Search
- Page Path
- HOME > Search
Original Articles
- The clinical outcome of treating elderly distal radius fractures by long volar locking plate with the elimination of irreducible metaphyseal comminuted volar cortical fragments: a retrospective case series
- Soo Min Cha
- J Musculoskelet Trauma 2025;38(1):13-22. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00003

-
 Abstract
Abstract
 PDF
PDF - Background
In severe comminuted metaphyseal distal radius fracture (DRF) of elderly patients, after maintaining only radiological parameters of the radius using long volar locking plates (VLPs), we inevitably eliminated a few volar cortical fragments of metaphysis. Here, we report the final radiological and clinical outcomes of our method. Methods: For the patients who were treated between 2014 and 2018, the demographic factors, the preoperative radiologic factors, area of the eliminated volar cortical fragment, and final radiologic parameter, were evaluated. Clinical outcomes and ranges of active motion were evaluated. Results: In total, 31 patients were included. The mean patient age was 77.3 years and the mean eliminated cortical area was 3.30 cm2. At the final follow-up, the mean volar tilt, radial inclination, articular step-off, and ulnar variance were 10.35°, 20.00°, 0.58 mm, and 0.71 mm, respectively. There were no definitive correlations between bone mineral density, fragment area, the largest cortical fragment diameter ratio and differences in final and immediate postoperative measurements of these radiological parameters, respectively. Visual analog scale and disabilities of the arm, shoulder, and hand (DASH) scores were satisfactory, and the mean arcs of flexion-extension and pronation-supination were 124.35° and 133.23°. Clinical outcomes were not significantly different according to the AO system category. Conclusions: For maintenance of radiological parameters of the radius, long VLPs are useful in older patients with DRFs who exhibit volar metaphyseal comminution, despite concurrent ulnar fractures. Inevitable elimination of irreducible free comminuted cortical fragments when filling the defect does not affect final radiological and clinical outcomes. Level of evidence: Level IV, case series.
- 1,092 View
- 40 Download

- Does the Operator’s Experience Affect the Occurrence of Complications after Distal Radius Fracture Volar Locking Plate Fixation? A Comparative Study of the First Four Years and Thereafter
- Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
- J Musculoskelet Trauma 2024;37(4):175-183. Published online October 25, 2024
- DOI: https://doi.org/10.12671/jmt.2024.37.4.175
- Correction in: J Musculoskelet Trauma 2025;38(1):40
-
 Abstract
Abstract
 PDF
PDF - Purpose
The management of distal radius fractures (DRFs) has evolved with the introduction of volar locking plate (VLP) fixation, offering stable fixation and better outcomes. Nevertheless, the impact of the surgeon’s experience on the complication rates in VLP fixation remains to be determined, particularly for less-experienced surgeons. This study compared the complication rates during the initial four years and subsequent two years of a hand surgeon’s practice of VLP fixation for DRFs.
Materials and Methods
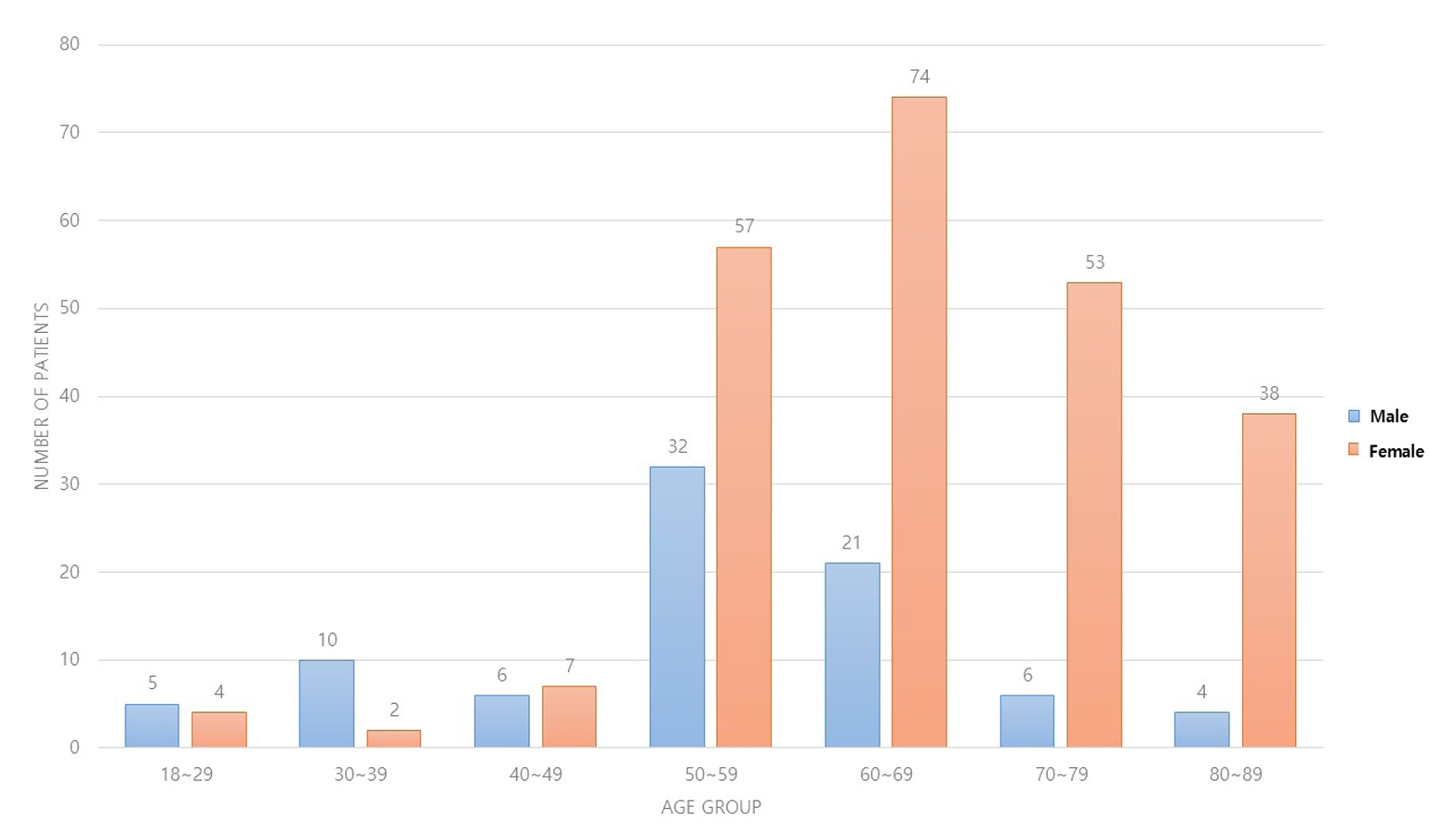
The data between March 2016 and December 2022 were analyzed retrospectively under the Institutional Review Board approval. A single surgeon performed all VLP fixation surgeries after finishing regular hand surgery training, with the first four years representing the less experienced phase (Group 1) and the following two years indicating the experienced phase (Group 2). The patients’ characteristics, operation-related factors, and postoperative complications, including tendon injuries, nerve-related complications, fixation and instrument-related issues, osteosynthesis-related problems, and infections, were compared. In addition, the authors compared the data with a large multicenter study conducted by experienced hand surgeons.
Results
Three hundred and nineteen patients (321 wrists) were included. The mean age was 63.3 years, and 26.3% were male and 73.7% were female. The operation time was 53.7±14.5 minutes and 74.4±26.5 minutes in groups 1 and 2, respectively, which was statistically significantly shorter (p<0.001). The complication rates between the two groups were similar, except for the higher implant removal rates in Group 1. A comparison with a previous multicenter study revealed higher reduction losses and carpal tunnel syndrome in this study, but the overall complication rate was low.
Conclusion
In DRF management, when the operating surgeon has completed an accredited training course, VLP fixation is a good treatment method that can be performed effectively even by less experienced surgeons with low complication rates. -
Citations
Citations to this article as recorded by- Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2025; 38(1): 40. CrossRef - Characteristics of patients with distal radius fracture requiring arthroscopic foveal repair after bone union
Min Jung Park, Cheungsoo Ha, Hyun Tak Kang, Yong Hyun Yoon, Jun-Ku Lee, Soo-Hong Han
Arthroscopy and Orthopedic Sports Medicine.2025; 12(2): 70. CrossRef
- Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
- 2,456 View
- 52 Download
- 2 Crossref

- Demographic and Radiographic Parameters as Predictors of Reduction Loss after Conservative Treatment of Distal Radius Fractures in Adults
- Kyu Jin Kim, Dae Won Shin, Seong Kee Shin
- J Korean Fract Soc 2023;36(2):45-51. Published online April 30, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.2.45
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the demographic and radiological risk factors for later reduction loss of distal radius fractures treated conservatively. Materials and Methods This study enrolled patients treated for distal radius fractures between January 2017 and December 2019. Seventy-eight patients were included in the analysis and divided into two groups. The patients who showed minimal reduction loss within an acceptable radiologic angle after initial manual reduction were classified as Group A. The patients who showed reduction loss out of an acceptable radiologic angle and finally malunited or converted to surgical treatments were classified as Group B. The patient’s age and bone marrow density were used as demographic data. The initial X-ray images were evaluated to determine the fracture type. Various radiological parameters were measured. Results The 78-patient study cohort consisted of nine men and 69 women with a mean age of 67 years. Forty-eight cases were sorted into Group A, and 30 cases into Group B. On logistic regression analysis, the age of 80 or older was a risk factor for later fracture displacement among the demographic factors (p=0.037, odds ratio=4.937). Among the radiographic factors, the presence of distal ulnar fracture and dorsal cortical comminution were disclosed as risk factors of later displacement (p=0.049, 0.003, odds ratio=3.429, 7.196). Conclusion When conservative management for distal radius fracture is decided in patients more than 80 years of age or accompanied by a distal ulnar fracture or with dorsal cortical comminution, the possibility of later displacement of the distal radius should be considered.
- 448 View
- 1 Download

Review Article
- Pediatric Fractures around the Wrist
- Gihun Kim, Kun-Bo Park
- J Korean Fract Soc 2021;34(2):80-86. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.80
-
 Abstract
Abstract
 PDF
PDF - Fractures around the wrist are the third most common fracture among all pediatric fractures. Furthermore, distal radius fractures, a type of wrist fracture, are the most common fractures in children. Understanding pediatric fractures around the wrist is very important considering their prevalence. There is a specific belief that pediatric fractures can heal easily because of remodeling, but not all fractures can heal without proper treatment. Complications such as growth problems, nonunion can occur if the fracture is not treated properly. This paper reviewed recent articles about distal radius fractures, Galeazzi-equivalent fractures, and carpal bone fractures, including scaphoid fractures in children and adolescents. Successful treatment can be achieved without complications when an accurate diagnosis and proper non-surgical or surgical treatment are performed based on this article.
- 1,254 View
- 25 Download

Original Articles
- Primary Open Reduction and Plate Fixation in Open Comminuted Intra-Articular Distal Radius Fracture
- Jun-Ku Lee, Soonchul Lee, Weon Min Cho, Minkyu Kil, Soo-Hong Han
- J Korean Fract Soc 2021;34(1):16-22. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.16
-
 Abstract
Abstract
 PDF
PDF - Purpose
There are no standard surgical treatments for open distal radius fractures (DRFs), and the fracture fixator is chosen by the surgeon’s own experience. This study compared the outcomes of open reduction and volar locking plating (OR VLP) between closed and open AO-OTA type C3 DRFs. Materials and Methods: Patient data were retrospectively collected between January 2010 and December 2018. Only patients aged >18 years with AO-OTA C3 DRFs were included. After further exclusion, the patients with DRFs were divided into two groups: 13 patients with open DRFs in Group 1 and 203 patients with closed DRFs in Group 2. Data on the patient characteristics and treatment-related factors were further investigated. For the radiological evaluation, the radial height, volar height, and volar titling were measured based on the final plain radiography, and the union time was measured. The wrist range of motion (ROM), pain visual analogue scale score, and modified Mayo wrist score for function were measured at the final outpatient follow-up. Finally, the complications associated with OR VLP fixa-tion were investigated. Results: In the demographic comparison, the patients with open fractures were older (mean age, 62years) than those with closed fractures (mean age, 57 years), without a statistically significant differ-ence. The patients with open DRFs had longer antibiotic therapy and hospital stay durations. Although they presented a higher radial inclination, with statistical significance, the clinical implication was low with a mean difference of 3°. No significant differences were observed for the remaining radiological parameters, wrist ROM, and functional scores. An open DRF did not increase the complication rates,including deep infection. Conclusion: Depending on the expertise of the operating surgeon, the primary OR VLP fixation in open intra-articular comminuted DRF did not increase the incidence of deep infections and yielded similar outcomes to a closed intra-articular comminuted DRF.
- 960 View
- 10 Download

- Results of Single Small Incision Minimally Invasive Plate Osteosynthesis in the Treatment of the Distal Radius Fractures
- Young Sung Kim, Jong Pil Kim, Phil Hyun Chung, Ho Min Lee, Bo Sung Go
- J Korean Fract Soc 2020;33(2):72-80. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.72
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared minimally invasive plate osteosynthesis (MIPO) using a single small skin incision and conventional open volar locking plate fixation (OP) for distal radius fracture to identify outcome difference.
Materials and Methods
Forty-three patients who underwent MIPO using a single small skin incision or OP for distal radius fractures were evaluated retrospectively. Of the patients, 21 were treated with MIPO using a single small skin incision and 22 with the OP method through the conventional volar approach. The postoperative radiographic results and clinical outcomes at the final follow-up in each group were compared.
Results
All patients achieved bone union in the MIPO and OP groups. No significant differences in the bone union time, alignment, range of motion, QuickDASH, or pain score were observed. On the other hand, the size of the incision was significant: 23 mm in the MIPO group and 55 mm in the OP group (p<0.001).
Conclusion
MIPO technique using a single small incision showed similar satisfactory radiographic and functional outcomes compared to conventional OP for distal radius fractures. The MIPO technique using a single small incision offered advantages, including cosmetic benefits and minimal soft tissue damage, is recommended, particularly in young women and high functional demand patients.
- 596 View
- 8 Download

Case Report
- Tension Band Wiring Technique for Distal Radius Fracture with a Volar Articular Marginal Fragment: Technical Note
- Neunghan Jeon, Jong Keon Oh, Jae Woo Cho, Youngwoo Kim
- J Korean Fract Soc 2020;33(1):38-42. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.38
-
 Abstract
Abstract
 PDF
PDF - Most distal radius fractures are currently being treated with anterior plating using anatomical precontoured locking compression plates via the anterior approach. However, it is difficult to fix the volar articular marginal fragment because these anatomical plates should be placed proximally to the watershed line. There were just a few methods of fixation for this fragment on medical literature. Herein, we introduced a tension band wiring technique for fixation of a volar articular marginal fragment in the distal radius.
-
Citations
Citations to this article as recorded by- Hook plate versus periarticular-type volar locking plate for distal radius fractures involving the volar lunate facet in Korea: a retrospective cohort study
Hyun-Jae Park, Joo-Hak Kim
Journal of Musculoskeletal Trauma.2025; 38(4): 221. CrossRef
- Hook plate versus periarticular-type volar locking plate for distal radius fractures involving the volar lunate facet in Korea: a retrospective cohort study
- 698 View
- 6 Download
- 1 Crossref

Original Articles
- Use of Miniplate for Severe Comminuted Metadiaphyseal Fractures of the Distal Radius
- Jong Ryoon Baek, Yong Cheol Yoon, Seung Hyun Baek
- J Korean Fract Soc 2019;32(4):204-210. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.204
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study investigated the clinical and radiological outcomes of patients undergoing provisional fixation in conjunction with locking plate fixation. Miniplates were used as the reduction plates for the surgical treatment of severe comminuted metadiaphyseal fractures with an intra-articular fracture of the distal radius.
MATERIALS AND METHODS
The radial length, radial inclination, volar tilt, and radial intra-articular step-off were measured preoperatively, postoperatively, and at one year after surgery in 12 patients (eight males, four females, mean age 55.4 years old). The patients underwent volar locking plate fixation with miniplate as a reduction plate for severe comminuted metadiaphyseal fractures with an intra-articular fracture of the distal radius. Clinical evaluations were conducted using the modified Mayo wrist score (MMWS).
RESULTS
Bone union was achieved in all cases. The mean MMWS was 81.8 points, including two excellent, three good, and seven fair cases. Radiological improvements were observed in the average radial length (preoperative, 6.4 mm; postoperative, 11.8 mm), average radial inclination (10.2° to 22.4°), average volar tilt (−4.5° to 10.6°), and average radial intra-articular step-off (4.8–0.8 mm) (all, p<0.05). Radiographic measurements obtained immediately after surgery and at the final follow-up revealed insignificant decreases in radial length (0.6 mm), radial inclination (0.4°), and volar tilt (0.9°) (all, p>0.05).
CONCLUSION
Miniplate fixation can be an effective treatment option as a reduction plate for the treatment of distal radial fractures, which is challenging to reduce and maintain due to severely comminuted metadiaphysis fractures with the intra-articular fracture.
- 623 View
- 3 Download

- A Comparison of the Results between Internal Fixation and External Fixation in AO C Type Distal Radius Fractures
- Yoon min Lee, Hwa Sung Lee, Seok Whan Song, Jae Hoon Choi, Jong Tae Park
- J Korean Fract Soc 2018;31(3):87-93. Published online July 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.3.87
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to evaluate the radiological and clinical results of plate fixation and external fixation with additional devices for treating distal radius fracture in AO type C subtypes, and propose a treatment method according to the subtypes.
MATERIALS AND METHODS
Two hundred and one AO type C distal radius fracture patients were retrospectively reviewed. Eighty-five patients in group 1 were treated with volar or dorsal plate, and 116 patients in group 2, were treated with external fixation with additional fixation devices. Clinical (range of mtion, Green and O'Brien's score) and radiological outcomes were evaluated.
RESULTS
At the 12-month follow-up, group 1 showed flexion of 64.4°, extension of 68.3°, ulnar deviation of 30.6°, radial deviation of 20.8°, supination of 76.1°, and pronation of 79.4° in average; group 2 showed flexion of 60.5°, extension of 66.9°, ulnar deviation of 25.5°, radial deviation of 18.6°, supination of 73.5°, and pronation of 75.0° in average. The mean Green and O'Brien score was 92.2 in group 1 and 88.6 in group 2. The radial height of group 1 and group 2 was 11.6/11.4 mm; radial inclination was 23.2°/22.5°; volar tilt was 11.6°/8.7°; and the ulnar displacement was 1.27/0.93 mm.
CONCLUSION
Judicious surgical techniques during device application and tips for postoperative management during external fixation can produce similar clinical results compared with internal fixation patients. -
Citations
Citations to this article as recorded by- Intra-articular fracture distal end radius external fixation versus locking volar radius plate: A comparative study
S.P.S Gill, Manish Raj, Santosh Singh, Ajay Rajpoot, Ankit Mittal, Nitin Yadav
Journal of Orthopedics, Traumatology and Rehabilitation.2019; 11(1): 31. CrossRef
- Intra-articular fracture distal end radius external fixation versus locking volar radius plate: A comparative study
- 443 View
- 1 Download
- 1 Crossref

Review Article
- Nonsurgical Treatment of a Distal Radius Fracture: When & How?
- Young Ho Shin, Jun O Yoon, Jae Kwang Kim
- J Korean Fract Soc 2018;31(2):71-78. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.71
-
 Abstract
Abstract
 PDF
PDF - Distal radius fractures are a common upper extremity fracture and a considerable number of patients have a stable fracture. In the treatment of distal radius fractures, there is considerable disagreement regarding the need for a strict anatomical restoration with operation in elderly patients. Therefore, nonsurgical treatment is a still important treatment option in distal radius fractures. The radiological parameters of before or after manual reduction are important for deciding whether to perform operation or not. The radiological parameters include dorsal angulation of the articular surface, radial shortening, extent of dorsal comminution, intra-articular displacement, concomitant ulnar metaphyseal fracture, shear fracture, and fracture-dislocation of the distal radio-ulnar joint. In addition, clinical situations of patients, including age, activity level, underline disease, and recovery level, which the patients wish should be considered, comprehensively. For the duration of a splint or cast, three to four weeks are recommended in impacted or minimally displaced fractures and five to six weeks in displaced fractures. After reduction of the displaced fractures, patients should undergo a radiologicical examination every week to check the redisplacement or deformity of the fracture site until two or three weeks post trauma. Arm elevation is important for controlling fracture site swelling and finger exercises, including metacarpophalangeal joint motion, are needed to prevent hand stiffness. Active range of motion exercise of the wrist should be initiated immediately after removing the splint or cast.
-
Citations
Citations to this article as recorded by- The Clinical Effect of Complex Korean Medical Admission Treatment in Patients with Fractures of Distal Radius by Traffic Accident: 2 Cases Series Report
Gyu-cheol Choi, Ji-won Lee, Ji-Eun Bae, Dong-jin Kim, Jeong-su Hong, Da-hyun Kyung
Journal of Korean Medicine Rehabilitation.2021; 31(1): 187. CrossRef - The Clinical Effect of Rehabilitation Protocol for Distal Radius Fracture in Korean Medicine: A Report of 3 Cases
Won-Bae Ha, Ji-Hye Geum, Nak-Yong Koh, Jung-Han Lee
Journal of Korean Medicine Rehabilitation.2018; 28(3): 97. CrossRef
- The Clinical Effect of Complex Korean Medical Admission Treatment in Patients with Fractures of Distal Radius by Traffic Accident: 2 Cases Series Report
- 465 View
- 7 Download
- 2 Crossref

Original Articles
- Anatomical Reduction with Brick-Work Technique in Comminuted Intraarticular Distal Radius Fractures
- Hyoung Min Kim, Hyung Lae Cho, Jong Woo Chae, Myung Ji Shin
- J Korean Fract Soc 2018;31(1):1-8. Published online January 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study examined the clinical outcomes of comminuted intraarticular distal radius fractures treated by an anatomical reduction using a brick-work technique.
MATERIALS AND METHODS
Seventeen patients with AO/OTA type 23-C3 distal radius fractures were enrolled in this study. An anatomical reduction of the articular surface was achieved using a brick-work technique through the dorsal approach and dorsal plates were used for fixation. The postoperative functional results were assessed with the range of motion of the wrist and the modified Mayo wrist score (MMWS). In addition, the radial length, radial inclination, volar tilt, and Lidstrom score were evaluated from the radiology results. The mean postoperative follow-up period was 13.6 months.
RESULTS
All patients showed bony union and the mean range of motion of the injured wrists was 94% (92% to 95%) of the uninjured side. The mean MMWS was 85.3, and the functional results were excellent in 12 patients, good in 4, and fair in one at the final follow-up. Based on the final radiographic measurements, the radial length, volar tilt, and radial inclination were 11.4 mm (10.0 to 13.5 mm), 6.6° (−1.8° to 9.2°), and 21.3° (20.1° to 25.7°), respectively. The radiologic results according to the Lidstrom score were excellent in 14 patients and good in three.
CONCLUSION
An anatomical reduction with the brick-work technique is relatively easy, results in a reproducible clinical outcome, and could be a safe and effective treatment option for severe comminuted intraarticular distal radius fractures that are not amenable to volar plate fixation.
- 294 View
- 1 Download

- Ultrasonographic Assessment of the Pronator Quadratus Muscle after Surgical Treatment for Distal Radius Fractures
- Dong Hyuk Choi, Hyun Kyun Chung, Ji Won Lee, Cheol Hwan Kim, Yong Soo Choi
- J Korean Fract Soc 2017;30(2):69-74. Published online April 30, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.2.69
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study was to assess the morphological changes of the pronator quadratus (PQ) muscle using an ultrasonography in the volar locking plate fixation group and in the percutaneous K-wire fixation group for distal radius fracture, and to evaluate the impact on clinical outcomes.
MATERIALS AND METHODS
Fifty-four patients who received surgical treatment for distal radius fracture were enrolled in this study. They were divided into two groups according to treatment modality: Group 1 included 34 patients who underwent internal fixation with volar locking plate and Group 2 included 20 patients with percutaneous K-wire fixation. Thickness of the PQ muscle was measured using an ultrasonography at the final follow-up. We evaluated the outcomes using the Mayo wrist score, wrist range of motion, and grip strength at the final follow-up.
RESULTS
Compared with the uninjured side, thickness of the PQ muscle showed 31.9% of mean atrophy in Group 1 and 11.4% in Group 2. The atrophy of PQ muscle was severe in Group 1 (p=0.01). However, there was no significant difference in the mean Mayo wrist score between the two groups (83.1±10.9 in Group 1 and 80.2±8.9 in Group 2, p=0.28), except a mild limitation of pronation in Group 1.
CONCLUSION
The healed PQ muscle from fracture itself after distal radius fracture revealed a morphological atrophy. Moreover, the volar locking plate resulted in greater atrophy of the PQ muscle, but there was no specific impact on clinical outcomes. -
Citations
Citations to this article as recorded by- Quantitative analysis of radial torsion angle according to location with CT scan
Eic Ju Lim, Seungyeob Sakong, Jeong Seok Choi, Wonseok Choi, Jong-Keon Oh, Jae-Woo Cho
Injury.2025; 56(10): 112634. CrossRef
- Quantitative analysis of radial torsion angle according to location with CT scan
- 614 View
- 6 Download
- 1 Crossref

- Radiologic Analysis of Distal Radius Fracture Accompanying Spontaneous Extensor Pollicis Longus Rupture
- Jun Ku Lee, In Tae Hong, Young Woo Kwon, Gyu Chol Jang, Soo Hong Han
- J Korean Fract Soc 2017;30(2):63-68. Published online April 30, 2017
- DOI: https://doi.org/10.12671/jkfs.2017.30.2.63
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The spontaneous extensor pollicis longus (EPL) tendon rupture is a well-documented complication of non-displaced or minimally displaced distal radius fracture. Authors analyzed the radiographs of patients treated for closed EPL rupture after distal radius fracture.
MATERIALS AND METHODS
Twenty-eight patients (21 females, 7 males; average age of 58 years) with tendon transfer for spontaneous rupture of EPL after distal radius fracture were included. Wrist radiographs were taken at the first visit with EPL rupture. On the lateral view, posterior cortical displacement, distance from highest point in Lister's tubercle to fracture line, and height of the Lister's tubercle were measured. The distance from the lunate facet to the fracture line was measured on anteroposterior view. Radiologic change at the time of EPL rupture around the Lister's tubercle was evaluated by comparing it with the contra lateral wrist radiograph. Radial beak fracture pattern was also identified.
RESULTS
The interval between the injury and the spontaneous EPL rupture varied from 2 to 20 weeks, with an average of 6.7 weeks. There were 25 cases of non-displacement, 3 cases of mean 2.0 mm cortical displacement. The average distance from the lunate facet to the fracture line was 9.1 mm (3-12.1 mm), from the highest point in Lister's tubercle to the fracture line was 3.0 mm toward proximal radius (1.7-4.9 mm). The average height of the Lister's tubercle was 3.4 mm in the injured wrist and 3.1 mm in the opposite wrist. Radial beak fracture pattern was shown at 11 cases.
CONCLUSION
All cases presented no or minimal displaced fracture, and the fracture line was in the vicinity of the Lister's tubercle. Those kinds of fractures can highlight the possibility of spontaneous EPL rupture, depites its rarity.
- 500 View
- 2 Download

- Outcomes of Severe Comminuted Distal Radius Fractures with Pronator Preserving Approach
- Seung Hyun Cho, Hong Gi Park, Deuk Soo Jun, Jae Ang Sim, Young Hak Roh, Yong Cheol Yoon, Jong Ryoon Baek
- J Korean Fract Soc 2015;28(3):178-185. Published online July 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.3.178
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We investigate the outcomes of treatment of patients with severe comminuted distal radius fractures with volar plate fixation using a pronator-preserving approach.
MATERIALS AND METHODS
Fourteen patients with severe comminution of the distal radius fractures for whom anatomical reduction of the fractures was deemed difficult to achieve with traditional approaches were enrolled. The gender ratio was 8 males to 6 females, and the average age of the patients was 64.9 years. According to the AO/OTA classification of fractures, 2 patients had 23-A3 fractures, 7 patients had 23-C2, and 5 patients had 23-C3. Radial length, radial inclination, and volar tilt were measured for radiologic evaluation. Modified Mayo wrist score (MMWS) was used for clinical outcome.
RESULTS
Bony union was achieved in all 14 patients without signs of complications. The average time-to-union was 4.3 months (3-6 months). The radiological findings at the final follow-up were as follows: the average radial inclination was 20.5degrees; the average volar tilt, 7.57degrees; and the average radial length, 11.8 mm. At the final follow-up, the results of the MMWS were 'Fair' in 1 patient, 'Good' in 4, and 'Excellent' in 9.
CONCLUSION
We propose that a pronator-preserving approach is an effective treatment for severe comminuted distal radius fracture. -
Citations
Citations to this article as recorded by- Use of Miniplate for Severe Comminuted Metadiaphyseal Fractures of the Distal Radius
Jong-Ryoon Baek, Yong-Cheol Yoon, Seung Hyun Baek
Journal of the Korean Fracture Society.2019; 32(4): 204. CrossRef
- Use of Miniplate for Severe Comminuted Metadiaphyseal Fractures of the Distal Radius
- 692 View
- 1 Download
- 1 Crossref

- Treatment of the Communited Distal Radius Fracture Using Volar Locking Plate Fixation with Allogenic Cancellous Bone Graft in the Elderly
- Je Kang Hong, Chang Hyun Shin
- J Korean Fract Soc 2015;28(1):8-16. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.8
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We studied results of the communited distal radius fracture treated with allogenic cancellous bone graft and volar locking plate in the elderly.
MATERIALS AND METHODS
We studied 29 cases of communited distal radius fracture treated with allogenic cancellous bone graft and volar locking plate from April 2009 to April 2013. Fracture was classified according to AO/OTA classification. Postoperative clinical evaluation was performed with measurement of wrist range of motion (ROM) at last follow-up, modified Mayo wrist scoring system (MMWS), and visual analogue pain scale (VAS). Radiologic evaluation was performed with measurement of radial length on immediate postoperation and last follow-up, radial inclination, volar tilt and ulnar variance checked at the last follow-up using Sarmiento criteria.
RESULTS
Using the MMWS, 13 cases were classified as 'good', 10 'fair', and 5 'normal'. The average wrist ROM was 88.5% for flexion, 92.2% for extension, 90.5% for adduction, and 94.0% for abduction. The average VAS was 1.7. On the last follow-up, average radius length, radial inclination and volar tilt did not show statistically significant improvement (p>0.05) compared to immediate post operation measurements, and according to Sarmiento criteria, 5 cases were classified as 'good', 14 'fair', and 7 'normal'.
CONCLUSION
Treatment of severe communited distal radius fracture accompanied by bone defect with volar locking plate and allogenic cancellous bone graft is a satisfying and effective treatment method in the elderly.
- 731 View
- 3 Download

- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
- Jae Cheon Sim, Sung Sik Ha, Ki Do Hong, Tae Ho Kim, Min Chul Sung
- J Korean Fract Soc 2015;28(1):46-52. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.46
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate outcome of variable-angle volar locking plate for treatment of distal radius fractures.
MATERIALS AND METHODS
We retrospectively analyzed the results in 45 cases treated by variable-angle volar locking plate. We evaluated the clinical results according to the Mayo wrist performance scoring system and radiographic results.
RESULTS
All cases had bony union. The mean Mayo wrist performance scoring system was 84.8. Between preoperative and immediate postoperative radiographic measurement, the mean radial length improved from 8.4 to 11.8 mm, radial inclination from 14.2degrees to 22.4degrees, volar tilt from -4.5degrees to 9.6degrees, and intraarticular step-off from 1.8 to 0.3 mm (p<0.05). Between immediate postoperative and latest follow-up radiographic measurements, the mean loss of radial length measured 0.8 mm, radial inclination 0.4degrees, and volar tilt 0.9degrees (p>0.05). All cases showed bone union with no evidence of malunion, nonunion, or metal failure.
CONCLUSION
Treatment of distal radius fractures using variable angle volar locking plate showed satisfactory outcomes. It is a good option to obtain stable fixation without significant loss of reduction.
- 472 View
- 3 Download

- The Surgical Outcome of Unstable Distal Clavicle Fractures Treated with 2.4 mm Volar Distal Radius Locking Plate
- Suk Kyu Choo, Ji Ho Nam, Youngwoo Kim, Hyoung Keun Oh
- J Korean Fract Soc 2015;28(1):38-45. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.38
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study evaluated the surgical outcomes of unstable distal clavicular fractures treated with a 2.4 mm volar distal radius locking plate.
MATERIALS AND METHODS
From August 2009 to August 2012, 16 patients with distal clavicle fractures underwent surgical treatment. Mean age was 36 years (18-62 years) and mean follow-up period was 12.9 months (6-32 months). Two cases were Neer type I, six cases IIa, three cases IIb, three cases III, and two cases V. For the radiologic assessment, union time and metal failure were evaluated, and coracoidiologic assessment, union time and metal failure were evaluatethe acromioclavicular joint. The clinical results were evaluated by range of motion, postoperative complication, and University of California at Los Angeles (UCLA) score.
RESULTS
Mean time to fracture union was 7.4 weeks (6-14 weeks) in all cases. No statistical difference in coracoid-clavicle distance was observed between immediate post-operation group and contra-lateral group (p=0.6), but an increase of 2.1 mm was observed in the last follow up group compared with the contra-lateral group (p<0.01). The UCLA scoring system showed excellent results in 15 cases and good results in one case. Acromial-clavicle instability occurred in one case so that metal removal and distal clavicle resection were performed.
CONCLUSION
A 2.4 mm volar distal radius locking plate can provide rigid fixation through several screw fixation in the short distal fragment and lead to satisfactory clinical outcomes in unstable distal clavicular fractures. -
Citations
Citations to this article as recorded by- Estudo retrospectivo da placa anterior superior como tratamento para fraturas instáveis da clavícula distal (tipo 2 de Neer)
Syed Ibrahim, Jimmy Joseph Meleppuram
Revista Brasileira de Ortopedia.2018; 53(3): 306. CrossRef - Retrospective study of superior anterior plate as a treatment for unstable (Neer type 2) distal clavicle fractures
Syed Ibrahim, Jimmy Joseph Meleppuram
Revista Brasileira de Ortopedia (English Edition).2018; 53(3): 306. CrossRef
- Estudo retrospectivo da placa anterior superior como tratamento para fraturas instáveis da clavícula distal (tipo 2 de Neer)
- 554 View
- 1 Download
- 2 Crossref

- Concomitant Carpal Injuries in Distal Radius Fractures: Retrospective Analysis by Plain Radiographs and Computed Tomography
- Chul Hyun Cho, Eun Seok Son
- J Korean Fract Soc 2015;28(1):1-7. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.1
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the incidence and characteristics of concomitant carpal bone fractures and ligament injuries and to analyze risk factors for carpal injuries in patients with distal radius fractures.
MATERIALS AND METHODS
A total of 362 patients with 379 distal radius fractures were reviewed retrospectively. Associated carpal bone fractures and ligament injuries were evaluated by plain radiographs and computed tomography at the time of initial trauma. Correlation between associated carpal injuries and various parameters was also analyzed.
RESULTS
Of 379 distal radius fractures, 39 cases (10.3%) had one or more carpal bone fracture and 40 cases (10.6%) had carpal ligament injuries. Overall, carpal injuries occurred in 59 cases (15.6%) distal radius fractures. Associated carpal ligament injuries showed correlation with young age and associated carpal bone fractures showed correlation with AO type B distal radius fractures. Carpal injuries including fracture and ligament injury showed correlation with male, high energy trauma, or associated injuries beyond wrist.
CONCLUSION
The incidence of concomitant carpal injuries in patients with distal radius fractures is relatively high. Concomitant carpal injuries were more common in young age, male, high energy trauma, AO type B distal radius fractures, or associated injuries beyond wrist. -
Citations
Citations to this article as recorded by- Korean Medicine Treatments for the Angular Deformity of Wrist Fracture with Disuse Osteopenia: A Case Report
Myung Jin Oh
Korean Journal of Acupuncture.2018; 35(4): 234. CrossRef - Comparison of Distal Radius Fractures with or without Scaphoid Fractures
Jin Rok Oh, Dong Woo Lee, Jun Pyo Lee
Journal of the Korean Society for Surgery of the Hand.2016; 21(1): 23. CrossRef
- Korean Medicine Treatments for the Angular Deformity of Wrist Fracture with Disuse Osteopenia: A Case Report
- 806 View
- 15 Download
- 2 Crossref

- The Fate of Pronator Quadratus Muscle after Volar Locking Plating of Unstable Distal Radius Fractures
- Chae Hyun Lim, Heun Guyn Jung, Ju Yeong Heo, Young Jae Jang, Yong Soo Choi
- J Korean Fract Soc 2014;27(3):191-197. Published online July 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.3.191
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the pronator quadrates muscle in patients who underwent internal fixation with a volar locking plate for unstable distal radius fractures.
MATERIALS AND METHODS
Forty patients who underwent internal fixation with a volar locking plate for unstable distal radius fracture were enrolled. We evaluated the clinical results according to the Mayo wrist score, the wrist range of motion, and the grip strength at the last follow-up. Using ultrasonography, muscle thickness of the pronator quadrates was compared between injured and uninjured arm.
RESULTS
Bone union was achieved in all cases. The mean Mayo wrist score was 82.79 points. The grip strength of the injured arm was decreased to 89.1% of the uninjured side. The decrease of pronation range of the injured wrist motions was significant (82.3degrees, p=0.004). There was significant atrophy of the pronator quadrates muscle on the injured side (injured side: 3.19 mm, uninjured side: 4.72 mm, p=0.001); and the decrement of muscle thickness in pronator quadrates showed an association with the Mayo wrist score (r=-0.35, p=0.042).
CONCLUSION
These results suggest that continuity of the muscle is maintained after use of the volar locking plating for unstable distal radius fractures with repair of pronator quadrates; however, there is atrophy of pronator quadrates muscle and limitation of pronation in the injured wrist.
- 389 View
- 0 Download

- The Clinical Results of Opening Wedge Osteotomy in the Volarly Malunited Distal Radius
- Seoung Joon Lee, Jin Ho Choi
- J Korean Fract Soc 2014;27(1):29-35. Published online January 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.1.29
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To report the clinical results of opening wedge osteotomy graft in the volarly malunited distal radius.
MATERIALS AND METHODS
Ten patients with volarly malunited distal radius fractures treated by opening wedge osteotomy were included in this study. Grip power, range of motion of the wrist, radiographic parameter and Mayo wrist scores were retrospectively evaluated.
RESULTS
At the final follow-up, the rotation of the forearm, the range of motion of wrist, and the grip power were improved. The average radial inclination improved to 22.2degrees, the average volar tilting improved to 5.6degrees, and the average ulnar variance improved to 0.8 mm. The average Mayo wrist score was improved to 85.6.
CONCLUSION
Opening wedge osteotomy for volarly malunited distal radius was considered as one of the good treatments to restore anatomy of the distal radius and distal radioulnar joint and also to improve the function of the wrist joint.
- 445 View
- 3 Download

- Clinical Assessment after the Volar Locking Plate Removal of Distal Radius Fracture
- Hee Chul Gwak, Joo Yong Kim, Gyu Min Kong, Jung Won Kim, Jae Yong Kwak, Dong Gyun Kim
- J Korean Fract Soc 2014;27(1):23-28. Published online January 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.1.23
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate the clinical outcomes after removing the volar locking plate for distal radius fracture.
MATERIALS AND METHODS
We reviewed retrospectively the medical records of 34 patients, 36 cases after removing the plates among 150 patients, with 162 cases that underwent open reduction and internal fixation using the volar locking plate between January 2006 and May 2011. We performed preoperative and postoperative clinical assessments using the quick-disabilities of the arm, shoulder and hand (Q-DASH), the visual analog scale (VAS) score, and the range of motion on wrist, grip and pinch power.
RESULTS
The major reason for plate removal was the time to remove the plate according to the fracture union and the patient's demand without other specific complaints (28 cases). The mean preoperative VAS score was 1.78 and the mean postoperative VAS score 1.81 (p=0.64). The mean preoperative Q-DASH score was 30.02 and the mean postoperative Q-DASH score 38.46 (p<0.001). The mean preoperative grip and pinch power were 18.14 kg and 7.67 kg. The mean postoperative grip and pinch power were 15.27 kg and 6.94 kg (p=0.23).
CONCLUSION
The removal of the volar locking plate for distal radius fracture should be decided by considering the patient's clinical and socioeconomic conditions carefully.
- 690 View
- 0 Download

Case Report
- Rupture of the Extensor Pollicis Longus Tendon at the Proximal Screw of Volar Plate Fixation for Distal Radius Fracture: A Case Report
- Dong Ju Shin, Seung Oh Nam, Hun Sik Cho
- J Korean Fract Soc 2013;26(4):338-342. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.338
-
 Abstract
Abstract
 PDF
PDF - As volar plate fixation of distal radius fracture becomes more common, reports of ruptured extensor pollicis longus tendon by a protruding distal screw tip are also increasing steadily. Authors have experienced a rare case of ruptured extensor pollicis longus tendon at the prominent proximal screw of fixed volar plate for distal radius fracture, and we report it herein with a review of the literature.
- 474 View
- 1 Download

Original Articles
- Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
- Ki Chan An, Gyu Min Kong, Jang Seok Choi, Hi Chul Gwak, Joo Yong Kim, Sung Yub Jin
- J Korean Fract Soc 2013;26(4):248-253. Published online October 31, 2013
- DOI: https://doi.org/10.12671/jkfs.2013.26.4.248
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To determine the influence of osteoporosis on the results of percutaneous K-wire fixation for distal radius fractures.
MATERIALS AND METHODS
Between March 2007 and February 2011, Fifty seven patients who underwent fixative surgery with K-wires after closed reduction and those available for follow-up for at least 6 months were reviewed. They were divided into the two groups of T score -3 or more (group 1) and T score less than -3 (group 2). These groups were compared by the range of motion of the wrist and Disabilities of the Arm, Shoulder and Hand (DASH) score. Radiologic evaluations consisting of radial length, radial inclination and volar tilt were compared. In group 1 with 34 cases, the average age was 65.4 years (50 to 78 years) and T score was -1.97 (-0.1 to -2.93). In group 2 with 23 cases, the average age was 74 years (54 to 89 years) and T score was -4.11 (-3.1 to -6.97).
RESULTS
There was no statistical difference between group 1 and group 2 in terms of range of motion, DASH score and radiologic evaluations.
CONCLUSION
In the case of no volar side cortical comminution, percutaneous K-wire fixation can be applied for the treatment of distal radius fracture with osteoporosis.
- 405 View
- 2 Download

- Comparative Analysis of the Results of Fixed-angle versus Variable-angle Volar Locking Plate for Distal Radius Fracture Fixation
- Seung Do Cha, Jai Hyung Park, Hyung Soo Kim, Soo Tae Chung, Jeong Hyun Yoo, Joo Hak Kim, Jung Hwan Park
- J Korean Fract Soc 2012;25(3):197-202. Published online July 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.3.197
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the outcomes of distal radius fractures in a fixed-angle volar locking plate group and variable-angle volar locking plate group.
MATERIALS AND METHODS
Forty-one patients observed at least 6 months after surgery were included in this retrospective study. We used the range of motion, visual analogue scale score, Disabilities of the Arm, Shoulder and Hand Questionnaire score, and radiologic findings to measure the clinical results.
RESULTS
No differences in clinical results or radiologic results were noted between the fixed-angle volar locking plate group and variable-angle volar locking plate group.
CONCLUSION
We believe that it is important to minimize complications by using appropriate screws and plates according to the fracture type, though no differences in the surgical outcome were noted between the fixed-angle volar locking plate group and variable-angle volar locking plate group with distal radius fracture. -
Citations
Citations to this article as recorded by- Volar locking plate fixation for distal radius fractures: did variable-angle plates make difference?
Mohamed Abdel-Wahed, Ahmed Abdel-Zaher Khater, Mahmoud Ahmed El-Desouky
International Orthopaedics.2022; 46(9): 2165. CrossRef - Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
Jae-Cheon Sim, Sung-Sik Ha, Ki-Do Hong, Tae-Ho Kim, Min-Chul Sung
Journal of the Korean Fracture Society.2015; 28(1): 46. CrossRef - Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
Ki-Chan An, Gyu-Min Kong, Jang-Seok Choi, Hi-Chul Gwak, Joo-Yong Kim, Sung-Yub Jin
Journal of the Korean Fracture Society.2013; 26(4): 248. CrossRef
- Volar locking plate fixation for distal radius fractures: did variable-angle plates make difference?
- 659 View
- 5 Download
- 3 Crossref

- Results of the Kapandji Procedure in the AO Type C Distal Radius Fracture in Patients over Age 60
- Chul Hong Kim, Sung Soo Kim, Myung Jin Lee, Hyeon Jun Kim, Bo Kun Kim, Young Hoon Lim
- J Korean Fract Soc 2012;25(3):191-196. Published online July 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.3.191
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the clinical and radiologic results of the Kapandji procedure in AO classification type C distal radius fracture patients over 60 years old.
MATERIALS AND METHODS
Twenty-one type C distal radius fracture patients over the age of 60 years who were treated with the Kapandji procedure from June 2004 to June 2009 in our hospital and had a post-operative follow-up period of more than 1 year were enrolled. The volar tilt, radial inclination, and radial length were measured for the radiographic analysis using the modified Lidstrom scoring system about post-operative reduction loss in every follow-up radiogram. The clinical result was assessed with a visual analogue scale (VAS) and Korean Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH) score at the last follow-up.
RESULTS
The mean radiologic loss of volar tilt was 1.1degrees and the mean loss of radial length was 2.6 mm and the mean radial inclination loss was 2.7degrees compared with the immediate post-operative period and last follow-up period. The average VAS and DASH scores were 1.4 and 15.9.
CONCLUSION
The radiologic results of closed reduction and percutaneous pinning using the Kapandji technique for distal radius AO type C fracture patients over 60 years of age was not satisfactory. Nevertheless, the clinical results were satisfactory.
- 357 View
- 2 Download

Case Report
- Ipsilateral Distal Radius and Scaphoid Fractures Associated with Posteromedial Dislocation of the Elbow Joint: A Case Report
- Jin Wan Kim, Young Chul Ko, Chul Young Jung, Il Soo Eun, Young Jun Kim, Chang Kyu Kim
- J Korean Fract Soc 2012;25(2):150-154. Published online April 30, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.2.150
-
 Abstract
Abstract
 PDF
PDF - Arm injuries occurring from high energy injuries such as falls or traffic accidents can be accompanied by wrist and elbow injuries. Monteggia fracture, Galeazzi fracture, and Essex-Lopresti fracture-dislocation are known some examples of such injuries. However, there are no reports on the dislocation of the elbow occurring from a distal radius fracture accompanied by scaphoid fracture, and there is nothing published about its prognosis. The authors report on the treatment and outcomes of a case of a 42-year-old male who had a distal radius and scaphoid fracture associated with posteromedial dislocation of the elbow on the same side of his arm along with a literature review.
- 491 View
- 2 Download

Original Article
- Extensor Pollicis Longus Rupture after Distal Radius Fracture
- Nam Young Cho, Chang Young Seo, Myung Sun Kim, Ha Sung Kim, Keun Bae Lee
- J Korean Fract Soc 2012;25(1):52-57. Published online January 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.1.52
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the cause and surgical outcome of extensor pollicis longus rupture after distal radius fractures.
MATERIALS AND METHODS
Nineteen cases in which the patients underwent surgical treatment for rupture of the extensor pollicis longus after distal radius fractures were followed for more than one year. Among the nineteen cases, fourteen extensor pollicis longus ruptures occurred after conservative treatment, four occurred after closed reduction with K-wire fixation, and one occurred after open reduction and internal fixation with a plate. All cases were treated by extensor indicis proprius transfer.
RESULTS
Extensor pollicis longus ruptures were caused by K-wire irritation in two, by a protruding screw tip in one, and by a callus in one. In the conservative treatment group, tendon ruptures were diagnosed at an average of 3.1 months (0.7~17). Tendon ruptures were detected in the surgical treatment group at an average of 12.8 months (1~48). All the patients showed favorable recovery of the extension capability of the thumb at the final follow-up.
CONCLUSION
The main cause of extensor pollicis longus rupture after distal radius fracture was ischemic damage. Therefore, during the surgery, the length and direction of screws and K-wires should be fixed carefully to avoid such damage. Distal radius fracture also requires careful observation of the extensor pollicis longus during follow-up. Furthermore, extensor indicis proprius transfer is considered to be an effective method for extensor pollicis longus rupture. -
Citations
Citations to this article as recorded by- Radiologic Analysis of Distal Radius Fracture Accompanying Spontaneous Extensor Pollicis Longus Rupture
Jun-Ku Lee, In-Tae Hong, Young-Woo Kwon, Gyu-Chol Jang, Soo-Hong Han
Journal of the Korean Fracture Society.2017; 30(2): 63. CrossRef - Assessment of penetration of dorsal screws after fixation of the distal radius using ultrasound: cadaveric study
D Williams, J Singh, N Heidari, M Ahmad, A Noorani, L Di Mascio
The Annals of The Royal College of Surgeons of England.2016; 98(2): 138. CrossRef - Rupture of the Extensor Pollicis Longus Tendon at the Proximal Screw of Volar Plate Fixation for Distal Radius Fracture - A Case Report -
Dong-Ju Shin, Seung-Oh Nam, Hun-Sik Cho
Journal of the Korean Fracture Society.2013; 26(4): 338. CrossRef
- Radiologic Analysis of Distal Radius Fracture Accompanying Spontaneous Extensor Pollicis Longus Rupture
- 620 View
- 6 Download
- 3 Crossref

Case Report
- Flexor Pollicis Longus Tendon Rupture as a Complication of a Closed Distal Radius Fracture: A Case Report
- Do Young Kim, Eun Min Seo, Woo Dong Nam, Seung Jae Park, Sang Soo Lee
- J Korean Fract Soc 2011;24(2):191-194. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.191
-
 Abstract
Abstract
 PDF
PDF - There are few reported cases of flexor pollicis longus tendon (FPL) rupture complicating a closed distal radius fracture. We report a case of FPL tendon rupture complicating a closed distal radius fracture. A 24-year-old male presented with a severe right wrist pain. He had a closed distal radius fracture that was treated by closed manual reduction. Three days later, he complained forearm pain and limitation of thumb motion. The physical examination revealed loss of active interphalangeal joint flexion of thumb. He was taken to the operating room. Intraoperatively, the FPL was found to be discontinuous at the level of the radius fracture site. The FPL was repaired by a modified Kessler technique, and the fracture was repaired with a volar plate. Clinicians must be cautious in possibility of tendon injury complicating a closed distal radius fracture and assessing patients with distal radius fracture following closed reduction.
-
Citations
Citations to this article as recorded by- Acute Rupture of Flexor Tendons as a Complication of Distal Radius Fracture
Youn Moo Heo, Sang Bum Kim, Kwang Kyoun Kim, Doo Hyun Kim, Won Keun Park
Journal of the Korean Orthopaedic Association.2015; 50(1): 60. CrossRef
- Acute Rupture of Flexor Tendons as a Complication of Distal Radius Fracture
- 635 View
- 1 Download
- 1 Crossref

Original Articles
- Comparison of Operative Management in Distal Radius Fractures Using 3.5 mm Versus 2.4 mm Volar Locking Compression Plates
- Sung Sik Ha, Tae Ho Kim, Ki Do Hong, Jae Chun Sim, Jong Hyun Kim
- J Korean Fract Soc 2011;24(2):156-162. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.156
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate clinical and radiological results using 3.5 mm & 2.4 mm volar locking compression plate (LCP) in distal radius fractures.
MATERIALS AND METHODS
This study reviewed the results of 115 cases of distal radius fractures treated with 3.5 mm volar LCP (73 cases) & 2.4 mm volar LCP (42 cases) from September 2003 to June 2009. The radiographic results were evaluated by radiographic assessment, and the clinical results were evaluated by Knirk and Jupiter's criteria, Modified Mayo wrist scoring system and DASH score.
RESULTS
Radiological evaluation of the radial length, radial inclination, volar tilt and intraarticular step off were improved both 3.5 mm volar LCP and 2.4 mm volar LCP. Nine cases of arthritis occured in 3.5 mm volar LCP and 7 cases in 2.4 mm volar by using the Knirk and Jupiter's criteria. The mean score evaluated by Modified Mayo was 86.7 in 3.5 mm volar LCP and 84.8 in 2.4 mm volar LCP. DASH score was 11.2 point in 3.5 mm volar LCP, 10.9 point in 2.4 mm volar LCP. All cases showed bone union showing no evidence of malunion, nounion, nor metal failure.
CONCLUSION
Distal radius fractures treated with 3.5 mm volar LCP and 2.4 mm volar LCP show satisfying radiological and clinical outcome. -
Citations
Citations to this article as recorded by- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
Jae-Cheon Sim, Sung-Sik Ha, Ki-Do Hong, Tae-Ho Kim, Min-Chul Sung
Journal of the Korean Fracture Society.2015; 28(1): 46. CrossRef - Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
Ki-Chan An, Gyu-Min Kong, Jang-Seok Choi, Hi-Chul Gwak, Joo-Yong Kim, Sung-Yub Jin
Journal of the Korean Fracture Society.2013; 26(4): 248. CrossRef
- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
- 515 View
- 0 Download
- 2 Crossref

- 2.4 mm Volar Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
- Sung Jin Kim, Chul Hyun Cho
- J Korean Fract Soc 2011;24(2):151-155. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.151
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate outcomes 2.4 mm volar locking compression plate for treatment of unstable distal radius fractures.
MATERIALS AND METHODS
We retrospectively analyzed the results in 22 cases, which were treated by 2.4 mm volar locking compression plate. We evaluated the clinical results according to the Mayo wrist performance scoring system and radiographic results.
RESULTS
All cases had bony union. The mean Mayo wrist performance score was 85.23. Between preoperative and immediate postoperative radiographic measurements, the mean radial length was improved from 6.04 mm to 9.68 mm, radial inclination from 15.61degrees to 19.61degrees, volar tilt from -13.73degrees to 7.66degrees and intraarticular step-off from 0.79 mm to 0.33 mm (p<0.05). Between immediate postoperative and latest follow-up radiographic measurements, the mean loss of radial length measured 0.86 mm, radial inclination 0.41degrees, volar tilt 0.54degrees and intraarticular step-off 0.02 mm (p>0.05). Postoperative complication included that flexor pollicis longus and 2nd flexor digitorum profundus were ruptured in 1 case.
CONCLUSION
Treatment of unstable distal radius fractures using a 2.4 mm volar locking compression plate showed satisfactory outcomes. It is a good option to obtain stable fixation without significant loss of reduction. -
Citations
Citations to this article as recorded by- Is dorsal cortex drilling necessary for distal radius fractures treated with a volar locking plate? A comparative study of near-cortex-only and far-cortex drilling
Chul Hong Kim, Sung Yoon Jung, Hyeon Jun Kim, Si-Hyun Park
Journal of Trauma and Injury.2025; 38(3): 248. CrossRef - Treatment of the Communited Distal Radius Fracture Using Volar Locking Plate Fixation with Allogenic Cancellous Bone Graft in the Elderly
Je Kang Hong, Chang Hyun Shin
Journal of the Korean Fracture Society.2015; 28(1): 8. CrossRef
- Is dorsal cortex drilling necessary for distal radius fractures treated with a volar locking plate? A comparative study of near-cortex-only and far-cortex drilling
- 537 View
- 1 Download
- 2 Crossref

- Treatment for Unstable Distal Radius Fracture with Osteoporosis: Internal Fixation versus External Fixation
- Jin Rok Oh, Tae Yean Cho, Sung Min Kwan
- J Korean Fract Soc 2010;23(1):76-82. Published online January 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.1.76
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the functional and radiological outcomes of volar plating to that of external fixation for treating unstable osteoporotic distal radius fracture.
MATERIALS AND METHODS
From March 2006 to March 2008, 36 patients with osteoporosis over 60-year old were selected for this study. They were divided into two groups; group I (open reduction and internal fixation with volar fixed angle plate) and group II (closed reduction and external fixation). Clinical outcomes and radiologic outcomes were evaluated.
RESULTS
There was no statistical difference between group I and group II in range of motion and DASH score, BMD score. However, the grip strength and PRWE score were found to be higher in group II (p<0.05). In radiologic evaluation, group I showed higher radial inclination, volar tilting angle (p<0.05).
CONCLUSION
Internal fixation using Volar-fixed Angle Plate seems to give more stable fixation for distal articular fragments compared to external fixation. it could allow early postoperative exercise and could result in low incidence of postoperative complication such as pin track infections and joint stiffness. Therefore, the internal fixation could be more desirable treatment method to manage unstable distal radius fracture. -
Citations
Citations to this article as recorded by- Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
Ki-Chan An, Gyu-Min Kong, Jang-Seok Choi, Hi-Chul Gwak, Joo-Yong Kim, Sung-Yub Jin
Journal of the Korean Fracture Society.2013; 26(4): 248. CrossRef
- Functional Outcomes of Percutaneous K-Wire Fixation for Distal Radius Fractures with or without Osteoporosis
- 588 View
- 0 Download
- 1 Crossref

- Short Term Results of Operative Management with 2.4 mm Volar Locking Compression Plates in Distal Radius Fractures
- Ki Chul Park, Chang Hun Lee
- J Korean Fract Soc 2009;22(4):264-269. Published online October 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.4.264
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the short term outcome of internal fixation using 2.4 mm volar locking compression plate for the treatment of unstable distal radius fractures. MATERIALS AND METHODS: We retrospectively analyzed the results in 22 cases, which were treated with 2.4 mm volar locking compression plate. We evaluated the radiologic results and the clinical results according to Disabilities of the Arm, Shoulder and Hand (DASH) score and visual analogue scale. RESULTS: At final follow up, the mean VAS was 1.2 and mean DASH score was 10. Average loss of reduction from initial postoperative to final follow up radiographs was 0.36 mm of radial length, 0.2degrees of radial inclination, 0.6degrees of volar tilt. CONCLUSION: Fixation of unstable dorsally displaced distal radius fractures with a 2.4 mm volar locking compression plate provides sufficient stability with minimal loss of reduction and good enough clinical outcomes with less complications. -
Citations
Citations to this article as recorded by- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
Jae-Cheon Sim, Sung-Sik Ha, Ki-Do Hong, Tae-Ho Kim, Min-Chul Sung
Journal of the Korean Fracture Society.2015; 28(1): 46. CrossRef - 2.4 mm Volar Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
Sung-Jin Kim, Chul-Hyun Cho
Journal of the Korean Fracture Society.2011; 24(2): 151. CrossRef
- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
- 559 View
- 1 Download
- 2 Crossref

- Plate Fixation of AO Type C3 Fractures of the Distal Radius
- Eun Sun Moon, Myung Sun Kim, Hyeong Won Park, Min Sun Choi
- J Korean Fract Soc 2009;22(3):172-178. Published online July 31, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.3.172
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate clinical and radiographic results of open reduction and internal fixation with plate in AO type C3 distal radius fracture.
MATERIALS AND METHODS
We treated 18 fractures and the mean follow up was 16 months. The average age was 47.1 years old, 12 male and 6 female were included. There were 9 C3.1 fracture, 5 C3.2 and 4 C3.3. Green & O'Brien's modified clinical scoring system and Demerit Point system were applied to evaluate clinical results, for radiographic evaluation, radial length, radial inclination, volar tilt, and Sarmiento's Criteria for Anatomic results were assessed.
RESULTS
Clinical results were 5 of excellent, 7 of good, and 6 of fair by Green & O'Brien's score and were 5 of excellent, 6 of good, and 7 of fair by Demerit point. There was no significant difference of radiographic results between immediate postoperation and last follow-up, and Sarmiento's Criteria showed 8 excellent, 4 good, and 6 fair.
CONCLUSION
The open reduction and internal fixation with plate in AO type C3 distal radius is considered as a good treatment method that particularly benefits from fracture stable fixation without fixation loss and early rehabilitation.
- 937 View
- 6 Download

Review Article
- Volar Plating of Distal Radius Fractures
- Kwang Hyun Lee
- J Korean Fract Soc 2008;21(4):325-333. Published online October 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.4.325
-
 Abstract
Abstract
 PDF
PDF - Volar plating seems to indicate that many surgeons believe it leads to superior results, and is attractive because of the ease of the operative approach and the soft tissue sleeve to protect digital and wrist tendons. And also it have a locking mechanism to produce the fixed angle device with a low profile and may be thought to be a new era in the surgical treatment of dorsally displaced distal radius fractures even in the face of comminuted or osteoporotic bone. Locked volar plating allows direct fracture reduction, stable fixation and provides stability enough to allow early mobilization and function. The results with volar locking or fixed angle fixation for the general treatment of unstable distal radius fractures in elderly patients has been favorable. Volar plating has fewer complications than external fixation and dorsal plating and allow for earlier return to function. The current indications, technical aspects, clinical results, and complications of the volar plating are being reviewed.
-
Citations
Citations to this article as recorded by- Ultrasonographic Assessment of the Pronator Quadratus Muscle after Surgical Treatment for Distal Radius Fractures
Dong Hyuk Choi, Hyun Kyun Chung, Ji Won Lee, Cheol Hwan Kim, Yong Soo Choi
Journal of the Korean Fracture Society.2017; 30(2): 69. CrossRef - The Fate of Pronator Quadratus Muscle after Volar Locking Plating of Unstable Distal Radius Fractures
Chae-Hyun Lim, Heun-Guyn Jung, Ju-Yeong Heo, Young-Jae Jang, Yong-Soo Choi
Journal of the Korean Fracture Society.2014; 27(3): 191. CrossRef - Comparison of Operative Management in Distal Radius Fractures Using 3.5 mm Versus 2.4 mm Volar Locking Compression Plates
Sung-Sik Ha, Tae-Ho Kim, Ki-Do Hong, Jae-Chun Sim, Jong Hyun Kim
Journal of the Korean Fracture Society.2011; 24(2): 156. CrossRef - Treatment for Unstable Distal Radius Fracture with Osteoporosis -Internal Fixation versus External Fixation-
Jin Rok Oh, Tae Yean Cho, Sung Min Kwan
Journal of the Korean Fracture Society.2010; 23(1): 76. CrossRef - Short Term Results of Operative Management with 2.4 mm Volar Locking Compression Plates in Distal Radius Fractures
Ki-Chul Park, Chang-Hun Lee
Journal of the Korean Fracture Society.2009; 22(4): 264. CrossRef
- Ultrasonographic Assessment of the Pronator Quadratus Muscle after Surgical Treatment for Distal Radius Fractures
- 572 View
- 1 Download
- 5 Crossref

Original Articles
- Epiphyseal Fractures of the Distal Radius in the Children
- Hui Taek Kim, Myung Soo Youn, Jong Seo Lee, Young Jun Choi, Yoon Jae Seong
- J Korean Fract Soc 2008;21(3):225-231. Published online July 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.3.225
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the long-term results of treatment of epiphyseal fractures of the distal radius in children.
MATERIALS AND METHODS
23 cases of distal radial epiphyseal fracture, treated by two methods: group 1, closed reduction (CR) plus cast (6 cases); group 2, CR and K-wire fixation (under anesthesia due to marked translation of the distal fragment and swelling) plus cast (17 cases), were selected for this study. All patients were followed up for more than 1 year (average: 3.2 years). Postoperatively, epiphyseal displacement and epiphyseal angulation were measured on anteroposterior and lateral radiographs. At follow-up, the affected and normal sides were compared. Final results were classified by radiologic (radial inclination, volar tilting and radial shortening) and clinical (limitation of ROM, wrist pain, grip strength and wrist deformity) criteria.
RESULTS
Group 1 had 5 good, 1 fair result; group 2 had 14 good, 2 fair and 1 poor - there was no statistically significant difference between two groups. All cases where the epiphyseal displacement was less than 30% had good results. A poor case showed a radial shortening, wrist deformity and pain due to premature epiphyseal closure. Premature epiphyseal closure was treated by bar resection and free fat, along with corrective osteotomy when necessary and lengthening of radius with or without epiphysiodesis of the ulna.
CONCLUSION
Remodeling can be expected in epiphyseal fractures of the distal radius. Repeated forceful attempts to achieve accurate reduction should be avoided to prevent secondary physeal injury. -
Citations
Citations to this article as recorded by- How long does it to achieve sagittal realignment of the displaced epiphysis in Salter-Harris type II distal radial fracture when treated by manual reduction?
Seung Hoo Lee, Hyun Dae Shin, Eun-Seok Choi, Soo Min Cha
Journal of Plastic Surgery and Hand Surgery.2023; 57(1-6): 346. CrossRef
- How long does it to achieve sagittal realignment of the displaced epiphysis in Salter-Harris type II distal radial fracture when treated by manual reduction?
- 2,401 View
- 27 Download
- 1 Crossref

- Volar T-Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
- Chul Hyun Cho, Ki Choer Bae, Doo Hyun Kwon
- J Korean Fract Soc 2008;21(3):220-224. Published online July 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.3.220
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate outcomes volar T-locking compression plate for treatment of unstable distal radius fractures.
MATERIALS AND METHODS
We retrospectively analysed the results in 35 cases, which were treated by volar plating with T-LCP. We evaluated the clinical results according to the Mayo wrist scoring system and radiographic results.
RESULTS
The mean score was 83.86 respectively. Between preoperative and immediate postoperative radiographic measurements, averaged radial length was improved from 5.75 mm to 11.53 mm, radial inclination from 12.86 degrees to 22.56 degrees, volar tilt from -3.64 degrees to 9.90 degrees and intraarticular step-off from 1.48 mm to 0.42 mm. Between immediate postoperative and latest follow-up radiographic measurements, mean loss of radial length measured 0.43 mm, radial inclination 0.46 degrees, volar tilt 0.89 degrees.
CONCLUSION
Treatment of unstable distal radius fractures using a volar T-LCP showed satisfactory outcomes. We think that it is good surgical option to allow return to daily living, result in early postsurgical wrist motion. -
Citations
Citations to this article as recorded by- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
Jae-Cheon Sim, Sung-Sik Ha, Ki-Do Hong, Tae-Ho Kim, Min-Chul Sung
Journal of the Korean Fracture Society.2015; 28(1): 46. CrossRef - The Fate of Pronator Quadratus Muscle after Volar Locking Plating of Unstable Distal Radius Fractures
Chae-Hyun Lim, Heun-Guyn Jung, Ju-Yeong Heo, Young-Jae Jang, Yong-Soo Choi
Journal of the Korean Fracture Society.2014; 27(3): 191. CrossRef - 2.4 mm Volar Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
Sung-Jin Kim, Chul-Hyun Cho
Journal of the Korean Fracture Society.2011; 24(2): 151. CrossRef - Short Term Results of Operative Management with 2.4 mm Volar Locking Compression Plates in Distal Radius Fractures
Ki-Chul Park, Chang-Hun Lee
Journal of the Korean Fracture Society.2009; 22(4): 264. CrossRef - Plate Fixation of AO Type C3 Fractures of the Distal Radius
Eun-Sun Moon, Myung-Sun Kim, Hyeong-Won Park, Min-Sun Choi
Journal of the Korean Fracture Society.2009; 22(3): 172. CrossRef - Biosorption of Mercury (II) from Aqueous Solutions by Zygnema fanicum Algae
Gh. Shams Khoramabad, A. Jafari, J. Hasanvand Jamshidi
Journal of Applied Sciences.2008; 8(11): 2168. CrossRef - Volar Plating of Distal Radius Fractures
Kwang-Hyun Lee
Journal of the Korean Fracture Society.2008; 21(4): 325. CrossRef
- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
- 596 View
- 0 Download
- 7 Crossref

- Comparison of Outcomes for Unstable Distal Radius Intraarticular Fractures: T-locking Compression Plate versus External Fixator
- Chul Hyun Cho, Su Won Jung, Sung Won Sohn, Chul Hyung Kang, Ki Cheor Bae, Kyung Jae Lee
- J Korean Fract Soc 2008;21(1):51-56. Published online January 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.1.51
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To compare the outcomes between T-locking compression plate (T-LCP) and external fixator (EF) for unstable distal radius intraarticular fractures.
MATERIALS AND METHODS
We retrospectively analysed the results in 22 cases with T-LCP, 20 cases with EF. We evaluated the clinical results according to the Mayo Wrist Scoring System, radiographic results.
RESULTS
The mean score was 84.6 in the T-LCP group and 80.5 in the EF group respectively. Final radiographic measurements for the T-LCP group averaged 10.5 mm radial length, 21.7degrees radial inclination, 9.8degrees volar tilt and 0.25 mm intraarticular step-off. The EF group averaged 10.1 mm radial length, 20.3 degrees radial inclination, 6.3 degrees volar tilt and 0.73 mm intraarticular step-off.
CONCLUSION
Both groups showed satisfactory final clinical outcomes. But T-LCP group allowed return to daily living, resulting in early postsurgical wrist motion. By the anatomical reduction, final volar tilt, intraarticular step-off were statistically better in the T-LCP group. -
Citations
Citations to this article as recorded by- Comparative Analysis of the Results of Fixed-angle versus Variable-angle Volar Locking Plate for Distal Radius Fracture Fixation
Seung-Do Cha, Jai-Hyung Park, Hyung-Soo Kim, Soo-Tae Chung, Jeong-Hyun Yoo, Joo-Hak Kim, Jung-Hwan Park
Journal of the Korean Fracture Society.2012; 25(3): 197. CrossRef - Treatment for Unstable Distal Radius Fracture with Osteoporosis -Internal Fixation versus External Fixation-
Jin Rok Oh, Tae Yean Cho, Sung Min Kwan
Journal of the Korean Fracture Society.2010; 23(1): 76. CrossRef
- Comparative Analysis of the Results of Fixed-angle versus Variable-angle Volar Locking Plate for Distal Radius Fracture Fixation
- 614 View
- 0 Download
- 2 Crossref

- The Amount and Related Factors of Reduction Loss in Distal Radius Fracture after Treatment by Kapandji Technique
- Eun Sun Moon, Myung Sun Kim, Il Kyu Kong
- J Korean Fract Soc 2007;20(3):252-259. Published online July 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.3.252
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the amount and related factors of reduction loss in distal radius fracture after treatment by Kapandji technique.
MATERIALS AND METHODS
From September 2004 to May 2006, 44 cases (43 patients) of distal radius fractures were treated by Kapandji technique. Fracture were classified with AO classification and volar tilt, radial inclination, and radial length were measured in preoperative, immediate, postoperative radiographs. Also the amount and related risk factors of reduction loss were analyzed. In addition, the radiological results at last follow up were evaluated using modified Lidstrom scoring system.
RESULTS
There was significantly more reduction loss of volar tilt in the patients with AO type C comparing with other fracture types, but the patients who were treated using three k-wire fixations including intrafocal K-wires showed significantly more reduction loss of volar tilt also. Overall radiological results at last follow up showed that excellent was 50% in cases with dorsal comminution, but, the other cases 90%. In addition, excellent was 70% in type A cases, but, in type C 44%.
CONCLUSION
Kapandji technique percutaneous pinning is the one of effective treatment options for distal radius fracture. But, type of fracture, total number of K-wires, and presence of dorsal cortical comminution showed the significant relation with postoperative reduction loss of volar tilt and overall radiological results at last follow up. -
Citations
Citations to this article as recorded by- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
Jae-Cheon Sim, Sung-Sik Ha, Ki-Do Hong, Tae-Ho Kim, Min-Chul Sung
Journal of the Korean Fracture Society.2015; 28(1): 46. CrossRef - Comparative Analysis of the Results of Fixed-angle versus Variable-angle Volar Locking Plate for Distal Radius Fracture Fixation
Seung-Do Cha, Jai-Hyung Park, Hyung-Soo Kim, Soo-Tae Chung, Jeong-Hyun Yoo, Joo-Hak Kim, Jung-Hwan Park
Journal of the Korean Fracture Society.2012; 25(3): 197. CrossRef - Results of the Kapandji Procedure in the AO Type C Distal Radius Fracture in Patients over Age 60
Chul Hong Kim, Sung Soo Kim, Myung Jin Lee, Hyeon Jun Kim, Bo Kun Kim, Young Hoon Lim
Journal of the Korean Fracture Society.2012; 25(3): 191. CrossRef
- Treatment of Fractures of the Distal Radius Using Variable-Angle Volar Locking Plate
- 964 View
- 21 Download
- 3 Crossref

- Radiologic Reduction Loss after Surgical Treatment of Distal Radius Fracture
- Heun Guyn Jung, Jin Bae Choi, Seung Yong Seo, Yong Soo Choi
- J Korean Fract Soc 2006;19(4):454-459. Published online October 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.4.454
-
 Abstract
Abstract
- PURPOSE
To compare and analyse radiologic reduction loss between fixation with K-wire only group and fixation with K-wire and external fixator group for surgical treatment of distal radial fracture.
MATERIALS AND METHOD
We analysed 60 patients who received the operative treatment with K-wire fixation only or K-wire and external fixator and also were in regular follow up at least one year. We compared radiologic reduction loss of radial length, radial inclination and volar tilt between immediate post-operative radiograph and latest follow up radiograph according to operative methods, fracture patterns and age groups.
RESULTS
Reduction loss of volar tilt was greater in fixation with K-wire only group than fixation with K-wire and external fixator group (p<0.05). Reduction losses of radial length and radial inclination were more in intra-articular subgroup than extra-articular subgroup in fixation with K-wire only group (p<0.05). No significant difference of reduction loss was noted between intra-articular and extra-articular subgroups in fixation with K-wire and external fixator group.
CONCLUSION
More radiologic reduction loss can be expected in fixation with K-wire only group for intra-articular distal radius fracture compared with extra-articular distal radius fracture. Additional external fixation should be added in intra-articular distal radius fracture to reduce radiologic reduction loss.
- 315 View
- 0 Download

- Treatment of the Unstable Distal Radius Fracture with External Fixation and Bone Cement in Elderly Patients
- Dong Chul Kim, Suc Hyun Kweon, Dae Moo Shim, Churl Hong Chun, Ha Heon Song, Jeung Woo Kim
- J Korean Fract Soc 2006;19(3):352-356. Published online July 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.3.352
-
 Abstract
Abstract
- PURPOSE
To evaluate the functional and radiologic results in the using of external fixation with bone cement (polymethylmethacrylate, PMMA) for unstable, osteoporotic distal radius fractures in elderly patients that have high morbidity and chronic medical problems.
MATERIALS AND METHODS
We retrospectively analyzed 12 cases of 12 patients who were treated by external fixation and bone cement for unstable distal radius fractures in the aged persons with poor general condition from January 2003 to July 2004 and followed over one year. We analyzed the radiologic results, and measured the ranges of motion and grip strengths. Functional results were evaluated using the Modified Mayo Wrist Scoring System.
RESULTS
Radiographically, mean volar tilt, mean radial inclination and mean radial length were 8.33o, 24.66 mm and 11.31o respectively on the last follow-up. The mean arc of range of motion was 74.4% of that the uninjured side, and the mean grip strength was 78.0% of that the contralateral side. The average Modified Mayo Wrist Score was 78.3. There were reflex sympathetic dystrophy in a case and pin tract infection in 3 cases as complications associated with external fixator.
CONCLUSION
External fixation and bone cement is useful method for radial length maintenance, preventing reduction loss, restoring the articular surface, early exercise of the wrist joint without morbidity of donor site for unstable distal radius fractures requiring autogenous bone graft in the elderly patients.
- 324 View
- 0 Download

- External Fixation with Five Pins for Unstable Fractures of the Distal Radius
- Kyoung Duck Kwak, Cheol Eun Ko, Seung Il Baek, Sang Min Ahn, Chan Jong Jung, Ki Baek Ahn, Jae Su Roh
- J Korean Fract Soc 2006;19(3):346-351. Published online July 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.3.346
-
 Abstract
Abstract
- PURPOSE
To evaluate the results of five-pin external fixation, with the fifth pin stabilizing the distal radius articular fragment, for unstable distal radial fractures.
MATERIALS AND METHODS
Twenty cases of unstable distal radial fractures were treated with five-pin external fixation (5-pin group). The fifth pin was inserted into the distal articular fragment and attached to the external fixation frame. Metacarpal pins were removed at sixth week in 12 cases and at third in 8 cases, and radial pins were removed at eighth or ninth week. The radiographic results of 5-pin group were compared with those of 20 cases of traditional four-pin external fixation (4-pin group).
RESULTS
The postoperative radial inclination was 23.1 degrees in 5-pin group and 22.2 degrees in 4-pin group; while at last follow-up 21.8o and 15.1 degrees respectively. Postoperative volar tilt was 8.5 degrees and 7.3o; while at last follow-up 6.3 degrees and 0.1 degrees respectively. Postoperative radial shortening was 0.3 mm, 0.4 mm; while at last follow-up 1.1 mm and 2.1 mm respectively. In 5-pin group, there were no significant differences in results whether the metacarpal pins were removed at sixth or third week.
CONCLUSION
Five-pin external fixation, with the fifth pin stabilizing the distal articular fragment, enhanced early motion of the wrist maintaining fracture stability in unstable fractures of the distal radius.
- 283 View
- 0 Download

- Treatment of Distal Radius Fractures Using the Percutaneous K-wire Reduction-Fixation and External Fixator
- Sang Jin Cheon, Ja Gyung Ku, Dong Ho Lee, Hui Taek Kim, Jeung Tak Suh
- J Korean Fract Soc 2006;19(2):228-235. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.228
-
 Abstract
Abstract
- PURPOSE
To analyse the results of treatment of unstable intra-articular distal radius fractures using the percutaneous K-wire reduction-fixation and external fixator.
MATERIALS AND METHODS
A retrospective follow-up study of 22 cases was carried out. With use of the system of AO classification 9 cases were in C1 and 7 in C2, and 6 in C3. The average duration of follow-up for all fractures was 35 months. We evaluated the radiologic results, the functional results according to clinical evaluation scoring system by Green and O'Brien and osteoarthritis grade according to arthritic grading system by Knirk and Jupiter.
RESULTS
Excellent and good results were rated in 17 cases (77%) of all cases. At last follow-up the mean loss of radial length, radial inclination and volar tilt were 1.4 mm, 1.0o, and 1.4o respectively. Also 7 patients had grade I, 1 patient grade II, and 1 patient grade III arthritis.
CONCLUSION
We think that percutaneous K-wire reduction-fixation and external fixation is useful treatment method for the unstable intra-articular distal radius fracture. But severely comminuted AO type C3 fractures would need additional treatments such as open reduction and bone graft to acquire and maintain the articular reduction for better results. -
Citations
Citations to this article as recorded by- Management of Comminuted Intra-articular Fractures of the Distal Radius: Arthroscopically Assisted Reduction and Pin Fixation Supplemented with External Fixation
Jong-Pil Kim, Hyun-Jin Yu
The Journal of the Korean Orthopaedic Association.2009; 44(2): 233. CrossRef - Comparison of Outcomes for Unstable Distal Radius Intraarticular Fractures - T-locking Compression Plate versus External Fixator -
Chul-Hyun Cho, Su-Won Jung, Sung-Won Sohn, Chul Hyung Kang, Ki-Cheor Bae, Kyung-Jae Lee
Journal of the Korean Fracture Society.2008; 21(1): 51. CrossRef - Volar T-Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
Chul Hyun Cho, Ki Choer Bae, Doo Hyun Kwon
Journal of the Korean Fracture Society.2008; 21(3): 220. CrossRef
- Management of Comminuted Intra-articular Fractures of the Distal Radius: Arthroscopically Assisted Reduction and Pin Fixation Supplemented with External Fixation
- 505 View
- 0 Download
- 3 Crossref

- Distal Radioulnar Joint Injuries Associated with Intra-articular Fracture of Distal Radius
- Woo Sik Kim, Yong Sang Kim, Whan Yong Chung, Woo Suk Lee, Taek Soo Jeon, Seung Ryul Ryu
- J Korean Fract Soc 2006;19(2):221-227. Published online April 30, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.2.221
-
 Abstract
Abstract
- PURPOSE
To evaluate the significance of distal radioulnar joint injury which may affect the postoperative radiologic and clinical results of AO classification, type C distal radius fractures.
MATERIALS AND METHODS
From October 2000 to October 2005, 58 patients of AO classification, type C distal radius fracture, who had been treated with operative methods were studied. They are thirty-six men and twenty-two women. The average follow up period was 14 months. The patients were divided into five groups. In the first group (13 cases), there was no distal radioulnar joint injuries. In the second group (20 cases), there were ulnar styloid fractures. In the third group (11 cases), there were separation of distal radioulnar joint. In the fourth group (9 cases), there were ulnar styloid fractures with separation of distal radioulnar joint. In the fifth group (5 cases), there were displacement of ulna in sagittal plane. We measured the radial length, radial inclination and volar tilt in plain radiograph in each group and analyzed the results through Scheck's methods. To analyzed the clinical results, we used the Demerit Point System by Sarmiento.
RESULTS
There was no significant differences in radiologic and clinical results among the five groups.
CONCLUSION
According to compairing the radiologic results of each group which was suspicious of distal radioulnar joint injuries, in the intraarticular comminuted fractures of distal radius, the distal radioulnar joint injuries did not affect the results of treatment when anatomical reduction of distal radius was achieved. -
Citations
Citations to this article as recorded by- Treatment of Distal Radioulnar Joint Injuries Associated with a Distal Radius Fracture
Ki-Bum Choi, Sung-Woo Huh, Seong-Eun Kim, Jung-Woo Lee, Seok-Whan Song, Seung-Koo Rhee
Journal of the Korean Society for Surgery of the Hand.2012; 17(4): 147. CrossRef
- Treatment of Distal Radioulnar Joint Injuries Associated with a Distal Radius Fracture
- 584 View
- 0 Download
- 1 Crossref

- External Fixator and External Fixator Supplemented with K-wire in the Treatment of Distal Radius Fractures
- Sang Wook Bae, Ho Yoon Kwak, Baik Yong Song, Young Joo Ahn
- J Korean Fract Soc 2005;18(3):311-316. Published online July 31, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.3.311
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the differences of the outcome between external fixator and external fixator supplemented with K-wire in the treatment of distal radius fractures.
MATERIALS AND METHODS
Twenty-one cases which underwent external fixation (external fixation group) and 28 cases, external fixation supplemented with K-wire (external fixation with K-wire group), were analyzed. Radial length, radial inclination and volar tilt were compared in preoperative, immediate postoperative radiographs, and radiographs after removal of external fixator between two groups. And functional outcome including flexion, extension, pronation and supination of wrist were compared between two groups and wrist pain, as well.
RESULT
Radial length and radial inclination in the postoperative radiographs and radiographs after removal of external fixator showed no difference between two groups, but volar tilt of external fixation group measured 2.1+/-4.2 degrees, 1.3+/-3.8 degrees and external fixation with K-wire group, 8.8+/-2.3 degrees, 8.5+/-2.4 degrees respectively, so that external fixation with K-wire group showed better reduction and maintenance. Wrist flexion and extension about postoperative 6 months measured 25.6+/-8.2 degrees, 25.1+/-10.2 degrees, respectively, in external fixation group and 42.5+/-15.2 degrees, 33.6+/-9.5 degrees in external fixation with K-wire group, so that external fixation with K-wire group showed better functional results.
CONCLUSION
In the treatment of distal radius fractures, to obtain better reduction and function result, external fixations supplemented with K-wire need to be taken into consideration.
- 378 View
- 1 Download

- Clinical Results after Percutaneous Surgical Treatment of Intra-articular Fracture of the Distal Radius
- Jae Ryong Cha, Jung Hoei Ku, Hyung Lae Cho, Jin Wan Kim, Yoo Dae Kim, Young Il Park, Seong Hwak Hong
- J Korean Fract Soc 2005;18(3):304-310. Published online July 31, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.3.304
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the clinical and radiologic results of percutaneous surgical treatment of the intra-articular fractures of the distal radius, we have compared the results of percutaneous pinning and the combination of percutaneous pinning with external fixation after closed reduction.
MATERIALS AND METHODS
We analysed the results of 52 patients with intra-articular fracture who received the operative treatment with closed reduction in the period of June, 1995 to June, 2001 and also were in regular follow-up at least one year. We used the subjective analysis by Cole & Obletz and the objective analysis by Scheck.
RESULTS
We have found the outcome that 83.3% of percutaneous pinning were graded above "Good" in type B and C1 and 82.2% of the combination treatment of percutaneous pinning with external fixation were graded above "Good" in type C2 and C3.
CONCLUSION
The percutaneous pinning and external fixator after closed reduction in intra-articular fractures of the distal radius are considered useful to restore the articular congruity and make good clinical results.
- 297 View
- 0 Download

- Treatment of Fractures of the Distal Radius using Locking Compression Plate
- Jae Cheon Sim, Nam Sik Chung, Ki Do Hong, Sung Sik Ha, Ji Hoon Kang
- J Korean Fract Soc 2005;18(2):100-104. Published online April 30, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.2.100
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the usefulness of locking compression plate (LCP) and volar plating through anterior approach for distal radius fracture.
MATERIALS AND METHODS
We retrospectively analysed that 15 distal radius fracture, which would not be reduced by closed reduction or too comminuated to maintain reduction or articular surface inconguency, were treated by open reduction through anterior approach and volar plating using LCP. The results were evaluated by preoperative and postoperative radiographs. Functional results were analysed using the Modified Mayo Wrist Scoring System.
RESULTS
All cases achieved anatomical articular surface reduction postoperatively. In terms of radiologic analysis, mean radial length (9.0 mm vs. 11.8 mm), radial inclination (14.7degrees vs. 20.9degrees ), volar tilt (-6.3degrees vs. 8.3degrees ) and articular step-off (1.4 mm vs. 0.3 mm) were improved. The average Modified Wrist Score was 89. Nonunion or malunion was not occurred.
CONCLUSION
Open reduction through anterior approach and volar plating using LCP is a useful method that provides excellent results with few complications in the treatment of fracture of the distal radius. -
Citations
Citations to this article as recorded by- Periprosthetic Fracture after Locked Plating in the Osteoporotic Long Bone Fracture
Ki-Chul Park, Hong-Sik Kim, Jeong-Han Oh
Journal of the Korean Orthopaedic Association.2012; 47(3): 222. CrossRef - 2.4 mm Volar Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
Sung-Jin Kim, Chul-Hyun Cho
Journal of the Korean Fracture Society.2011; 24(2): 151. CrossRef - Treatment of Femur Supracondylar Fracture with Locking Compression Plate
Seong Ho Bae, Seung Han Cha, Jeung Tak Suh
Journal of the Korean Fracture Society.2010; 23(3): 282. CrossRef - Comparison of Outcomes for Unstable Distal Radius Intraarticular Fractures - T-locking Compression Plate versus External Fixator -
Chul-Hyun Cho, Su-Won Jung, Sung-Won Sohn, Chul Hyung Kang, Ki-Cheor Bae, Kyung-Jae Lee
Journal of the Korean Fracture Society.2008; 21(1): 51. CrossRef - Basic Principle of the Locking Compression Plate
Keun Bae Lee
Journal of the Korean Fracture Society.2008; 21(3): 261. CrossRef - Volar T-Locking Compression Plate for Treatment of Unstable Distal Radius Fractures
Chul Hyun Cho, Ki Choer Bae, Doo Hyun Kwon
Journal of the Korean Fracture Society.2008; 21(3): 220. CrossRef
- Periprosthetic Fracture after Locked Plating in the Osteoporotic Long Bone Fracture
- 550 View
- 1 Download
- 6 Crossref

- Intramedullary K-wire Fixation for Displaced Fracture of Distal Radius
- Byung Woo Ahn, Chong Kwan Kim, Jong Youl Lee, Chae Ik Chung, Jong Ho Yoon, Young Min Kim, Jin Woo Jin, Kang Hoon Kim, Guk Sang Chung, Dong Wook Kim
- J Korean Fract Soc 2005;18(1):54-59. Published online January 31, 2005
- DOI: https://doi.org/10.12671/jkfs.2005.18.1.54
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate indications and effectiveness of intramedullary K-wire fixation for distal radial fractures.
MATERIALS AND METHODS
Twenty one fractures of distal radius treated with intramedullary K-wire fixation from April 2001 to September 2002 were evaluated. The mean age was 67.8(range 46~82). Severely comminuted intra-articular fractures and Barton's fractures were excluded. One or two K-wires were added percutaneously. To assess the functional result, we used Green and O'Brien score system. The radiographic assessment included a scoring system based on measurements of radial length, radial inclination, volar tilt and step-off of the radial articular surface.
RESULTS
Average follow up period was 13.5 months. In functional result, excellent and good result were obtained in 18 cases (86%). In radiologic result, mean loss of radial length, radial inclination and volar tilt were 0.9 mm, 1.4degrees, 0.9degrees, respectively.
CONCLUSION
The advantages of intramedullary K-wire fixation were relatively simple procedure, low occurrence of soft tissue complications and early wrist motion. Intramedullary K-wire fixation was good to maintaining reduction in osteoporotic bone.
- 330 View
- 1 Download

- T-Plate Fixation for Fractures of Distal Radius
- Jae Yeol Choi, Hwa Jae Jung, Hong Kyun Kim, Jong Keun Lee, Il Sung Chang
- J Korean Fract Soc 2004;17(4):350-358. Published online October 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.4.350
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To review the result of fractures of distal radius treated with the T-plate fixation and to recommend guideline for treatment of fracture of distal radius.
MATERIALS AND METHODS
Between January 1999 and December 2002, among the patients with fractures of distal radius underwent T-plate fixation, we retrospectively reviewed 52 cases that had a minimum follow-up of 12 months. According to the Fernandez classification of distal radius fractures, 18 cases were type I, 4 cases were type II, 22 cases were type III, 2 cases were type IV and 6 cases were type V. To assess the clinical result, we used the Demerit Point System and for the radiologic result, we used the Point system by Scheck. We Compare the result of treatment in fractures of distal radius by T-plate fixation and K-wire fixation in Type I and III.
RESULTS
Excellent to good results were obtained in 38 cases (73%) in clinical result and 39 cases (75%) in radiological results. Radiologic evidence of arthritis was presented 6 cases at follow-up examination. There was no evidence of statistical difference between Type I using T-plate and K-wire fixation (p>0.05). However in type III, result in the group of T-plate fixation were better than in pinning group (p<0.05).
CONCLUSION
We obtained good result for type III with T-plate but only T-plate fiaxtion for type V was not satisfactory -
Citations
Citations to this article as recorded by- Flexor Pollicis Longus Tendon Rupture as a Complication of a Closed Distal Radius Fracture - A Case Report -
Do-Young Kim, Eun-Min Seo, Woo-Dong Nam, Seung-Jae Park, Sang-Soo Lee
Journal of the Korean Fracture Society.2011; 24(2): 191. CrossRef
- Flexor Pollicis Longus Tendon Rupture as a Complication of a Closed Distal Radius Fracture - A Case Report -
- 502 View
- 1 Download
- 1 Crossref

- The Usefulness of Non-operative Treatment of Distal Radius Fracture in Elderly Patients
- Ki Ser Kang, Han Jun Lee, Sang Hak Lee
- J Korean Fract Soc 2004;17(4):345-349. Published online October 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.4.345
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To disclose the correlation between the functional and radiologic results of the treatment of distal radius fracture in elderly patients by non-operative versus operative treatment.
MATERIALS AND METHODS
From January 1995 to December 2000, 36 patients, more than 60 years old with fractures of distal radius were treated and followed up for more than one year. We classified them using the Fernandez classification and evaluated functional and radiological results according to the subjective point system of Cole & Obletz and objective evaluation by Scheck.
RESULTS
In functional result, excellent to good results were obtained in 12 cases (71%) in the non-operative group and 14 cases (74%) in the operative group, there were no evidence of statistical difference between two groups (p>0.05). In radiographic results, mean radial inclination, loss of radial length and volar tilt were 13degree, 12.3 mm, 7.2degrees in the non-operative goup and 5.2degrees, 5.1 mm, 3.3degrees in the operative group on last follw-up radiographs, there were evidence of statistical difference between two groups (p<0.05).
CONCLUSION
Operative treatment is radiographically better result in distal radius of elderly patients but functional satisfaction is not significantly related with radiographic result. When we decide the treatment of elderly patients, non-operative treatment can be useful method, considering with patient's age and activity status.
- 323 View
- 0 Download

- Surgical Treatment of Fractures of the Distal Radius in Patients Older Than 65 Years
- Jeung Tak Suh, Dae Woong Kim, Chong Il Yoo
- J Korean Soc Fract 2003;16(4):563-569. Published online October 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.4.563
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the results of surgical treatment of the displaced distal radius fractures in elderly patients over 65 years old who were treated with percutaneous K-wire fixation only and percutaneous K-wire fixation with external fixation. MATERIAL AND METHOD: We evaluated 24 cases of the distal radius fracture in patients older than 65 years from January 1998 to December 2001. The patients were followed up at least 12 months postoperatively. We compared the surgical results of 14 cases, treated with percutaneous K-wire fixation only with the surgical results of 10 cases, treated with percutaneous K-wire fixation with external fixation. We evaluated the functional results according to demerit point system and the radiographic results (radial length, radial inclination, volar tilt).
RESULTS
According to demerit point system, the mean score of demerit point was 9.9 in the group of percutaneous K-wire fixation and 5.3 in the group of percutaneous K-wire with external fixation respectively (p<0.05). In radiographic results, the percent of the mean loss of radial length, radial inclination and volar tilt were 23.2%, 12% and 41.7% in the group of percutaneous K-wire fixation and 11%, 5.9% and 27.4% in the group of percutaneous K-wire with external fixation respectively (p<0.05).
CONCLUSION
Percutaneous K-wire with external fixation showed better functional and radiographic results than percutaneous K-wire fixation only for the treatment of the displaced distal radius fractures in elderly patients older than 65 years and percutaneous K-wire with external fixation is thought to be a one of the most effective treatment of the displaced distal radius fractures in elderly patients. -
Citations
Citations to this article as recorded by- Osteoporotic Distal Radius Fracture-conservative Treatment
Seok-Whan Song
Journal of the Korean Fracture Society.2008; 21(1): 81. CrossRef
- Osteoporotic Distal Radius Fracture-conservative Treatment
- 503 View
- 3 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


