Search
- Page Path
- HOME > Search
Original Article
- Association between decreased bone mineral density and Pauwels angle in femoral neck fractures: a cross-sectional study
- Soo-Hwan Jung, Yong-Uk Kwon, Ji-Hun Park
- J Musculoskelet Trauma 2026;39(1):20-29. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00269
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
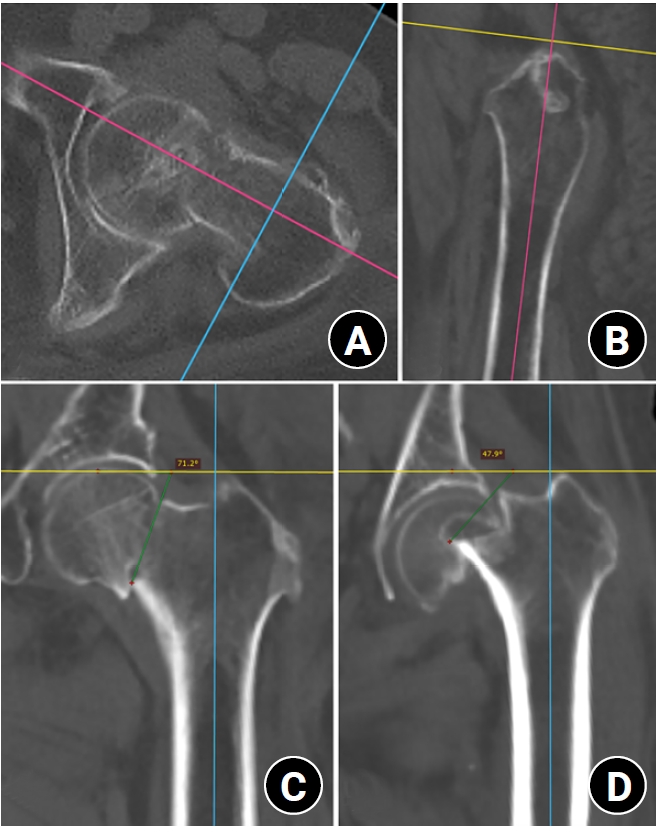
Progressive osteoporosis reduces the trabecular structures of the proximal femur, whereas the primary compression trabeculae (PCTs) are relatively preserved. We hypothesize that the loss of the vertically oriented PCTs in osteoporosis, which act as a mechanical barrier, affects fracture line propagation and influences the Pauwels angle. This study investigated the association between bone mineral density (BMD) and Pauwels angles in low-energy femoral neck fractures (FNFs).
Methods
This cross-sectional study included 150 patients (mean age, 75.3 years; range, 50–94 years) diagnosed with intracapsular FNFs between May 2019 and May 2023. BMD was measured within 1 month of the injury date using dual-energy X-ray absorptiometry, and modified Pauwels angles were assessed using a computed tomography-based multiplanar reconstruction program. Multiple linear regression analysis was performed to evaluate the factors influencing the Pauwels angles. The dependent variable was the Pauwels angle, while the independent variables included sex, age, height, body weight, body mass index, American Society of Anesthesiologists score, Charlson comorbidity index score, smoking status, alcohol use, preinjury walking ability, and femoral neck BMD T-scores.
Results
Higher femoral neck BMD T-scores were significantly associated with increased Pauwels angles (β=3.449, P<0.001). Greater body weight was independently associated with increased Pauwels angles (β=0.213, P=0.007).
Conclusions
The Pauwels angle demonstrated a significant association with BMD, with lower BMD associated with less steep Pauwels angles. In the absence of BMD measurement, the Pauwels angle may indicate osteoporosis severity in patients with low-energy FNFs. Level of evidence: III.
- 114 View
- 3 Download

Review Article
- Osteoporotic Hip Fracture: How We Make Better Results?
- Byung-Chan Choi, Kyung-Jae Lee
- J Korean Fract Soc 2024;37(1):52-59. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.52
-
 Abstract
Abstract
 PDF
PDF - The prevalence of osteoporosis and incidence of osteoporotic fractures is increasing gradually as life expectancy is prolonged and the aged population increases. Osteoporotic hip fractures (femoral neck fractures and femoral intertrochanteric fractures) have high mortality because the patients with these fractures are elderly and have several comorbidities. Thorough preparation and a multidisciplinary approach in the preoperative period are critical, and early surgery is recommended. There are also several principles to treat osteoporotic hip fractures and prevent fixation failures. Many studies have suggested various treatment methods for femoral neck fractures and femoral intertrochanteric fractures. Functional recovery treatment is essential based on the patient’s health and activity levels. Finally, aggressive management of osteoporosis and the prevention of falling is needed to treat osteoporotic hip fractures successfully.
- 630 View
- 24 Download

Original Article
- Short-term Treatment Comparison of Teriparatide and Percutaneous Vertebroplasty in Patients with Acute Osteoporotic Vertebral Compression Fractures
- Joonoh Seo, Ki Youn Kwon, Bumseok Lee, Hoon-Sang Sohn
- J Korean Fract Soc 2024;37(1):15-21. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.15
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the 3-month treatment effects of teriparatide and percutaneous vertebroplasty for acute osteoporotic vertebral compression fractures.
Materials and Methods
A retrospective study was conducted on 76 patients diagnosed with acute osteoporotic vertebral compression fractures from January 1, 2020 to December 31, 2022. The patients were divided into the teriparatide group and the percutaneous vertebroplasty+alendronate group. The visual analog scale (VAS), Oswestry disability index (ODI), and height of the vertebrae anterior wall were measured before treatment and at 1 and 3 months after treatment.
Results
Of the 76 patients, 42 were treated with teriparatide, and 34 were treated with percutaneous vertebroplasty. The symptoms improved in both groups, with a decrease in the VAS and ODI scores at 1 and 3 months after treatment, respectively. On the other hand, there was no significant difference in the VAS, ODI score, and anterior vertebral body height between the two groups before treatment and at 1 and 3 months after treatment.
Conclusion
In the treatment of acute osteoporotic vertebral compression fractures, conservative treatment using teriparatide showed similar short-term (3 months) treatment results to percutaneous vertebroplasty in terms of improvement in back pain and function and degree of reduction in anterior vertebral body height.
- 976 View
- 32 Download

Review Article
- Fragility Fractures of the Pelvis and Sacrum
- Se-Won Lee, Ju-Yeong Kim
- J Korean Fract Soc 2023;36(1):29-38. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.29
-
 Abstract
Abstract
 PDF
PDF - The incidence of fragility fractures of the pelvis (FFP) has increased significantly due to the aging popu-lation and improved diagnostic modalities. The evaluation and treatment of these patients differ from that of high-energy pelvic ring injuries typically seen in younger patients. Therefore, it is important to classify the FFP by patterns of the classification system to standardize optimal treatment criteria and appropriate treatment strategy. However, some cases are not classifiable according to the FFP classifi-cation. A newly proposed classification that can be verified by comparing existing FFP classifications is needed to overcome the weak points. Non-operative treatment is usually considered first and should focus on early mobilization. Operative fixation should focus on stabilizing the minimally invasive pelvic ring than the reduction of fractures to facilitate early mobilization and avoid complications that can arise from comorbidities associated with immobility.
- 1,850 View
- 33 Download

Original Article
- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
- J Korean Fract Soc 2022;35(4):151-161. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.151
-
 Abstract
Abstract
 PDF
PDF - Purpose
Osteoporosis causes various fixation failures in patients with intertrochanteric fractures. This study aimed to investigate the effect of a demineralized bone matrix (DBM) for cancellous or cortical bone defects on internal fixation in older osteoporotic patients with intertrochanteric fractures.
Materials and Methods
Among patients with intertrochanteric fractures who underwent surgical treatment from January 2016 to December 2021 at a facility, 171 patients were AO/OTA type 31-A1 and type 2 fractures which are considered relatively stable. The patients were grouped based on DBM use (Group A: DBM use, Group B: DBM non-use), and their clinical and radiology results were analyzed retrospectively. The patients were then subdivided into Group A-a and -b after removing factors that could cause treatment failures, such as the reduction status and location of the helical blade, and then further subdivided (Group A-a-1/2/3/4 and Group B-b-1/2/3/4) according to cancellous or cortical bone defects that could accompany intertrochanteric fractures. The time to full weight-bearing (FWB) and Harris hip score (HSS) 3 months after surgery in these subgroups were investigated.
Results
There was no significant difference in the clinical radiology results and complications between Group A and Group B. However, the time to FWB (p<0.001) and HSS (p=0.029) were significantly superior in Group A. In Group A-a with DBM use, after removing the risk factors for intertrochanteric fracture failure, the time to FWB (p=0.055) was close to the significance level, and HSS (p=0.036) was significantly superior. In Group A-a-1 (cancellous defect only) and Group A-a-3 (cancellous and cortical defect), the time to FWB (p=0.088, 0.052) was close to the significance level, and the HSS (p=0.039, 0.018) was significantly superior when DBM was used.
Conclusion
In patients with intertrochanteric fractures of AO/OTA type 31-A2.3 or less, if stable reduction and firm fixation are achieved, selective DBM use may help early recovery after surgery.
- 454 View
- 2 Download

Case Report
- Insufficiency Fracture of Simultaneously Bilateral Femur Neck in Patient Treated with Long-Term Bisphosphonate Treatment - A Case Report -
- Seong Kee Shin, Hyung Gon Ryu, Dae Won Shin, Beom Su Han
- J Korean Fract Soc 2022;35(3):109-113. Published online July 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.3.109
-
 Abstract
Abstract
 PDF
PDF - Bisphosphonate is used widely for osteoporosis management. On the other hand, some studies have reported that prolonged use of bisphosphonate without a proper resting period can cause insufficiency fracture and, in rare cases, fractures on the femur neck. This paper reports a case of an elderly patient who suffered bilateral femur neck insufficiency fractures induced by non-stopped long-term bisphosphonate therapy. The patient complained of pain in her buttocks at the first visit. During the admission period, inguinal area pain newly developed. Both a femur neck insufficiency fracture was observed on the hip radiographic image. Hip pinning and postoperative parathyroid hormone treatment were performed. The patient was discharged without specific complications and reported improvement in symptoms on the last follow-up. Several authors have reported one-sided femoral neck insufficiency fractures due to bisphosphonate use, but the present case is uncommon in that it occurred simultaneously in both femur necks. In addition, in the case of bilateral femur fractures, the walking ability after surgery is lower than that of one-sided fracture cases, so active rehabilitation is necessary.
- 539 View
- 2 Download

Review Articles
- Romosozumab: A Novel Agent in the Management of Osteoporosis
- Nam Hoon Moon, Won Chul Shin, Jae Hoon Jang
- J Korean Fract Soc 2021;34(4):148-153. Published online October 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.4.148
-
 Abstract
Abstract
 PDF
PDF - With the discovery of screlostin as a pivotal player in bone metabolism, a novel medication targeting sclerostin has been introduced. Romosozumab, a humanized anti-sclerostin monoclonal antibody, is a unique approach to the treatment of osteoporosis that inhibits sclerostin, a key regulator that has the dual properties of promoting bone formation and inhibiting bone resorption. Romosozumab has been shown to be superior to conventional agents, in increasing bone mineral density and preventing osteoporotic fractures. Romosozumab may also be effective in the management of treatment-resistant osteoporosis and in the prevention of osteoporotic fractures in the very high risk population. However, further studies are necessary as there is insufficient data on its clinical efficacy and safety.
-
Citations
Citations to this article as recorded by- The 2024 Guidelines for Osteoporosis - Korean Society of Menopause: Part II
Dong Ock Lee, Yeon Hee Hong, Moon Kyoung Cho, Young Sik Choi, Sungwook Chun, Youn-Jee Chung, Seung Hwa Hong, Kyu Ri Hwang, Jinju Kim, Hoon Kim, Dong-Yun Lee, Sa Ra Lee, Hyun-Tae Park, Seok Kyo Seo, Jung-Ho Shin, Jae Yen Song, Kyong Wook Yi, Haerin Paik, J
Journal of Menopausal Medicine.2024; 30(2): 55. CrossRef
- The 2024 Guidelines for Osteoporosis - Korean Society of Menopause: Part II
- 1,014 View
- 7 Download
- 1 Crossref

- Denosumab (RANKL Inhibitor): A Potent Anti-Resorptive Agent
- Seong-Eun Byun
- J Korean Fract Soc 2021;34(4):142-147. Published online October 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.4.142
-
 Abstract
Abstract
 PDF
PDF - Denosumab, a fully human monoclonal antibody to the receptor activator of nuclear factor-kappa B ligand, was introduced and used as an anti-osteoporotic agent. Denosumab prevents bone resorption by inhibiting the differentiation and action of osteoclasts, resulting in an increase of bone mineral density and broad-spectrum anti-fracture efficacy. Clinical studies, including FREEDOM (Fracture Reduction Evaluation of Denosumab in Osteoporosis Every Six Months) and its extension up to 10 years, FREEDOM Extension, demonstrated its long-term efficacy and safety in postmenopausal osteoporosis. In addition, the efficacy and safety of denosumab were confirmed in male osteoporosis and glucocorticoid- induced osteoporosis. Therefore, recent clinical guidelines recommend denosumab as an initial treatment. This review summarizes the mechanism of action, pharmacological characteristics, efficacy, and safety issue of denosumab.
- 841 View
- 5 Download

- Current Concepts of Vitamin D and Calcium in the Healing of Fractures
- Jihyo Hwang
- J Korean Fract Soc 2021;34(3):117-121. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.117
-
 Abstract
Abstract
 PDF
PDF - Fragile fractures, also known as osteoporosis fractures, insufficiency fractures, and senile fractures are a significant problem encountered by orthopedic surgeons. Calcium and vitamin D are essential for maintaining bone health and deficiencies in calcium and vitamin D are major risk factors for the development of osteoporosis. Sufficient amounts of calcium are also required for fracture-callus mineralization. Hence, compromised bone repair that is frequently observed in osteoporotic patients might be attributed to calcium and vitamin D deficiencies. Consequently, calcium and vitamin D supplementation represents a potential strategy for treating compromised fracture healing in osteoporotic patients. There is some clinical evidence of the positive effect of supplementation in fracture healing and posttraumatic bone turnover, but research in this area is ongoing. Calcium and vitamin D should be the primary treatment of choice in osteopenic patients with an insufficiency of calcium and vitamin D and for the prevention of secondary osteoporotic fractures. Calcium and vitamin D can also be used as addition to other primary osteoporotic medications such as antiresorptive or bone-forming agents. The role of calcium and vitamin D in fracture healing and the therapeutic potential of calcium and vitamin D supplementation is summarized in this context.
- 6,791 View
- 81 Download

Case Report
- Ulnar Insufficiency Fractures in Patients on Prolonged Bisphosphonate Therapy: A Case Report
- Kyu Min Kong, Yong Uk Kwon, Young Kyung Min, Doo Yeol Kim
- J Korean Fract Soc 2019;32(3):143-147. Published online July 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.3.143
-
 Abstract
Abstract
 PDF
PDF - Atypical fractures associated with prolonged bisphosphonate (BP) therapy rarely occur outside the femur, and the diagnostic criteria, appropriate treatment principles, and fixation methods for atypical ulnar fractures have not been established. The authors experienced the use of internal fixation with a metal plate and a new internal fixation method with an intramedullary nail in the treatment of an atypical ulnar fracture in a patient who had been on BP therapy for 10 to 20 years. This paper reports findings along with a review of the relevant literature.
-
Citations
Citations to this article as recorded by- Treatment of Atypical Ulnar Fracture Associated with Bisphosphonate Therapy: A Case Report
Dong-Soo Kim, Ji-Kang Park, Eui-Sung Choi, Ho-Seung Jeong, Seok-Hyun Hong, Byung-Hyun Ahn
Journal of the Korean Fracture Society.2020; 33(2): 101. CrossRef
- Treatment of Atypical Ulnar Fracture Associated with Bisphosphonate Therapy: A Case Report
- 828 View
- 1 Download
- 1 Crossref

Original Article
- Radiologic and Serologic Factors Associated with Bone Union at Femoral Atypical Fracture
- Suc Hyun Kweon, Byung Min Yoo
- J Korean Fract Soc 2019;32(1):27-34. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.27
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to investigate the radiologic and serologic factors related to postoperative union using intramedullary (IM) internal fixation in atypical femoral fractures (AFF), which are closely related to bisphosphonates (BPs) for osteoporosis.
MATERIALS AND METHODS
From February 2008 to December 2016, 65 patients (71 cases) who had undergone IM nail fixation after diagnosis of AFF were enrolled in this study. Patients were divided into group A, who experienced union within 6 months and group B, who did not experience union within 6 months. They were evaluated for duration of BPs use, radiologic factors and serological factors.
RESULTS
The mean duration of BPs use was 6.17 years in group A and 8.24 years in group B (p=0.039). In the subtrochanteric area, there were 14 cases (27.5%) in group A and 14 cases (70.0%) in group B. In the femoral shaft, there were 37 cases (72.5%) in group A and 6 cases (30.0%) in group B (p=0.001). On the preoperative, the flexion in the coronal plane was 5.9° (2.1°–9.2°) in group A and 8.0° (3.1°–12.1°) in group B (p=0.041). On the postoperative, conversion to valgus was 15 cases (29.4%), 8 cases (40.0%); conversion to neutral was 34 cases (66.7%) and 8 cases (40.0%); conversion to varus was 2 cases (3.9%) and 4 cases (20.0%), each (p=0.037). The fracture site gap was 1.5 mm (0–2.9 mm) on the front side and 1.2 mm (0–2.2 mm) on lateral side and 2.2 mm (0.9–4.7 mm) and 1.9 mm (0.5–3.5 mm), each (p=0.042, p=0.049). Among serological factors, there was no significant difference between the two groups.
CONCLUSION
Factors adversely affecting the union should be recognized before surgery, such as longterm BPs use or a severe degree of bending of the femur in the coronal plane. During surgery, proper reduction and spacing of the fracture site on the coronal plane should allow adequate reduction of the anterior and posterior surfaces. Obtaining anatomic reduction would be most beneficial for union, but if that is not possible, obtaining congenital valgus rather than varus on the coronal plane may be helpful for union. -
Citations
Citations to this article as recorded by- Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
Gyu Min Kong
Journal of the Korean Fracture Society.2019; 32(2): 107. CrossRef
- Subtrochanteric Fracture Reduction during Intramedullary Nailing: Technical Note
- 836 View
- 1 Download
- 1 Crossref

Review Articles
- Medical Treatment of Osteoporosis/Prevention of Falls
- Hyoung Keun Oh
- J Korean Fract Soc 2018;31(4):165-171. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.165
-
 Abstract
Abstract
 PDF
PDF - The prevention and treatment of fragility fractures is evolving continuously. Adequate fracture care should involve treating the fracture itself as well as the underlying bone disease. Although effective treatments of osteoporosis are available, a large proportion of patients with fragility fractures are not prescribed anti-osteoporotic medications after their injury. Recent advances in diagnostic tools and medications allow for a more effective and comprehensive treatment of fragility fractures.
-
Citations
Citations to this article as recorded by- Risk Factors for Falls or Fractures in Stroke Patients: An Analysis of 2020 Patient Sample Data
Miso Lee, Mikyung Moon
The Korean Journal of Rehabilitation Nursing.2024; 27(1): 58. CrossRef - Synthesis of Niobium η-Carbide Nb3(Fe,Al)3C by Mechanical Alloying in a Liquid Organic Medium
M. A. Eryomina, S. F. Lomayeva
Журнал физической химии.2023; 97(5): 680. CrossRef - The Effect of Denosumab in Elderly Patients Regarding Bone Density and Fracture Risk
Sung-Hyun Yoon, Karam Kim, Ki-Choul Kim
Journal of Bone Metabolism.2023; 30(3): 275. CrossRef - Trends of Nursing Research on Accidental Falls: A Topic Modeling Analysis
Yeji Seo, Kyunghee Kim, Ji-Su Kim
International Journal of Environmental Research and Public Health.2021; 18(8): 3963. CrossRef - Review on Korean Herbal Medicine Complex Prescriptions and Single Herbal Medicines for Osteoporosis : Focused on Domestic Research Published Since 2013
Jung Min Lee, Nam Hoon Kim, Eun-Jung Lee
Journal of Physiology & Pathology in Korean Medicine.2021; 35(3): 87. CrossRef
- Risk Factors for Falls or Fractures in Stroke Patients: An Analysis of 2020 Patient Sample Data
- 558 View
- 7 Download
- 5 Crossref

- Atypical Femoral Fractures: What Do We Know about Them?
- Beom Seok Lee, Young Kyun Lee, Heejae Won, Hyungkook Kim, Kyung Hoi Koo
- J Korean Fract Soc 2018;31(4):159-164. Published online October 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.4.159
-
 Abstract
Abstract
 PDF
PDF - Recently, atypical femoral fractures (AFFs) have been found in patients who were prescribed bisphosphonate to prevent osteoporotic fractures. Although the occurrence of AFF is rare, there are some concerns, such as a higher risk of delayed or non-union of AFF. This paper reviews the treatment of AFF and suggests some considerations during surgery.
-
Citations
Citations to this article as recorded by- How to Improve Fracture Healing in Atypical Femoral Fractures
Sang-Jin Jeong, Chan-Woo Park, Seung-Jae Lim
Journal of the Korean Orthopaedic Association.2024; 59(1): 9. CrossRef - Atypical Femoral Fracture Occurring at a Proximal Screw Insertion Site after Plate Removal in a Distal Femoral Fracture
Jin Woo Jin, Sung Jin Shin, Jong Min Jeon
Journal of the Korean Orthopaedic Association.2024; 59(4): 314. CrossRef - Position Statement: Atypical Femoral Fracture from the Korean Society for Bone and Mineral Research in 2023
Jae-Hwi Nho, Byung-Woong Jang, Dong Woo Lee, Jae-Hyun Kim, Tae Kang Lim, Soo Min Cha, Dong-Kyo Seo, Yong-Geun Park, Dong-Geun Kang, Young-Kyun Lee, Yong-Chan Ha
Journal of Bone Metabolism.2023; 30(3): 209. CrossRef
- How to Improve Fracture Healing in Atypical Femoral Fractures
- 568 View
- 5 Download
- 3 Crossref

- Treatment Options of Osteoporotic Vertebral Compression Fractures
- Yu Mi Kim, Tae Kyun Kim, Dae Moo Shim, Kyeong Hoon Lim
- J Korean Fract Soc 2018;31(3):114-121. Published online July 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.3.114
-
 Abstract
Abstract
 PDF
PDF - This paper reviews previous studies on the treatment of osteoporotic vertebral compression fractures in elderly patients to determine what factors should be considered for successful treatment. In osteoporotic vertebral compression fractures, the primary treatment is conservative treatments. Other treatments include osteoporosis treatment, pain control, orthosis, and physical therapy. Recently, percutaneous catheterization or balloon plasty is performed for rapid pain recovery and early ambulation. Percutaneous catheterization or balloon posterior plasty is effective in reducing pain and improving the activity ability. Surgical treatment should be considered in cases of nonunion or osteonecrosis, dent, deformation, and spinal cord compression after conservative treatment has failed. In surgical treatment, posterior spinal fixation and vertebroplasty are more advantageous in terms of the amount of bleeding, operation time compared to the anterior approach, but the most appropriate method should be selected through the patient's condition and understanding of each surgical method.
-
Citations
Citations to this article as recorded by- Maigne Syndrome and Thoracolumbar Compression Fracture – An Overlooked Combination in Low Back Pain: A Case Report
Jae-Yong Shim, Myung-Hoon Shin
The Nerve.2025; 11(1): 21. CrossRef - Effects of Herbal Medicines on Bone Mineral Density Score in Osteoporosis or Osteopenia: Study Protocol for a Systematic Review and Meta-Analysis
Su Min Hong, Eun Jung Lee
Journal of Korean Medicine Rehabilitation.2021; 31(2): 49. CrossRef -
Spinal Stability Evaluation According to the Change in the Spinal Fixation Segment Based on Finite Element Analysis
Cheol-Jeong Kim, Seung Min Son, Jin-Young Heo, Chi-Seung Lee
Journal of the Computational Structural Engineering Institute of Korea.2020; 33(3): 145. CrossRef
- Maigne Syndrome and Thoracolumbar Compression Fracture – An Overlooked Combination in Low Back Pain: A Case Report
- 639 View
- 8 Download
- 3 Crossref

Original Article
- Clinical Features and Outcomes of Pelvic Insufficiency Fractures
- Yong Min Seo, Young Chang Kim, Ji Wan Kim
- J Korean Fract Soc 2017;30(4):186-191. Published online October 31, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.4.186
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to investigate the radiological and epidemiological characteristics, as well as the clinical course of pelvic insufficiency fractures in the elderly population.
MATERIALS AND METHODS
At a Haeundae Paik Hospital, we retrospectively reviewed patients with pelvic insufficiency fractures between March 2010 and May 2017. The demographic data of patients were analyzed, and bone mineral density and bone turnover markers were evaluated to estimate the metabolic status of the bone. The radiological characteristics were evaluated by comparing the simple x-ray images with the computed tomography images, and the types of fractures were classified via computed tomography images. For clinical course evaluation, we investigated comorbid complications, and compared the walking ability scale before and 6 months after the fracture.
RESULTS
A total of 42 patients were included, with an average age of 76.5 years. All were female except one case. In 5 cases where the initial medical examination was from another institution, the fracture was not found in 3 cases. All cases received conservative treatment. After the diagnosis of pelvic bone fracture using a simple x-ray imaging, additional fractures were found in 81.0% of the study population using a computed tomography. Initiation of gait occurred at an average of 2.8 weeks, and every case except 1 (97.6%) fully recovered their gait ability.
CONCLUSION
We concluded that there was a limitation with diagnosing pelvic insufficiency fracture using only a simple x-ray imaging technique. In general, cases in this study showed conservative treatment yielded favorable clinical outcome with relatively less critical complications.
- 576 View
- 1 Download

Case Reports
- Insufficiency Fracture of the Femoral Neck after Intramedullary Nailing for the Treatment of Atypical Femoral Fracture - A Case Report -
- Nam Hoon Moon, Jae Hoon Jang, Tae Hyuk Hwang, Ki Young Park
- J Korean Fract Soc 2016;29(4):258-264. Published online October 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.4.258
-
 Abstract
Abstract
 PDF
PDF - Although several publications have reported delayed or non-union, there is a consensus that the standard treatment for atypical femoral fracture (AFF) is an intramedullary nailing. However, no case of tensile insufficiency fracture of femoral neck associated with intramedullary nailing in patients with AFF have been reported. Here, we report an 82-year-old woman with tensile type of insufficiency fracture of the femoral neck after intramedullary nailing for the treatment of AFF.
- 463 View
- 4 Download

- Medial and Lateral Dual Plate Fixation for Osteoporotic Proximal Humerus Comminuted Fracture: 2 Case Reports
- Sam Guk Park
- J Korean Fract Soc 2016;29(1):61-67. Published online January 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.1.61
-
 Abstract
Abstract
 PDF
PDF - Some proximal humeral fractures in elderly patients are accompanied by medial metaphyseal comminution and quality of the bone is so poor that head preserving osteosynthesis seems to be amenable. In cases of medial metaphyseal comminution, lateral locking compression plate (LCP) fixation also has a tendency to become a matter of screw cut out or loss of fixation. The author reports on successful treatment of two osteoporotic proximal humeral fractures combined with medial meta-physeal comminution, with application of additional direct medial supporting plate fixation. Medial plate fixations were added when the fractures were still unstable after the conventional lateral LCP fixation and anterior circumflex humeral arteries had been ruptured before. The fixations were stable enough to start exercise immediately after surgery. The inclinations of the humeral neck were not changed until the last follow-up and clinical results were satisfactory without humeral head osteonecrosis which was a concern.
-
Citations
Citations to this article as recorded by- Dual-Plate Fixation for Proximal Humerus Fractures With Unstable Medial Column in Patients With Osteoporosis
Hyun-Gyu Seok, Sam-Guk Park
Journal of Orthopaedic Trauma.2023; 37(10): e387. CrossRef - The plate fixation strategy of complex proximal humeral fractures
Qi Sun, Xiaoming Wu, Lei Wang, Ming Cai
International Orthopaedics.2020; 44(9): 1785. CrossRef - Biomechanical evaluation of a novel dualplate fixation method for proximal humeral fractures without medial support
Yu He, Yaoshen Zhang, Yan Wang, Dongsheng Zhou, Fu Wang
Journal of Orthopaedic Surgery and Research.2017;[Epub] CrossRef
- Dual-Plate Fixation for Proximal Humerus Fractures With Unstable Medial Column in Patients With Osteoporosis
- 681 View
- 7 Download
- 3 Crossref

Original Articles
- The Result of Conservative Treatment of Proximal Humerus Fracture in Elderly Patients
- Seung Gil Baek, Chang Wug Oh, Young Soo Byun, Jong Keon Oh, Joon Woo Kim, Jong Pil Yoon, Hyun Joo Lee, Hyung Sub Kim
- J Korean Fract Soc 2013;26(4):292-298. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.292
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
With the increase in the old age population, proximal humerus fractures have been increasing recently. However, complications after operative treatment, such as fixation failure, are common because of osteoporosis. We treated proximal humerus fractures in patients with osteoporosis conservatively, and evaluated the radiographic and functional results by analyzing the factors affecting the results.
MATERIALS AND METHODS
Nineteen out of 30 cases for whom the clinical follow-up was over 1 year were included in this retrospective study. There were 17 females and 2 males, and the mean age was 73.2 years. The causes were slip from a short height (18 cases) and a minor car accident (1 case). We evaluated the union period, nonunion, malunion and the Constant score and analyzed several factors affecting the functional result, such as age, fracture pattern, and malunion.
RESULTS
Seventeen cases (89.5%) obtained union within 12.8 weeks on average. Neck-shaft angle was 125.3degrees on average, with seven cases of malunion. The Constant score was 84.1 on average, and there were excellent scores in 11 cases, good scores in 4 cases, and fair scores in 2 cases. Fracture pattern, neck-shaft angle, or malunion did not affect the functional outcome, and elderly patients showed poorer shoulder function.
CONCLUSION
Proximal humeral fractures with osteoporosis may achieve a high rate of bony union when treated with conservative methods. Despite the common occurrence of malunion, a satisfactory functional outcome may be expected.
- 755 View
- 6 Download

- Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
- Ki Chan An, Gyu Min Kong, Jang Seok Choi, Hi Chul Gwak, Joo Yong Kim, Sung Yub Jin
- J Korean Fract Soc 2013;26(4):248-253. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.248
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To determine the influence of osteoporosis on the results of percutaneous K-wire fixation for distal radius fractures.
MATERIALS AND METHODS
Between March 2007 and February 2011, Fifty seven patients who underwent fixative surgery with K-wires after closed reduction and those available for follow-up for at least 6 months were reviewed. They were divided into the two groups of T score -3 or more (group 1) and T score less than -3 (group 2). These groups were compared by the range of motion of the wrist and Disabilities of the Arm, Shoulder and Hand (DASH) score. Radiologic evaluations consisting of radial length, radial inclination and volar tilt were compared. In group 1 with 34 cases, the average age was 65.4 years (50 to 78 years) and T score was -1.97 (-0.1 to -2.93). In group 2 with 23 cases, the average age was 74 years (54 to 89 years) and T score was -4.11 (-3.1 to -6.97).
RESULTS
There was no statistical difference between group 1 and group 2 in terms of range of motion, DASH score and radiologic evaluations.
CONCLUSION
In the case of no volar side cortical comminution, percutaneous K-wire fixation can be applied for the treatment of distal radius fracture with osteoporosis.
- 480 View
- 2 Download

- Osteoporotic Spinal Compression Fracture and Degree of Vitamin D Deficiency
- Hong Sik Kim, Youn Ho Choi, Ki Chul Park, Ye Soo Park
- J Korean Fract Soc 2013;26(1):27-31. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.27
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The aim of the present study was to evaluate the degree of serum vitamin D deficiency in patients with osteoporotic spinal compression fracture and correlation of serum vitamin D level with several variables.
MATERIALS AND METHODS
The medical records of 134 patients with osteoporotic spinal compression fracture, diagnosed at our hospital between October 2008 and June 2011, were reviewed. Serum 25(OH)vitamin D3 was used to evaluate the status of vitamin D level. Serum 25(OH)vitamin D3 level was compared and analyzed according to sex, the number of fractured vertebral body, living environment, and the season of injury. The correlation between vitamin D level and age, bone mineral density, and bone turnover marker were evaluated.
RESULTS
In the serum 25(OH)vitamin D3, 87 patients (65%) associated with osteoporotic spinal compression fracture had an insufficient level. Vitamin D level was the lowest in winter, the highest in summer, and significantly higher in the living home than nursing home. Vitamin D level was negatively correlated with age (r=-0.201, p=0.02) and positively correlated with bone mineral density (r=0.217, p=0.012).
CONCLUSION
Evaluation of vitamin D level in osteoporotic vertebral compression fracture patients may be helpful in planning the treatment of the patients. For insufficient vitamin D level, the adequate sun exposure and supplement of vitamin D may be used. -
Citations
Citations to this article as recorded by- Vitamin D Status according to the Diseases in Hospitalized Rehabilitation Patients: Single Center Study
Hanbit Ko, Jin Hee Nam, Soo-kyung Bok
Brain & Neurorehabilitation.2019;[Epub] CrossRef
- Vitamin D Status according to the Diseases in Hospitalized Rehabilitation Patients: Single Center Study
- 892 View
- 1 Download
- 1 Crossref

- Polarus Intramedullary Nail for Proximal Humeral and Humeral Shaft Fractures in Elderly Patients with Osteoporosis
- Youn Soo Hwang, Kwang Yeol Kim, Hyung Chun Kim, Su Han Ahn, Dong Eun Lee
- J Korean Fract Soc 2013;26(1):14-20. Published online January 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.1.14
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To assess the effectiveness of optimal treatment of proximal humeral fractures and humeral shaft fractures in elderly patients with osteoporosis using the Polarus nail.
MATERIALS AND METHODS
Twenty-three patients with proximal humeral and humeral shaft fractures in elderly osteoporosis patients were treated using the Polarus intramedullary nail. Nine patients had proximal humeral fracture, 10 had humeral shaft fracture and 4 had the proximal humeral frac-ture extended diaphyseally. Radiological outcomes included the bone-union and the degree of re-sidual deformity. The residual deformities of the proximal humerus were assessed by the neck-shaft angle and the shaft angulation. Clinical outcome was assessed with the American Shoulder and Elbow Surgeons (ASES) score.
RESULTS
All cases had bony union and the mean union period was 16.5 weeks. The average neck/shaft alignment at the time of bone union was 135degrees and varus deformities of neck-shaft angle was not seen in all patients. Varus shaft angulation was seen in 5 patients. The mean ASES score after surgery was 86.7 points.
CONCLUSION
The Polarus intramedullary nail is effective for the treatment of proximal humeral and humeral shaft fractures in elderly patients with osteoporosis because it not only enables early postoperative mobilization, but also obtains bone-union without avascular necrosis and nonunion. -
Citations
Citations to this article as recorded by- Surgical Management of Osteoporotic Fractures: Humerus Shaft Fractures
Shankar Ramaprasad Kurpad
Indian Journal of Orthopaedics.2025; 59(8): 1053. CrossRef
- Surgical Management of Osteoporotic Fractures: Humerus Shaft Fractures
- 699 View
- 3 Download
- 1 Crossref

- The Diagnosis of Osteoporotic Occult Vertebral Fracture and Vertebroplasty
- Seong Jun Ahn, Bu Hwan Kim, Moo Ho Song, Seong Ho Yoo, Yeong Joon Kim
- J Korean Fract Soc 2012;25(3):208-214. Published online July 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.3.208
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the effectiveness of magnetic resonance imaging (MRI) for the diagnosis and usefulness of vertebroplasty in osteoporotic occult vertebral fractures.
MATERIALS AND METHODS
Of 472 osteoporotic vertebral fractures treated from May 2003 to July 2009, 45 patients were diagnosed with occult osteoporotic vertebral fracture. Their medical charts and radiographs were reviewed. The degree of vertebral body collapse was graded by a semiquantitative method. In order to increase the reliability, interpretation was based on radiographic diagnoses from 3 orthopedic surgeons. Vertebroplasty was performed at 31 of the 45 patients, for whom conservative treatment failed. Pre-operatively and post-operatively, pain was evaluated using a visual analog scale (VAS).
RESULTS
We observed 55 occult fractures in 45 patients. Forty vertebrae (72.7%) among the 55 vertebrae were just adjacent to an old vertebral fracture with deformation of the vertebral body. The rediagnosis rate of occult fracture attempted without MRI was only 21.8%. The average pre-operative VAS score of 8.07 (6~9) was improved to 2.43 after surgery and showed no delayed vertebral body collapse.
CONCLUSION
Gadolinium enhancement of MRI is critical to the diagnosis of occult vertebral fractures, which are 9% of whole osteoporotic vertebral fractures. Seventy-two point seven percent of occult vertebral fractures were just adjacent to an old vertebral fracture with collapse of the vertebral body. This means that if vertebroplasty is performed without thorough MRI examination, it may fail.
- 620 View
- 1 Download

- Results of Osteoporotic Treatment Drug after Periarticular Fracture of Hip
- Soo Jae Yim, Young Koo Lee, Cheong Kwan Kim, Hyun Seok Song, Hee Kyung Kang
- J Korean Fract Soc 2010;23(2):167-171. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.167
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The Purpose of the study is to know patients' compliance of drug treatment of osteoporosis after operation of fracture and to compare of accompanying fractures between patients who diagnosed with osteoporosis itself and had the drug treatment of osteoporosis after surgery of periarticular fracture of hip.
MATERIALS AND METHODS
In experimental group, consecutive 60 patients who had fracture of femoral neck and trochanter. And in control group, 61 patients diagnosed osteoporosis with drug treatment within the same period in orthopedic department from July 2006 to July 2007. The average age is 73.8 (+/-6.7) year in experimental group, and 66.6 (+/-7.46) year in control group. Both groups had at least a year follow-up with drug treatment and had BMD again at least a year later.
RESULTS
BMD test in experimental group showed -3.05 (+/-1.35) preoperatively and -2.74 (+/-1.50) in last follow-up. BMD test in control group showed -3.55 (+/-0.52) in initial administration and -3.10 (+/-0.87) in last follow-up. The results showed a significant improvement in statistical analysis (p=0.0002, p<0.0001).
CONCLUSION
The compliance of drug treatment of osteoporosis after operation of periarticular fracture of hip is the same as in patients' diagnosed osteoporosis. -
Citations
Citations to this article as recorded by- Does the Time of Postoperative Bisphosphonate Administration Affect the Bone Union in Osteoporotic Intertrochanteric Fracture of Femur?
Yoon Je Cho, Young Soo Chun, Kee Hyung Rhyu, Joon Soon Kang, Gwang Young Jung, Jun Hee Lee
Hip & Pelvis.2015; 27(4): 258. CrossRef - Sequential Hip Fractures in Elderly Osteoporotic Patients
Soojae Yim, Yuseok Seo, Sanghyok Lee, Joonghyun Ahn
Hip & Pelvis.2012; 24(4): 309. CrossRef
- Does the Time of Postoperative Bisphosphonate Administration Affect the Bone Union in Osteoporotic Intertrochanteric Fracture of Femur?
- 601 View
- 0 Download
- 2 Crossref

- Treatment for Unstable Distal Radius Fracture with Osteoporosis: Internal Fixation versus External Fixation
- Jin Rok Oh, Tae Yean Cho, Sung Min Kwan
- J Korean Fract Soc 2010;23(1):76-82. Published online January 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.1.76
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the functional and radiological outcomes of volar plating to that of external fixation for treating unstable osteoporotic distal radius fracture.
MATERIALS AND METHODS
From March 2006 to March 2008, 36 patients with osteoporosis over 60-year old were selected for this study. They were divided into two groups; group I (open reduction and internal fixation with volar fixed angle plate) and group II (closed reduction and external fixation). Clinical outcomes and radiologic outcomes were evaluated.
RESULTS
There was no statistical difference between group I and group II in range of motion and DASH score, BMD score. However, the grip strength and PRWE score were found to be higher in group II (p<0.05). In radiologic evaluation, group I showed higher radial inclination, volar tilting angle (p<0.05).
CONCLUSION
Internal fixation using Volar-fixed Angle Plate seems to give more stable fixation for distal articular fragments compared to external fixation. it could allow early postoperative exercise and could result in low incidence of postoperative complication such as pin track infections and joint stiffness. Therefore, the internal fixation could be more desirable treatment method to manage unstable distal radius fracture. -
Citations
Citations to this article as recorded by- Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
Ki-Chan An, Gyu-Min Kong, Jang-Seok Choi, Hi-Chul Gwak, Joo-Yong Kim, Sung-Yub Jin
Journal of the Korean Fracture Society.2013; 26(4): 248. CrossRef
- Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
- 682 View
- 0 Download
- 1 Crossref

- The Relationship between Progression of Body Collapse and MRI Findings in Osteoporotic Stable Thoracolumbar Fractures
- Young Do Koh, Jong Seok Yoon, Ji Young Hwang, Hyun Sik Park
- J Korean Fract Soc 2008;21(4):304-311. Published online October 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.4.304
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To find out the relationship between the initial Magnetic Resonance Image (MRI) findings and the progression of vertebra collapse when treated with Jewett brace in osteoporotic stable thoracolumbar fractures.
MATERIALS AND METHODS
We divided 38 cases of 37 patients of thoracolumbar osteoporotic stable thoracolumbar fractures who were treated with Jewett brace into two groups. One group was composed of those body collapse progressed more than 10% compared with the initial state, and the other group less than 10%. We analyzed the relationships between the progression of collapse and the superior endplate fractures, the fracture line extending to posterior cortex, the size of bone marrow edema, the signal intensity on T1 and T2 weighted MR images, the presence of paravertebral hematoma, and the degree of posterior extensor muscle atrophy using MR images.
RESULTS
The body collapse was more likely to progress when there was superior endplate fracture, when it showed larger size of bone marrow edema on T1 weighted image, and transverse low signal on T2 weighted image. But extending of fracture line to posterior cortex, presence of paravertebral hematoma, and degree of posterior extensor muscle atrophy did not show any statistical correlations to progression of collapse.
CONCLUSION
The body collapse is more likely to progress when there was superior endplate fracture, larger low signal on T1 weighted image and low signal on T2 weighted image at initial MRI treated with Jewett brace. -
Citations
Citations to this article as recorded by- The Factors between the Progression of the Compression Rate and Magnetic Resonance Imaging Findings in Osteoporotic Vertebral Fracture Patients Treated with Teriparatide
Taebyeong Kang, Seung-Pyo Suh, Jeongwoon Han, Byungjun Kang, Changhyun Park
Journal of the Korean Orthopaedic Association.2023; 58(5): 392. CrossRef - Statistical Analysis on Hospitalized Patients with Thoracolumbar Compression Fracture at Single Korean Medicine Hospital: Retrospective Review
Hyun jin Jang, So jeong Kim, Min Ju Kim, Hyeon Kyu Choi, Pil Je Park, Kang Yeon soo, Jeong Kyo Jeong, Ju Hyun Jeon, Young Il Kim
Journal of Korean Medicine.2023; 44(2): 149. CrossRef - The Influence of Initial Magnetic Resonance Imaging Findings on the Compression Rate of Thoracolumbar Osteoporotic Vertebral Compression Fracture
Seok-Ha Hwang, Seung-Pyo Suh, Young-Kyun Woo, Ho-Seung Jeon, Ho-Won Jeong
Journal of the Korean Orthopaedic Association.2018; 53(4): 341. CrossRef - The Relationship between the Progression of Kyphosis in Stable Thoracolumbar Fractures and Magnetic Resonance Imaging Findings
Deuk Soo Jun, Won Ju Shin, Byoung Keun An, Je Won Paik, Min Ho Park
Asian Spine Journal.2015; 9(2): 170. CrossRef
- The Factors between the Progression of the Compression Rate and Magnetic Resonance Imaging Findings in Osteoporotic Vertebral Fracture Patients Treated with Teriparatide
- 754 View
- 1 Download
- 4 Crossref

- Comparison between Results of Internal Fixation and Hemiarthroplasty in Unstable Intertrochanter Fracture of Osteoporotic Bone
- Haw Jae Jung, Jae Yeol Choi, Hun Kyu Shin, Eugene Kim, Se Jin Park, Yong Taek Lee, Gwang Sin Kim, Jong Min Kim
- J Korean Fract Soc 2007;20(4):291-296. Published online October 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.4.291
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To perform comparative analysis between the results of internal fixation and hemiarthroplasty in unstable intertrochanteric fracture of osteoporotic bone.
MATERIALS AND METHODS
From February 2003 to February 2006, 36 patients treated surgically for unstable intertrochanteric fractures were evaluated. The patient's age was older than 70 year old; the T-score of preoperative bone mineral density (BMD) was lower than -3.0; they were followed up for more than 1 year. The patient were divided into two groups. One group was treated with dynamic hip screw or proximal femoral nail (Group A, 23 cases), and the other group was treated with bipolar hemiarthroplasty (Group B, 13 cases). The two groups were compared in terms of hip joint function using Clawson classification and radiologically.
RESULTS
Nonunion and fixation failure happened in 6 cases (26%) of gruop A. However, all patients in group B showed stable maintenance of implant. Recovery of hip joint function was found in 13 cases (43%) of group A, whereas 12 cases (93%) of group B recovered.
CONCLUSION
Nonunion and failure of fixation happened more frequently in internal fixation than bipolar hemiarthroplasty, and the postoperative hip joint function was better in bipolar hemiarthroplasty than internal fixation. Therefore, bipolar hemiarthroplasty might be better operative treatment for unstable intertrochanteric fracture of osteoporotic bone. -
Citations
Citations to this article as recorded by- The Stability Score of the Intramedullary Nailed Intertrochanteric Fractures: Stability of Nailed Fracture and Postoperative Patient Mobilization
Sung-Rak Lee, Seong-Tae Kim, Min Geun Yoon, Myung-Sang Moon, Jee-Hyun Heo
Clinics in Orthopedic Surgery.2013; 5(1): 10. CrossRef - Analysis of the Factors Involved in Failed Fixation in Elderly Intertrochanteric Femoral Fracture
Joon Soon Kang, Ryuh Sup Kim, Bom Soo Kim, Young Tae Kim, Seung Hyun Hong
Journal of the Korean Fracture Society.2012; 25(4): 263. CrossRef - Results of Osteoporotic Treatment Drug after Periarticular Fracture of Hip
Soo Jae Yim, Young Koo Lee, Cheong Kwan Kim, Hyun Seok Song, Hee Kyung Kang
Journal of the Korean Fracture Society.2010; 23(2): 167. CrossRef
- The Stability Score of the Intramedullary Nailed Intertrochanteric Fractures: Stability of Nailed Fracture and Postoperative Patient Mobilization
- 940 View
- 4 Download
- 3 Crossref

- Comparison of LC-DCP versus LCP for Internal Fixation of Humeral Shaft Fractures in Elderly Patient
- Chang Yong Hur, Won Yong Shon, Jun Gyu Moon, Sang Hwan Han, Jae Young Hong, Sung Kang Chun
- J Korean Fract Soc 2007;20(3):246-251. Published online July 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.3.246
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare outcomes of humeral shaft fractures fixed with locking compression plate and those fixed with dynamic compression plate in elderly patients.
MATERIALS AND METHODS
Nineteen consecutive elderly patients with a fracture of the humeral diaphysis were evaluated retrospectively. Ten patients had been fixed with LC-DCP, and nine had been fixed with LCP. Radiological and clinical results were compared and comparison of implants was done.
RESULTS
Loosening of the plate occurred in one case each from the LCP group and the LC-DCP group. The rest of the patients achieved union uneventfully without any complications. Union rate, clinical score and hardware were not significantly different between the two groups. One patient who developed loosening in the LC DCP underwent reoperation whereas one patient with loosening in the LCP was successfully managed conservatively.
CONCLUSION
Principle of fracture fixation was more important than plate selection in humeral shaft fracture of elderly patient. -
Citations
Citations to this article as recorded by- Plate osteosynthesis of fractures of the shaft of the humerus: comparison of limited contact dynamic compression plates and locking compression plates
Ashutosh Kumar Singh, Nidhi Narsaria, R. R. Seth, S. Garg
Journal of Orthopaedics and Traumatology.2014; 15(2): 117. CrossRef - Clinical and Radiographical Follow-up for Residual Displacement of Fracture Fragments after Interlocking Intramedullary Nailing in Humeral Shaft Fractures
Jae-Kwang Yum, Dong-Ju Lim, Eui-Yub Jung, Su-Een Sohn
The Journal of the Korean Shoulder and Elbow Society.2013; 16(2): 107. CrossRef
- Plate osteosynthesis of fractures of the shaft of the humerus: comparison of limited contact dynamic compression plates and locking compression plates
- 972 View
- 4 Download
- 2 Crossref

- Treatment of Senile Osteoporotic Intertrochanteric Fracture using Proximal Femoral Nail
- Dong Hui Kim, Sang Hong Lee, Young Lae Moon, Jun Young Lee, Kun Sang Song
- J Korean Fract Soc 2007;20(3):215-221. Published online July 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.3.215
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Clinical and radiologic results of femur intertrochanteric fractures treated with ITST nail in elderly patients with osteoporosis were analysized to evaluate the efficacy and complication of ITST nailing.
MATERIALS AND METHODS
32 patients who were treated with ITST nail due to femur intertrochanteric fracture and were followed up for more than 1 year were analysed. According to Evans classification, 11 cases were stable fractures and 21 cases were unstable fractures. Clinically, ambulatory function was compared and radiologically, BMD of healthy leg was checked with analysis of postoperative bone union and complication.
RESULTS
In ambulatory function comparison before and after the operation, there were 9 cases of good, 17 cases of moderate and 6 cases of poor. Considering social activity after the operation, 7 cases showed normal ambulation, 9 cases showed ambulatory with one cane, 5 cases showed two cane ambulation and 11 cases showed dependent ambulation. In radiologic evaluation, T-score of ward triangle in healthy femoral neck showed BMD of -3.12. In 20 cases, bone union was observed within 3 months. The patients with low BMD result had poor outcome. There were 2 cases of intraoperative proximal femur fracture, 3 cases of nonunion and 4 cases of death within 1 year.
CONCLUSION
In elderly patients with intertrochanteric fracture, ITST nailing is relatively efficient treatment. However, in pateint with severe osteoporosis (T-score<-3.0) and unstable fracture pattern, arthroplasty should be considered due to relatively high complicaton rate. -
Citations
Citations to this article as recorded by- The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
Jeoung Ho Kim, Sang Hong Lee, Kwang Chul Lee, Sung Won Cho
Journal of the Korean Fracture Society.2011; 24(3): 217. CrossRef - Results of Osteoporotic Treatment Drug after Periarticular Fracture of Hip
Soo Jae Yim, Young Koo Lee, Cheong Kwan Kim, Hyun Seok Song, Hee Kyung Kang
Journal of the Korean Fracture Society.2010; 23(2): 167. CrossRef
- The PFNA Nail for Pertrochanteric Fracture of the Femur without Fracture Table
- 814 View
- 2 Download
- 2 Crossref

- Treatment with Modified Steinmann Pins and Tension Band Wiring Technique in Proximal Humeral Comminuted Fractures with Osteoporosis
- Soo Tai Chung, Joo Hak Kim, Hyung Soo Kim, Sang Joon Park
- J Korean Fract Soc 2007;20(2):184-189. Published online April 30, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.2.184
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the usefulness of internal fixation with modified Steinmann pins and tension band wiring technique in comminuted proximal humeral fracture with osteoporosis and the correlations among bone mineral density, age, Neer's score and period of union.
MATERIALS AND METHODS
Twelve cases of comminuted proximal humeral fracture with osteoporosis were surgically treated with modified Steinmann pins and tension band technique, and followed up for an average 20.8 months (range, 6~39 months). Average age was 73.6 years old (range, 59~85 years old). Results were assessed using Neer's evaluation criteria.
RESULTS
Excellent results were noted in eight cases and satisfactory results in four cases. Radiological union was obtained in all cases. Two cases showed impingement syndrome of the proximal portions of Steinmann pins, which were managed by early removal of the metal. One case developed operative wound infection, which were managed by antibiotics therapy, irrigation and secondary closure.
CONCLUSION
Internal fixation using modified Steinmann pins and tension band wiring technique for proximal humeral fracture, with osteoporosis, makes complete union of fracture, minimizes risk of complications, and enables early rehabilitation by rendering relatively rigid fixation.
- 438 View
- 1 Download

- Factors Confluencing the Result of Percutaneous Balloon Kyphoplasty in Osteoporotic Thoracolumbar Compression Fracture
- Jung Hee Lee, Dae Woo Hwang, Jae Heung Shin, Woo Sung Hong, Ju Wan Kim
- J Korean Fract Soc 2007;20(1):76-82. Published online January 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.1.76
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We are to find the method to objectify postoperative prognosis, analyzing the factors confluencing the result of kyphoplasty in osteoporotic vertebral compression fracture (OVCF).
MATERIALS AND METHODS
Our study included 50 patients (55 vertebral bodies) who have undergone kyphoplasty from Sep. 2004 until Oct. 2005. We divided in the group according to bone mineral density (BMD), compression rate, recovery rate and cement leakage. We verified the significance of each group, using independent t-test, and ANOVA test among observers.
RESULTS
We performed kyphoplasty on 55 vertebral bodies, 12 cases with more than 0.4 g/cm2 in BMD (mean: 0.53 g/cm2) and their mean preoperative compression rate (CR), immediate postoperative recovery rate (RR-IPO), and recovery rate after 6 months (RR-6M) was each 30.58%, 12.35%P, 9.93%P. 15 cases under 0.4 g/cm2 (mean 0.31 g/cm2), and their CR, RR-IPO and RR-6M was 26.73%, 11.77%P, 5.26%P respectively. The p-value was 0.004. Another studies according to CR, RR-IPO and leakage of cement revealed the better results in the cases of the lower CR, the smaller reduction and abscecnce of cement leakage, but statistically insignificant (p=0.309, 0.069, 0.356).
CONCLUSION
Preoperative BMD was most important factor that confluencing postoperative radiological result in OVCF. Other factors were also thought to be confluencing factors, but statistically insignificant.. -
Citations
Citations to this article as recorded by- Cement Leakage into Disc after Kyphoplasty: Does It Increases the Risk of New Adjacent Vertebral Fractures?
Hoon-Sang Sohn, Seong-Kee Shin, Eun-Seok Seo, Kang-Seob Chang
Journal of the Korean Fracture Society.2011; 24(4): 361. CrossRef
- Cement Leakage into Disc after Kyphoplasty: Does It Increases the Risk of New Adjacent Vertebral Fractures?
- 635 View
- 0 Download
- 1 Crossref

- A Clinical Analysis of 260 Percutaneous Vertebroplasty in the Treatment of Osteoporotic Compression Fracture
- Sang Hyuk Min, Myung Ho Kim, Hee Gon Park, Ho Dong Paik
- J Korean Fract Soc 2006;19(3):357-362. Published online July 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.3.357
-
 Abstract
Abstract
- PURPOSE
To evaluate retrospectively the results regarding pain relief, complication after percutaneous vertebroplasty, for an osteoporotic compression fractures.
MATERIALS AND METHODS
260 patients (male 55, female 260, mean age 69.4 years old) treated by percutaneous vertebroplasty in Dankook University Hospital from July 1997 to July 2004 were reviewed. We performed percutaneous vertebroplasty and observed the degree of pain relief using pain scale pre-/postoperation. we evaluate the complication by plain radiographs and computed tomography, ABGA and chest X-ray. we evaluate pain relief and complication for 1 week by follow-up plain radiographs. we recommended BMD follow-up per 1 year and osteoporosis medication at least 2 years. A clinical result was evaluated as excellent, good, fair, poor and visual analogue scale (VAS 0~10) for 1 year. We prefaced a statistical analysis by T-test using SPSS (version 11.0) correlating 1 week and 1 years effects.
RESULTS
73 (28.3%) of the patients were evaluated as excellent: 123 (45.5%), as good: 45 (17.8%), as fair; and 23 (8.5%), as poor, show 73.8% over good in 1 week. 76 (29.3%) of the patients were evaluated as excellent; 120 (44.3%), as good; 43 (16.8%), as fair; and 25 (9.6%), as poor in 1 year, show 73.6% over good result. 1 week follow-up and 1 year follow-up show similar results. 1 patient had death (hemothorax), 4 patients had arrhythmia, 15 patients (21 vertebrae) had fracture around vertebroplasty.
CONCLUSION
Percutaneous vertebroplasty using PMMA is valuable method in the treatment of osteoporotic compression fracture, providing immediately pain relief, long term pain relief, prevention of complication originated from long term traction and bed rest, unwearing brace and early ambulation. -
Citations
Citations to this article as recorded by- Comparison of Outcomes of Conservative Treatment, Early Vertebroplasty, and Delayed Vertebroplasty in Patients with Osteoporotic Vertebral Compression Fractures
Se-Hyuk Im, Young-Joon Ahn, Bo-Kyu Yang, Seung-Rim Yi, Ye-Hyun Lee, Ji-Eun Kwon, Jong-Min Kim
Journal of Korean Society of Spine Surgery.2016; 23(3): 139. CrossRef - Comparison of Outcomes of Conservative Treatment, Early Vertebroplasty, and Delayed Vertebroplasty in Patients with Osteoporotic Vertebral Compression Fractures
Se-Hyuk Im, Young-Joon Ahn, Bo-Kyu Yang, Seung-Rim Yi, Ye-Hyun Lee, Ji-Eun Kwon, Jong-Min Kim
Journal of Korean Society of Spine Surgery.2016; 23(3): 139. CrossRef - Large Pulmonary Embolus after Percutaneous Vertebroplasty - A Case Report -
Sang Ho Moon, Soo Won Lee, Byoung Ho Suh, Sung Hwan Kim
Journal of Korean Society of Spine Surgery.2009; 16(1): 46. CrossRef - Risk Factors of New Compression Fractures in Adjacent Vertebrae after Percutaneous Vertebroplasty
Myung-Ho Kim, Sang-Hyuk Min, Suk-Ha Jeon
Journal of the Korean Fracture Society.2007; 20(3): 260. CrossRef
- Comparison of Outcomes of Conservative Treatment, Early Vertebroplasty, and Delayed Vertebroplasty in Patients with Osteoporotic Vertebral Compression Fractures
- 587 View
- 0 Download
- 4 Crossref

- Percutaneous Vertebroplasty in the Treatment of Osteoporotic Compression Fracture (99 Patients, 171 Vertebral Bodies)
- Chung Hwan Kim, Hyung Sun Ahn, Jae Kwang Hwang, Jung Suk Song, Eui Jung Bae
- J Korean Fract Soc 2006;19(2):259-264. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.259
-
 Abstract
Abstract
- PURPOSE
This study was designed to compare the clinical and radiologic outcome of the patients who underwent percutaneous vertebroplasty among the groups based on follow-up period and BMD.
MATERIALS AND METHODS
A total of 99 patients (171 vertebral bodies) underwent percutaneous vertebroplasty from January 2001 to September 2003. The patients were divided into 3 groups by follow-up periods, and also divided into 2 groups by BMD. We investigated the difference of radiologic and clinical effects among the groups. Radiologic findings was assessed as vertebral height restoration rate and rate of reduction loss by measurement of the height of vertebral body. The clinical outcomes were graded into 5. The statistical analysis was done using Chi-squire test and Independent-samples T test.
RESULTS
Among the groups divided by follow-up period, there was no statistically significant difference of clinical and radiologic results except the rate of reduction loss between group I and group III (p>0.05). Between the groups divided by BMD, there was no statistically significant difference of clinical and radiologic results.
CONCLUSION
Percutaneous vertebroplasty with bone cement for the osteoporotic compression fracture is an efficient procedure and considered as technique producing pleasurable clinical and radiologic results regardless of follow up-period and BMD.
- 440 View
- 0 Download

Case Report
- Inlay Fibular Autograft and Helical LCP Fixation for a Segmental Comminuted Fracture of the Osteoporotic Proximal Humerus: A Case Report
- Young Soo Byun, Dong Ju Shin, Se Ang Chang, Do Yop Kwon
- J Korean Fract Soc 2006;19(1):100-103. Published online January 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.1.100
-
 Abstract
Abstract
- Unstable fractures of the proximal humerus should be treated with precise reduction and stable fixation, and early joint motion should be permitted. But stable fixation of the proximal humerus is frequently difficult to obtain in older patients due to osteoporosis and fracture comminution. We treated one case of a segmental comminuted fracture of the proximal humerus with severe osteoporosis with a method of inlay fibular autograft and fixation with a helical locking compression plate (LCP). Stable fixation was obtained, so early motion of the shoulder joint was permitted. The fracture was healed in 12 weeks after the operation without loss of fixation and there were no problems at the donor site of the fibula. Functional recovery of the shoulder was satisfactory. The result of Neer's functional score was 87 points (satisfactory) and Constant score was 83 points.
-
Citations
Citations to this article as recorded by- Helical Plating for Fractures of the Proximal Humeral Shaft
Young-Soo Byun, Dong-Ju Shin, Young-Bo Park, Min-Guek Kim, Toe-Hoe Gu, Jae-Hwi Han
Journal of the Korean Orthopaedic Association.2017; 52(3): 232. CrossRef - Allogeneic Inlay Cortical Strut Grafts for Large Cysts or Post-curettage Cavitary Bony Defects
Yang-Guk Chung, Yong-Koo Kang, Chol-Jin Kim, An-Hi Lee, Jeong-Mi Park, Won-Jong Bahk, Hyun-Ho Yoo
The Journal of the Korean Bone and Joint Tumor Society.2011; 17(2): 73. CrossRef - Minimally Invasive Plate Osteosynthesis, MIPO
Young-Soo Byun
Journal of the Korean Fracture Society.2007; 20(1): 99. CrossRef
- Helical Plating for Fractures of the Proximal Humeral Shaft
- 512 View
- 0 Download
- 3 Crossref

Original Articles
- Differences of Bone Mineral Density between Spine and Hip in Osteoporotic Patients
- Gyu Min Kong, Sang Eon Lee, Dong Jun Kim, Tae Hyun Yoon
- J Korean Fract Soc 2005;18(2):181-184. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.181
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate differences and correlations of spine and hip region BMD in osteoporotic patients with or without spine fracture.
MATERIALS AND METHODS
From January 1999 to December 2002, We measured and evaluated BMD of L3 and hip by DXA in 52 patients with spine fracture (fracture group) and 96 osteoporotic patients without spine fracture (non-fracture group) above 60 years.
RESULTS
The average age of patients with spine fracture is 72.1 years and without spine fracture is 66.9 years. There were no statistical significant differences of BMD of spine, neck of femur and trochanteric area between 2 groups. But the BMD of Ward triangle of fracture group decreased significantly in statistics. The correlation coefficient between the lumbar spine and trochanteric area were 0.674 in fracture group and 0.794 in non-fracture group. They had statistical significance (<0.01).
CONCLUSION
The BMD of Ward triangle of fracture group had lower value, but the BMD of lumbar spine had no differences between 2 groups. Therefore in these persons who have decreased BMD in Ward triangle should be concerned about high vertebral compression fracture risk vertebral compression fracture. -
Citations
Citations to this article as recorded by- Comparison of vertebral and femoral bone mineral density in adult females
Han Seong Choe, Jae Hong Lee, Dong Ki Min, So Hong Shin
Journal of Physical Therapy Science.2016; 28(6): 1928. CrossRef - Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
Ki-Chan An, Gyu-Min Kong, Jang-Seok Choi, Hi-Chul Gwak, Joo-Yong Kim, Sung-Yub Jin
Journal of the Korean Fracture Society.2013; 26(4): 248. CrossRef - Comparison of Bone Mineral Density in Elderly Patients over 65 Years according to Presence and Types of Hip Fracture
Myung-Ho Kim, Moon-Jib Yoo, Joong-Bae Seo, Hyun-Yul Yoo, Sang-Young Moon
Journal of the Korean Fracture Society.2010; 23(3): 263. CrossRef - Comparison of Bone Mineral Density in Elderly Patients according to Presence of Intertrochanteric Fracture
Sang Ho Moon, Byoung Ho Suh, Dong Joon Kim, Gyu Min Kong, Hyeon Guk Cho
Journal of the Korean Fracture Society.2007; 20(3): 222. CrossRef
- Comparison of vertebral and femoral bone mineral density in adult females
- 684 View
- 1 Download
- 4 Crossref

- A Comparison of Vertebroplasty Versus Conservative Treatment in Osteoporotic Compression Fractures
- Sang Ho Moon, Dong Joon Kim, Chung Soo Hwang, Sang Eon Lee, Se Won Park
- J Korean Fract Soc 2004;17(4):374-379. Published online October 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.4.374
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare clinical and radiological results between vertebroplasty and conservative treatment in osteoporotic compression fractures of thoracolumbar spine.
MATERIALS AND METHODS
34 patients were reviewed with at least 1 year follow up. Vertebroplasty was used in 14 and conservative treatment was done in 20 fractures. These groups were compared by clinical results which were evaluated by the scoring system according to pain, mobility and analgesic usage at preoperative, postoperative 1 month and postoperative 1 year. And also compared by the increment of kyphosis and loss of vertebral body height in lateral films at the same time. We compared duration of hospitalization between two groups.
RESULTS
Vertebroplasty group showed statistically significant less pain and mobility than conservative treatment (p<0.05), but there was no differences in analgesic usage at postoperative 1 year while significant difference at 1 month. In radiological comparison, vertebroplasty showed less increment of kyphosis and loss of body height significantly (p<0.05). Also vertebroplasty group had shorter hospitalization stay significantly (p<0.05).
CONCLUSION
Our retrospective analysis demonstrated that vertebroplasty provided significant pain relief, improvement of motion and reduction of analgesic usage and also provided considerable spinal stabilization that prevented further kyphosis and collapse. -
Citations
Citations to this article as recorded by- Outcome Comparison between Percutaneous Vertebroplasty and Conservative Treatment in Acute Painful Osteoporotic Vertebral Compression Fracture
Hwa-Yeop Na, Young-Sang Lee, Tae-Hoon Park, Tae-Hwan Kim, Kang-Won Seo
Journal of Korean Society of Spine Surgery.2014; 21(2): 70. CrossRef - Large Pulmonary Embolus after Percutaneous Vertebroplasty - A Case Report -
Sang Ho Moon, Soo Won Lee, Byoung Ho Suh, Sung Hwan Kim
Journal of Korean Society of Spine Surgery.2009; 16(1): 46. CrossRef
- Outcome Comparison between Percutaneous Vertebroplasty and Conservative Treatment in Acute Painful Osteoporotic Vertebral Compression Fracture
- 841 View
- 1 Download
- 2 Crossref

- Insufficiency Fractures of the Femoral Shaft Associated with Osteoporosis
- Hae Seok Koh, Yong Koo Kang, Han Yong Lee, Kee Won Rhyu, Joo Hyoun Song, Jin Young Jeong, Eun Seong Song
- J Korean Fract Soc 2004;17(1):19-24. Published online January 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.1.19
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To present a clinical experience of the insufficiency fractures of the femoral shaft associated with osteoporosis MATERIALS AND METHODS: From January 1995 to December 2002, four patients (8 cases, four females) more than 1-year follow up were reviewed retrospectively. The mean age was 61 years (range, 55 to 73). Medical records and roentgenograms were reviewed.
RESULTS
The fractures were bilateral. Plain film revealed fracture line in six among seven cases excluding 1 displaced fracture at initial presentation. All cases presented osteoporosis, anterolateral bowing of the femur, and hot spot in bone scan. Five cases (four displaced, one impending displaced fracture) underwent interlocking intramedullary nailing and all five of them manifested no evidence of delayed union. The preoperative thigh and knee joint pain improved postoperatively.
CONCLUSION
Femoral shaft insufficiency fracture could occur rarely in patients with anterolateral bowing of the femur and postmenopausal osteoporosis. Careful history taking, radiography and bone scan are necessary, and bone scan is helpful for early diagnosis. Once diagnosed as the insufficiency fracture with fracture-related symptoms, prophylactic nailing may be necessary lest complete displaced fracture should occur. -
Citations
Citations to this article as recorded by- Quantification and material modelling of the localized non-bone regions in the trabecular architecture of the sacrum
Immanuel Ries, Anantha Narayanan Ramakrishnan, Amadeus Alcântara, Munir Skaf, Christopher Ludtka, Thomas Mendel, Friederike Klauke, Stefan Schwan
Computer Methods in Biomechanics and Biomedical Engineering.2025; : 1. CrossRef - Research on the Coverage Expansion and Optimization Strategy of Unemployment Insurance System Based on the Comparison between China and Britain
Ruolan Xiao, M. Md Husin
SHS Web of Conferences.2024; 193: 01039. CrossRef - Pelvic Insufficiency Fracture in Severe Osteoporosis Patient
Woong Chae Na, Sang Hong Lee, Sung Jung, Hyun Woong Jang, Suenghwan Jo
Hip & Pelvis.2017; 29(2): 120. CrossRef - Femoral Shaft Fracture of a Middle-aged Male Adult during Playing Baseball
Ho-Seung Jeon, Young-Kyun Woo, Seok-Ha Hwang, Seung-Pyo Seo, Ho-Won Jeong, Sung-Tae Lim
The Korean Journal of Sports Medicine.2017; 35(1): 57. CrossRef - Surgical Treatment of Atypical Femoral Fracture
Kyung-Jae Lee, Yong-Wook Kwon, Yong Chan Ha, Young-Kyun Lee, Beom-Soo Kim, Byung-Woo Min
Journal of the Korean Orthopaedic Association.2013; 48(3): 185. CrossRef - Letter: Repeated Metal Breakage in a Femoral Shaft Fracture with Lateral Bowing - A Case Report -
Hae Seok Koh
Journal of the Korean Fracture Society.2012; 25(3): 240. CrossRef - Association of Low-energy Femoral Shaft Fractures and Bisphosphonate Use
Hae Seok Koh
Orthopedics.2012; 35(9): 736. CrossRef - Repetitive Insufficiency Fractures of the Femoral Shaft - A Case Report -
Ji-Hwan Kim, Young-Ho Cho, Young-Soo Byun, Jung-Hoon Shin, Chung-Yeol Lee, Tae-Gyun Kim
Journal of the Korean Fracture Society.2010; 23(1): 109. CrossRef
- Quantification and material modelling of the localized non-bone regions in the trabecular architecture of the sacrum
- 593 View
- 4 Download
- 8 Crossref

- Complications after Vertebroplasty of Treatment for Compression Fracture with Osteoporosis
- Hee Gon Park, Myung Ho Kim, Moon Jib Yoo, Sung Chul Lee, Jin Young Park, Woo Yeon Hwang, Jin Woo An
- J Korean Soc Fract 2003;16(4):534-540. Published online October 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.4.534
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the complications of percutaneous vertebroplasty using PMMA (polymethylmethacrylate) in the treatment of osteoporotic compression fractures.
MATERIALS AND METHODS
Authors reviewed 113 patients treated by percutaneous vertebroplasty from 1998 to 2001. After treatment, Simple x-ray and computed tomography were done of methods for analysis of complication, especially bone cement leakage.
RESULTS
In each case, we injected bone cement (PMMA) in one vertebra, average amount is 5.6 cc. The complications were 39 cases (34.5%): 1 case was dead by hemothorax, 1 case was arrhythmia, 12 cases were intercostals neuralgia, 7 cases were back pain, 2 cases were mild dyspnea, 14 cases were abdominal pain and 2 case were injection site pain. In follow-up x-ray and CT, bone cement (PMMA) leakage were 45 cases (39.8%).
CONCLUSION
Bone cement (PMMA) leakage can be cause of complications in vertebroplasty. We try to avoid the complication of bone cement leakage. -
Citations
Citations to this article as recorded by- A Review of Korean Medicine Treatment for Managing the Thoracolumbar Compression Fractures: A Retrospective Observational Study
Min-Jin Cho, Jiyun Lee, Myeong-Jong Lee, Hojun Kim, Kyungsun Han
Journal of Korean Medicine Rehabilitation.2023; 33(4): 109. CrossRef - Clinical and radiological outcomes of denosumab and teriparatide treatment in elderly patients with osteoporotic spinal compression fracture without vertebroplasty
Joo Young Jung, Byoung Hun Lee, Jong Young Lee, Hong Jun Jeon, Byung Moon Cho, Su Yeon Kim, Se Hyuck Park
Journal of Korean Society of Geriatric Neurosurgery.2021; 17(2): 69. CrossRef - A Retrospective Clinical Survey of Vertebral Compression Fractures
Ji Hye Oh, Yun Kyu Lee, Jae Soo Kim, Hyun Jong Lee, Sung Chul Lim
Journal of Acupuncture Research.2018; 35(4): 219. CrossRef - Survival Analysis of Conservative Treatement in Osteoporotic Vertebral Fracture
Young Do Koh, Jong-Oh Kim, Rag Gyu Kim, Dae Youn Kim, Nam-Ki Kim, Dong Jun Kim
Journal of Korean Society of Spine Surgery.2012; 19(4): 138. CrossRef - Factor Analysis Affecting the Leakage of Bone Cement After Vertebroplasty
Jae-Hoon Kim, Kyung-Jin Song, Tai-Seung Kim, Jae-Lim Cho, Ye-Soo Park
Journal of Korean Society of Spine Surgery.2010; 17(1): 13. CrossRef
- A Review of Korean Medicine Treatment for Managing the Thoracolumbar Compression Fractures: A Retrospective Observational Study
- 677 View
- 2 Download
- 5 Crossref

- Vertebroplasty on osteoporotic compression fracture
- Chunghwan Kim, Youngjoon Choi, Seungki Baek, Hyungsun Ahn, Jaekwang Hwang, Sujung Choi, Jaiwoo Cho, Kyeungjune Park, Hyeuntae Ahn
- J Korean Soc Fract 2002;15(2):123-128. Published online April 30, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.2.123
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Percutaneous vertebroplasty is the procedure of bone cement injection and allogenous bone graft for pain relief in case of compression fracture, hemangioma etc. Recently, osteoporotic compression fracture increases as the old age increase. We analyzed the postoperative clinical symptoms and radiologic findings.
MATERIALS AND METHODS
From Jan. 2000 to Apr. 2001, we have analyzed 111 osteoporotic compression fractures(59 patients) at Kangneung hospital. Before the procedure, we checked BMD, bone scan and CT. Most common fracture site was the thoracolumbar junction area. Fluoroscopic control was necessary for the cement injection to prevent cement leakage. The amount of cement injection was 4.7ml. We have studied the increase of vertebral body height, symptom recovery time & pain relief, postoperative complications.
RESULT
The vertebral body height was increased from 55.5% to 70.3% postoperatively and the symptom was improved in 48 persons at POD 1, 3 persons at postoperative 2 weeks, and 4 persons at postoperative 2 months. Most common complication was cement leakage to the epidural vessel, disc space, and spinal canal. But serious complication-spinal canal leakage- was only 1 case and had been improved after decompression.
CONCLUSION
Percutaneous vertebroplasty with bone cement(PMMA) is effective treatment in osteoporotic compression fracture, especially in pain relief. -
Citations
Citations to this article as recorded by- Outcome Comparison between Percutaneous Vertebroplasty and Conservative Treatment in Acute Painful Osteoporotic Vertebral Compression Fracture
Hwa-Yeop Na, Young-Sang Lee, Tae-Hoon Park, Tae-Hwan Kim, Kang-Won Seo
Journal of Korean Society of Spine Surgery.2014; 21(2): 70. CrossRef - Adjacent Vertebral Compression Fracture after Percutaneous Vertebroplasty
Chung-Hwan Kim, Jae-Kwang Hwang, Jun-Seok Park
Journal of Korean Society of Spine Surgery.2013; 20(4): 163. CrossRef - The Diagnosis of Osteoporotic Occult Vertebral Fracture and Vertebroplasty
Seong Jun Ahn, Bu Hwan Kim, Moo Ho Song, Seong Ho Yoo, Yeong Joon Kim
Journal of the Korean Fracture Society.2012; 25(3): 208. CrossRef - Factor Analysis Affecting the Leakage of Bone Cement After Vertebroplasty
Jae-Hoon Kim, Kyung-Jin Song, Tai-Seung Kim, Jae-Lim Cho, Ye-Soo Park
Journal of Korean Society of Spine Surgery.2010; 17(1): 13. CrossRef - Treatment of Combined Degenerative Lumbar Disease and Adjacent Vertebral Fracture
Jae-Lim Cho, IL-Hoon Sung, Seung-Wook Baek, Ye-Soo Park
Journal of Korean Society of Spine Surgery.2008; 15(4): 236. CrossRef
- Outcome Comparison between Percutaneous Vertebroplasty and Conservative Treatment in Acute Painful Osteoporotic Vertebral Compression Fracture
- 745 View
- 1 Download
- 5 Crossref

- Comparison Study between Internal Fixation with Compression Hip Screw and Bipolar Hemiarffiroplasty in Unstable Intertrochanteric Fracture
- You Sung Suh, Sai Won Kwon, Ho Won Jung, Jong Seok Park, Byung Ill Lee
- J Korean Soc Fract 2001;14(4):584-591. Published online October 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.4.584
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To define the appropriate treatment of unstable intertrochanteric fracture for aged patients by conducting a clinical and roentgenographical comparative analysis of internal fixation with compression hip screw and primary bipolar hemiarthroplasty.
MATERIALS AND METHODS
38 patients aged 65 or above with intertrochanteric fracture of Singh index below grade III or bone mineral density(BMD) -3.0 who had both severe osteoporosis and unstable fracture, from the period of January 1995 to January 2000. The 38 patients had either internal fixation with compression hip screw(18 cases, Group I) or primary bipolar hemiarthroplasty(20 cases, Group II), and were followed-up for at least one year afterwards. To prevent postoperative complication, early ambulation was permitted as early as possible to both groups.
RESULTS
The average age was 76(range 65-87) for Group I and 79.8(range 78-92) for Group II, respectively. 19 patients were diagnosed to have I-c fracture, following Evans Classification. 35 cases(92.1%) were given grade III or below according to the preoperative Singh index, while all cases showed severe osteoporosis with average bone density of -4.26(-6.95 ~ -2.54). 60% of Group II were given very good or above diagnosis following Merle d'Aubignè's postoperative functional outcome, compared with 16.7% of Group I, thus showed statistic difference of p=0.006. The average for postoperative Harris hip score was also higher with 77 points(range 43-95) for Group I than with 86 points(range 57-94) for Group II, thus showed statistic difference of p=0.0216.
CONCLUSION
For aged patients with unstable intertrochanteric fracture, primary bipolar hemiarthroplasty is considered to have better clinical and roentgenographical results, and able to decrease local and general complications, compared with internal fixation with compression hip screw.
- 308 View
- 0 Download

- Differences of Bone Mineral Density and Fracture Threshold Between Lumbar Spine Fracture and Control group
- Ig Gon Kim, Jae Hyek Kim, Jung Ill Kim, Young Ill Hong
- J Korean Soc Fract 2001;14(2):257-264. Published online April 30, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.2.257
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to show how bone mineral densities of the lumbar spine decrease with aging, to investigate the relationship between the bone mineral densities of the control and fracture group, and to obtain fracture threshold values.
MATERIALS AND METHOD
From January 1995 to December 1999, we measured and evaluated BMD of L3 by DXA in 239 normal volunteers(96 men and 143 women), and in 218 patients with lumbar spine fracture(91 men and 127 women) above 50 years. The Chi-Square test was used for statistical analysis.
RESULTS
1. The average BMD of L3 in control group and lumbar spine fracture group were 0.772+/-0.030 g/cm2 in male and 0.732+/-0 . 0 8 9 g / c m2 i n female and 0.720+/-0 . 0 3 1 g / c m2 in male and 0.692+/-0 . 0 0 2 g / c m2 i n female, respectively.
RESULTS
2. The BMD of the control group and fracture group decreased with aging(p<0.05) and were higher in men than in women. There were statistically significant difference(p<0.001).
RESULTS
3. There were statistically significant difference between BMD of the control group and BMD of the lumbar spine fracture group(p<0.05). The BMD were higher in the control group than fracture group.
RESULTS
4. Fracture threshold of the lumbar spine fracture group were 0.867g/cm2( male: 0.898g /cm2, female:0.836g/cm2) according to 90 percentile.
- 433 View
- 0 Download

- The Surgical Reconstruction of Osteoporotic Vertebral Fractures
- Suck Woo Kim, Yung Khee Chung
- J Korean Soc Fract 2001;14(1):30-36. Published online January 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.1.30
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to analyze the surgical results of 11 patients who underwent posterior instrumentation and anterior interbody fusion using titanium mesh vertebral ring(MOSS) in osteoporotic vertebral fracture. MATERIAL AND METHODS: From May 1997 to July 1999, we checked plain radiographs every 3 months and evaluated the change of kyphotic angle, fusion rate, change of clinical, neurologic symptoms and complications of these patients.
RESULTS
There were only average 0.2 degree correction of preoperative kyphotic angle at last follow-up X-ray. However, we confirmed successful bony fusion at nine of eleven patients(82%) and ten of eleven patients(90.9%) got satisfactory clinical results. Four patients with neurologic symptoms have recovered from their original neurologic status. Only one patient reoperated her back because of displacement of surgical device used in previous operation.
CONCLUSION
Among the surgical treatment methods in osteoporotic vertebral fractures, posterior instrumentation and anterior interbody fusion using titanium mesh vertebral ring(MOSS) is recommended as one of the effective surgical methods in severe osteoporotic patients. -
Citations
Citations to this article as recorded by- Kümmell's Disease Treated with Percutaneous Vertebroplasty: Minimum 1 Year Follow-Up
Jae Won Park, Jong-Hwa Park, Hong Jun Jeon, Jong Young Lee, Byung Moon Cho, Se-Hyuck Park
Korean Journal of Neurotrauma.2017; 13(2): 119. CrossRef - Peculiarities of Treatment of Patients with Complicated Compression Fractures of Thoracic and Lumbar Spine Vertebral Bodies on the Background of Osteoporosis
S T Vetrile, Aleksandr Alekseevich Kuleshov, L Yu Darchiya, S T Vetrile, A A Kuleshov, L Yu Darchiya
N.N. Priorov Journal of Traumatology and Orthopedics.2009; 16(2): 34. CrossRef - Delayed vertebral collapse with neurological deficits secondary to osteoporosis
K-T Kim, K-S Suk, J-M Kim, S-H Lee
International Orthopaedics.2003; 27(2): 65. CrossRef - Surgical Treatment of Kümmell Disease with Neurologic Deficits - Posterolateral Decompression and Posterior Reconstruction -
Ki-Tack Kim, Kyung-Soo Suk, Jin-Moon Kim
Journal of Korean Society of Spine Surgery.2001; 8(2): 136. CrossRef
- Kümmell's Disease Treated with Percutaneous Vertebroplasty: Minimum 1 Year Follow-Up
- 540 View
- 0 Download
- 4 Crossref

- Treatment of trochanteric fractures of the femur in osteoporotic patients
- Joo Tae Park, Chang Sung So, Jae Yong Byun, Kyung Ho You, Ho Yeun Hwang
- J Korean Soc Fract 2001;14(1):16-22. Published online January 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.1.16
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To determine more useful method by comparing the functional recovery and postoperative complications according to operative methods in treatment of unstable trochanteric fracture of the femur with osteoporotic bone.
MATERIALS AND METHODS
Of 45 cases with unstable femoral trochanteric fracture with osteoporosis who had been able to ambulate before injury, we compared postoperative functional recovery and complications between 25 cases treated by cemented bipolar hemiarthroplasty and 20 cases treated by dynamic compression hip screw.
RESULTS
Of 45 cases who had been treated by cemented bipolar hemiarthroplasty and dynamic compression hip screw, the functional results, according to the rating scale of Merle d Aubigne were rated as above good in 23 cases and 14 cases, respectively and postoperative mechanical complications were found in 2 cases and 7 cases, respectively. There was statistically significant difference(P<0.05).
CONCLUSION
Unstable trochanteric fracture of the femur with osteoporotic bone treated by cemented bipolar hemiarthroplasty showed good functional results and few mechanical complications for short term follow-up.
- 405 View
- 2 Download

- Treatment by Composite Fixation of Fractures in Osteoporotic Patients Aged over 60Years
- Keun Woo Kim, Yong Hoon Kim, Hak Jin Min, Ui Seoung Yoon, Hee Oh Kim, Young Joon Ahn, Yoon Jong Kim, Ki Chan Yoo, Sang Rim Kim
- J Korean Soc Fract 2001;14(1):121-127. Published online January 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.1.121
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study summarizes the satisfactory results obtained using a composite fixation method for the surgical treatment of long bone fractures in elderly patients with osteoporosis.
MATERIALS AND METHODS
We reviewed 10 cases of long bone fractures, that were treated by composite fixation, involving patients over 60 years of age that presented with radiological osteoporosis. Composite fixation was applied incorporating, traditional plate and screw fixation in conjunction with bone graft, plate or intramedullary bone cement at four cases of humeral shaft fractures, three cases of femur supracondylar fractures, two cases of femur shaft fractures, and one case of tibia shaft fracture. Results were evaluated in methods of ambulation, range of motion, bony union and complications.
RESULTS
Satisfactory ambulation and range of motion was observed in all cases, which showed bony union without early implant failure. No re-operation were necessary due to nonunion. No medical complication was noted.
CONCLUSION
The results shows that the composite fixation method provided a stable reduction and a rigid fixation, which facilitated bony union, and allowed elderly patients with osteoporosis an early range of motion and mobility after the surgical treatment of long bone fractures.
- 409 View
- 0 Download

- The Result Of Surgical Treatment Of The Femur Unstable Intertrochanteric Fracture Using Compression Hip Screw: Analysis Of Effect Of Degree Of Force On Trauma And Degree Of Osteoporosis
- Ki Do Hong, Sung Sik Ha, Sang Weon Park
- J Korean Soc Fract 2000;13(4):795-803. Published online October 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.4.795
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyise the effect of degree of force on trauma and degree of osteoporosis in femoral unstable intertrochanteric fracture's result of treatment using compression hip screw.
MATERIALS AND METHODS
From January 1993 to December 1997, 55 patients who were operated with compression hip screw and followed up for more than 1 year were devided into high and low energy injured group by the mechanism of the trauma and also devided low(gradeIV,V,VI) and high grade osteoporosis group(gradeI,II,III) by Singh's index. We analize and compare the result of treatment in each groups.
RESULTS
The averrage rate of mechanincal complication was 24%. The mechanical complication rate of the high grade osteoporosis group(34%) was higher than low grade osteoporosis group(9%)(p<0.05). The average subsidence of compression screw was 9.9mm and it shows significant difference between low(7.8mm ) and high grade osteoporosis group(11.5mm )(p<0.05). The average increased varus deformity of neckshaft angel during follow up was 3.8degrees and it shows singnificant defference between high energy injuried group(4.6degrees ) and low energy injuried group(2.7degrees)(p<0.05). No difference was seen in each groups for time of bone union(p>0.05). In view of functional recovery by Clawson's method, no difference between pre-injury and postoperative state was seen in 7 cases(22%) in high grade osteoporosis group and 13 cases(57%) in low grade osteoporosis group, thus worse functional recovery was seen in high grade osteoporosis group.
CONCLUSIONS
We observed higher mechanical complication rate, more compression screw subsidence and worse functional recovery in high grade osteoporosis group and more varus deformity in high energy injured group. Thus we need more attension to treatment and follow up in high energy injured, severe osteoporotic unstable intertrochanteric fracture.
- 406 View
- 1 Download

- Differences of Bone Mineral Density and Fracture Threshold Between Hip Joint Fracture and the Control group
- Ig Gon Kim, Jae Hyek Kim, Cul Hyun Kim, Jong Suck Kim
- J Korean Soc Fract 1999;12(2):231-238. Published online April 30, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.2.231
-
 Abstract
Abstract
 PDF
PDF - Osteoporosis represents reduced amount of bone mass per unit volume as compared with controls of the same age and sex. In this condition, bone mineral density decreases and the skeleton becomes more prone to fracture. The purpose of this study was to show how bone mineral densities of the femoral neck area decrease with aging, to in vestigate the relationship between the bone mineral densities of the control and fracture group, and to obtain fracture threshold values. This report observed BMD of femoral neck region in femoral neck and intertrochanteric fracture group was less than that of control group and the differences were significant. We measured and evaluated BMD of femoral neck region by DEXA in 234 normal volunteers(99 men and 135 women), in 105 patien ts with femoral neck fracture(41 men and 64 women) and in 103 patients with intertrochanteric fracture(40 men and 63 women) above 50 years-old. Following results were obtained: 1. The average BMD of femoral neck region in control group, femoral neck fracture group and intertrochanteric fracture group were 0.751+/-0.030 g/cm2 in male and 0.661+/-0.089g/cm2 in female, 0.660+/- 0.031g/cm2 in male and 0.557+/-0.002g/cm2 in female and 0.661+/-0.008g/cm2 in male and 0.562+/-0.005g/cm2 in 2. The BMD of the control group and fracture group decreased with aging and were higher in men than in women and there were statistically significant difference(p<0.001). 3. There were statistically significant difference between BMD of the control group and BMD of the hip fracture group(p<0.005) but no significant differences between BMD of the femoral neck fracture group and intertrochanteric fracture group. 4. Fracture threshold of the hip fracture group were 0.815g/cm2(male:0.832g/cm2, female:0.733g/cm2) according to 95 percentile.
- 448 View
- 2 Download

- Diffrences of Bone Mineral Density between Osteoporotic Group with or without Compression Fracture of the Spine
- Eu Sub Jung, Young Ki Lee, Seung Ill Baek
- J Korean Soc Fract 1998;11(3):629-633. Published online July 31, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.3.629
-
 Abstract
Abstract
 PDF
PDF - Osteoporosis is the metabolic bone disease and the bone is easily fracture by minimal stress due to decreased bone mass. It gets to attract more and more interest due to surprisingly high incidence and prevalence as well as its complications, fracture. We compared the bone mineral density between 45 osteoporotic patients group with compression fractures of the spine, 105 osteoporotic patients group without fractures and 45 normal control group using dual energy X-ray absorptiometry. We obtained following results. 1. There are statistically no significant differences between bone mineral density of the osteoporotic group with compression fracture of the spine and bone mineral density of the osteoporotic group without fractures. 2. Height and weight had statistically significant correlation with bone mineral density of the lumbar spine anteroposterior view, lateral view and Ward triangle. 3. Fracture threshold of the lumbar spine anteroposterior view, lateral wiew and Ward triangle are 0.884g/cm2, 0.694g/cm2 and 0.514g/cm2 according to 90percentile, 0.979g/cm2, 0.732g/cm2, 0.545g/cm2 according to 95percentile.
-
Citations
Citations to this article as recorded by- Subsequent Hip Fracture in Osteoporotic Hip Fracture Patients
Sang Ho Lee, Tong Joo Lee, Kyu Jung Cho, Sang Hyun Shin, Kyoung Ho Moon
Yonsei Medical Journal.2012; 53(5): 1005. CrossRef
- Subsequent Hip Fracture in Osteoporotic Hip Fracture Patients
- 556 View
- 0 Download
- 1 Crossref

- Treatment of Intertrochanteric Fractures of the Femur using Compression Hip Screw in the Senile Osteoporosis
- Eui Hwan Ahn, In Whan Chung, Jeong Hwan Oh, Hyuck Jun Lee
- J Korean Soc Fract 1998;11(1):168-174. Published online January 31, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.1.168
-
 Abstract
Abstract
 PDF
PDF - The intertrochanteric fracture of the femur are seen in elderly patients who are highly vulnerable to generalized osteoporosis and various senile disease. Firm internal fixation and early ambulation is a goal of treatment. The morbidity and mortality after fracture remain high despite of the development of various devices. For this purpose, compression hip screw becomes popular recently. The purpose of this report is to assess the availability of compression hip screw in the intertrochanteric fracture in the senile osteoporosis by the review of 107 cases from Jan. 1990 to Jan. 1996. The result were as follows : 1. Eighty-three cases(77.6%) were unstable fractures. 2. The lag screw position in the femoral head of 76 cases(71%) were centerd 3. The average length of sliding of the lag screw was 9.9mm. 4. Satisfactory results were obtained in 91% of patients by the functional class of Clawson.
- 447 View
- 0 Download

- Interlocking Intramedullary Nail Fixation for Tibiotalocalcaneal Fusion(2 cases)
- Young Ki Chung, Jung Han Yoo, Sung Il Shin, Yong Wook Park, Dong Cheol Pyo
- J Korean Soc Fract 1997;10(4):860-865. Published online October 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.4.860
-
 Abstract
Abstract
 PDF
PDF - Multiple fixation techniques for tibiotalocalcaneal arthrodesis have been introduced. The interlocking intramedullary nailing for tibiotalocalcaneal osteoarthritis with osteoporosis permits excellent internal fixation. We had two retrograde interlocking intramedullary nail fixation for tibiotalocalcaneal arthrodesis. One patient is chronic infectious osteoarthritis of the ankle and subtalar joints. And the other is non-union of the distal tibia with arthrofibrosis of the ankle and subtalar joints. Two patients also had osteoporosis due to long immobilization. The follow up period were 12 and 22 months respectively. The leg and foot is aesthetically pleasing and the musculature around the ankle and foot is maintained in the normal balanced position after the tibiotalocalcaneal fusion. So, we believed that the interlocking intramedullary nailing is an excellent treatment method for tibio talocalcaneal arthritis with osteoporosis.
- 423 View
- 0 Download

- Treatment of Intertrochanteric Fractures of femur in Elderly Patient with Osteoporosis
- Chung Nam Kang, Jin Man Wang, Kwon Jae Roh, Jong Oh Kim, Yeo Hon Yun, Seok Beom Lee, Dong Jun Kim, Chung Hyok Choi, Dong Wook Kim, Seok Woo Kim
- J Korean Soc Fract 1994;7(2):404-411. Published online November 30, 1994
- DOI: https://doi.org/10.12671/jksf.1994.7.2.404
-
 Abstract
Abstract
 PDF
PDF - With the age of our population advancing, the number of elderly osteoporotic patients with comminuted intertrochanteric fractures of the femur has increased dramatically. Intertrochanteric fractures of the femur usually occur in a more elderly age group than femoral neck fractures of the femur usually occur in a more elderly age group than femoral neck fractures. Intertrochanteric fractures are best treated by intenal fixation, since this mehod provides satisfactory positioning of the fragments and obviates the hazards of recumbency. However, in some caces with severe osteoporosis, arthroplasty is an excellent altemative to the internal fixation. From 1987 to 1992, thirty-six intertrochanteric fractures of femur in the elderly patients(over 60 years of age) were treated by operation at the department of orthopaedic surgery in the Ewha Womans University Hospital. Thirty-three caces were internally fixated with the sliding-compression hip screws-plates(30), the Gamma interlocking intramedullary nails(2), the Rohs plate(1), and in three caces endoprosthetic or total hip replacement arthroplaties were performed.
- 442 View
- 1 Download

- Cases of bipolar endoprosthetic replacement of unstable intertrocha nteric femoral fracture in the elderly, osteoporotic patients
- Yong Baek Kim, Jae Chang Lee, Jae Do Kim
- J Korean Soc Fract 1991;4(2):289-292. Published online November 30, 1991
- DOI: https://doi.org/10.12671/jksf.1991.4.2.289
- 393 View
- 1 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


