Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 37(4); 2024 > Article
-
Original Article
- Does the Operator’s Experience Affect the Occurrence of Complications after Distal Radius Fracture Volar Locking Plate Fixation? A Comparative Study of the First Four Years and Thereafter
-
Kee-Bum Hong, M.D.*,†
 , Chi-Hoon Oh, M.D., Ph.D.‡
, Chi-Hoon Oh, M.D., Ph.D.‡ , Chae Kwang Lim, M.D.*,†
, Chae Kwang Lim, M.D.*,† , Sungwoo Lee, M.D.*,†
, Sungwoo Lee, M.D.*,† , Soo-Hong Han, M.D., Ph.D.‡
, Soo-Hong Han, M.D., Ph.D.‡ , Jun-Ku Lee, M.D., Ph.D.*,†
, Jun-Ku Lee, M.D., Ph.D.*,†
-
Journal of Musculoskeletal Trauma 2024;37(4):175-183.
DOI: https://doi.org/10.12671/jmt.2024.37.4.175
Published online: October 25, 2024
*Department of Orthopedic Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea
†Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea
‡Department of Orthopedic Surgery, CHA Bundang Medical Center, Seongnam, Korea
- Correspondence to: Jun-Ku Lee, M.D., Ph.D. Department of Orthopedic Surgery, National Health Insurance Service Ilsan Hospital, 100 Ilsan-ro, Ilsandong-gu, Goyang 10444, Korea Tel: +82-31-900-0340 Fax: +82-31-900-0343 E-mail: jg197@naver.com
- Chi-Hoon Oh’s current affiliation: Department of Orthopedic Surgery, Korea University Ansan Hospital, Ansan, Korea
© 2024 The Korean Fracture Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,593 Views
- 53 Download
- 2 Crossref
Abstract
-
Purpose The management of distal radius fractures (DRFs) has evolved with the introduction of volar locking plate (VLP) fixation, offering stable fixation and better outcomes. Nevertheless, the impact of the surgeon’s experience on the complication rates in VLP fixation remains to be determined, particularly for less-experienced surgeons. This study compared the complication rates during the initial four years and subsequent two years of a hand surgeon’s practice of VLP fixation for DRFs.
-
Materials and Methods The data between March 2016 and December 2022 were analyzed retrospectively under the Institutional Review Board approval. A single surgeon performed all VLP fixation surgeries after finishing regular hand surgery training, with the first four years representing the less experienced phase (Group 1) and the following two years indicating the experienced phase (Group 2). The patients’ characteristics, operation-related factors, and postoperative complications, including tendon injuries, nerve-related complications, fixation and instrument-related issues, osteosynthesis-related problems, and infections, were compared. In addition, the authors compared the data with a large multicenter study conducted by experienced hand surgeons.
-
Results Three hundred and nineteen patients (321 wrists) were included. The mean age was 63.3 years, and 26.3% were male and 73.7% were female. The operation time was 53.7±14.5 minutes and 74.4±26.5 minutes in groups 1 and 2, respectively, which was statistically significantly shorter (p<0.001). The complication rates between the two groups were similar, except for the higher implant removal rates in Group 1. A comparison with a previous multicenter study revealed higher reduction losses and carpal tunnel syndrome in this study, but the overall complication rate was low.
-
Conclusion In DRF management, when the operating surgeon has completed an accredited training course, VLP fixation is a good treatment method that can be performed effectively even by less experienced surgeons with low complication rates.
Introduction
Materials and Methods
Results
1) Tendon related
2) Nerve related
3) Fixation and instrument related
4) Osteosynthesis related
5) Infection
6) Others
Discussion
Conclusion
| Characteristic | Group 1 (157 patients) | Group 2 (162 patients) | p-value |
|---|---|---|---|
| Sex | 0.422 | ||
| Female | 112 (71.3) | 123 (75.9) | |
| Male | 45 (28.7) | 39 (24.1) | |
| Age (yr) | 61.6±12.6 | 64.8±14.7 | 0.038* |
| Weight (kg) | 61.9±10.9 | 62.1±12.4 | 0.907 |
| Height (m) | 1.6±0.1 | 1.6±0.1 | 0.389 |
| BMI (kg/m2) | 24.5±3.9 | 24.1±3.6 | 0.465 |
| Group 1 (159 wrists) | Group 2 (162 wrists) | p-value | |
|---|---|---|---|
| Fractured arm | 0.204 | ||
| Right | 68 (42.8) | 83 (51.2) | |
| Left | 91 (57.2) | 79 (48.8) | |
| AO-OTA classification | 0.133 | ||
| A2 | 24 (15.1) | 12 (7.4) | |
| A3 | 21 (13.2) | 26 (16.0) | |
| B2 | 6 (3.8) | 3 (1.9) | |
| B3 | 10 (6.3) | 12 (7.4) | |
| C1 | 26 (16.4) | 24 (14.8) | |
| C2 | 35 (22.0) | 53 (32.7) | |
| C3 | 37 (23.3) | 32 (19.8) | |
| Ulnar fracture combined | 0.904 | ||
| None | 55 (34.6) | 54 (33.3) | |
| Yes | 104 (65.4) | 108 (66.7) | |
| Preoperative duration (d) | 3.9±5.4 | 5.2±10.8 | 0.169 |
| Operation time (min) | 74.4±26.5 | 53.7±14.5 | <0.001* |
| Union time (d) | 53.5±25.7 | 53.5±23.6 | 0.988 |
| Total follow-up duration (d) | 292.6±240.9 | 213.3±146.0 | <0.001* |
| Complication | Group 1 (159 wrists) | Group 2 (162 wrists) | p-value | |
|---|---|---|---|---|
| Tendon injury | Tendon rupture | 4 (2.5) | 3 (1.9) | |
| Flexor tendon rupture | 1 (0.6) | 1 (0.6) | >0.999 | |
| Extensor tendon rupture | 3 (1.9) | 2 (1.2) | 0.987 | |
| Nerve related | Palmar sensory branch damage of median nerve | 2 (1.3) | 1 (0.6) | 0.628 |
| CRPS | 1 (0.6) | 3 (1.9) | 0.628 | |
| Carpal tunnel syndrome | 13 (8.2) | 17 (10.5) | 0.602 | |
| Acute | 0 | 3 (1.9) | ||
| Subacute | 9 (5.7) | 7 (4.3) | ||
| Delayed | 4 (2.5) | 7 (4.3) | ||
| Carpal tunnel release | 3 (1.9) | 9 (5.6) | 0.102 | |
| Fixation and instrument related | Reduction loss | 8 (5.0) | 3 (1.9) | 0.136 |
| Implant failure or screw breakage | 4 (2.5) | 1 (0.6) | 0.211 | |
| Screw penetration | 3 (1.9) | 1 (0.6) | 0.368 | |
| Implant removal | 42 (26.4) | 18 (11.1) | 0.001* | |
| Osteosynthesis | Delayed union | 0 | 2 (1.2) | 0.486 |
| Non-union | 0 | 0 | - | |
| Infection | Superficial | 1 (0.6) | 3 (1.9) | 0.628 |
| Deep | 0 | 0 | - | |
| Others | Compartment | 0 | 0 | - |
| Radial artery injury | 2 (1.3) | 0 | 0.470 | |
| This study (321 wrists in 319 patients) | Lee et al.5) (2020) (1,955 wrists in 1,921 patients) | p-value | ||
|---|---|---|---|---|
| Age (yr) | 63.3±13.8 | 60.3±14.6 | ||
| Sex | Male | 84 (26.3) | 587 (30.6) | 0.205 |
| Female | 235 (73.7) | 1,334 (69.4) | ||
| Complication | ||||
| Tendon injury | Tendon rupture | 7 (2.2) | 21 (1.1) | 0.106 |
| Flexor tendon rupture | 2 (0.6) | 9 (0.5) | >0.999 | |
| Extensor tendon rupture | 5 (1.6) | 12 (0.6) | 0.141 | |
| Nerve related | Palmar sensory branch damage of median nerve | 3 (0.9) | 9 (0.5) | 0.502 |
| CRPS | 4 (1.2) | 15 (0.8) | 0.587 | |
| Carpal tunnel syndrome | 30 (9.3) | 36 (1.8) | <0.001* | |
| Carpal tunnel release | 12 (3.7) | 17 (0.9) | <0.001* | |
| Fixation and Instrument related | Reduction loss | 11 (3.4) | 4 (0.2) | <0.001* |
| Implant failure including screw loosening or breakage | 5 (1.6) | 6 (0.3) | 0.010* | |
| Screw penetration in joint | 4 (1.2) | 26 (1.3) | >0.999 | |
| Implant removal | 60 (18.7) | 511 (26.1) | 0.005* | |
| Osteosynthesis | Delayed union | 2 (0.6) | 5 (0.3) | 0.577 |
| Non-union | 0 | 3 (0.2) | >0.999 | |
| Infection | Superficial | 4 (1.2) | 83 (4.2) | 0.015* |
| Deep | 0 | 2 (0.1) | >0.999 | |
| Others | Compartment | 0 | 2 (0.1) | >0.999 |
| Radial artery injury | 2 (0.6) | 3 (0.2) | 0.307 | |
- 1. Tang JB: Distal radius fracture: diagnosis, treatment, and controversies. Clin Plast Surg, 41: 481-499, 2014.PubMed
- 2. Wilcke MK, Hammarberg H, Adolphson PY: Epidemiology and changed surgical treatment methods for fractures of the distal radius: a registry analysis of 42,583 patients in Stockholm County, Sweden, 2004-2010. Acta Orthop, 84: 292-296, 2013.PubMedPMC
- 3. Hevonkorpi TP, Launonen AP, Huttunen TT, Kannus P, Niemi S, Mattila VM: Incidence of distal radius fracture surgery in Finns aged 50 years or more between 1998 and 2016 - too many patients are yet operated on? BMC Musculoskelet Disord, 19: 70, 2018.ArticlePubMedPDF
- 4. Medoff RJ, Saucedo JM: Common errors of volar plate fixation. In: del Piñal F, Haerle M, Krimmer H eds. Distal radius fractures and carpal instabilities. FESSH IFSSH 2019 Instructional Book. Thieme: 146-148, 2019.
- 5. Lee JH, Lee JK, Park JS, et al: Complications associated with volar locking plate fixation for distal radius fractures in 1955 cases: a multicentre retrospective study. Int Orthop, 44: 2057-2067, 2020.ArticlePubMedPDF
- 6. Tang JB: Re: Levels of experience of surgeons in clinical studies. J Hand Surg Eur Vol, 34: 137-138, 2009.ArticlePubMedPDF
- 7. Wolfe SW: Distal radius fractures. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS eds. Green’s operative hand surgery. 7th ed. Elsevier: 516-587, 2017.
- 8. Soong M, Earp BE, Bishop G, Leung A, Blazar P: Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am, 93: 328-335, 2011.ArticlePubMed
- 9. Lee JK, Bang JY, Choi YS, Kim TH, Yu WJ, Han SH: Extensor pollicis longus tendon rupture caused by a displaced dorsal "beak" fragment of Lister's tubercle in distal radius fractures. Handchir Mikrochir Plast Chir, 51: 199-204, 2019.ArticlePubMed
- 10. Tang JB, Giddins G: Why and how to report surgeons’ levels of expertise. J Hand Surg Eur Vol, 41: 365-366, 2016.ArticlePubMedPDF
- 11. Yamamoto M, Fujihara Y, Fujihara N, Hirata H: A systematic review of volar locking plate removal after distal radius fracture. Injury, 48: 2650-2656, 2017.ArticlePubMed
- 12. Tan A, Chong A: Reasons for implant removal after distal radius fractures. J Hand Surg Asian Pac Vol, 21: 321-325, 2016.ArticlePubMed
- 13. Lee JK, Lee Y, Kim C, Kim M, Han SH: Volar locking plate removal after distal radius fracture: a 10-year retrospective study. Arch Orthop Trauma Surg, 141: 1711-1719, 2021.ArticlePubMedPDF
- 14. Orbay JL, Badia A, Indriago IR, et al: The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Up Extrem Surg, 5: 204-211, 2001.Article
- 15. Costa ML, Achten J, Rangan A, Lamb SE, Parsons NR: Percutaneous fixation with Kirschner wires versus volar locking-plate fixation in adults with dorsally displaced fracture of distal radius: five-year follow-up of a randomized controlled trial. Bone Joint J, 101-B: 978-983, 2019.ArticlePubMedPMCPDF
- 16. Jeudy J, Steiger V, Boyer P, Cronier P, Bizot P, Massin P: Treatment of complex fractures of the distal radius: a prospective randomised comparison of external fixation 'versus' locked volar plating. Injury, 43: 174-179, 2012.ArticlePubMed
- 17. McFadyen I, Field J, McCann P, Ward J, Nicol S, Curwen C: Should unstable extra-articular distal radial fractures be treated with fixed-angle volar-locked plates or percutaneous Kirschner wires? A prospective randomised controlled trial. Injury, 42: 162-166, 2011.ArticlePubMed
- 18. Orbay JL, Fernandez DL: Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am, 29: 96-102, 2004.ArticlePubMed
- 19. Twigt B, Bemelman M, Lansink K, Leenen L: Type C distal radial fractures treated with conventional AO plates: an easy and cost-saving solution in a locking plate era. Int Orthop, 37: 483-488, 2013.ArticlePubMedPMCPDF
- 20. Orbay JL: The treatment of unstable distal radius fractures with volar fixation. Hand Surg, 5: 103-112, 2000.ArticlePubMed
- 21. Ruch DS, McQueen MM: Distal radius and ulna fractures. In: Bucholz RW, Beaty JH, Rockwood CA, Green DP eds. Rockwood and Green’s fractures in adults. Lippincott Williams & Wilkins: 829-880, 2010.
- 22. Lee JK, Yoon BH, Kim B, et al: Is early mobilization after volar locking plate fixation in distal radius fractures really beneficial? A meta-analysis of prospective randomized studies. J Hand Ther, 36: 196-207, 2023.ArticlePubMed
- 23. Cafarelli L, El Amiri L, Facca S, Chakfé N, Sapa MC, Liverneaux P: Anterior plating technique for distal radius: comparing performance after learning through naive versus deliberate practice. Int Orthop, 46: 1821-1829, 2022.ArticlePubMedPDF
References
Figure & Data
REFERENCES
Citations

- Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2025; 38(1): 40. CrossRef - Characteristics of patients with distal radius fracture requiring arthroscopic foveal repair after bone union
Min Jung Park, Cheungsoo Ha, Hyun Tak Kang, Yong Hyun Yoon, Jun-Ku Lee, Soo-Hong Han
Arthroscopy and Orthopedic Sports Medicine.2025; 12(2): 70. CrossRef
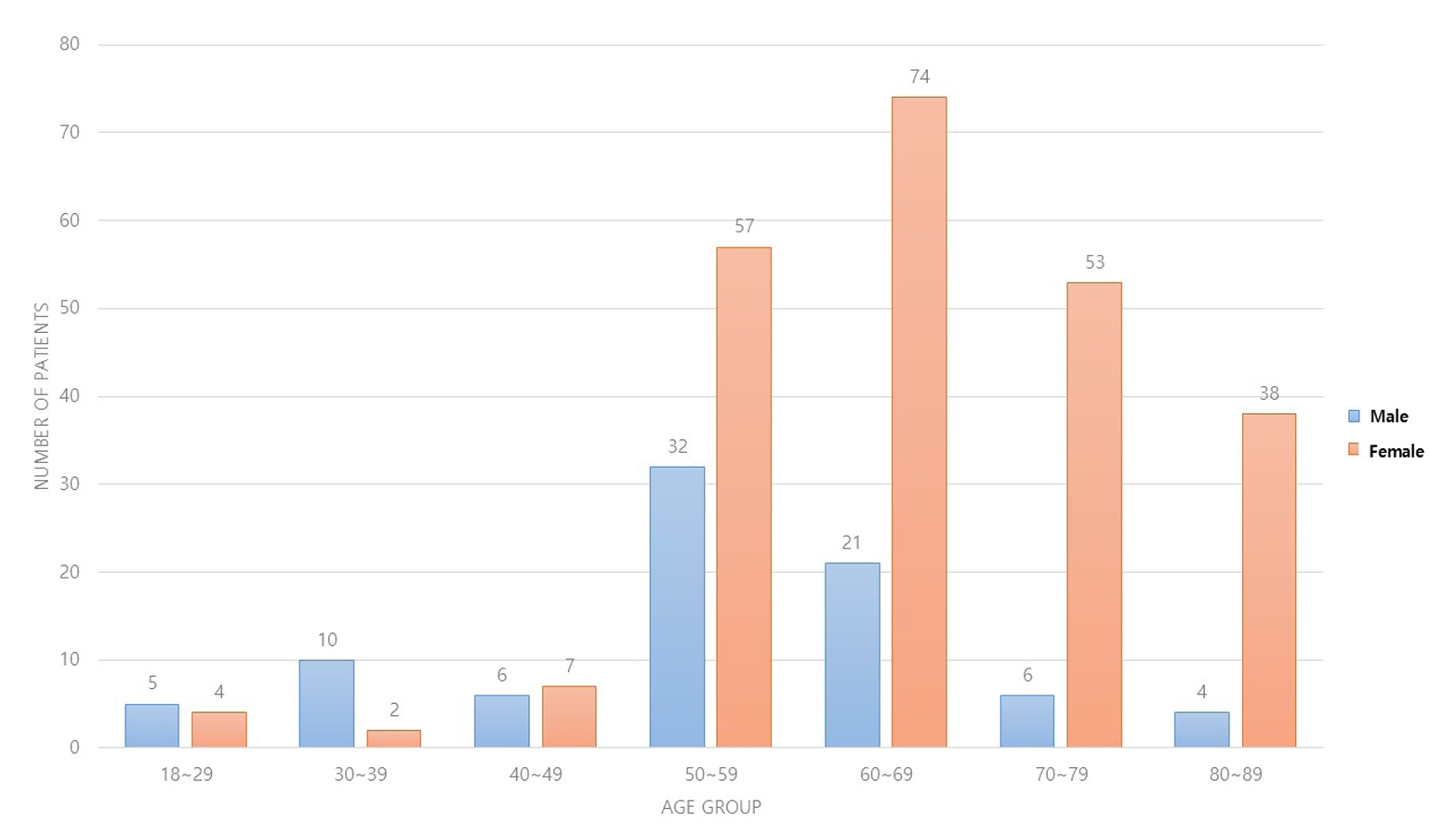
Fig. 1.
| Characteristic | Group 1 (157 patients) | Group 2 (162 patients) | p-value |
|---|---|---|---|
| Sex | 0.422 | ||
| Female | 112 (71.3) | 123 (75.9) | |
| Male | 45 (28.7) | 39 (24.1) | |
| Age (yr) | 61.6±12.6 | 64.8±14.7 | 0.038 |
| Weight (kg) | 61.9±10.9 | 62.1±12.4 | 0.907 |
| Height (m) | 1.6±0.1 | 1.6±0.1 | 0.389 |
| BMI (kg/m2) | 24.5±3.9 | 24.1±3.6 | 0.465 |
| Group 1 (159 wrists) | Group 2 (162 wrists) | p-value | |
|---|---|---|---|
| Fractured arm | 0.204 | ||
| Right | 68 (42.8) | 83 (51.2) | |
| Left | 91 (57.2) | 79 (48.8) | |
| AO-OTA classification | 0.133 | ||
| A2 | 24 (15.1) | 12 (7.4) | |
| A3 | 21 (13.2) | 26 (16.0) | |
| B2 | 6 (3.8) | 3 (1.9) | |
| B3 | 10 (6.3) | 12 (7.4) | |
| C1 | 26 (16.4) | 24 (14.8) | |
| C2 | 35 (22.0) | 53 (32.7) | |
| C3 | 37 (23.3) | 32 (19.8) | |
| Ulnar fracture combined | 0.904 | ||
| None | 55 (34.6) | 54 (33.3) | |
| Yes | 104 (65.4) | 108 (66.7) | |
| Preoperative duration (d) | 3.9±5.4 | 5.2±10.8 | 0.169 |
| Operation time (min) | 74.4±26.5 | 53.7±14.5 | <0.001 |
| Union time (d) | 53.5±25.7 | 53.5±23.6 | 0.988 |
| Total follow-up duration (d) | 292.6±240.9 | 213.3±146.0 | <0.001 |
| Complication | Group 1 (159 wrists) | Group 2 (162 wrists) | p-value | |
|---|---|---|---|---|
| Tendon injury | Tendon rupture | 4 (2.5) | 3 (1.9) | |
| Flexor tendon rupture | 1 (0.6) | 1 (0.6) | >0.999 | |
| Extensor tendon rupture | 3 (1.9) | 2 (1.2) | 0.987 | |
| Nerve related | Palmar sensory branch damage of median nerve | 2 (1.3) | 1 (0.6) | 0.628 |
| CRPS | 1 (0.6) | 3 (1.9) | 0.628 | |
| Carpal tunnel syndrome | 13 (8.2) | 17 (10.5) | 0.602 | |
| Acute | 0 | 3 (1.9) | ||
| Subacute | 9 (5.7) | 7 (4.3) | ||
| Delayed | 4 (2.5) | 7 (4.3) | ||
| Carpal tunnel release | 3 (1.9) | 9 (5.6) | 0.102 | |
| Fixation and instrument related | Reduction loss | 8 (5.0) | 3 (1.9) | 0.136 |
| Implant failure or screw breakage | 4 (2.5) | 1 (0.6) | 0.211 | |
| Screw penetration | 3 (1.9) | 1 (0.6) | 0.368 | |
| Implant removal | 42 (26.4) | 18 (11.1) | 0.001 |
|
| Osteosynthesis | Delayed union | 0 | 2 (1.2) | 0.486 |
| Non-union | 0 | 0 | - | |
| Infection | Superficial | 1 (0.6) | 3 (1.9) | 0.628 |
| Deep | 0 | 0 | - | |
| Others | Compartment | 0 | 0 | - |
| Radial artery injury | 2 (1.3) | 0 | 0.470 | |
| This study (321 wrists in 319 patients) | Lee et al.5) (2020) (1,955 wrists in 1,921 patients) | p-value | ||
|---|---|---|---|---|
| Age (yr) | 63.3±13.8 | 60.3±14.6 | ||
| Sex | Male | 84 (26.3) | 587 (30.6) | 0.205 |
| Female | 235 (73.7) | 1,334 (69.4) | ||
| Complication | ||||
| Tendon injury | Tendon rupture | 7 (2.2) | 21 (1.1) | 0.106 |
| Flexor tendon rupture | 2 (0.6) | 9 (0.5) | >0.999 | |
| Extensor tendon rupture | 5 (1.6) | 12 (0.6) | 0.141 | |
| Nerve related | Palmar sensory branch damage of median nerve | 3 (0.9) | 9 (0.5) | 0.502 |
| CRPS | 4 (1.2) | 15 (0.8) | 0.587 | |
| Carpal tunnel syndrome | 30 (9.3) | 36 (1.8) | <0.001 |
|
| Carpal tunnel release | 12 (3.7) | 17 (0.9) | <0.001 |
|
| Fixation and Instrument related | Reduction loss | 11 (3.4) | 4 (0.2) | <0.001 |
| Implant failure including screw loosening or breakage | 5 (1.6) | 6 (0.3) | 0.010 |
|
| Screw penetration in joint | 4 (1.2) | 26 (1.3) | >0.999 | |
| Implant removal | 60 (18.7) | 511 (26.1) | 0.005 |
|
| Osteosynthesis | Delayed union | 2 (0.6) | 5 (0.3) | 0.577 |
| Non-union | 0 | 3 (0.2) | >0.999 | |
| Infection | Superficial | 4 (1.2) | 83 (4.2) | 0.015 |
| Deep | 0 | 2 (0.1) | >0.999 | |
| Others | Compartment | 0 | 2 (0.1) | >0.999 |
| Radial artery injury | 2 (0.6) | 3 (0.2) | 0.307 | |
Values are presented as number (%) or mean±standard deviation. Group 1: comprising cases within the first four years, Group 2: covering the subsequent four years until the study’s conclusion. p<0.05.
Values are presented as number (%) or mean±standard deviation. Group 1: comprising cases within the first four years, Group 2: covering the subsequent four years until the study’s conclusion. p<0.05.
Values are presented as number (%). Group 1: comprising cases within the first four years, Group 2: covering the subsequent four years until the study’s conclusion. p<0.05. CRPS: complex regional pain syndrome.
Values are presented as mean±standard deviation or number (%). Group 1: comprising cases within the first four years, Group 2: covering the subsequent four years until the study’s conclusion. p<0.05. CRPS: complex regional pain syndrome.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 ePub Link
ePub Link Cite
Cite

