Search
- Page Path
- HOME > Search
Original Articles
- Epidemiological changes and surgical trends of distal radius fractures in adults over 50 years during the COVID-19 pandemic in Korea: a nationwide repeated cross-sectional study
- Han-Kook Yoon, So Ra Yoon, Kee-Bum Hong, Youngsu Jung, SeongJu Choi, Jun-Ku Lee
- J Musculoskelet Trauma 2026;39(1):12-19. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00297
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
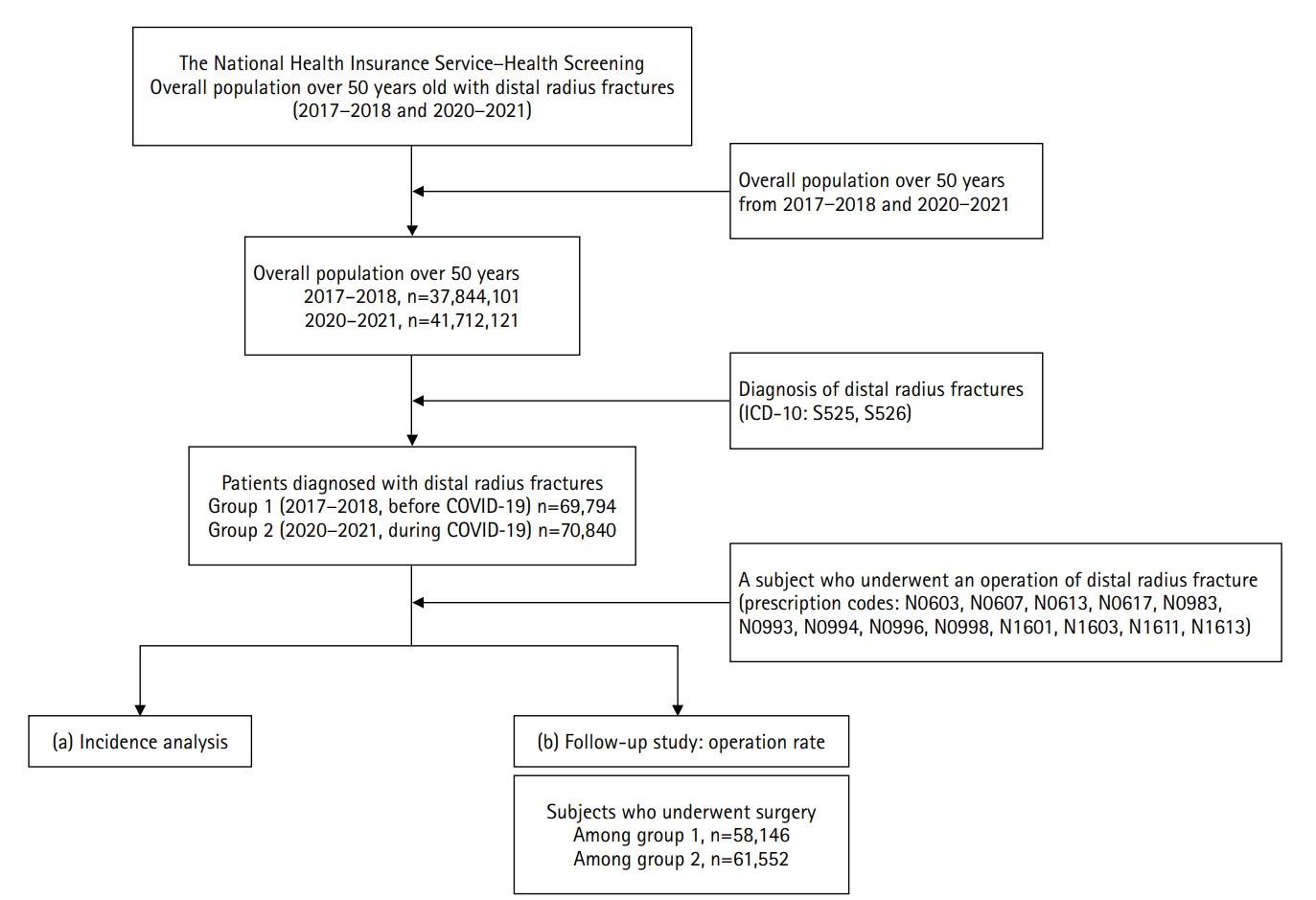
The COVID-19 pandemic is likely to have affected bone health in older adults in Korea. This study aimed to analyze changes in the epidemiology and management of distal radius fractures (DRFs) in older adults before and during the COVID-19 pandemic.
Methods
Patients with DRF aged over 50 years in 2017, 2018, 2020, and 2021 were included in this study. Patients were classified into a group with DRF occurring between 2017 and 2018 (before COVID-19) and a group with DRF occurring between 2020 and 2021 (during COVID-19). We calculated the incidence rates of DRF and compared them between the two groups. We also analyzed and compared demographic data (age, sex, income, residence) and the operation rate for DRF between the two groups. Patient selection and treatment were based on International Classification of Diseases, 10th revision codes.
Results
A total of 140,634 patients with DRF (before COVID-19, 69,794; during COVID-19, 70,840) were included. The incidence of DRF before COVID-19 (184.4/100,000 person-years) was higher than during COVID-19 (169.8/100,000 person-years). The operation rate was higher during COVID-19 (86.9%) than before COVID-19 (83.3%).
Conclusion
During the COVID-19 pandemic, the incidence of DRF decreased in South Korea. However, the rate of surgical treatment increased and exceeded the global surgical rate. Level of evidence: III.
- 82 View
- 3 Download

- Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
- Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
- J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00276
-
 Abstract
Abstract
 PDF
PDF - Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
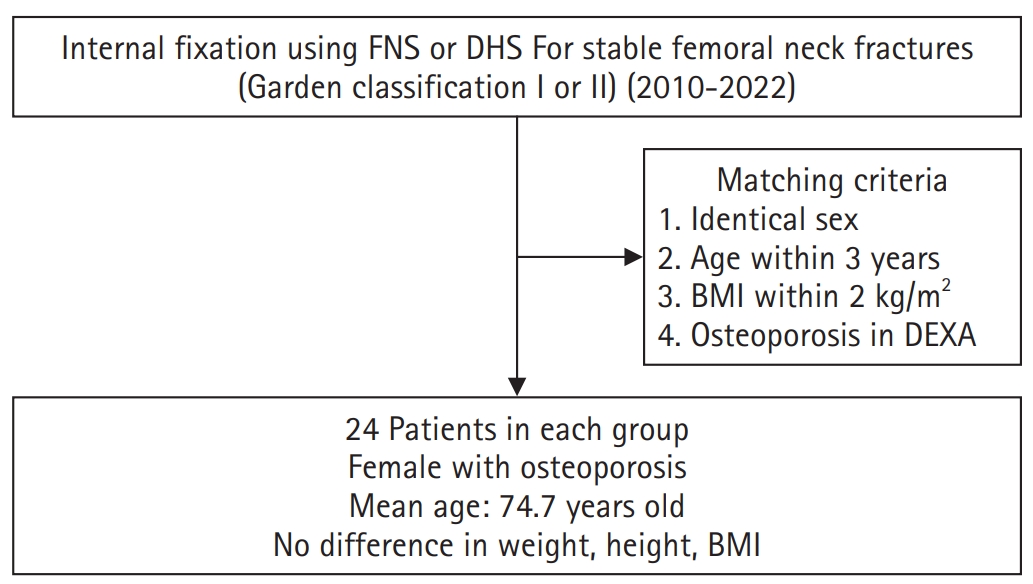
Methods
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results. Level of evidence: IV.
- 1,496 View
- 20 Download

- Correlation of bone mineral density with ankle fractures in older adults in Korea: a retrospective cohort study
- Seung Hyun Lee, Chae Hun Lee, Seo Jin Park, Jun Young Lee
- J Musculoskelet Trauma 2025;38(4):186-192. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00150
-
 Abstract
Abstract
 PDF
PDF - Background
Bone mineral density (BMD) is well-documented in relation to fractures of the spine, hip, distal radius, and proximal humerus; however, its correlations with other fracture types are less established. This study aimed to analyze BMD and associated risk factors in older adults (≥65 years of age) with osteoporotic ankle fractures. These fractures involve low-energy trauma, resulting from falls from a standing height or lower, and occur from impacts which typically do not cause fractures in individuals with normal bone.
Methods
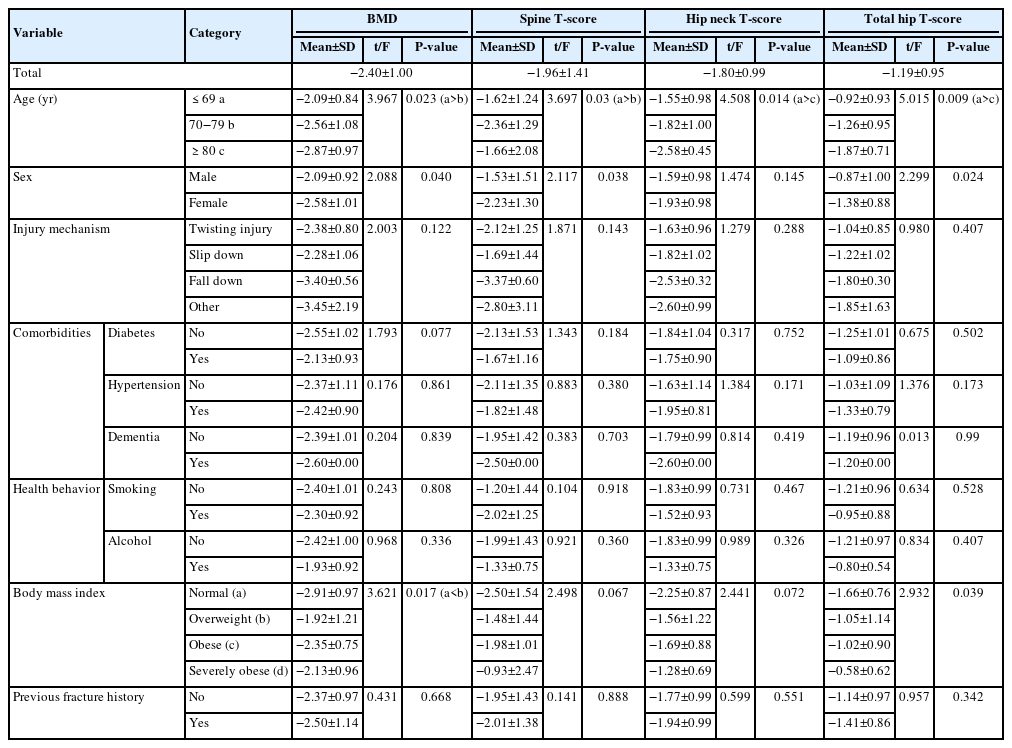
This retrospective study analyzed data from 1,411 patients diagnosed with ankle fractures admitted to Chosun University Hospital between February 2012 and April 2023. After applying inclusion criteria (age ≥65 years; low energy ankle fracture) and exclusion criteria (high energy trauma, open/multiple fractures, missing dual X-ray absorptiometry [DXA]), 73 of 1,411 patients were analyzed. Lumbar spine, femoral neck, and total hip T scores were obtained with a Horizon Wi DXA scanner, and associations with age, sex, mechanism of injury, comorbidities, smoking status, alcohol consumption, body mass index (BMI), and history of fractures were tested by ANOVA with Scheffe post hoc and Fisher exact tests.
Results
Lower BMD correlated significantly with older age, female sex, and lower BMI (P<0.05) in older adults with ankle fractures. No significant associations were observed for comorbidities (diabetes, hypertension, dementia), smoking, alcohol consumption, injury mechanism, or prior fractures.
Conclusion
These results indicate that older age, female, and lower BMI are linked to reduced BMD in ankle fracture patients over 65 years of age. Focused osteoporosis screening and management may therefore be most beneficial for older, low BMI women presenting with ankle fractures. Level of evidence: IV.
- 832 View
- 2,147,483,670 Download

- Risk factors for ankle fractures in older adults based on clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities in Korea: a retrospective case-control study
- Myeong Jun Song, Se Woong Jang, Jun Young Lee, Seojin Park
- J Musculoskelet Trauma 2025;38(4):193-202. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00143
-
 Abstract
Abstract
 PDF
PDF - Background
Ankle fractures are common in older adults; however, their relationship with osteoporotic fractures remains unclear. This study aimed to evaluate potential risk factors for ankle fractures in older adults by analyzing individual clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities.
Methods
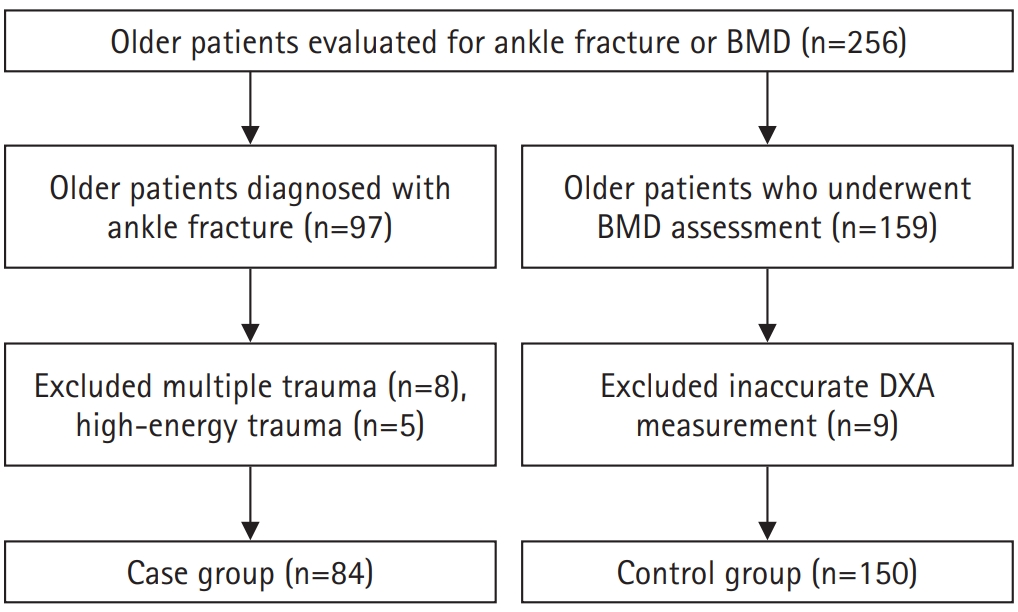
We conducted a retrospective case-control study including 84 patients aged ≥65 years with ankle fractures and 150 controls who underwent bone mineral density (BMD) testing without prior ankle fractures. The variables analyzed included age, sex, body mass index, smoking, alcohol consumption, prior fracture history, and comorbidities such as hypertension, diabetes mellitus, and dementia. BMD was measured at the spine, total hip, and femoral neck.
Results
Univariate analysis showed that alcohol consumption, diabetes mellitus, and total hip T-score categories were significantly associated with ankle fractures. In binary logistic regression, alcohol consumption remained significantly associated with higher ankle fracture risk (odds ratio [OR], 5.302; 95% confidence interval [CI], 1.778–15.811; P=0.003), and both osteopenia and osteoporosis at the total hip were also associated with increased risk (OR, 3.260, P=0.049; OR, 3.561, P=0.031, respectively). Diabetes mellitus did not reach statistical significance in the adjusted model (P=0.074). Model fit was adequate (Hosmer-Lemeshow P=0.377), and post hoc power analysis confirmed sufficient sample size.
Conclusions
These findings suggest that lower total hip BMD and alcohol-related factors may be associated with ankle fracture risk in older adults. The FRAX score itself was not calculated; instead, this study focused on analyzing selected clinical components. Limitations include the retrospective design, lack of fall and medication data, and cross-sectional BMD assessment. Level of evidence: III.
- 1,049 View
- 21 Download

Review Articles
- Current concepts in the management of phalangeal fractures in the hand
- Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):109-123. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00136
-
 Abstract
Abstract
 PDF
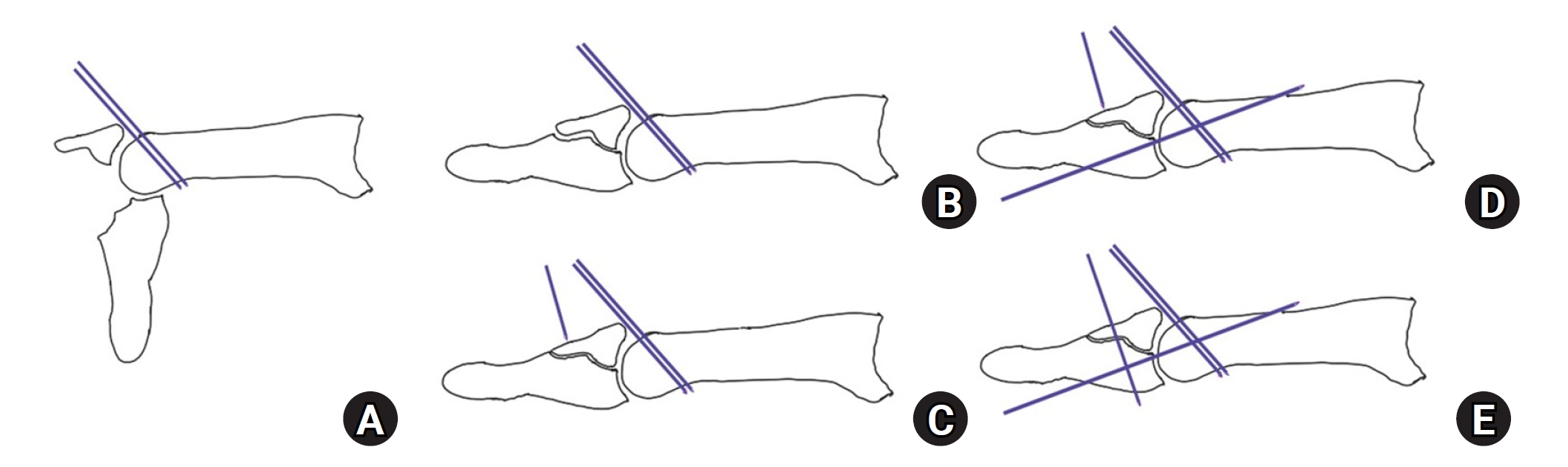
PDF - This review focuses on the treatment of hand fractures based on the anatomical location of the fractured phalanx, excluding the thumb, and examines recent studies on the topic. The main points are as follows: in most cases of hand fractures, conservative treatment should be prioritized over surgical intervention. The three key factors in determining whether surgical treatment is necessary are (1) whether the fracture is intraarticular, (2) the stability of the fracture itself, and (3) the extent of damage to surrounding soft tissues. The primary surgical treatment is closed reduction and Kirschner-wire fixation. The risk of rotational deformity increases with fractures closer to the proximal region. Intra- articular fractures may lead to subsequent stiffness and arthritis; thus, computed tomography is recommended to assess the fracture pattern. Anatomic reduction of intraarticular fragments is required, along with correction of the inherent joint instability. No surgical method has proven to be superior; it is advantageous for the surgeon to choose a surgical approach they are familiar with and confident in, based on the specific fracture and patient factors. Complications in hand fractures are various; the most frequent is stiffness, and nonunion is uncommon. Early joint motion is crucial in minimizing the risk of stiffness.
- 15,426 View
- 322 Download

- Current Concepts in the Articular Cartilage Repair
- Eui Dong Yeo, Whi Je Cho, Young Koo Lee
- J Korean Fract Soc 2020;33(3):164-170. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.164
-
 Abstract
Abstract
 PDF
PDF - Articular cartilage defects are common in orthopedic practice. Most clinical and research efforts focus on restoring the damaged cartilage in connection with osteoarthritis or trauma. This article explains the current clinical approaches for repairing cartilage, as well as the research approaches and those under translation into clinical practice. Tissue engineering techniques are being employed with aims of repopulating a cartilage defect with hyaline cartilage containing living chondrocytes with hopes of improving the clinical outcomes. Cartilage tissue engineering involves the cell source, biomaterial and membranes, and growth stimulators. Tissue engineering is being applied to clinical medicine by autologous chondrocyte implantation or similar techniques. While basic science has refined orthopedic treatment of chondral lesions, available evidence does not conclude the superiority of tissue engineering methods over other techniques in improving the clinical symptoms or restoring the native joint mechanics.
- 729 View
- 2 Download

Case Report
- Rare Experience of Bilateral Femoral Neck and Shaft Fractures - A Case Report -
- DaeHyun Choe, Jae-Ho Lee, Ki-Chul Park
- J Korean Fract Soc 2020;33(3):154-158. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.154
-
 Abstract
Abstract
 PDF
PDF - Ipsilateral fractures of the femoral neck and shaft are relatively common injuries and accompany 2% to 9% of all femoral shaft fractures. On the other hand, it is extremely rare for these injuries to occur bilaterally. This paper reports the authors’ experience of a case with bilateral femoral neck and shaft fractures. The patient sustained multiple injuries, including liver laceration with hemoperitoneum, bilateral open fractures of the tibia, and bilateral femoral neck, and shaft fractures caused by a high-speed motor vehicle accident. Under the circumstances, damage-control orthopedic principles were applied, and external fixators were initially placed. After the patient’s general condition showed improvement, both femurs were fixed with a reconstruction nail. Fracture healing was achieved without complications, such as avascular necrosis of the femoral head. Despite the rare occurrence, this paper describes this case because these injuries must be managed with meticulous attention.
- 494 View
- 8 Download

Original Articles
- Does the Use of a Silicone Ring Tourniquet Help Reduce Bleeding in the Minimally Invasive Internal Fixation with Locking Plate for Distal Femoral Fractures?
- Ki-Bong Park, Hong-Ki Jin, Il-Yeong Hwang, Sung-Who Chang, Sung-Cheon Na
- J Korean Fract Soc 2020;33(3):148-153. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.148
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the usefulness of a silicone ring tourniquet by analyzing the changes in the perioperative hemoglobin (Hb) levels or amount of perioperative bleeding compared to those of a pneumatic tourniquet or no usage during minimally invasive plate fixation for distal femoral fractures.
Materials and Methods
From January 2017 to December 2019, 30 patients who underwent minimally invasive plate fixation using a locking compression plate for distal femoral fractures were evaluated and classified as a silicone ring tourniquet (Group 1), a pneumatic tourniquet (Group 2), and no usage (Group 3). The variables for analysis were age, sex, preoperative Hb (preHb), postoperative 72-hour Hb (postHb), differences between preHb and postHb (preHb-postHb), amount of intraoperative and overall transfusion, estimated unit of transfusion corrected by preHb-postHb and total transfusion (Hb-lost), amount of intraoperative and postoperative and total bleeding. One-way ANOVA was used to identify the differences between the groups.
Results
The age, sex, operation time, preHb, preHb-postHb, amount of intraoperative and overall transfusion and Hb-lost were similar in the two groups. The amount of intraoperative bleeding was significantly lower in Group 1 than Group 3 (p=0.004), but there was no difference in the amount of postoperative and total bleeding between the two groups.
Conclusion
The use of a silicone ring tourniquet in the minimally invasive plate fixation for distal femoral fractures decreased the amount of intraoperative bleeding compared to no use of a tourniquet. -
Citations
Citations to this article as recorded by- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
Tae sung Lee, Kwan Kyu Park, Byung Woo Cho, Woo-Suk Lee, Hyuck Min Kwon
BMC Musculoskeletal Disorders.2023;[Epub] CrossRef
- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
- 909 View
- 6 Download
- 1 Crossref

- Comparison of a Novel Box-Frame External Fixator and Conventional Delta-Frame External Fixator in the Staged Treatment of Distal Tibia Fractures
- Yong-Cheol Yoon, MinKyu Shin, Chang-Wug Oh, Jong-Keon Oh
- J Korean Fract Soc 2020;33(3):125-133. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.125
-
 Abstract
Abstract
 PDF
PDF - Purpose
Distal tibia fractures with severe soft-tissue edema or intra-articular fractures are treated by staged operations using external fixators. Definitive surgery that maintains ligamentotaxis has been difficult using existing fixators. This study introduced a novel ‘box-frame’ external fixator and evaluated its clinical usefulness.
Materials and Methods
This study included 45 patients (32 males, 13 females) diagnosed with distal tibia fractures who underwent staged operations between March 2012 and March 2016, with a follow-up of at least one year. The patients were divided into two groups. In one group, fixation was performed with a box-frame external fixator (Group A). In the other group, fixation was performed with a delta-frame external fixator (Group B). The following outcomes were evaluated: the time until definitive surgery, operative time of the definitive surgery, radiation exposure time, bone union, time to achieve bone union, postsurgical complications, American Orthopaedic Foot & Ankle Society anklehindfoot score, and ankle range of motion.
Results
Compared to the delta-frame, the box-frame showed a statistically significant reduction in the mean radiation-exposure time and operative time during the definitive surgery by 58 seconds and 25 minutes, respectively. The differences in the time until definitive surgery, bone union, time to achieve bone union, postsurgical complications, and functional scores were not significant.
Conclusion
The box-frame external fixator can be a useful treatment method in the staged surgery of distal tibia fractures. -
Citations
Citations to this article as recorded by- Temporary Circular External Fixation for Spanning the Traumatized Ankle Joint
Nando Ferreira, Niel Bruwer, Adriaan Jansen van Rensburg, Ernest Muserere, Shao-Ting Jerry Tsang
JBJS Essential Surgical Techniques.2024;[Epub] CrossRef - Temporary circular external fixation for spanning the traumatised ankle joint: A cohort comparison study
William D. Harrison, Franklin Fortuin, Matthieu Durand-Hill, Etienne Joubert, Nando Ferreira
Injury.2022; 53(10): 3525. CrossRef
- Temporary Circular External Fixation for Spanning the Traumatized Ankle Joint
- 2,120 View
- 21 Download
- 2 Crossref

Case Report
- Major Limb Replantation of Lower Leg Amputation with Ipsilateral Distal Femoral Comminuted Fracture in Old Age: A Case Report
- Tae Young Ahn, Seung Joon Rhee, Sang Ho Kwak, Hyo Seok Jang, Sang Hyun Lee
- J Korean Fract Soc 2019;32(4):227-231. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.227
-
 Abstract
Abstract
 PDF
PDF - The development of microsurgical techniques has also increased the success rate of replantation surgery. This paper reports the results of limb replantation performed on a lower extremity amputation that was associated with crush amputation and an ipsilateral comminuted fracture in and elderly patient. A 68-year-old female presented with a right distal tibia amputation due to a traffic accident. At that time, with a comminuted fracture in the distal femoral condyle, simple wound repair was recommended, but the caregivers strongly wanted replantation. Three years after surgery, normal walking was possible without a cane and the patient was satisfied with the function and aesthetics. What used to be contraindicated in limb replantation in the past are now indications due to the development of microsurgical techniques, surgical experience, and postoperative rehabilitation treatment. If the patient is willing to be treated, good results in contraindications can be obtained.
- 674 View
- 4 Download

Original Articles
- Prediction of Concomitant Lateral Meniscus Injury with a Tibia Plateau Fracture Based on Computed Tomography Assessment
- Wonchul Choi, Yunseong Choi, Go Tak Kim
- J Korean Fract Soc 2018;31(4):132-138. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.132
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study examined whether any fracture pattern shown in computed tomography (CT) scan is associated with the presence of lateral meniscus (LM) injury in a tibia plateau fracture.
MATERIALS AND METHODS
Fifty-three tibia plateau fractures with both preoperative CT and magnetic resonance imagings (MRI) available were reviewed. The patient demographics, including age, sex, body mass index, and energy level of injury were recorded. The fracture type according to the Schatzker classification, patterns including the lateral plateau depression (LPD), lateral plateau widening (LPW), fracture fragment location, and the number of columns involved were assessed from the CT scans. The presence of a LM injury was determined from the MRI. The differences in the factors between the patients with (Group 1) and without (Group 2) LM injuries were compared and the correlation between the factors and the presence of LM injury was analyzed.
RESULTS
The LM was injured in 23 cases (Group 1, 43.4%) and intact in 30 cases (Group 2, 56.6%). The LPD in Group 1 (average, 8.2 mm; range, 3.0–20.0 mm) and Group 2 (average, 3.8 mm; range, 1.4–12.1 mm) was significantly different (p < 0.001). The difference in LPW of Group 1 (average, 6.9 mm; range, 1.2–15.3 mm) and Group 2 (average, 4.8 mm; range, 1.4–9.4 mm) was not significant (p=0.097). The other fracture patterns or demographics were similar between in the two groups. Regression analysis revealed that an increased LPD (p=0.003, odds ratio [OR]=2.12) and LPW (p=0.048, OR=1.23) were significantly related to the presence of a LM tear.
CONCLUSION
LPD and LPW measured from the CT scans were associated with an increased risk of concomitant LM injury in tibia plateau fractures. If such fracture patterns exist, concomitant LM injury should be considered and an MRI may be beneficial for an accurate diagnosis and effective treatment. -
Citations
Citations to this article as recorded by- The value of magnetic resonance imaging in the preoperative diagnosis of tibial plateau fractures: a systematic literature review
Gregoire Thürig, Alexander Korthaus, Karl-Heinz Frosch, Matthias Krause
European Journal of Trauma and Emergency Surgery.2023; 49(2): 661. CrossRef
- The value of magnetic resonance imaging in the preoperative diagnosis of tibial plateau fractures: a systematic literature review
- 506 View
- 1 Download
- 1 Crossref

- The Determination of Optimal Entry Point for Proximal Femoral Nail Antirotation-II by Fluoroscopic Simulation: A Cadaveric Study
- Jin Hoon Jeong, Gu Hee Jung
- J Korean Fract Soc 2017;30(4):173-179. Published online October 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.4.173
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study seeks to determine the anatomically optimal entry point of proximal femoral nail antirotation-II (PFNA-II®) according to geographic features of Korean cadaveric femoral trochanters for successful reduction of osteoporotic proximal femoral fractures.
MATERIALS AND METHODS
Forty-three adult cadaveric femurs without previous fractures or surgeries were included. Anteroposterior (AP) and lateral images of all femurs and PFNA-II® were taken with an image intensifier. Using the image synthesis process via the image editing program (Adobe Photoshop CS6), the optimal entry point was verified and compared with the tip of the greater trochanter (GT) and the cervicotro-chanteric junction on AP images, as well as the width of the trochanter and the neck on lateral images.
RESULTS
The optimal entry point of PFNA-II® was an average distance of 9.1 mm (range, 7–15 mm) medially from the tip of GT on AP images. The center of the nail was located at an average of 30% (range, 21%–44%) area from the posterior margin of the middle neck, which is an average area of 38% (range, 26%–48%) from the posterior cortex of the trochanter on lateral images. Furthermore, the ideal entry point was at the extended line of the cervico-trochanteric junction.
CONCLUSION
The optimal entry point, which was found to be medial to the tip of the GT and posterior to the center of the middle femoral neck and the trochanter, was at on the extended line of the cervicotrochanteric junction. -
Citations
Citations to this article as recorded by- Clinical Research through Computational Anatomy and Virtual Fixation
Ju Yeong Kim, Dong-Geun Kang, Gu-Hee Jung
Journal of the Korean Orthopaedic Association.2023; 58(4): 299. CrossRef - Does the Entry Point of Proximal Femoral Nail Antirotation Affect the Malalignment of Intertrochanteric Fracture? A Cadaveric Study
Chittawee Jiamton, Nonpawit Nimmankiatkul, Pongsakorn Rungchamrassopa, Wichan Kanchanatawan, Pariyut Chiarapatanakom, Wirat Kongcharoensombat
Journal of Southeast Asian Orthopaedics.2022;[Epub] CrossRef
- Clinical Research through Computational Anatomy and Virtual Fixation
- 1,670 View
- 44 Download
- 2 Crossref

Case Report
- Arthroscopic Assisted Bioabsorbable Screw Fixation for Radial Head Fractures: A Report of Two Cases
- Bong Ju Park, Ki Yong An, Yong Suk Choi
- J Korean Fract Soc 2017;30(1):35-39. Published online January 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.1.35
-
 Abstract
Abstract
 PDF
PDF - Most radial head fractures occur as the result of low-energy mechanisms, such as a trip or fall on the outstretched hand. These fractures typically occur when an axial load is applied to the forearm, causing the radial head to hit the capitellum of the humerus. Good results are shown with nonsurgical treatments for Mason type 2 fractures. However, if there is a limitation of elbow joint exercise or displacement of more than 2 mm, an operative treatment should be considered. We treated two patients with arthroscopic assisted bioabsorbable screw (K-METâ„¢; U&I Corporation, Uijeongbu, Korea) fixation for radial head fractures to prevent complications of open reduction and minimize radiation exposure.
-
Citations
Citations to this article as recorded by- Bioabsorbable Screws Used in Hallux Valgus Treatment Using Proximal Chevron Osteotomy
Woo-Jin Shin, Young-Woo Chung, Ki-Yong An, Jae-Woong Seo
Journal of Korean Foot and Ankle Society.2018; 22(4): 181. CrossRef
- Bioabsorbable Screws Used in Hallux Valgus Treatment Using Proximal Chevron Osteotomy
- 650 View
- 3 Download
- 1 Crossref

Review Article
- Diagnosis and Management of Ligament Injuries of the Wrist
- Ki Tae Na, Joo Yup Lee
- J Korean Fract Soc 2016;29(2):160-170. Published online April 30, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.2.160
-
 Abstract
Abstract
 PDF
PDF - The wrist joint is formed by the distal end of the radius and ulna proximally, and eight carpal bones distally. It has many ligaments to maintain stability of the complex bony structures. The incidence of ligament injuries of the wrist has increased due to sports activities. However, diagnosis and management of these injuries are sometimes difficult because of the anatomic complexity and variable injury patterns. Among them, scapholunate ligament injury and triangular fibrocartilage tears are the two most common injuries resulting in chronic disabling wrist pain. Thorough understanding of the wrist anatomy and physical and radiologic examination is mandatory for proper diagnosis and management of these conditions. This article will briefly discuss the wrist joint anatomy and biomechanics, and review the diagnosis and management of the scapholunate ligament injury and triangular fibrocartilage injury.
- 1,006 View
- 15 Download

Case Reports
- Breakage of Cephalomedullary Nail Used in the Treatment of Proximal Femur Fractures: Case Report
- Seok Hyun Kweon, Chang Hyun Shin, Jin Sung Park, Byoung San Choi
- J Korean Fract Soc 2016;29(1):42-49. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.42
-
 Abstract
Abstract
 PDF
PDF - Internal fixation using a cephalomedullary nail as treatment for proximal femur fracture has recently been popular for early ambulation and rehabilitation. However metal breakage at the lag screw insertion site was reported due to non-union, delayed-union, and early weight bearing. In our orthopedic department, we experienced 2 cases of nail breakage at the lag screw insertion site, therefore we report on evaluation of the cause of metal failure and prevention of complications with literature review.
-
Citations
Citations to this article as recorded by- Breakage of the Tail Portion of the Lag Screw during Removal of Proximal Femoral Zimmer Natural Nail: Report of Two Cases with Technical Notes
Asep Santoso, Ik-Sun Choi, Kyung-Soon Park, Taek-Rim Yoon
Hip & Pelvis.2017; 29(3): 199. CrossRef
- Breakage of the Tail Portion of the Lag Screw during Removal of Proximal Femoral Zimmer Natural Nail: Report of Two Cases with Technical Notes
- 671 View
- 4 Download
- 1 Crossref

- Salvage Therapy from Traumatic Ischemic Finger Necrosis via Prostaglandin E1 Assisted Conservative Treatment: A Case Report
- Jae Hyuk Shin, Ho Guen Chang, Cheol Jung Yang, Jungtae Ahn
- J Korean Fract Soc 2015;28(4):245-249. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.245
-
 Abstract
Abstract
 PDF
PDF - Prostaglandin E1 (PGE-1) is a potent vasodilator, which also inhibits platelet aggregation, affects the blood flow viscosity, and fibrinolysis. The compound also excerts anti-inflammatory effects by inhibiting the monocyte and neutrophil function. PGE-1 has been widely administered following microvascular flap surgery, along with perioperative antithrombotic agents such as low molecular weight heparin or aspirin, showing excellent results. We report a case showing successful salvage recovery from post-traumatic ischemic necrosis of the finger via PGE-1 assisted conservative treatment.
- 625 View
- 2 Download

Original Articles
- Clinical Outcomes of Fasciotomy for Acute Compartment Syndrome
- Ji Yong Park, Young Chang Kim, Ji Wan Kim
- J Korean Fract Soc 2015;28(4):223-229. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.223
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate clinical outcomes and complications after fasciotomy in acute compartment syndrome.
MATERIALS AND METHODS
Seventeen cases diagnosed as compartment syndrome and underwent fasciotomy from January 2011 to February 2015 were evaluated retrospectively. We investigated the causes and regions of acute compartment syndrome, the methods of wound management, the necessity of skin graft, and the complications including amputation and infection.
RESULTS
According to the causes of acute compartment syndrome, there were 7 fractures, 1 traumatic hematoma, 6 reperfusion injury, and 3 rhabdomyolysis. The regions of acute compartment syndrome were 3 cases of thigh, 10 cases of leg, and 3 cases of foot. One case had acute compartment syndrome involving thigh, leg, and foot. Of 17 cases, 3 cases died due to reperfusion injury and one case with severe necrosis of soft tissues underwent amputation. Among the 13 cases excluding 4 cases with death or amputation, 3 cases underwent split thickness skin graft. Shoelace technique and/or vacuum-assisted closure (VAC) was used for 9 cases, and wound closure without skin graft was achieved in all except one case, while 2 cases required skin graft among 4 cases without shoelace technique or VAC. There were 2 cases of infection.
CONCLUSION
Acute compartment syndrome caused by reperfusion injury had poor outcomes. Shoelace technique and/or VAC were useful for management of wound after fasciotomy.
- 561 View
- 5 Download

- Results of Tension Band Wiring and Additional Circumferential Wiring in Treatment of Comminuted Patella Fracture
- Young Min Lee, Kook Jin Chung, Ji Hyo Hwang, Hong Kyun Kim, Yong Hyun Yoon
- J Korean Fract Soc 2014;27(3):206-212. Published online July 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.3.206
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the results of tension band wiring and additional circumferential wiring in treatment of comminuted patella fractures.
MATERIALS AND METHODS
A retrospective study of 67 patients with follow-up period longer than six months who underwent tension band wiring and additional circumferential wiring for comminuted patellar fracture from January 2004 to December 2012 was conducted. Analysis was based on radiological evaluation of bony union and articular surface displacement, and clinically by evaluating the postoperative function of the knee joint using the Levack scoring system.
RESULTS
Only one case out of 67 (1.5%) showed nonunion without metal breakage while good bone union was achieved in all other cases. Excluding the nonunion case, range of motion was 90 degrees minimum, 135 maximum, 129 on average. Average displacement was less than 2 mm, and 64 out of 67 cases showed satisfactory outcome with excellent functional score according to the Levack scoring system.
CONCLUSION
Tension band wiring and additional circumferential wiring technique for treatment of comminuted patella fractures can be considered as an effective treatment for achievement of good bone union and restoration of normal knee function. -
Citations
Citations to this article as recorded by- A Novel Technique in Comminuted Patella Fractures: Minimally Invasive Pericerclage Osteosynthesis Using Drainage Trocar
Fırat Fidan, Abdülkadir Polat, Cengiz Kazdal, Emre Bal
Bakirkoy Tip Dergisi / Medical Journal of Bakirkoy.2022; 18(4): 427. CrossRef - Current Treatment Strategies for Patella Fractures
David J. Hak, Philip F. Stahel, Dustin J. Schuett, Mark E. Hake, Cyril Mauffrey, E. Mark Hammerberg, Philip F. Stahel, David J. Hak
Orthopedics.2015; 38(6): 377. CrossRef
- A Novel Technique in Comminuted Patella Fractures: Minimally Invasive Pericerclage Osteosynthesis Using Drainage Trocar
- 744 View
- 8 Download
- 2 Crossref

Case Report
- Modified Tension Band Wiring Combined with Anti-Gliding Loop Augmentation Technique for the Treatment of Comminuted Patellar Fracture: Technical Note and Report of Early Results: Technical Note
- Han Jun Lee, Jae Jun Yang, Ho Joong Jung, Hyoung Seok Jung
- J Korean Fract Soc 2013;26(4):321-326. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.321
-
 Abstract
Abstract
 PDF
PDF - In order to investigate the feasibility of a modified tension band combined with anti-gliding loop augmentation technique for the treatment of comminuted patellar fracture, 21 patients with comminuted patellar fracture were enrolled in this study. After the modified tension band wiring of patellar fracture, a cerclage wire was passed around the patella. Anti-gliding loops were made on the bending sites of Kirshner-wires. A knot was tied using both ends of the anti-gliding loops, and the cerclage wire was tightened using proximal knots. Bone union was achieved at 4.5+/-1.5 months postoperatively without nonunion. The Lysholm score was 87.1+/-2.8, and the range of motion of the knee was 2.1degrees+/-3.4degrees to 132.2degrees+/-6.5degrees at the last follow-up. The modified tension band combined with anti-gliding loop augmentation technique might be considered an alternative modification of modified tension band wiring for the treatment of comminuted patellar fracture.
- 448 View
- 0 Download

Original Articles
- The Result of Conservative Treatment of Proximal Humerus Fracture in Elderly Patients
- Seung Gil Baek, Chang Wug Oh, Young Soo Byun, Jong Keon Oh, Joon Woo Kim, Jong Pil Yoon, Hyun Joo Lee, Hyung Sub Kim
- J Korean Fract Soc 2013;26(4):292-298. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.292
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
With the increase in the old age population, proximal humerus fractures have been increasing recently. However, complications after operative treatment, such as fixation failure, are common because of osteoporosis. We treated proximal humerus fractures in patients with osteoporosis conservatively, and evaluated the radiographic and functional results by analyzing the factors affecting the results.
MATERIALS AND METHODS
Nineteen out of 30 cases for whom the clinical follow-up was over 1 year were included in this retrospective study. There were 17 females and 2 males, and the mean age was 73.2 years. The causes were slip from a short height (18 cases) and a minor car accident (1 case). We evaluated the union period, nonunion, malunion and the Constant score and analyzed several factors affecting the functional result, such as age, fracture pattern, and malunion.
RESULTS
Seventeen cases (89.5%) obtained union within 12.8 weeks on average. Neck-shaft angle was 125.3degrees on average, with seven cases of malunion. The Constant score was 84.1 on average, and there were excellent scores in 11 cases, good scores in 4 cases, and fair scores in 2 cases. Fracture pattern, neck-shaft angle, or malunion did not affect the functional outcome, and elderly patients showed poorer shoulder function.
CONCLUSION
Proximal humeral fractures with osteoporosis may achieve a high rate of bony union when treated with conservative methods. Despite the common occurrence of malunion, a satisfactory functional outcome may be expected.
- 730 View
- 6 Download

- Results of the Kapandji Procedure in the AO Type C Distal Radius Fracture in Patients over Age 60
- Chul Hong Kim, Sung Soo Kim, Myung Jin Lee, Hyeon Jun Kim, Bo Kun Kim, Young Hoon Lim
- J Korean Fract Soc 2012;25(3):191-196. Published online July 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.3.191
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the clinical and radiologic results of the Kapandji procedure in AO classification type C distal radius fracture patients over 60 years old.
MATERIALS AND METHODS
Twenty-one type C distal radius fracture patients over the age of 60 years who were treated with the Kapandji procedure from June 2004 to June 2009 in our hospital and had a post-operative follow-up period of more than 1 year were enrolled. The volar tilt, radial inclination, and radial length were measured for the radiographic analysis using the modified Lidstrom scoring system about post-operative reduction loss in every follow-up radiogram. The clinical result was assessed with a visual analogue scale (VAS) and Korean Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH) score at the last follow-up.
RESULTS
The mean radiologic loss of volar tilt was 1.1degrees and the mean loss of radial length was 2.6 mm and the mean radial inclination loss was 2.7degrees compared with the immediate post-operative period and last follow-up period. The average VAS and DASH scores were 1.4 and 15.9.
CONCLUSION
The radiologic results of closed reduction and percutaneous pinning using the Kapandji technique for distal radius AO type C fracture patients over 60 years of age was not satisfactory. Nevertheless, the clinical results were satisfactory.
- 392 View
- 2 Download

- The Results of Two Stage Surgical Treatment of Pilon Fractures
- Hong Moon Sohn, Jun Young Lee, Sang Ho Ha, Sang Hong Lee, Gwang Chul Lee, Kwang Hyo Seo
- J Korean Fract Soc 2012;25(3):177-184. Published online July 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.3.177
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To report the good results of two-stage treatment in pilon fractures.
MATERIALS AND METHODS
A retrospective study of 23 patients among 30 patients with pilon fractures from March 2006 to November 2008, who underwent two-stage treatment of pilon fractures with a minimum of 24 months follow-up. The mean follow-up period was 28 months (24~41 months). In the first stage of the operation, open reduction of the articular surface and external fixation were performed after minimal incision. As the soft tissue healed, locking compression plate fixation was performed with the Minimally invasive plate osteosynthesis. Radiographic evaluation was graded by the criteria of Burwell and Charnley, and functional assessment of the ankle was evaluated by the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score.
RESULTS
The fractures were united within 16 weeks (12~30 weeks). The radiologic results showed anatomical reduction in 18 cases and a mean AOFAS score of 81. The mean range of ankle motion was 44 degrees. There were four complications: 1 case of wound infection and 3 cases of ankle osteoarthritis.
CONCLUSION
Two-stage treatment of pilon fractures is a good treatment method because it is designed to obtain early anatomical reduction, definitive stable fixation, low rates of soft tissue complication, and good range of ankle motion. -
Citations
Citations to this article as recorded by- Current Concepts in Management of Pilon Fracture
Jun-Young Lee, Sang-Joon Lee
Journal of the Korean Fracture Society.2014; 27(2): 173. CrossRef
- Current Concepts in Management of Pilon Fracture
- 707 View
- 4 Download
- 1 Crossref

Case Report
- Repeated Metal Breakage in a Femoral Shaft Fracture with Lateral Bowing: A Case Report
- Dong Soo Kim, Yong Min Kim, Eui Sung Choi, Hyun Chul Shon, Kyoung Jin Park, Byung Ki Cho, Ji Kang Park, Hyun Cheol Lee, Kyung Ho Hong
- J Korean Fract Soc 2012;25(2):136-141. Published online April 30, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.2.136
-
 Abstract
Abstract
 PDF
PDF - Fractures of the femoral shaft with marked bowing face some obstacles in fixation of the fracture such as difficulty in insertion of the intramedullary nail (IM nail) or exact contouring plate. Locking compression plates (LCP) are an option to manage this problem. However, we experienced consecutive breakage of LCP twice and IM nail once in an 80-year-old female. Finally, union of the fracture was achieved after fixation of the IM nail and additional plate together. Fractures of the femur shaft with marked bowing are thought to have different biomechanical properties; therefore, we present this case with a review of the literature.
-
Citations
Citations to this article as recorded by- Comparative analysis of operation time and intraoperative fluoroscopy time in intramedullary and extramedullary fixation of trochanteric fractures
Milan Mitkovic, Sasa Milenkovic, Ivan Micic, Predrag Stojiljkovic, Igor Kostic, Milorad Mitkovic
Vojnosanitetski pregled.2022; 79(2): 177. CrossRef - Pre-operative planning for fracture fixation using locking plates: device configuration and other considerations
Alisdair R. MacLeod, Pankaj Pankaj
Injury.2018; 49: S12. CrossRef - Letter: Repeated Metal Breakage in a Femoral Shaft Fracture with Lateral Bowing - A Case Report -
Hae Seok Koh
Journal of the Korean Fracture Society.2012; 25(3): 240. CrossRef
- Comparative analysis of operation time and intraoperative fluoroscopy time in intramedullary and extramedullary fixation of trochanteric fractures
- 564 View
- 3 Download
- 3 Crossref

Original Articles
- Bleeding Volume after Surgery for Trochanteric Fractures of the Femur in Patients Treated with Antiplatelet Agents: Comparison according to Surgical Timing
- Se Ang Jang, Young Ho Cho, Young Soo Byun, Tae Gyun Kim, Hun Sik Cho, Sung Choi
- J Korean Fract Soc 2012;25(2):105-109. Published online April 30, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.2.105
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We evaluated the bleeding volume after surgery for trochanteric fractures of the femur in patients treated with antiplatelet agents according to surgical timing.
MATERIALS AND METHODS
We selected 20 patients who had trochanteric fractures of the femur treated with antiplatelet agents from January 2009 to June 2010. Group I included 9 patients who discontinued antiplatelet medication and had delayed operations at an average of 6.5 days and Group II included 11 patients who underwent early operations within 24 hours. Group I included 2 males and 7 females; their average age was 77.8 years (range 59~86). Group II included 4 males and 7 females, with an average age of 73.5 years (range 61~84). We compared the two groups' volume of intraoperative bleeding, the preoperative and postoperative hemoglobin levels and the volume of postoperative transfusion. The Mann-Whitney U test was used for statistical analysis.
RESULTS
The volume of intraoperative bleeding was 88 ml in group I and 106 ml in group II (p>0.01). The difference in the hemoglobin was a decrease of 2.4 mg% in group I and a decrease of 2.2 mg% in group II (p>0.01). The volume of postoperative transfusion was 0.6 pints in group I and 1 pint in group II (p>0.01).
CONCLUSION
We found a similar bleeding volume regardless of operative timing after surgery for trochanteric fractures of the femur in patients treated with antiplatelet agents. -
Citations
Citations to this article as recorded by- Is early hip fracture surgery safe for patients on clopidogrel? Systematic review, meta-analysis and meta-regression
B. Doleman, I.K. Moppett
Injury.2015; 46(6): 954. CrossRef - Morbidity and Mortality of the Elderly after Early Operation for Trochanteric Fractures
Se-Ang Jang, Young-Ho Cho, Young-Soo Byun, Ki-Hong Park, Hyun-Seong Yoo, Chul Jung
Journal of the Korean Fracture Society.2013; 26(3): 199. CrossRef
- Is early hip fracture surgery safe for patients on clopidogrel? Systematic review, meta-analysis and meta-regression
- 604 View
- 1 Download
- 2 Crossref

- Radiation Exposure Over the Course of a Year from an Image Intensifier in the Orthopaedic Operating Room
- Gu Hee Jung, Jae Ho Jang, Jae Do Kim, Chung Kyu Kim
- J Korean Fract Soc 2012;25(1):58-63. Published online January 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.1.58
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To measure the annual radiation exposure of staff in the orthopaedic surgical room.
MATERIALS AND METHODS
From January 2010 to December 2010, we measured the radiation exposure of a tumor surgeon, spine surgeon, trauma surgeon, six residents, and six scrub nurses. Radiation was monitored with the use of thermoluminescent dosimeters placed on the chest under the lead apron. The annual dose of radiation exposure was compared to the maximum yearly permissible dose (20 mSv). During the study period, the trauma surgeon made a deliberate effort to minimize the radiation time and maintain a distance of 1 m from the image intensifier.
RESULTS
The annual exposure levels were 0.04 mSv (radiation time, 34 min 50 s), 0.08 mSv (151 min 46 s), and 0.12 mSv (135 min 27 s) for the tumor surgeon, trauma surgeon, and spine surgeon, respectively. The mean exposure was 0.0146 mSv (range, 0.4~0.39 mSv) for the residents and 0.06 mSv (range, 0.04~0.13 mSv) for the scrub nurses. Overall, the annual radiation exposure was 0.2~1.95% of the maximal yearly permissible dose. Despite the longer period of radiation exposure, the trauma surgeon was exposed to a lower dose of radiation than the spine surgeon.
CONCLUSION
The annual radiation exposure of a trauma surgeon can be reduced by a deliberate effort to decrease exposure time and maintain a distance of at least 1 m from the image intensifier. -
Citations
Citations to this article as recorded by- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
Jungtae Ahn, Se-Lin Jeong, Gu-Hee Jung
Journal of Musculoskeletal Trauma.2025; 38(2): 74. CrossRef - Current status of occupational radiation exposure and protection among medical interns and residents
Seungwon Cho, Hangyeol Lee, Minku Kang, Won Jin Lee, Seulki Ko
Journal of the Korean Medical Association.2024; 67(2): 134. CrossRef - Radiation exposure and fluoroscopically-guided interventional procedures among orthopedic surgeons in South Korea
Seonghoon Kang, Eun Shil Cha, Ye Jin Bang, Teresa W. Na, Dalnim Lee, Sang Youn Song, Won Jin Lee
Journal of Occupational Medicine and Toxicology.2020;[Epub] CrossRef
- How to obtain the desired results from distal tibial nailing based on anatomy, biomechanics, and reduction techniques
- 648 View
- 2 Download
- 3 Crossref

- Cement Leakage into Disc after Kyphoplasty: Does It Increases the Risk of New Adjacent Vertebral Fractures?
- Hoon Sang Sohn, Seong Kee Shin, Eun Seok Seo, Kang Seob Chang
- J Korean Fract Soc 2011;24(4):361-366. Published online October 31, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.4.361
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study aims to investigate the relationship between cement leakage into the disc during percutaneous balloon kyphoplasty and subsequent compression fractures in adjacent vertebrae during treatment of osteoporotic vertebral compression fracture.
MATERIALS AND METHODS
103 patients (118 vertebrae) who have been treated with balloon kyphoplasty due to osteoporotic compression fracture from June 2007 to July 2010 were retrospectively analyzed. The group was composed of 13 males and 90 females. The mean age was 75 years (57~95 years). The mean follow-up period was 10 months (6~30 months). Patients were divided into two groups; one with cement leakage into the disc and the other without cement leakage into the disc. The study was performed to determine whether subsequent compression fractures in adjacent vertebrae were related to several factors.
RESULTS
The cement leakages into the disc occurred in 16 of 118 vertebrae. Of the 16 vertebrae with cement leakage into the disc, 5 (31%) had subsequent adjacent vertebral compression fractures; however, of the 102 vertebrae in which cement leakage did not occur, only 11 (11%) had subsequent adjacent vertebral compression fractures (p<0.05). Of the 16 vertebrae with cement leakage into the disc, subsequent adjacent vertebral compression fractures occurred 1 vertebrae of 10 vertebrae with definite trauma history. Out of the 6 vertebrae with cement leakage and no definite trauma history, 4 vertebrae (67%) had subsequent adjacent vertebral compression fractures (p<0.05).
CONCLUSION
The cement leakage into the disc significantly increases the incidence of subsequent adjacent vertebral compression fractures. Most of the subsequent fractures occurred in the early post-operative period. When cement leakage into the disc occurred in patients with no definite trauma history such as slip down, the incidence of subsequent adjacent vertebral compression fracture increased significantly.
- 810 View
- 7 Download

- Does Interfragmentary Cerclage Wire Fixation in Clavicle Shaft Fracture Interfere the Fracture Healing?
- Jae Kwang Yum, Yong Woon Shin, Hee Sung Lee, Jae Gu Park
- J Korean Fract Soc 2011;24(2):138-143. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.138
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
A technique of cerclage wire fixation in comminuted fracture of the clavicle shaft is thought to interfere the fracture healing, so authors studied radiographically and clinically about the cases of cerclage wiring of the fracture fragments with the plate and screws fixation in the comminuted fracture of the shaft of the clavicle.
MATERIALS AND METHODS
According to following inclusion criteria, total 18 patients (male: 15, female: 3) were investigated; Patients who visited hospital due to clavicle shaft comminuted fracture from February 2005 to April 2009, who underwent surgery utilizing more than 2 cerclage wire fixation for the fragments when open reduction and plate fixation were operated and who could be follow-up over one year. The duration for fracture union, functional outcome and complications were investigated retrospectively.
RESULTS
Radiological bone union was accomplished in average 13.3 weeks (12~16 weeks) and there was no complication such as nonunion, delayed union or infection. Range of motion of ipsilateral shoulder joint was recovered in all patients except one at the final follow-up.
CONCLUSION
The clinical and radiographical results of the plate and screws fixation with cerclage wiring of the fragments in comminuted clavicle shaft fracture showed that the cerclage wiring does not interfere the fracture healing, so authors think that this method is a good alternative operation if it is performed carefully to minimize soft tissue dissection. -
Citations
Citations to this article as recorded by- Surgical Management of Comminuted Midshaft Clavicle Fractures Using Reconstruction Plate and Circumferential Wiring: Does the Circumferential Wiring Interfere with the Bone Union?
Kyung-Tae Kim, Chung-Shik Shin, Young-Chul Park, Dong-hyun Kim, Min-Woo Kim
Journal of the Korean Orthopaedic Association.2021; 56(3): 245. CrossRef - Supplementary Technique for Unstable Clavicle Shaft Fractures: Interfragmentary Wiring and Temporary Axial K-Wire Pinning
Jinmyoung Dan, Byung-Kook Kim, Ho-Jae Lee, Tae-Ho Kim, Young-Gun Kim
Clinics in Orthopedic Surgery.2018; 10(2): 142. CrossRef - Use of Composite Wiring on Surgical Treatments of Clavicle Shaft Fractures
Kyung Chul Kim, In Hyeok Rhyou, Ji Ho Lee, Kee Baek Ahn, Sung Chul Moon
Journal of the Korean Fracture Society.2016; 29(3): 185. CrossRef - TO EVALUATE THE SURGICAL OUTCOME OF NON-UNION CLAVICLE USING PLATE AND SLIVERS OF AUTOLOGOUS ILIAC CREST CORTICOCANCELLOUS BONE GRAFT
Mohammed Tauheed, Shashi Kumar Yalagach, Vivek Purushothaman, Anwar Shareef Kunnath K
Journal of Evidence Based Medicine and Healthcare.2016; 3(25): 1121. CrossRef - Anatomical Reduction of All Fracture Fragments and Fixation Using Inter-Fragmentary Screw and Plate in Comminuted and Displaced Clavicle Mid-Shaft Fracture
Kyoung Hwan Koh, Min Soo Shon, Seung Won Lee, Jong Ho Kim, Jae Chul Yoo
Journal of the Korean Fracture Society.2012; 25(4): 300. CrossRef
- Surgical Management of Comminuted Midshaft Clavicle Fractures Using Reconstruction Plate and Circumferential Wiring: Does the Circumferential Wiring Interfere with the Bone Union?
- 792 View
- 0 Download
- 5 Crossref

- Staged Minimally Invasive Plate Osteosynthesis of Proximal Tibial Fracture
- Joon Woo Kim, Chang Wug Oh, Jong Keon Oh, Hee Soo Kyung, Woo Kie Min, Byung Chul Park, Kyung Hoon Kim, Hee Joon Kim
- J Korean Fract Soc 2009;22(1):6-12. Published online January 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.1.6
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the results of staged MIPO (Minimally Invasive Plate Osteosynthesis) for proximal tibial fractures with compromised soft tissue.
MATERIALS AND METHODS
Eighteen proximal tibial fractures (AO 41:9 cases, AO 42:9 cases) included this study. Ten were open fractures. After temporary external fixation until soft tissue healed (mean 27.3 days), MIPO was performed secondarily without bone graft. We assessed the bony union and knee function, and affecting factors of the results were investigated.
RESULTS
All fractures united at 20 weeks (range, 11~32) except 1 case. Mean range of knee flexion was 134.4degrees and mean IOWA knee score was 89.1. There were 2 superficial and 2 delayed deep infections from open fractures (grade II:1 case, grade III:3 cases), although they healed after implant removal. Open fractures seem to influence the infection rate. Otherwise, there was no related factor affecting the results.
CONCLUSION
MIPO after temporary external fixation can provide favorable results in proximal tibial fractures with soft tissue injuries, but attention of delayed infection should be paid in open fractures. -
Citations
Citations to this article as recorded by- MINIMALLY INVASIVE OSTEOSYNTHESIS WITH PLATE OR NAIL FOR META-DIAPHYSEAL TIBIAL FRACTURES - WHAT IS BETTER?
B. Makelov
Trakia Journal of Sciences.2023; 21(4): 357. CrossRef - Effect of Korean Medicine Treatments in Patients with Proximal Tibia Fracture: A Retrospective Observational Study
Jung Min Lee, Eun-Jung Lee
Journal of Korean Medicine Rehabilitation.2020; 30(3): 141. CrossRef - Comparison of Time to Operation and Efficacies of Ultrasound-Guided Nerve Block and General Anesthesia in Emergency External Fixation of Lower Leg Fractures (AO 42, 43, 44)
Chan Kang, Sang-Bum Kim, Youn-Moo Heo, You-Gun Won, Byung-Hak Oh, June-Bum Jun, Gi-Soo Lee
The Journal of Foot and Ankle Surgery.2017; 56(5): 1019. CrossRef - Minimally Invasive Plate Osteosynthesis for Proximal Tibial Shaft Fracture
Young-Soo Byun, Ki-Chul Park, Hyun-Jong Bong, Chang-Hoon Lee
Journal of the Korean Fracture Society.2011; 24(1): 23. CrossRef - The Use of Fresh Frozen Allogenic Bone Graft in the Impacted Tibial Plateau Fractures
Yeung Jin Kim, Soo Uk Chae, Jung Hwan Yang, Ji Wan Lee, Dae Han Wi, Duk Hwa Choi
Journal of the Korean Fracture Society.2010; 23(1): 26. CrossRef - Management of Open Fracture
Gu-Hee Jung
Journal of the Korean Fracture Society.2010; 23(2): 236. CrossRef - Staged Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures
Sung-Ki Park, Chang-Wug Oh, Jong-Keon Oh, Kyung-Hoon Kim, Woo-Kie Min, Byung-Chul Park, Won-Ju Jeong, Joo-Chul Ihn
Journal of the Korean Fracture Society.2010; 23(3): 289. CrossRef - Intramedullary Nailing of Proximal Tibial Fractures
Young-Soo Byun, Dong-Ju Shin
Journal of the Korean Fracture Society.2009; 22(3): 197. CrossRef - Proximal Tibia Fracture: Plating
Ki-Chul Park
Journal of the Korean Fracture Society.2009; 22(3): 206. CrossRef
- MINIMALLY INVASIVE OSTEOSYNTHESIS WITH PLATE OR NAIL FOR META-DIAPHYSEAL TIBIAL FRACTURES - WHAT IS BETTER?
- 647 View
- 0 Download
- 9 Crossref

- Cerclage Wiring in Internal Fixation of Displaced Acetabular Fractures
- Chong Kwan Kim, Jin Woo Jin, Jong Ho Yoon, Sung Won Jung, Jung Wook Peang
- J Korean Fract Soc 2008;21(2):95-102. Published online April 30, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.2.95
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the usefulness of wire fixation in displaced acetabular fractures.
MATERIALS AND METHODS
From January 2000 to December 2005, 19 cases of displaced acetabular fracture were treated with wire fixation. According to Letournel's classification there were 9 both column fracture, 5 transverse fracture, 3 anterior column with posterior hemitransverse and 2 T-type fracture. Only wire fixation in 13 cases and wire with plate or wire with screw fixation in 6 cases.
RESULTS
We evaluate the accuracy of reduction by Matta' criteria, anatomical reduction in 12 cases, incomplete reduction in 4 cases, poor reduction in 2 cases and surgical secondary congruence in 1 case. The clinical results showed excellent in 12 cases, good in 4 cases, fair in 2 cases and poor in 1 case. The radiological results showed excellent in 10 cases, good in 4 cases, fair in 3 cases and poor in 2 cases. There were 4 cases of complication; wound infection in 1case, post-traumatic arthritis in 1 case and heterotopic ossification in 2 cases.
CONCLUSION
The cerclage wiring is a preferable method in internal fixation of displaced acetabular fractures that can facilitate reduction and achieve stable fixation. -
Citations
Citations to this article as recorded by- Cerclage Clamping Using Cerclage Passer for Reduction of Anterior and Posterior Column Fracture
Ki Chul Park, Hyun Joong Cho, Hun Chul Kim, Kyung-Sik Min, Hae Won Jeong
Journal of the Korean Orthopaedic Association.2016; 51(6): 486. CrossRef - Comparative Results of Acetabular Both Column Fracture According to the Fixation Method
Kyung-Jae Lee, Byung-Woo Min, Eun-Seok Son, Hyuk-Jun Seo, Jin-Hyun Park
Hip & Pelvis.2011; 23(2): 131. CrossRef
- Cerclage Clamping Using Cerclage Passer for Reduction of Anterior and Posterior Column Fracture
- 539 View
- 3 Download
- 2 Crossref

- Arthroscopic Repair for Traumatic Peripheral Tear of Triangular Fibrocartilage Complex
- Seung Ju Jeon, Chan Sam Moon, Ho Seung Jeon, Haeng Kee Noh, Sung Hwan Kim
- J Korean Fract Soc 2007;20(4):330-334. Published online October 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.4.330
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the results of an arthroscopic repair for traumatic peripheral tears of triangular fibrocartilage complex (TFCC, Palmer type Ib).
MATERIALS AND METHODS
10 patients with traumatic peripheral TFCC tear were treated with outside-in technique with arthroscope and evaluated with an average follow-up of 19 months (range, 15 to 28 months). The clinical outcomes were assessed with investigation of pain, range of motion, grip strength, return to job and patient's satisfaction.
RESULTS
The arthroscopic repair of traumatic peripheral TFCC tear resulted in significant pain relief and increase in functional ability of wrist, that is, 8 excellent, 1 good and 1 fair results. At last follow-up, the average of flexion was 79° (range 76~86°), average of extension was 78° (range 70~84°), average pronation was 85° (range 75~91°) and average supination was 87° (range 79~92°). Nine patients except one were back to their original job.
CONCLUSION
Arthroscopic repair of traumatic peripheral TFCC tear could be used for pain relief and increase in functional ability of wrist.
- 431 View
- 1 Download

Case Report
- Fatal Hemothorax Following Percutaneous Vertebroplasty: A Case Report
- Hee Gon Park, Joo Hong Lee
- J Korean Fract Soc 2007;20(2):202-205. Published online April 30, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.2.202
-
 Abstract
Abstract
 PDF
PDF - Overall, the percutaneous vertebroplasty has low complication rate. Nevertheless, severe complications can occur. The majority of these are related to cement leakage. The cement migration through perivertebral venous system can lead to fatal complication. We present a case of death by hemothorax due to cement leakage following percutaneous vertebroplasty with literature review.
- 330 View
- 3 Download

Original Articles
- Trochanteric Management for Unstable Intertrochanteric Femoral Fracture in the Elderly Patients
- Duk Hwan Kho, Ju Yong Shin, Ki Hwan Kim, Jun Hyuck Lee, Dong Heon Kim
- J Korean Fract Soc 2007;20(2):129-134. Published online April 30, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.2.129
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the results after fixation with figure of eight and cerclage wiring for comminuted trochanteric fracture. Because comminution of the femoral trochanteric fracture in elderly patients is severer in the operating field than x-ray findings, so the fixation is more difficult.
MATERIALS AND METHODS
Between March 1998 and March 2004, the clinical records on twenty-eight patients more than 70 years old who underwent the bipolar hemiarthroplaty using calcar replacement type of femoral stem and followed more than 24 months were reviewed. Figure of eight and cerclage wiring was used for the comminuted trochanteric fracture of the femoral intertrochanteric fracture. The mean age was 80.4 (70~103) years. 19 cases were female, 9 cases were male. Mean follow-up period was 58 (24~92) months. We evaluated the results by modified Harris hip score, walking ability, activity of daily living, radiologic findings and union of the fracture.
RESULTS
The mean duration of bony union was 12 weeks. The mean postoperative modified Harris hip score was 82.3. Preoperative walking ability was recovered in 23 cases (82%). Also basic activity of daily living was recovered in 22 cases (79%). Nonunion of trochanter was found in only one case by radiologic evaluation but clinical correlation was not significant.
CONCLUSION
We consider fixation with figure of eight and cerclage wiring for unstable intertrochanteric fracture of femur in the elderly patient is more appropriate in terms of convenience of fixation, duration of union, early ambulation and cost effectiveness. -
Citations
Citations to this article as recorded by- Outcomes of dynamic hip screw augmented with trochanteric wiring for treatment of unstable type A2 intertrochanteric femur fractures
Chetan Puram, Chetan Pradhan, Atul Patil, Vivek Sodhai, Parag Sancheti, Ashok Shyam
Injury.2017; 48: S72. CrossRef - Fixation of Greater Trochanter Using an AO Trochanteric Reattachment Device (AO TRD) in Arthroplasty for Intertrochanteric Femur Fracture of Elderly Patients
Weon-Yoo Kim, Young-Yul Kim, Jae-Jung Jeong, Do-Joon Kang
Hip & Pelvis.2013; 25(4): 274. CrossRef - Bipolar Hemiarthroplasty Using the Greater Trochanter Reattachment Device (GTRD) for Comminuted Intertrochanteric Femur Fracture in Elderly Patients
Jin-Wan Kim, Young-Chul Ko, Chul-Young Jung, Il-Soo Eun, Hyeon-Soo Choi, Ok-Gul Kim, Young-June Kim
Journal of the Korean Fracture Society.2009; 22(4): 232. CrossRef
- Outcomes of dynamic hip screw augmented with trochanteric wiring for treatment of unstable type A2 intertrochanteric femur fractures
- 844 View
- 6 Download
- 3 Crossref

- Treatment of High-energy Distal Tibia Intraarticular Fractures with Two-staged Delayed Minimal Invasive Plate Osteosynthesis
- Hong Moon Sohn, Jun Young Lee, Sang Ho Ha, Jae Won You, Sang Hong Lee, Kwang Chul Lee
- J Korean Fract Soc 2007;20(1):19-25. Published online January 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.1.19
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the short-term results of two-staged delayed minimal invasive plate osteosynthesis in high-energy intraarticular fractures of the distal tibia.
MATERIALS AND METHODS
Thirteen patients, who underwent two-staged delayed minimal invasive plate osteosynthesis for intraarticular fractures of the distal tibia between January 2002 and July 2004, were followed for more than one year. The mean interval time between first stage and second stage of the procedures was 28.6 days (range, 14~34 days). By Ruedi-Allgower classification, there were two cases in type I, three cases in type II, and eight cases in type III. There were six cases in type B and seven cases in type C patients according to AO/OTA classification. Radiographs were graded by the criteria of Burwell and Charnley and ankle functions were graded by the criteria of Mast and Teipner. Union time and postoperative complications were also analysed.
RESULTS
Average union time was 16.9 weeks (range, 14~20 weeks) in twelve of the thirteen fractures, but there was one fracture resulting in soft tissue complication and infected nonunion. At the latest follow-up, review of the radiographic results showed that ten cases of fractures (77%) achieved an anatomic reduction, two cases (15%) achieved fair reduction and one case (8%) achieved a poor reduction. And clinical functional assessment showed that nine cases (69%) were good results, three cases were (23%) fair results and one case (8%) was poor result.
CONCLUSION
Two-staged delayed minimal invasive plate osteosynthesis is an excellent option for the treatment of high-energy intraarticular fractures of the distal tibia. -
Citations
Citations to this article as recorded by- Staged Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures
Sung-Ki Park, Chang-Wug Oh, Jong-Keon Oh, Kyung-Hoon Kim, Woo-Kie Min, Byung-Chul Park, Won-Ju Jeong, Joo-Chul Ihn
Journal of the Korean Fracture Society.2010; 23(3): 289. CrossRef - The Comparison of Minimally Invasive Plate Osteosynthesis and Intramedullary Nailing in the Treatment of the Proximal and Distal Tibia Fracture
Joon Soon Kang, Seung Rim Park, Sang Rim Kim, Yong Geun Park, Jae Ho Jung, Sung Wook Choi
Journal of the Korean Fracture Society.2010; 23(2): 172. CrossRef - Two-staged Delayed Minimally Invasive Percutaneous Plate Osteosynthesis for Distal Tibial Open Fractures
Jung Hwan Yang, Seok Hyun Kweon, Jeung Woo Kim, Jin Young Park, Hyun Jun Kim, Chul Min Lim
Journal of the Korean Fracture Society.2008; 21(1): 24. CrossRef
- Staged Minimally Invasive Plate Osteosynthesis of Distal Tibial Fractures
- 587 View
- 2 Download
- 3 Crossref

- Comparison of Uniportal and Biportal Vertebroplasty in Bone Cement Distribution and Leakage
- Jae Hyup Lee, Kang Sup Yoon, Seung Baik Kang, Hyunchul Jo, Sang Ki Lee, Bong Soon Chang, Choon Ki Lee, Ji Ho Lee
- J Korean Fract Soc 2006;19(4):471-476. Published online October 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.4.471
-
 Abstract
Abstract
- PURPOSE
To evaluate the differences of radiological outcomes of uniportal and biportal vertebroplasty in the point of bone cement distribution and leakage.
MATERIALS AND METHODS
A retrospective study reviewing the period between May 2002 and January 2006 investigated 100 vertebrae which underwent vertebroplasty and followed for more than three months by uniportal approach (55 vertebrae, group 1) and biportal approach (45 vertebrae, group 2). The operative time, the amount of bone cement injected, anterior vertebral height restoration, kyphotic angle, bone cement distribution, and bone cement leakage were evaluated.
RESULTS
The amount of injected bone cement of group 1 (3.9 cc) was statistically smaller than that of group 2 (5.1 cc) (p=0.016). There were no significant differences in the operative time, anterior vertebral height restoration, kyphotic angle in both groups. The rate of bone cement distribution over 8 zones was significantly higher in group 2 than in group 1 (p=0.014). However, the rate of bone cement distribution over 7 zones and the rate of bone cement distributed on whole anterior vertebral body were not significantly different in both groups. The cement leakage was not also significantly different in both groups.
CONCLUSION
Although the amount of injected bone cement was smaller in uniportal vertebroplasty, the radiological results and cement leakage were similar to biportal vertebroplasty. These findings suggest that uniportal vertebroplasty can be the operative options in osteoporotic vertebral fracture.
- 327 View
- 0 Download

- Comparison of Open Fixation and Closed Percutaneous Pinning in Jakob Stage II Lateral Condylar Fractures of Children
- Eui Sung Choi, Dong Soo Kim, Hyun Chul Shon, Yong Min Kim, Kyoung Jin Park, Jun Mo Jeon, Gee Kang Park
- J Korean Fract Soc 2006;19(2):277-282. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.277
-
 Abstract
Abstract
- PURPOSE
To compare the results of open fixation and closed percutaneous pinning in managing Jakob stage II lateral condylar fractures of children's elbow.
MATERIALS AND METHODS
Since Febuary 2000, We operated 21 children with Jakob stage II lateral condylar fractures of elbow. Eleven of the 21 were treated with closed percutaneous pinning, open fixation was done to the other 10 children. Each patient was evaluated about range of motion, carrying angle, scar satisfaction and radiologic findings for comparison between closed pinning and open fixation groups.
RESULTS
Open fixation group showed 3.8 degrees decrease of elbow motion while closed pinning group showed no significant decrease. Carrying angle and radiologic findings were not different between the two groups. Open fixation group expressed dissatisfaction to their scars (average 5.2 cm) whereas all the patients of closed pinning group were satisfied with their functional and cosmetic outcomes.
CONCLUSION
In managing Jakob stage II lateral condyle fractures of children's elbow, closed percutaneous pinning was thought to be superior to open fixation because of the same functional outcome and much better cosmetic results.
- 343 View
- 0 Download

- Treatment of Pediatric Displaced Supracondylar Fractures of the Humerus by Pin Leverage Technique
- Han Yong Lee, Joo Hyoun Song
- J Korean Fract Soc 2006;19(1):83-88. Published online January 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.1.83
-
 Abstract
Abstract
- PURPOSE
To evaluate a new treatment method by pin leverage technique in Gartland type III fractures to avoid forceful manipulation or open reduction.
MATERIALS AND METHODS
99 cases were included in this study and divided into 3 groups (I;open reduction, II; closed reduction and percutaneous pin fixation, III; pin leverage technique), and we analyzed timing to operation, length of operation, associated neurovascular injuries, complications, and clinical and radiological outcomes at final follow-up.
RESULTS
The average length of operation 119, 57, and 68 minutes respectively. The associated nerve injuries were 8, 2, and 2 cases respectively. There were a case of superficial pin tract infection in group I, three cases of superficial pin tract infection and a case of iatrogenic ulnar nerve injury in group II. At final follow-up, clinical results were excellent or good in all cases and there were 5 cases (8.3%) of fair results in group II radiologically. Closed reduction with pin leverage technique were failed in 5 cases.
CONCLUSION
In treatment of Gartland type III fractures, pin leverage reduction technique is considered to be a good alternative prior to open reduction, because it provides shortened length of operation, avoidance of forceful manipulation and open reduction. -
Citations
Citations to this article as recorded by- Recent Trends in Treatment of Supracondylar Fracture of Distal Humerus in Children
Soon Chul Lee, Jong Sup Shim
Journal of the Korean Fracture Society.2012; 25(1): 82. CrossRef
- Recent Trends in Treatment of Supracondylar Fracture of Distal Humerus in Children
- 463 View
- 0 Download
- 1 Crossref

- Development and Accuracy Test of a Robot-arm Type Image-guided Surgery System for Percutaneous Screw Fixation of the Sacro-iliac Joint
- Jin Sup Yeom, Won Sik Choy, Hayong Kim, Jong Won Kang, Kwang Won Lee, Whoan Jeang Kim, Jae Hoon Ahn, Seong Kyu Park, Jong Hwa Won, Hyungmin Kim, Namkug Kim
- J Korean Fract Soc 2005;18(2):191-197. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.191
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To develop a robot-arm type image-guided surgery system for percuatneous screw fixation of the sacro-iliac joint and to evaluate its accuracy.
MATERIALS AND METHODS
We have developed an image-guided surgery system using a three-dimensional digitizer (Microscribe 3-D G2, Immersion, USA) and a personal computer. The registration error and target localization error at fiducial registration were measured 30 times for each using a phantom made with plastic pelvic bone model (Sawbones, USA). Sixteen 6.5 mm cannulated screws were inserted into four plastic bone models, and the accuracy was evaluated.
RESULTS
The target localization error was 1.46+/-0.47 mm while the registration error was 0.73+/-0.23 mm. All of the 16 screws were inserted well across the sacro-iliac joint, and there was neither cortical breach nor collision between screws or washers.
CONCLUSION
The accuracy of the developed system was similar to that of optical tracker-based navigation systems, and its helpfulness and usefulness was proven with simulation surgery using plastic bone models.
- 383 View
- 0 Download

- Treatment of Comminuted Femoral Shaft Fracture by Interlocking Intramedullary Nailing: Comparision of results between open reduction with cerclage wiring and closed reduction
- Jeung Tak Suh, Hyoung Lok Roh, Jeung Il Kim, Chong Il Yoo
- J Korean Fract Soc 2005;18(1):6-11. Published online January 31, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.1.6
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare of results between open interlocking intramedullary nailing combined with cerclage wiring and closed interlocking intramedullary nailing in treatment of femoral shaft comminuted fracture, we reviewed retrospectively 62 femoral shaft fractures.
MATERIALS AND METHODS
We reviewed retrospectively 62 femoral shaft comminuted fractures, who had been followed up for a minimum one year including Winquist-Hansen classification II, III, IV from January 1996 to December 2002. The group I include the patients who treated with closed interlocking intramedullary nailing. The group II include the patients who treated with open interlocking intramedullary nailing combined with cerclage wiring.
RESULTS
The average bone union time was 18.6 weeks in group I, 27.6 weeks in group II. The complication included 3 delayed unions, 1 nonunion and shortening of more than two centimeters in 1 patents in group I. In group II, The complication included 2 infections, 7 delayed unions and 3 nonunions.
CONCLUSION
We can use open interlocking intramedullary nailing with cerclage wiring in some femur shaft comminuted fractures, but there are many problems and complications. So we must consider it carefully before using this method.
- 369 View
- 0 Download

- Two-Stage Reconstruction of Infected Nonunion of Long Bones using Antibiotics-Impregnated Cement Beads
- Se Hyun Cho, Soon Taek Jeong, Hyung Bin Park, Sun Chul Hwang, Yong Chan Ha, In Hwan Hwang
- J Korean Fract Soc 2004;17(4):395-400. Published online October 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.4.395
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate treatment results between internal and external fixation groups in two-stage reconstruction of infected nonunion of long bones using antibiotics-impregnated cement beads.
MATERIALS AND METHODS
In the first stage, preexisting hardwares were removed and radical debridement was done. The dead space was filled with antibiotics -impregnated cement beads and the nonunion site was immobilized by external fixation, cast or skeletal traction. In the second stage, all cases were divided into two groups; the nonunion was fixed by internal fixation in group I versus external fixation in group II. The intervening period between the first and second stage was average 8.7 weeks (range, 3~23 weeks).
RESULTS
The follow-up period was average 45 months (range, 16~71 months). Infection control and bone union were achieved in all 13 cases of group I. Infection recurred in two of 28 cases in group II, one underwent above-knee amputation and the other case was lost in follow-up. The mean number of supportive operations including repeated curettage, augmentation and change of infected pins, angular correction, and soft tissue flap was average 2 and 6.2 times respectively in group I and group II. Bony union period was average 19.3 and 23.1 weeks in each group. According to Paley's classification, group I was similar to group II in bony and functional result (p>0.05).
CONCLUSION
Antibiotics-impregnated cement beads provided positive effect on infection control. Internal fixation group showed less number of additional operations and earlier bony union than external fixation group. -
Citations
Citations to this article as recorded by- Treatment of Infected Nonunion
Sang-Ho Ha
Journal of the Korean Fracture Society.2007; 20(2): 206. CrossRef
- Treatment of Infected Nonunion
- 534 View
- 0 Download
- 1 Crossref

- Treatment for Intractable Infected Nonunion of Lower Extremity in Elderly People using External Fixator
- Seung Jun Park, Jong Sup Shim, Sung Kee Shin
- J Korean Fract Soc 2004;17(2):177-183. Published online April 30, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.2.177
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To introduce and report the results of treatment of old patients' infected nonunion using external fixator.
MATERIALS AND METHODS
Nine patients more than 60 years old were included in the study. Four cases had combined medical problems of diabetes, hypertension, and vascular disorder. We used Ilizarov fixator in eight cases and uni-lateral external fixator in one. All patients were treated with debridement, broad sequestrectomy, segmental resection, bone graft and compression of fracture site about 1~1.5 cm. We evaluated the final results by functional result and complication according to the criteria of Paley.
RESULTS
Average length discrepancy was 1.7 cm before operation by initial bone loss and final follow-up shortening was average 2.6 cm. Mean duration of fixtor removal was 5.2 months. We acquired bony union lastly in 8 cases. Final functional result was 3 excellent, 2 good, 2 fair and 2 poor. Among them, 2 good, 1 fair and 1 poor cases had medical problem.
CONCLUSION
In old patients, compression of nonunion site and early joint motion using external fixator seemed to be very useful in the treatment of intractable infected nonunion of lower extremity and in minimizing duration of treatment. -
Citations
Citations to this article as recorded by- Manufacturing Techniques of Ancient Forged High-tin Bronze Wares from Archaeological Sites in Bagan, Myanmar
Jae Sung Lee, Yee Yee Win, Bonnie Lee, Jae Eun Yu
Journal of Conservation Science.2023; 39(5): 673. CrossRef - Treatment of Infected Nonunion
Sang-Ho Ha
Journal of the Korean Fracture Society.2007; 20(2): 206. CrossRef
- Manufacturing Techniques of Ancient Forged High-tin Bronze Wares from Archaeological Sites in Bagan, Myanmar
- 555 View
- 0 Download
- 2 Crossref

- Reduction of Pediatric Forearm Diaphyseal Fractures by Pin Leverage Technique
- Soo Hong Han, Duck Yun Cho, Hyung Ku Yoon, Byung Soon Kim, Sung Hoon Kang, Tae Hyung Kim
- J Korean Fract Soc 2004;17(1):59-63. Published online January 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.1.59
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Although the majority of children's forearm diaphyseal fractures may be treated conservatively with closed reduction and cast immobilization, unstable or irreducible fractures are usually treated by surgical management. Authors performed percutaneous pin leverage reduction technique for irreducible displaced diaphyseal fractures. The aim of this study is to determine the efficacy of pin leverage technique in pediatric forearm diaphyseal fractures MATERIALS AND METHODS: In this retrospective study, we reviewed 22 cases of forearm diaphyseal fractures reduced by percutaneous pin leverage technique between 1997 and 2002. We analyzed radiographs, operation time, hospital stay and immobilization period, range of motion, postoperative complications and functional results by Thomas.
RESULTS
Average length of follow up was 28 months with mean age of 10.5 years. All fractures in this series healed less than 2 degrees of diaphyseal angulation. Average operation time including anesthesia was 42 minutes and hospital stay was 4.6 days. Time to union was 49.6 days in average and range of motion and functional results were satisfactory in all cases except one case of congenital radioulnar synostosis. There was one case of superficial pin track infection as complication.
CONCLUSION
In operative treatment of children's diaphyseal fractures of forearm bones, percutaneous pin leverage reduction technique is a good alternative method prior to open reduction in case of difficult closed reduction. -
Citations
Citations to this article as recorded by- Pediatric Forearm Bone Fractures Treated with Flexible Intramedullary Nail
Suk Kyu Choo, Jin Hwan Kim, Hyung Keun Oh, Dong Hyun Kim
Journal of the Korean Fracture Society.2007; 20(2): 190. CrossRef
- Pediatric Forearm Bone Fractures Treated with Flexible Intramedullary Nail
- 547 View
- 2 Download
- 1 Crossref

- Screw breakage in tibial interlocking nailing
- Hyung Bin Park, Bun Jung Kang, Hae Ryong Song, Kyong Hoi Koo, Soon Taek Jeong, Se Hyun Cho
- J Korean Soc Fract 2002;15(4):483-488. Published online October 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.4.483
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aims of this study were to investigate the prevalence and the causes of screw breakage in tibia nailing.
MATERIALS AND METHODS
Between 1995 and 2000, eighty-two tibial diaphyseal fractures were treated with interlocking nails. The loss of follow-up was 7 cases. We retrospectively reviewed seventy-five cases. We investigated the rate and location of metal failure and evaluated the fracture pattern, the presence of distraction after nailing and union abnormality.
RESULTS
Screw breakage was identified in seven cases (9.3%) and most frequently occurred on the second proximal locking screw. Screw breakage occurred in AO type B or C type fractures, fracture site distraction after nailing, open fracture, delayed union and nonunion.
CONCLUSION
The main cause of screw breakage is unstable bone to bone contact on the fracture site caused by comminution or distraction. The open fracture, delayed union, and nonunion also contributing factors for screw breakage. For preventing screw breakage, it is necessary to avoid fracture site distraction and delay full weight bearing in cases having unstable fracture site contact. -
Citations
Citations to this article as recorded by- Clinical Outcomes of the Tibia Segmental Fractures Treated by Intramedullary Nail Using Various Reduction Techniques
Oog-Jin Shon, Ji-Hoon Shin, Chul-Wung Ha
Journal of the Korean Fracture Society.2013; 26(1): 50. CrossRef
- Clinical Outcomes of the Tibia Segmental Fractures Treated by Intramedullary Nail Using Various Reduction Techniques
- 568 View
- 1 Download
- 1 Crossref

- Nail Breakage after Femoral Interlocking Intramedullary Nailing
- Suk Kang, Phil Hyun Chung, Dong Ju Chae, Jong Pil Kim, Joon Han Kim, Sung Pock Park, Jae Sang Park
- J Korean Soc Fract 2002;15(3):363-370. Published online July 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.3.363
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We analyze the clinical causes and precautions of nail breakage followed by femoral intramedullary nailing MATERIALS AND METHODS: We reviewed 12 cases of nail breakage followed by the femoral intramedullary nailing from Jan. 1993 to Feb. 2001 and for each cases, we analyzed used nail diameter, patient weight and used nail, time to nail breakage and configuration of non-union. We classified fracture site at the time of trauma as proximal 1/3, middle 1/3, distal 1/3, and evaluated gap of fracture site, displacement of fragment after surgery, location and treatment of broken nail on each part, and analyzed the causes of nail breakage RESULTS: The average time of nail breakage was 8.1 months and distal 1/3 fracture were major as 6 cases. Those were mainly comminuted fracture of Winquist-Hansen type II. After surgery, gap of fracture site and displacement of fragment were mostly observed in middle 1/3 fracture and, in the part of middle 1/3, the site of nail breakage took place in fracture site. Especially in the distal 1/3 fracture, nail breakage happened usually in distal first locking screw hole. The causes of nail breakage were inadequately small diameter of nail inserted into the isthmic portion of medullary canal in proximal fracture, inaccurate reduction of fracture site in middle fracture, and the use of short length of nail and its mechanical damage caused by inaccurate insertion of distal locking screw in distal fracture.
CONCLUSION
To prevent nail breakage while femoral intramedullary nailing, in proximal fracture, adequate diameter of nail has to be inserted into the isthmic portion of medullary canal. In middle fracture, the accurate reduction of fracture site will be necessary, and the case of distal fracture, enough length of nail has to be used and especially it is important not to cause mechanical injury with the accurate insertion of distal locking screw in nail -
Citations
Citations to this article as recorded by- Comparison of our self-designed rotary self-locking intramedullary nail and interlocking intramedullary nail in the treatment of long bone fractures
Bailian Liu, Ying Xiong, Hong Deng, Shao Gu, Fu Jia, Qunhui Li, Daxing Wang, Xuewen Gan, Wei Liu
Journal of Orthopaedic Surgery and Research.2014;[Epub] CrossRef - Limited Open Reduction and Intramedullary Nailing of Proximal Femoral Shaft Fracture
Sang Ho Ha, Jun Young Lee, Sang Hong Lee, Sung Hwan Jo, Jae Cheul Yu
Journal of the Korean Fracture Society.2009; 22(4): 225. CrossRef
- Comparison of our self-designed rotary self-locking intramedullary nail and interlocking intramedullary nail in the treatment of long bone fractures
- 694 View
- 1 Download
- 2 Crossref

- The Evaluation of Clinical and Radiographic Prognostic Factors for the Surgically Treated Unstable Ankle Fractures
- Hong Geun Jung, Hee Kon Park, Moon Jib Yoo, Tai Won Kim
- J Korean Soc Fract 2002;15(2):216-225. Published online April 30, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.2.216
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to analyze the clinical and radiographic prognostic factors which may affect the postoperative clinical results of the unstable ankle fractures.
MATERIALS AND METHODS
This study is based on 75 unstable ankle fractures treated by open reduction and internal fixation from May 1994 to August 2000, with a minimum follow-up period of 12 months(range : 13 months-7 years 3 months). The 75 patients were average 40.5 years old with male: female ratio of 52:23. Based on Lauge-Hansen classification, the supination-external rotation type was the most common with 42 (56.0%) cases. The clinical results was assessed by American Orthopaedic Foot and Ankle Society(AOFAS) functional scale. The sex, age, side of injury, body weight, trauma-operation interval, operation time, cause of injury as the possible postoperative clinical prognostic factors and fracture type, anatomical reduction of fracture, preoperative medial clear space, postoperative medial clear space, talo-crural angle, talar tilt, tibio-fibular clear space, tibio-fibular overlap space as the possible radiographic prognostic factor were statistically analyzed RESULT: Postoperative AOFAS functional scale was average 81.0 points with 23(30.7%) cases excellent, 17(22.7%) good, 18(24.0%) fair and 17(22.7%) cases poor results. The age, the operation time(p<0.001) and the anatomical reduction of fracture(p<0.005) were found to be statistically significant factors affecting the prognosis. The other clinical and radiographic factors did not significantly affect the clinical results.
CONCLUSION
The surgically treated unstable ankle fractures in patients whose age was above 41 years old or operation time exceeding 90 minutes or unsatisfied anatomical reduction of fractures showed significantly poor clinical results. -
Citations
Citations to this article as recorded by- Analysis of Bone Mineral Density of Ankle Fracture Patients
Tae Hyung Kim, Jae Hyung Lee, Seung-Hwan Park
Journal of the Korean Orthopaedic Association.2021; 56(4): 334. CrossRef
- Analysis of Bone Mineral Density of Ankle Fracture Patients
- 575 View
- 1 Download
- 1 Crossref

- Limb Salvage versus Early Amputation according to Mangled Extremity Severity Score in Treatment of the Lower Extremity Open Fractures associated with Severe Soft Tissue Injury
- Kyung Jin Song, Yong Min Kim, Kyung Rae Lee
- J Korean Soc Fract 2002;15(1):28-35. Published online January 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.1.28
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the availability of the mangled extremity severity score(MESS) in deciding the early treatment modality for the patients with open lower extremity fractures and severe soft tissue injury.
MATERIALS AND METHODS
Analyzed 27 patients for the lower extremity open fractures with extensive soft tissue injury. A comparative study using a MESS, a cause of injury, vascular injury and a fracture pattern, average hospital stay and average hospital charges were analyzed, and daily living ability and subjective self-evaluation were assessed.
RESULTS
There was statistically significant correlation applying MESS to patient group that had been operated by early amputation because of severe soft tissue and vascular injury. But there was no significant difference in the subjective self-assessment score, admission period and total cost during admission between each treatment method.
CONCLUSION
MESS can be used as an objective assessment criteria in deciding the proper treatment modality for the cases of lower limbs fracture with extensive soft tissues and vascular injury.
- 379 View
- 0 Download

- Intraarticular Soft Tissue Injuries in Fractures of the Distal Radius: A Descriptive Arthroscopic Study
- Seok Beom Lee, Chang Beom Lee
- J Korean Soc Fract 2001;14(4):726-732. Published online October 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.4.726
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of this study was to determine prevalence of the associated intraarticular soft tissue lesions with fractures of the distal radius by arthroscopic evaluation of the wrist joint and thus to avoid poor outcome after the conventional treatment. MATERIAL AND METHOD: Medical records, radiographs and arthroscopic findings of 27 patients with fractures of the distal radius that underwent arthroscopic procedures were reviewed . Relationships between fracture pattern and associated lesions of the triangular fibrocartilage complex (TFCC), scapholunate and lunotriquetral ligaments were investigated.
RESULTS
71% of fractures of the distal radius were associated with soft tissue lesions. Among those, tear of the triangular fibrocartilage complex was the most prevalent (47%). Associated lesions such as TFCC, scapholaunate and lunotriquetral lesion were more common with inraarticular fracture, while severe nature of the lesion that neccessiated pinning and/or arthroscopic repair was more common with extraarticular fractures of the distal radius.
CONCLUSION
Incidence of the associated soft tissue lesions in this study were comparably high with the latest publications. The authors suggest strongly that wrist arthroscopy should accompay any procedure for fractures of the distal radius, if it is to be done under anesthetic control, to get more favorable outcome. -
Citations
Citations to this article as recorded by- Arthroscopic Repair for Traumatic Peripheral Tear of Triangular Fibrocartilage Complex
Seung-Ju Jeon, Chan-Sam Moon, Ho-Seung Jeon, Haeng-Kee Noh, Sung-Hwan Kim
Journal of the Korean Fracture Society.2007; 20(4): 330. CrossRef
- Arthroscopic Repair for Traumatic Peripheral Tear of Triangular Fibrocartilage Complex
- 474 View
- 0 Download
- 1 Crossref

- The Effects of aging process on fracture healing in rat callus
- Sang Ho Song, Young Hee Choi, Shim Chang Gu, Sang Ho Yoo, Young Euy Park
- J Korean Soc Fract 2001;14(2):135-144. Published online April 30, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.2.135
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Patient age significantly influences the rate of fracture healing. The rate of healing declines with increasing age. The authors compared the aging effect on fracture healing in the callus of rat femur by the light microscopy.
MATERIALS AND METHODS
In this study the unilateral, closed fractures were created in the femur of 18 Sprague-Dawley rats. The rats were killed in three age group(8 weeks:7, 32weeks:6, 70weeks:5) at 2 weeks after fracture. The composition of fracture callus(new bone, cartilage, mesenchymal layer) was measured by image analyzer with H-E stain. Immunohistochemical stain (PCNA, TUNEL, TRAP) positive cells were counted for the comparing of cellular activity according to the aging.
RESULTS
The percent of intramembranous new bone in the younger rat(8 week:22.32%) was higher than the older ones(30 week:7.09%, 70 week:5.37%). The percent of PCNA positive osteoblast in the newbone decreased according to the aging(8 week:64.25%, 30 week:57.40%, 70 week:29.54%). The number of osteoclast in the osteochondral junction at the 8 week(43) was more than that of 30 week(25.57) and 72 week(29.87). The number of TRAP positive osteoclast was not different as aging, but the number of osteoclast in the osteochondral junction(5.89) was more than that in the metapyseal area(2.08).
CONCLUSIONS
More new bone was found in younger rat. There was a strong correlation (p<0.05) between age and PCNA activity. More number of active osteoblast and osteoclast was found in younger rat femoral fracture callus, which indicated rapid fracture healing in younger age.
- 393 View
- 1 Download

- Two-Stage Treatment of Infected Nonunion of the Tibia using Antibiotics Impregnated Cement Beads and External Fixator
- Yeon Cheon Jeong
- J Korean Soc Fract 2000;13(4):884-890. Published online October 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.4.884
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the results of two-stage treatment for infected nonunion of the tibia using antibiotics impregnated cement beads(AICB) and external skeletal fixation.
MATERIALS AND METHODS
We analyzed 25 infected tibial nonuinon that were treated with AICB and external skeletal fixation from July 1995 to April 1998. The average follow-up was 25 months. In the first stage, sequestrectomy and radical debridement was performed. and then the soft tissue and bony defects were filled with AICB and was stabilized with external skeletal fixation. In the second stage, after removal of AICB and the nonunion site was either grafted with autogenous cancellous bone graft(17 patients) or internal bone transport(8 patients) was performed according to the bone defect size.
RESULTS
The average bony union time was 36.8 weeks. The intervening time between the first and second stages of treatment was 4 to 6 weeks (average 5.4 weeks). There were 8 pin tract infections, 1 Postoperative infection after the second-stage bone grafting. According to Paley's functional assessment system, excellent or good results were obtained in 20 cases. There was no poor result.
CONCLUSION
In our opinion, the above advocated two-stage treatment is an acceptable treatment modality for the management of infected tibial nonunion.
- 381 View
- 0 Download

- Two Stage Treatment of Infected Nonunion of Femur with Antibiotics Impregnated Cement Beads and External Fixator
- Hyung Bin Park, Yeon Chen Jung, Hae Ryong Song
- J Korean Soc Fract 2000;13(4):817-824. Published online October 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.4.817
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to find out the treatment efficiency of two stage osteosynthesis with antibiotic cement beads and external skeletal fixation for infected nonunion of femur.
MATERIALS AND METHODS
In the first stage, radical debridement was performed. The soft tissue and bony defects were filled with antibiotics impregnated cement beads and the nonunion site was stabilized with external skeletal fixation. In the second stage, the debrided nonunion site was repaired with bone grafting. The intervening time between the first and second stages of treatment was 4 to 6 weeks (average 5.4 weeks). The bone defects ranged from 0.5 to 14cm, Autogeneous iliac cancellous bone grafting was performed in 17 patients and microvascularized fibular graft was performed in 5 patients.
RESULTS
The follow-up period was average 45 months (range, 27-62 months). Infection control and bone union were achieved in all 22 cases. Postoperative infection after the second-staged bone grafting occurred in one patient. This recurred case was treated with repeated two staged operation. Even though aggressive physical theraphy was done, all patients had relevant knee flexion deficits. 14 patients were achieved more than 100 degrees of knee flexion, but 8 patients had less than 80 degrees of range of motion.
CONCLUSION
We have found that two-stage treatment with antibiotic beads local therapy, external skeletal fixation, and staged bone grafting is an acceptable treatment modality for the management of infected femoral nonunion. It results in rapid recovery from osteomyelitis and a predictable recovery from nonunion.
- 311 View
- 1 Download

Case Report
- Segmental Breakage of Distal Interlocking Screw Complicating removal of broken nail: A Case Report
- Kyu Hyun Yang, Seong Jin Park, Hyung Jung Kim
- J Korean Soc Fract 2000;13(4):709-712. Published online October 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.4.709
-
 Abstract
Abstract
 PDF
PDF - Metal failure (nail breakage) after locked intramedullary nailing results from delayed union or nonunion, which necessitates removal of nail and interlocking screws. Breakage of interlocking screw(s) can be associated with failure of the intramedullary nail. It usually breaks into two parts. Proximal part, which contains the screw head, can be removed by screwdriver without difficulties. Distal part can be removed from the far cortex or be left in place if it does not hinder further procedures. We experienced a case of segmental breakage of distal interlocking screw, which was associated with failure of the femoral nail and nonunion. Middle part of the broken screw obstructed the hollow of the nail and complicated the removal of the broken nail.
- 387 View
- 2 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


