Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 30(2); 2017 > Article
-
Original Article
- Ultrasonographic Assessment of the Pronator Quadratus Muscle after Surgical Treatment for Distal Radius Fractures
- Dong Hyuk Choi, M.D., Hyun Kyun Chung, M.D., Ji Won Lee, M.D., Cheol Hwan Kim, M.D., Yong Soo Choi, Ph.D.
-
Journal of the Korean Fracture Society 2017;30(2):69-74.
DOI: https://doi.org/10.12671/jkfs.2017.30.2.69
Published online: April 18, 2017
Department of Orthopedic Surgery, Kwangju Christian Hospital, Gwangju, Korea.
- Correspondence to: Yong Soo Choi, Ph.D. Department of Orthopedic Surgery, Kwangju Christian Hospital, 37 Yangrim-ro, Nam-gu, Gwangju 61661, Korea. Tel: +82-62-650-5064, Fax: +82-62-650-5066, stemcellchoi@naver.com
Copyright © 2017 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 582 Views
- 6 Download
- 1 Crossref
Abstract
-
Purpose
- This study was to assess the morphological changes of the pronator quadratus (PQ) muscle using an ultrasonography in the volar locking plate fixation group and in the percutaneous K-wire fixation group for distal radius fracture, and to evaluate the impact on clinical outcomes.
-
Materials and Methods
- Fifty-four patients who received surgical treatment for distal radius fracture were enrolled in this study. They were divided into two groups according to treatment modality: Group 1 included 34 patients who underwent internal fixation with volar locking plate and Group 2 included 20 patients with percutaneous K-wire fixation. Thickness of the PQ muscle was measured using an ultrasonography at the final follow-up. We evaluated the outcomes using the Mayo wrist score, wrist range of motion, and grip strength at the final follow-up.
-
Results
- Compared with the uninjured side, thickness of the PQ muscle showed 31.9% of mean atrophy in Group 1 and 11.4% in Group 2. The atrophy of PQ muscle was severe in Group 1 (p=0.01). However, there was no significant difference in the mean Mayo wrist score between the two groups (83.1±10.9 in Group 1 and 80.2±8.9 in Group 2, p=0.28), except a mild limitation of pronation in Group 1.
-
Conclusion
- The healed PQ muscle from fracture itself after distal radius fracture revealed a morphological atrophy. Moreover, the volar locking plate resulted in greater atrophy of the PQ muscle, but there was no specific impact on clinical outcomes.
- 1. Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop, 2003;27:1-6.ArticlePDF
- 2. Knox J, Ambrose H, McCallister W, Trumble T. Percutaneous pins versus volar plates for unstable distal radius fractures: a biomechanic study using a cadaver model. J Hand Surg Am, 2007;32:813-817.Article
- 3. Lee KH. Volar plating of distal radius fractures. J Korean Fract Soc, 2008;21:325-333.Article
- 4. Orbay JL, Badia A, Indriago IR, et al. The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Up Extrem Surg, 2001;5:204-211.Article
- 5. Ahsan ZS, Yao J. The importance of pronator quadratus repair in the treatment of distal radius fractures with volar plating. Hand (N Y), 2012;7:276-280.Article
- 6. Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma, 2007;21:316-322.Article
- 7. Hershman SH, Immerman I, Bechtel C, Lekic N, Paksima N, Egol KA. The effects of pronator quadratus repair on outcomes after volar plating of distal radius fractures. J Orthop Trauma, 2013;27:130-133.Article
- 8. Sofka CM. Ultrasound of the hand and wrist. Ultrasound Q, 2014;30:184-192.Article
- 9. Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP 3rd, Linscheid RL. Scaphoid malunion. J Hand Surg Am, 1989;14:679-687.Article
- 10. Stuart PR. Pronator quadratus revisited. J Hand Surg Br, 1996;21:714-722.ArticlePDF
- 11. Gordon KD, Dunning CE, Johnson JA, King GJ. Influence of the pronator quadratus and supinator muscle load on DRUJ stability. J Hand Surg Am, 2003;28:943-950.Article
- 12. McConkey MO, Schwab TD, Travlos A, Oxland TR, Goetz T. Quantification of pronator quadratus contribution to isometric pronation torque of the forearm. J Hand Surg Am, 2009;34:1612-1617.Article
- 13. Armangil M, Bezirgan U, Başarır K, Bilen G, Demirtaş M, Bilgin SS. The pronator quadratus muscle after plating of distal radius fractures: is the muscle still working? Eur J Orthop Surg Traumatol, 2014;24:335-339.ArticlePDF
- 14. Swigart CR, Badon MA, Bruegel VL, Dodds SD. Assessment of pronator quadratus repair integrity following volar plate fixation for distal radius fractures: a prospective clinical cohort study. J Hand Surg Am, 2012;37:1868-1873.Article
REFERENCES
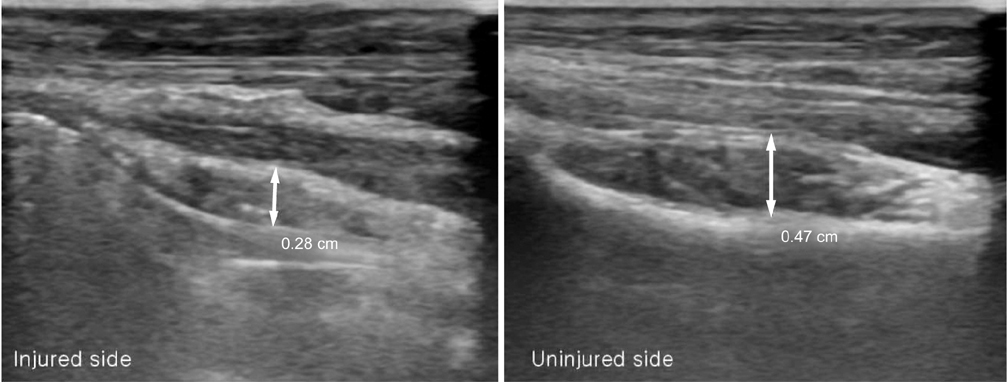
Ultrasound examination in longitudinal view shows a significant decrease (40%) in the thickness of pronator quadratus muscle (arrows) at postoperative 21 months of volar locking plate.
Demographic Characteristics
Values are presented as median (range), number (%), or mean±standard deviation. Group 1: patients of distal radius fractures treated with volar locking plate, Group 2: patients of distal radius fractures treated with percutaneous K-wire, BMI: body mass index, BMD: bone mineral density, AO: arbeitsgemeinschaft für osteosyntheses.
Thickness of the Pronator Quadratus Muscle at the Final Follow-Up
| Variable | Group 1 | Group 2 | p-value |
|---|---|---|---|
| Injured side (mm) | 3.2±0.9 (68.1) | 3.9±1.1 (88.6) | 0.01 |
| Uninjured side (mm) | 4.7±0.9 | 4.4±0.9 | 0.27 |
| p-value* | <0.001 | 0.002 |
Clinical Outcomes at the Final Follow-Up
Figure & Data
REFERENCES
Citations

- Quantitative analysis of radial torsion angle according to location with CT scan
Eic Ju Lim, Seungyeob Sakong, Jeong Seok Choi, Wonseok Choi, Jong-Keon Oh, Jae-Woo Cho
Injury.2025; 56(10): 112634. CrossRef
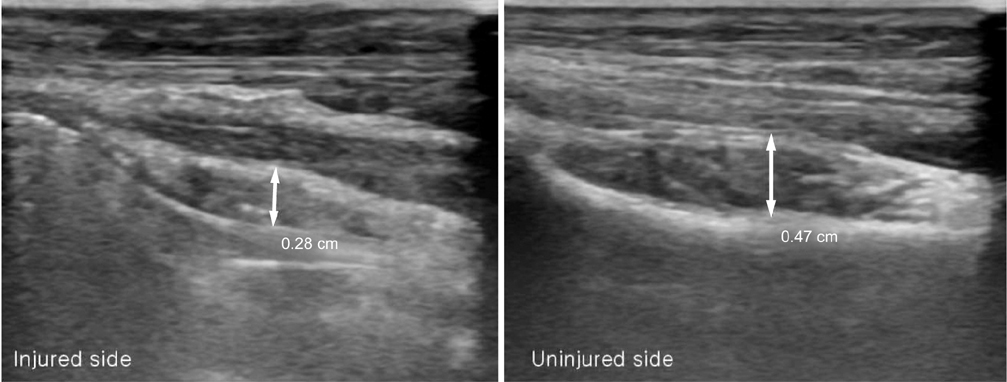
Fig. 1
Demographic Characteristics
| Variable | Group 1 (n=34) | Group 2 (n=20) | p-value |
|---|---|---|---|
| Mean age (yr) | 59.9 (42–84) | 57.1 (27–68) | 0.10 |
| Gender | 0.90 | ||
| Female | 25 (73.5) | 15 (75.0) | |
| Male | 9 (26.5) | 5 (25.0) | |
| Injured side | 0.89 | ||
| Dominant | 21 (61.8) | 13 (65.0) | |
| Non-dominant | 13 (38.2) | 7 (35.0) | |
| Mean follow-up (mo) | 19.1 (12–33) | 19.2 (12–36) | 0.82 |
| BMI | 22.8±2.4 | 22.8±2.5 | 0.96 |
| BMD (T-score) | −2.5±0.9 | −2.3±0.6 | 0.42 |
| AO fracture type | 0.76 | ||
| A | 3 (8.8) | 3 (15.0) | |
| B | 10 (29.4) | 6 (30.0) | |
| C | 21 (61.8) | 11 (55.0) |
Values are presented as median (range), number (%), or mean±standard deviation. Group 1: patients of distal radius fractures treated with volar locking plate, Group 2: patients of distal radius fractures treated with percutaneous K-wire, BMI: body mass index, BMD: bone mineral density, AO: arbeitsgemeinschaft für osteosyntheses.
Thickness of the Pronator Quadratus Muscle at the Final Follow-Up
| Variable | Group 1 | Group 2 | p-value |
|---|---|---|---|
| Injured side (mm) | 3.2±0.9 (68.1) | 3.9±1.1 (88.6) | 0.01 |
| Uninjured side (mm) | 4.7±0.9 | 4.4±0.9 | 0.27 |
| p-value* | <0.001 | 0.002 |
Values are presented as mean±standard deviation (percent of uninjured side). Group 1: patients of distal radius fractures treated with volar locking plate, Group 2: patients of distal radius fractures treated with percutaneous K-wire.
*p-value: comparison with uninjured side in each group.
Clinical Outcomes at the Final Follow-Up
| Variable | Group 1 | Group 2 | p-value |
|---|---|---|---|
| Mayo wrist score | 83.1±10.9 | 80.2±8.9 | 0.28 |
| Range of motion (°) | |||
| Extension | 63.1±9.7 (94.9) | 61.9±7.4 (94.6) | 0.86 |
| Flexion | 68.6±16.3 (93.4) | 65.6±8.1 (92.4) | 0.50 |
| Supination | 86.7±6.0 (98.5) | 81.0±7.8 (97.5) | 0.93 |
| Pronation | 67.3±9.0 (83.3) | 79.7±9.2 (98.1) | 0.02 |
| Ulnar deviation | 26.2±4.2 (93.2) | 26.3±2.7 (92.4) | 0.24 |
| Radial deviation | 18.5±2.0 (94.4) | 17.4±2.7 (92.5) | 0.61 |
| Grip strength (kg) | 21. 6±8.6 (91. 2) | 22.1±7.4 (91.3) | 0.84 |
Values are presented as mean±standard deviation (percent of uninjured side). Group 1: patients of distal radius fractures treated with volar locking plate, Group 2: patients of distal radius fractures treated with percutaneous K-wire.
Values are presented as median (range), number (%), or mean±standard deviation. Group 1: patients of distal radius fractures treated with volar locking plate, Group 2: patients of distal radius fractures treated with percutaneous K-wire, BMI: body mass index, BMD: bone mineral density, AO: arbeitsgemeinschaft für osteosyntheses.
Values are presented as mean±standard deviation (percent of uninjured side). Group 1: patients of distal radius fractures treated with volar locking plate, Group 2: patients of distal radius fractures treated with percutaneous K-wire. *p-value: comparison with uninjured side in each group.
Values are presented as mean±standard deviation (percent of uninjured side). Group 1: patients of distal radius fractures treated with volar locking plate, Group 2: patients of distal radius fractures treated with percutaneous K-wire.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

