Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(2); 2020 > Article
- Original Article Three-Dimensional Analysis of the Morphological Features in the Femur of Atypical Fracture and Practical Implications of Intramedullary Nailing
- Yong Uk Kwon, Kyung-Jae Lee, Joo Young Choi, Gu-Hee Jung
-
Journal of Musculoskeletal Trauma 2020;33(2):87-95.
DOI: https://doi.org/10.12671/jkfs.2020.33.2.87
Published online: April 30, 2020
2Department of Orthopaedic Surgery, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
3Institute of Health Sciences (Medical ICT Convergence Research Center), Gyeongsang National University College of Medicine, Jinju, Korea
4Department of Orthopaedic Surgery, Gyeongsang National University Changwon Hospital, Gyeongsang National University College of Medicine, Changwon, Korea
- 453 Views
- 5 Download
- 0 Crossref
- 0 Scopus
Abstract
Purpose
This study analyzed the morphological features of the contralateral femur without an atypical fracture by constructing a three-dimensional model with an actual size medullary canal.
Materials and Methods
Lateral and anterior bowing of the shaft were measured for 21 models, and the shape of the medullary canal was analyzed. To eliminate the projection error, the anteroposterior (AP) femur was rotated internally to the extent that the centerline of the head and neck, which is the ideal position of cephalomedullary nail screw, was neutral, and the lateral femur matched the medial and lateral condyle exactly.
Results
The lateral bowing and anterior bowing was an average of 5.5° (range, 2.8°-10.7°; standard deviation [SD], 2.4°) and 13.1° (range, 6.2°-21.4°; SD, 3.2°), respectively. In the area where lateral bowing increased, the lateral cortex became thicker, and the medullary canal was straightened. On the lateral femur, the anterior angle was increased significantly, and the diameter of curvature averaged 1,370.2 mm (range, 896-1,996 mm; SD, 249.5 mm).
Conclusion
Even if the anterolateral bowing increases in the atypical femur, the medullary canal tends to be straightened in the AP direction. So, it might be considered as a reference to the modification of an intramedullary nail to increase the conformity.
Published online Apr 28, 2020.
https://doi.org/10.12671/jkfs.2020.33.2.87
Three-Dimensional Analysis of the Morphological Features in the Femur of Atypical Fracture and Practical Implications of Intramedullary Nailing
 , M.D.,
Kyung-Jae Lee
, M.D.,
Kyung-Jae Lee , M.D., Ph.D.,*
Joo Young Choi
, M.D., Ph.D.,*
Joo Young Choi , B.D.,†
and Gu-Hee Jung
, B.D.,†
and Gu-Hee Jung , M.D., Ph.D.†,‡
, M.D., Ph.D.†,‡
Abstract
Purpose
This study analyzed the morphological features of the contralateral femur without an atypical fracture by constructing a three-dimensional model with an actual size medullary canal.
Materials and Methods
Lateral and anterior bowing of the shaft were measured for 21 models, and the shape of the medullary canal was analyzed. To eliminate the projection error, the anteroposterior (AP) femur was rotated internally to the extent that the centerline of the head and neck, which is the ideal position of cephalomedullary nail screw, was neutral, and the lateral femur matched the medial and lateral condyle exactly.
Results
The lateral bowing and anterior bowing was an average of 5.5° (range, 2.8°–10.7°; standard deviation [SD], 2.4°) and 13.1° (range, 6.2°–21.4°; SD, 3.2°), respectively. In the area where lateral bowing increased, the lateral cortex became thicker, and the medullary canal was straightened. On the lateral femur, the anterior angle was increased significantly, and the diameter of curvature averaged 1,370.2 mm (range, 896–1,996 mm; SD, 249.5 mm).
Conclusion
Even if the anterolateral bowing increases in the atypical femur, the medullary canal tends to be straightened in the AP direction. So, it might be considered as a reference to the modification of an intramedullary nail to increase the conformity.
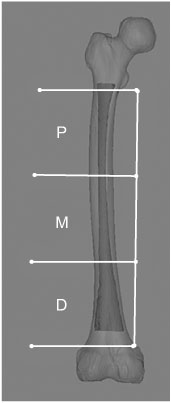
Fig. 1
The fracture location was classified into three parts (i.e., proximal [P], middle [M], and distal [D]) to trisect the femoral diaphysis from just distal to the lesser trochanter to just proximal to the supracondylar flare.
Fig. 2
To analyze the morphological features, (A) a line through the tip of the great trochanter and a condylar center (tip line) was made using a three-dimensional method and (B) compared with the young adult femur. (C) Lines of 60 mm perpendicular to the proximal and distal shaft were drawn and verified in the anteroposterior and lateral projection.
Fig. 3
The proximal (a) and distal angles (b) between the tip line and shaft lines were measured in the anteroposterior and lateral projection (c, d) and then, minus the sum of the proximal and distal angles at 180°, which was defined as the anterior bowing and lateral bowing.
Fig. 4
The diameter of curvature of the posterior surface of the medullary canal was measured to assess the anterior bowing.
Fig. 5
Despite the increased anterolateral bowing, (A) the medullary canal of the atypical femur tended to be straightened on the anteroposterior projection, and the anterior bowing was increased markedly. (B) By comparison, the femur of a 21-year-old adult male showed medial bowing of 2.9° in the femoral shaft.
Fig. 6
According to the degree of femur rotation, the relationship between the tip line and the center of the medullary canal was different. Thus, the projection error might be preoperatively assessed in the preoperative planning.
Fig. 7
Because the atypical femur showed increased anterolateral bowing compared with a normal young adult (A, B), the conventional intramedullary nailing of a 70-year-old female showed several problems, such as iatrogenic fracture, straightening of the femur, and lower limb malalignment (C, D).
Fig. 8
Computation simulations of intramedullary nailing, including the conventional technique (A), rotational technique (B), and cannulated femoral nail (CFN) technique (C), were performed. The results demonstrated that the CFN technique had the best conformity with the medullary canal.
Financial support:None.
Conflict of interests:None.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS








 Cite
Cite

