Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(3); 2020 > Article
- Review Article Current Concepts in the Articular Cartilage Repair
- Eui Dong Yeo, Whi Je Cho, Young Koo Lee
-
Journal of Musculoskeletal Trauma 2020;33(3):164-170.
DOI: https://doi.org/10.12671/jkfs.2020.33.3.164
Published online: July 31, 2020
2Department of Orthopedic Surgery, Soonchunhyang University Hospital Bucheon, Bucheon, Korea
- 763 Views
- 2 Download
- 0 Crossref
- 0 Scopus
Abstract
Articular cartilage defects are common in orthopedic practice. Most clinical and research efforts focus on restoring the damaged cartilage in connection with osteoarthritis or trauma. This article explains the current clinical approaches for repairing cartilage, as well as the research approaches and those under translation into clinical practice. Tissue engineering techniques are being employed with aims of repopulating a cartilage defect with hyaline cartilage containing living chondrocytes with hopes of improving the clinical outcomes. Cartilage tissue engineering involves the cell source, biomaterial and membranes, and growth stimulators. Tissue engineering is being applied to clinical medicine by autologous chondrocyte implantation or similar techniques. While basic science has refined orthopedic treatment of chondral lesions, available evidence does not conclude the superiority of tissue engineering methods over other techniques in improving the clinical symptoms or restoring the native joint mechanics.
Published online Jul 24, 2020.
https://doi.org/10.12671/jkfs.2020.33.3.164
Current Concepts in the Articular Cartilage Repair
Abstract
Articular cartilage defects are common in orthopedic practice. Most clinical and research efforts focus on restoring the damaged cartilage in connection with osteoarthritis or trauma. This article explains the current clinical approaches for repairing cartilage, as well as the research approaches and those under translation into clinical practice. Tissue engineering techniques are being employed with aims of repopulating a cartilage defect with hyaline cartilage containing living chondrocytes with hopes of improving the clinical outcomes. Cartilage tissue engineering involves the cell source, biomaterial and membranes, and growth stimulators. Tissue engineering is being applied to clinical medicine by autologous chondrocyte implantation or similar techniques. While basic science has refined orthopedic treatment of chondral lesions, available evidence does not conclude the superiority of tissue engineering methods over other techniques in improving the clinical symptoms or restoring the native joint mechanics.
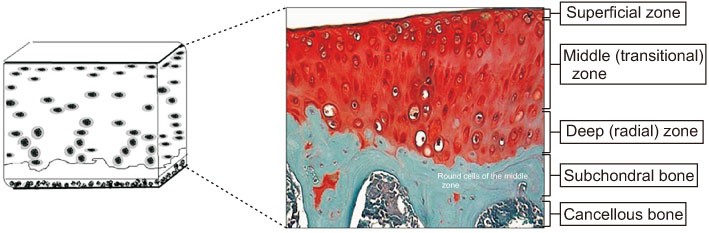
Fig. 1
Articular cartilage.
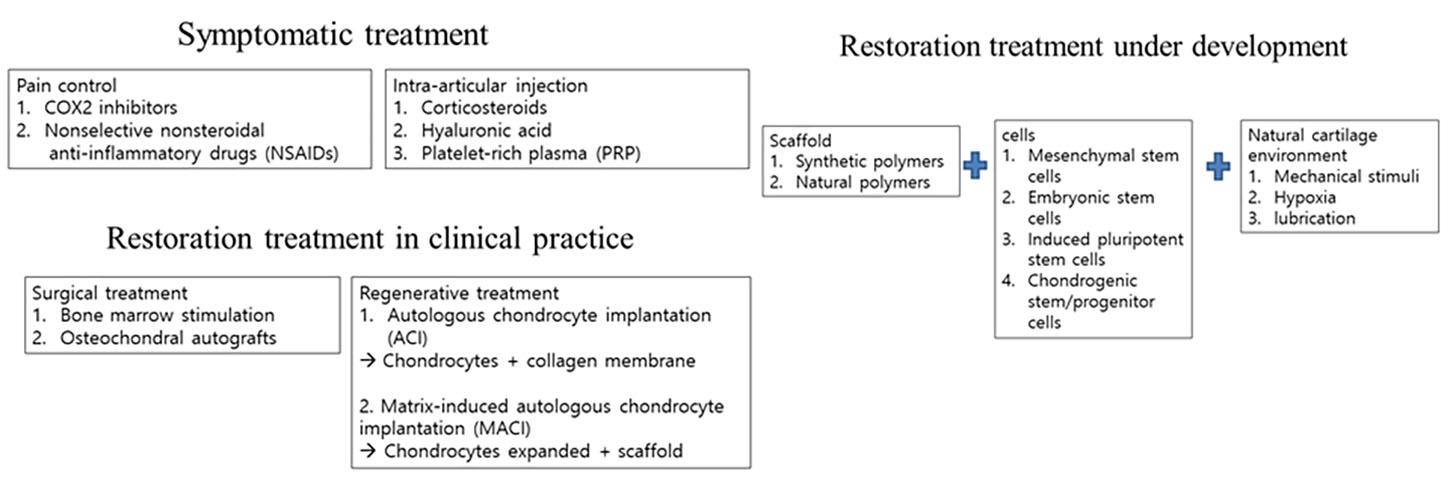
Fig. 2
Approaches to the restoration of cartilage.
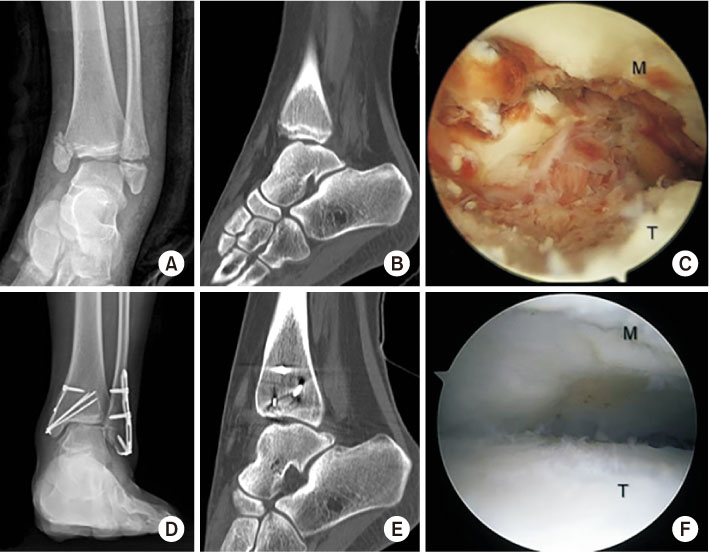
Fig. 3
Female, 12 years old, injured bimalleolar fracture and large osteochondral lesion of the talus on anteromedial talar dome. (A) Preoperative anteroposterior radiography. (B) Preoperative computed tomography (CT). (C) Intraoperative arthroscopy showed traumatic large osteochondral lesion of the talus. (D) Postoperative 8-month anteroposterior radiography. (E) Postoperative 8-month CT. (F) Postoperative 8-month second look arthroscopy showed a well-healed osteochondral lesion of the talus. M: medial malleolus, T: talus.
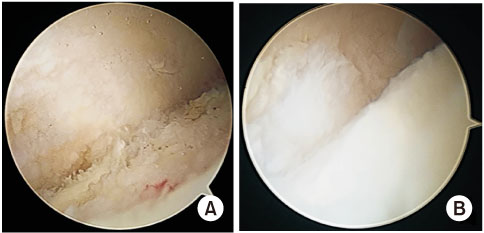
Fig. 4
Preoperative and postoperative photos of the patient undergoing microfracture for an osteochondral lesion of the talus. (A) Preoperative photo. (B) Postoperative photo.
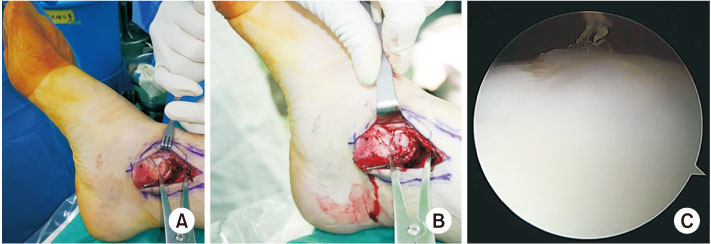
Fig. 5
Intraoperative and postoperative photographs of the osteochondral lesion with a talus cyst undergoing osteochondral autograft transplantation. (A) Photograph of osteochondral lesion of talus identification during operation. (B) Photograph of inserting a cylindrical plug during operation. (C) Arthroscopic photograph when removing metal implants.
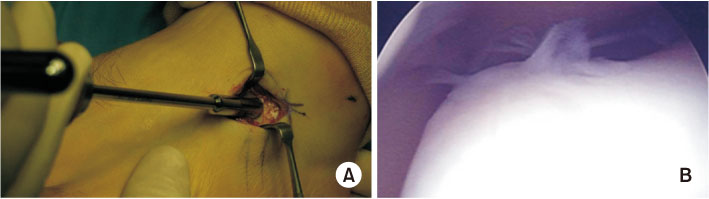
Fig. 6
Autologous chondrocyte implantation (ACI) operation. (A) Cartilage harvesting from the anterior process of the calcaneus. (B) Complete repair and filling of the defect, complete integration to the border zone when performing 2nd look arthroscopy after ACI of osteochondral lesion of the talus.
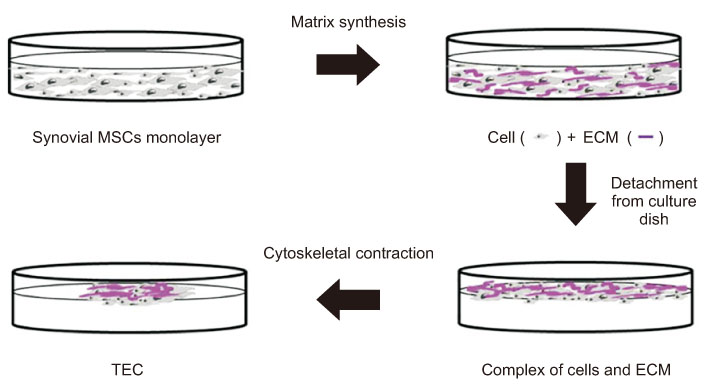
Fig. 7
Schematic representation of tissueengineered construct (TEC) development.
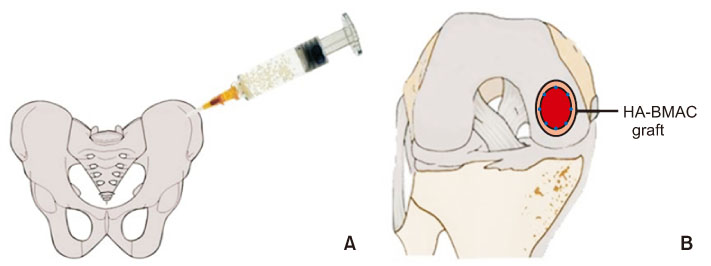
Fig. 8
Cartilage repair in the knee with a hyaluronic acid-based scaffold embedded with bone marrow aspirate concentrate (HA-BMAC). (A) Bone marrow aspirate. (B) HA-BMAC implanted into the chondral defect.
Financial support:None.
Conflict of interests:None.
References
-
Lee KT, Choi YS, Lee YK, Cha SD, Koo HM. Comparison of MRI and arthroscopy after autologous chondrocyte implantation in patients with osteochondral lesion of the talus. Orthopedics. 2011 [doi: 10.3928/01477447-20110627-10][epub].
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

