mean follow-up period of 44.6 months was relatively short, and the range of follow-up period was wide. Although a recent study demonstrated that a minimum of 2 years was sufficient to detect osteoarthritic progression,9) longer and homogeneous follow-up with a larger sample size is required to confirm our findings. Third, two surgeons performed ARIF for tibial plateau fractures with AO/OTA 41.B2 or B3 which might be potential bias although two surgeons performed ARIF with a homogeneous philosophy and technique. Fourth, the patients in the study cohort were limited to tibial plateau fractures with AO/OTA 41.B2 or B3 after ARIF; thus, the results cannot be generally applied to tibial plateau fractures overall. Nevertheless, the results of the current study provide useful information on why valgus progression is occasionally observed in AO/OTA 41.B2 or B3 fractures even after accurate reduction of intra-articular step-off and LM repair during ARIF. Lastly, a precise evaluation of medial laxity of the knee is needed to address factors affecting postoperative valgus deformity in such fractures, although the current study evaluated patients with occasional preoperative magnetic resonance imaging and immediate postoperative physical examination for medial collateral ligament injury. Despite several limitations, the current study had strength to provide valuable information to surgeon during ARIF for tibial plateau fractures with AO/OTA 41.B2 or B3 to preserve joint congruence including both articular depression and plateau widening as well as LM, which might prevent valgus malalignment and lateral compartment osteoarthritis.
Conclusion
Osteoarthritis progression was highly prevalent in patients with postoperative valgus deformity. Thus, the restoration of lateral plateau widening as well as articular depression and preservation of the meniscus are necessary to prevent valgus deformity after ARIF in lateral joint-depression tibial plateau fractures.
Financial support:None.
Conflict of interests:None.
Appendix
ICC of Inter-Observer and Intra-Observer Reliabilities for a Radiologic Evaluation
References
-
Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968;Suppl 277:7–72.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS



 Cite
Cite

