Abstract
-
Background
In severe comminuted metaphyseal distal radius fracture (DRF) of elderly patients, after maintaining only radiological parameters of the radius using long volar locking plates (VLPs), we inevitably eliminated a few volar cortical fragments of metaphysis. Here, we report the final radiological and clinical outcomes of our method.
-
Methods
For the patients who were treated between 2014 and 2018, the demographic factors, the preoperative radiologic factors, area of the eliminated volar cortical fragment, and final radiologic parameter, were evaluated. Clinical outcomes and ranges of active motion were evaluated.
-
Results
In total, 31 patients were included. The mean patient age was 77.3 years and the mean eliminated cortical area was 3.30 cm2. At the final follow-up, the mean volar tilt, radial inclination, articular step-off, and ulnar variance were 10.35°, 20.00°, 0.58 mm, and 0.71 mm, respectively. There were no definitive correlations between bone mineral density, fragment area, the largest cortical fragment diameter ratio and differences in final and immediate postoperative measurements of these radiological parameters, respectively. Visual analog scale and disabilities of the arm, shoulder, and hand (DASH) scores were satisfactory, and the mean arcs of flexion-extension and pronation-supination were 124.35° and 133.23°. Clinical outcomes were not significantly different according to the AO system category.
-
Conclusions
For maintenance of radiological parameters of the radius, long VLPs are useful in older patients with DRFs who exhibit volar metaphyseal comminution, despite concurrent ulnar fractures. Inevitable elimination of irreducible free comminuted cortical fragments when filling the defect does not affect final radiological and clinical outcomes.
-
Level of Evidence
Level of evidence: Level IV, case series.
-
Keywords: Metaphysis, Comminuted fracture, Wrist fractures, Ulna
Introduction
Distal radius fractures (DRFs) are the most common upper limb fractures, comprising more than 16% of all fractures [
1]. However, it remains difficult to treat high-energy fractures of the distal radius involving both an intra-articular component and metaphyseal comminution with diaphyseal extension. Furthermore, this type of fracture occasionally occurs just after a simple slippage in elderly patients over 70 years. These fractures are difficult to manage partly because of specific biological and mechanical aspects that must be considered when treating intra-articular fractures with proximal extension. Volar locking plates (VLPs) have been designed with longer shapes to cover more proximal metaphysis and diaphysis. These plates are considered useful for the management of volar comminuted fractures of the distal radius, which involve proximal extension into the diaphysis, and with their use, the complications of external fixation or dorsal bridging of distraction plates can be avoided or minimized [
2,
3].
On the other hand, a few fracture fragments have been considered essential for proper union in several anatomical areas of among the overall skeleton, such as the medial calcar fragments in the proximal humerus or femur [
4-
6]. Since the development of locking plates/screws and their implementation worldwide, the AO principle has been used to investigate several mechanical and biological aspects of comminuted fragment healing [
4]. The principle also suggests placement of the plate on the bony surface under conditions of distractive force. However, in older patients with low bone mineral density (BMD), low-energy injuries occasionally result in severe comminuted metaphyseal DRFs. Furthermore, it could be extremely difficult to fix and maintain for each volar fragment with long VLP.
In particular, for the maintenance of the radial length during plating and surgical manipulations (e.g., distal traction), a few free fragments never contact with other fragments, inevitably. Thus, we hypothesized the inevitable elimination for these irreducible fragments of volar cortex with comminution would not affect the final outcomes, if the radiological parameters of the radius were restored using long VLPs. Here, we report the final radiological and clinical outcomes of this procedure after at least 2 years of follow-up, along with factors that may influence these outcomes.
Methods
Ethics Statement
The study was approved by the Institutional Review Board of Chungnam National University Hospital (IRB No. 2021-09-056) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient Selection
We retrospectively analysed patients who had been diagnosed with DRFs at Chungnam National University Hospital between March 2014 and September 2018. Among 522 patients screened for analysis, 34 were included in the study. Patients were selected based on the following criteria: (1) age >70 years; (2) independent living before injury; (3) the presence of irreducible comminuted volar fragments at distal metaphysis or diaphysis (at least 0.5×0.5 cm2); (4) fixation with a long VLP for DRF with the inevitable elimination of one or more cortical fragments; (5) the presence of preoperative three-dimensional computed tomography (3D CT) images for the evaluation of fragment size; and (6) the availability of complete medical records and radiological data for at least 2 years postoperatively.
The exclusion criteria were (1) unstable concurrent ulnar fracture [
7,
8]; (2) other ipsilateral upper extremity injuries; (3) previous history of DRF treatment with conservative or surgical methods; (4) multiple comorbidities (i.e., >3 chronic diseases requiring medication); (5) history of trauma in the same wrist and/or neurological involvement; (6) atypical forearm fracture or administration of high-dose bisphosphonate as adjuvant chemotherapy for malignancy (e.g., breast cancer or multiple myeloma) [
9,
10]; (7) presence of symptomatic arthritis in the distal radioulnar joint at the time of surgery; and/or (8) comorbid autoimmune connective tissue disease requiring long-term steroid therapy.
Demographic factors were evaluated, including age, sex, smoking status, comorbidities (diabetes or other medical diseases) and BMD. In particular, BMD was measured at the time of diagnosis of osteoporosis and atypical fracture using a Lunar Prodigy dual-energy X‐ray absorptiometry instrument (GE Medical Systems) with enCORE ver. 8.8 (GE Medical Systems). Mean score values from the hip and spine were recorded. The lowest T score for the proximal femur and lumbar spine, except for the Ward area of the proximal femur, was recorded. We reported the level of expertise of the two surgeons as ‘‘Level 4/highly experienced category’’ for surgical practices [
11].
Preoperative radiographs (anteroposterior, lateral, and oblique) and 3D CT images were evaluated to identify the number of articular fragments and the extent of comminution. Fractures were classified using the AO system [
7]. First, the eliminated cortical segment area was measured based on picture archiving and communication system (PACS) software (m-view 5.4; Marosis Technologies Inc.). The fragment area was calculated automatically with the PACS software using the region-of-interest tool (
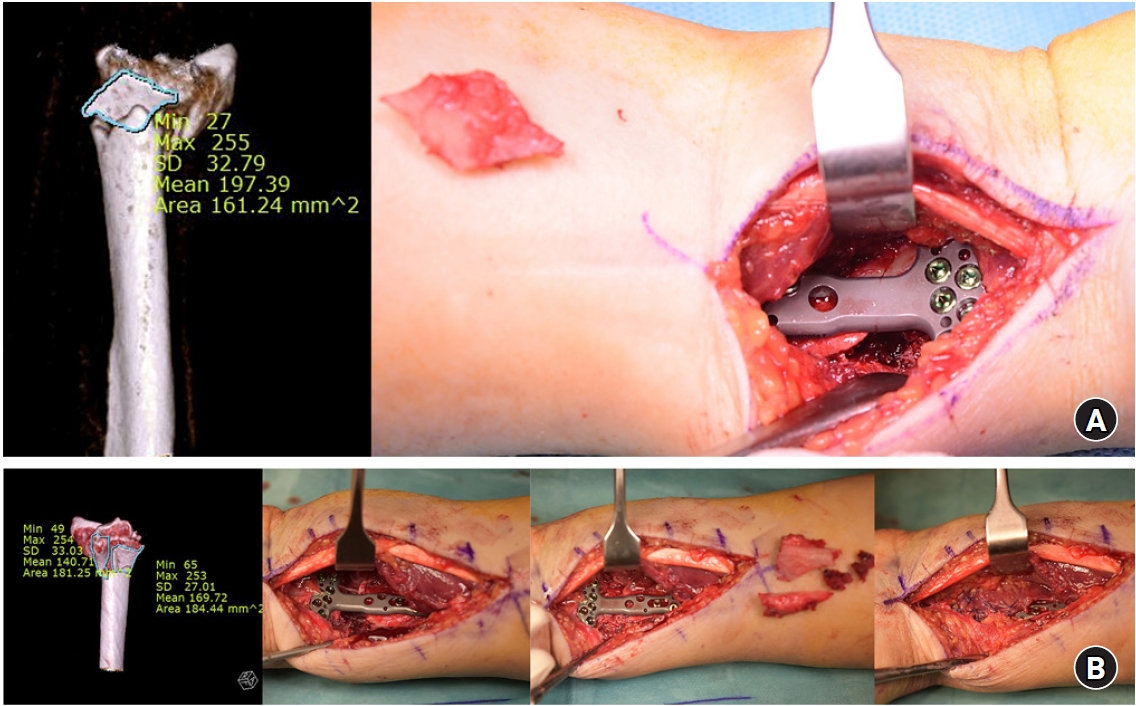
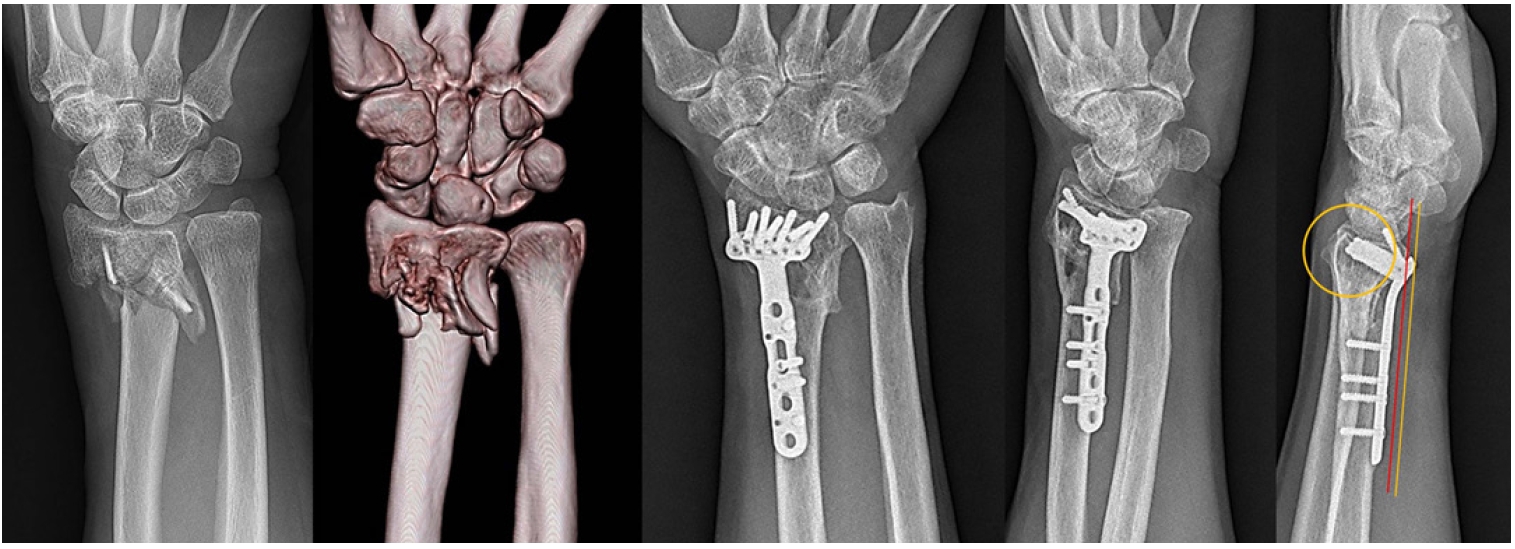
Fig. 1). Furthermore, the widest fragment diameter was measured intraoperatively and the corresponding radius diameter at the fragment location was measured concurrently. Finally, the ratio of the fragment diameter to the radial metaphysis/shaft diameter was evaluated.
Any concurrent distal ulnar fracture was classified using the Q modifier, where Q1 indicates fracture of the ulnar styloid at its base, Q2 indicates simple fracture of the ulnar neck, Q3 indicates comminuted fracture of the ulnar neck, Q4 indicates fracture of the ulnar head, and Q5 indicates fracture of the ulnar head and neck [
7]. Unstable ulnar fractures of this area, despite reduction and internal fixation of the radius, were characterized by two factors determined intraoperatively: malalignment and instability [
7,
8]. Malalignment was arbitrarily defined as >10° angular deformity. Instability of the ulnar fracture after the distal radius had been realigned and fixed was defined as the tendency for fracture fragments to move relative to one another (>50% translation) with passive forearm rotation. Ulnar fractures that met these two criteria were considered unstable and thus, excluded in this study [
7,
8].
The procedure was done with the patient in the supine position on a radiolucent operating table. A longitudinal incision was made slightly radial to the flexor carpi radialis (FCR). Dissection was implemented between the radial artery and FCR. The pronator quadratus was then detached. The incision was extended proximally, depending on the fracture pattern and plate length, along the radial border of the FCR. The fracture site was exposed, and the hematoma was removed by rongeur and curettage. By means of ligamentotaxis with gentle finger traction, metaphyseal comminution was roughly and provisionally reduced with minimal manipulation. Traction was then applied, under fluoroscopic inspection, to determine the initial radial length. Then, cortical screws were fixed in proximal holes until proper compression could be achieved on the volar surface of the radius. Being pulled by assistant orthopedic surgeon, one or two distal locking screws were fixed after confirmation of radial length. During these distal fixations, areas with less comminution were fixed first, if possible, to preserve radial length. Unreducible volar free cortical fragments were then removed (
Fig. 1). In a few patients with intra-articular DRFs, articular step-off was resolved by manipulation using a small elevator through the window of the original fragment location (
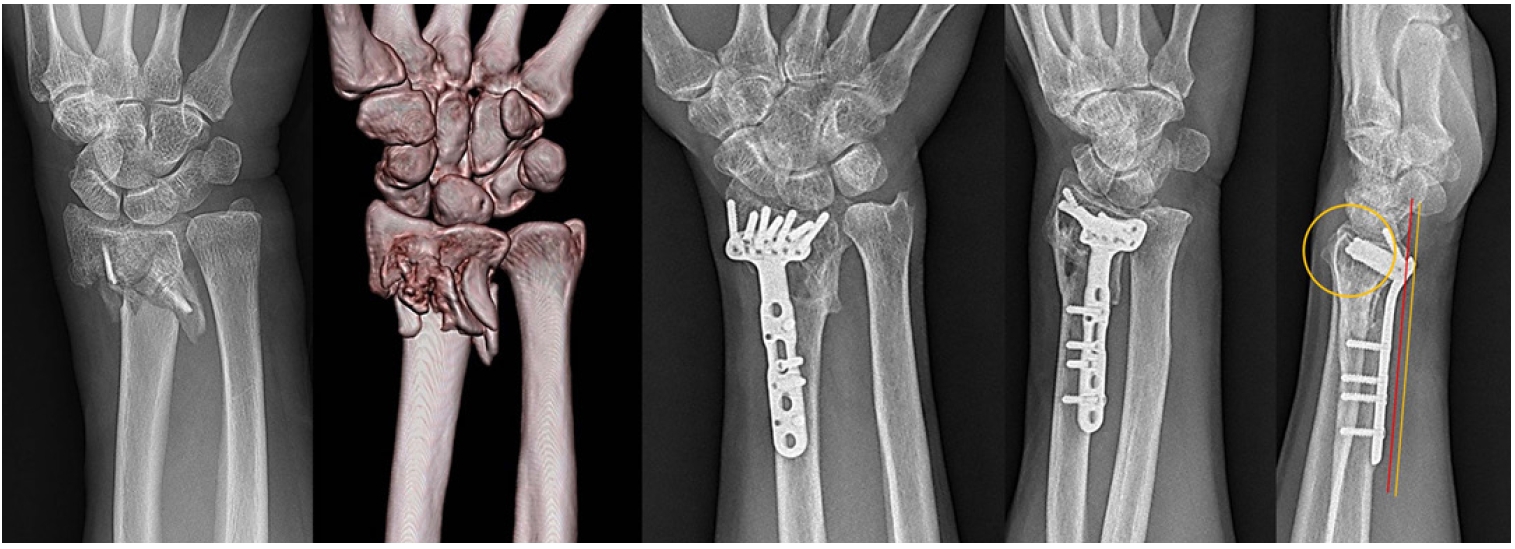
Fig. 2). Following fixation of other locking screws in the distal area, final proximal locking screws were inserted. No concurrent ulnar fractures were fixed surgically. After surgery, the wrist was immobilized in a long-arm splint. Active digit range of motion exercises commenced immediately postoperatively. At 3 weeks postoperatively, the wrist was placed in a short-arm cast for an additional 3 weeks; physiotherapy (active and passive wrist mobilization without the cast) commenced at 6 weeks postoperatively.
Radiological assessments were performed monthly for 3 months after surgery, then at 3-month intervals for 1 year. A final evaluation was conducted at least 2 years after the surgery. Fracture union was defined as >3 regions of bone bridging among the radial, ulnar, dorsal and volar cortical aspects of the distal part of the radius, as observed on anteroposterior, lateral and both oblique projections. Radiographic alignment was characterized by measurements of volar tilt, radial inclination, articular step-off and ulnar variance using standard measurement techniques [
12]. The extra-articular type was defined as a 0-mm step-off. Immediate postoperative measurements and final follow-up measurements were compared. All radiological images were evaluated twice by two orthopedic surgeons not involved in the surgeries, with a 1-day interval between evaluations.
Clinical outcomes were compared between groups at the final follow-up. Data were collected by an independent observer (an orthopedic surgeon) who was not an author of this study. The clinical outcomes were the visual analog scale (VAS) postoperative pain score, the disabilities of the arm, shoulder, and hand (DASH) score, and ranges of active motion. A score of 0 on the VAS indicated no pain, and a score of 10 indicated extreme pain. DASH is a 30-item questionnaire that evaluates limitations with respect to the performance of daily activities, including leisure (four items) and work (four items). Total scores range from 0 to 100. Active motion of the wrist joint was measured using a standardized technique, in which a goniometer was placed dorsally and laterally.
Inter- and Intraobserver Reliabilities of Radiological Measurements
Intraclass correlation coefficients of continuous variables were used as indices of inter- and intraobserver reliabilities [
13]. Kappa values were calculated for categorical variables, such as fracture type [
14], using Fleiss and Cohen’s ranges of >0.75, 0.40–0.75, and <0.40 to indicate excellent, good, and poor outcomes, respectively.
The optimal sample size was calculated based on expected differences in the DASH score. Power analysis revealed that at least 23 patients were needed to detect a minimum difference in DASH score of 15 points between the two groups, with 20% assumed to be lost to follow-up, a type I error rate of 0.05, and a power of 0.8. These values are similar to those reported by Cha et al. [
15] and Beaton et al. [
16]. Associations of BMD, fragment area, and diameter ratio with final radiological outcomes were analysed using Pearson correlation. Categorical variables, such as AO classification and ulnar fracture pattern, were analysed using one-way analysis of variance or Scheffé post-hoc analysis to investigate associations with clinical outcomes. Sample size was calculated using G∗ Power ver. 3.1.9.2 (Heinrich-Heine-Universität Düsseldorf). All data were analysed using IBM SPSS ver. 22.0 (IBM Corp.). In all analyses, P<0.05 was considered to indicate statistical significance.
Results
In total, 31 patients were included in the analysis. The mean patient age was 77.3±4.9 years and the mean eliminated fragment area was 3.30±0.68 cm
2. At the final follow-up, the mean volar tilt, radial inclination, articular step-off, and ulnar variance were 10.35°±1.11°, 20.00°±0.97°, 0.58±0.62 mm, and 0.71±0.82 mm, respectively (
Table 1). There were no definitive correlations between BMD, fragment area, largest fragment diameter ratio, and differences in the final and immediate postoperative measurements of these radiological parameters, respectively (
Table 2). According to the fragment size, there were no differences of bony union at postoperative 3 and 6 months (
Table 3). Furthermore, clinical outcomes in terms of VAS and DASH scores were satisfactory (0.23±0.43 and 6.41±2.38, respectively), and the mean arcs of flexion-extension and pronation-supination were 124.35°±8.34° and 133.23°±8.22°, respectively. Clinical outcomes were not significantly different according to the AO system category (
Table 4). Finally, with the exception of the pronation-supination arc, there were no significant differences among types of concurrent ulnar fracture (
Table 5).
In terms of radiological measurements, both inter- and intraobserver intraclass correlation coefficients indicated high reproducibility [
13]. The κ-values of the category classification of the AO system and ulnar fractures were 0.89 and 0.85, respectively [
14].
Discussion
There were some particular points for treatment of DRFs with volar metaphyseal cortical comminution for elderly patients, compared for fracture healing of the ordinary long bone through the well-established guideline of traumatology (AO principle). First, management of this injury requires basic knowledge concerning the distal one-third of the antebrachium and wrist. Furthermore, the metaphysis in DRFs in older patients exhibits further comminution, osteoporotic features, and concurrent dorsal cortex fragments, compared with ordinary long bone fractures [
17,
18]. Thus, the concepts of lag screw and compressive fixation for inter-segmental or butterfly fragments are difficult to apply. Second, VLPs have been established as an excellent option for a few decades and are associated with minimal complications. In particular, both fixed- and variable-angle VLPs have been used for the fixation of DRF fragments. Therefore, osteoporotic bones can be firmly secured by at least three-fourths of the distal locking screw length, considering the distance from the volar to dorsal cortex [
19]. Furthermore, a distally angulated plate design of approximately 10° in the sagittal plane is essential for the restoration of volar tilt for radiocarpal articular surface by simple plating on the volar surface. To our knowledge, there have been no specific options for the fixture of metaphyseal comminuted DRFs, except for long VLPs marketed by several companies. Accordingly, long dorsal plating (bridging plate) under distractive conditions satisfies the AO principle, but has minimal supporting clinical evidence in this context [
20-
22]. Finally, the values of volar metaphyseal fragments should be estimated in a manner that differs from those of medial calcar fragments in the proximal humerus and femur. Indeed, the thickness and size of these fragments could be critical for fracture healing. However, precise and anatomical reduction with specific fragment geometry is difficult and can be more problematic in terms of radial length maintenance. Therefore, we first focused on length maintenance, then eliminated the resulting free volar cortical fragments, inevitably.
However, one aspect was consistent with the AO principle with the current surgical procedure. Because fragments were removed inevitably, rather than because of failure during attempted reduction, there was minimal manipulation of the metaphysis. Thus, the overall operation time was similar to that of ordinary DRFs. A minimally invasive method was described by Wei et al. [
3], which was very similar to our approach in terms of hypothesis, treatment rationale and outcomes, although it involved preservation of the pronator quadratus. However, considering the basic demographic data and surgical method in the study, Wei et al. [
3] inserted screws only in the most distal rows of distal plate areas. Furthermore, their degrees of comminution and displacement of articular fragments were somewhat less complicated than in our study, so the minimally invasive method may be suitable for some patients. In many of our patients, the comminution around articular area and the articular displacement were definitive, such that fragments reduction and plating were difficult to achieve while preserving the pronator quadratus. In a few patients, articular displacement was manipulated through the window made by comminuted proximal metaphysis fragments, after incision of the pronator quadratus (
Fig. 2).
Although final solid union was achieved, all patients were informed that the VLP should not be removed during the follow-up period, if possible. When necessary, the reasons for removal were median nerve irritation, tendon-related concerns and procedures such as wrist fusion [
19,
23-
27]. Among these, tendon-related concerns were the only risks that could be minimized during plating. Thus, the distal margin of the plate was adjusted to be categorized as "Soong grade 0 or 1” to reduce the risk of flexor attrition [
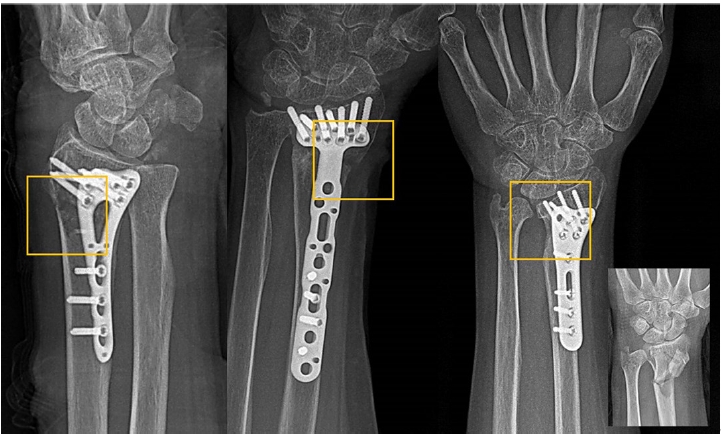
26], and all distal screws were inserted 2–3 mm shorter than the distance to the dorsal cortex for patients with extensor problems (
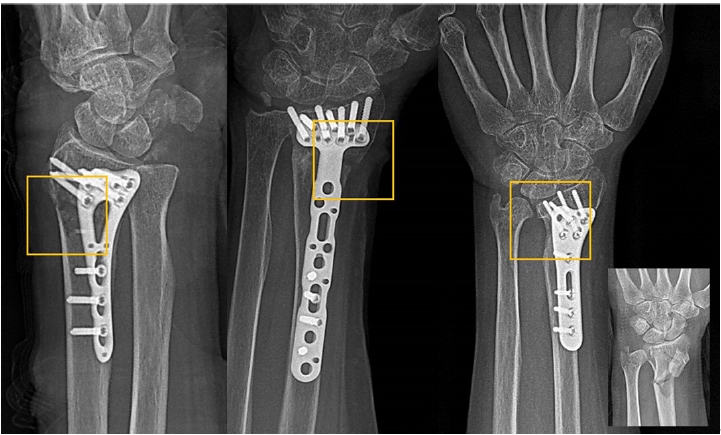
Fig. 3). As expected, the area from which the eliminated cortical fragment had been removed was considered a definitive defect at the final follow-up. However, no patient symptoms or signs merited plate removal.
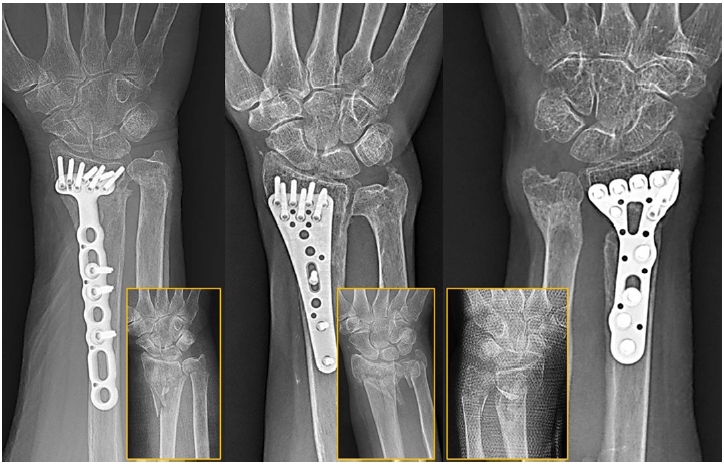
We filled defects caused by cortical fragment elimination with either a morselized cancellous graft from the removed fragment, tricalcium phosphate or demineralized bone matrix. If there were little amount of cancellous bone attached to the cortical fragment, we added synthetic material if the patient agreed, due to its high cost. At the final follow-up, all fractures had healed with various types of cortical defects present in simple radiographs without any signs of non-union, radial shortening or metal breakage (
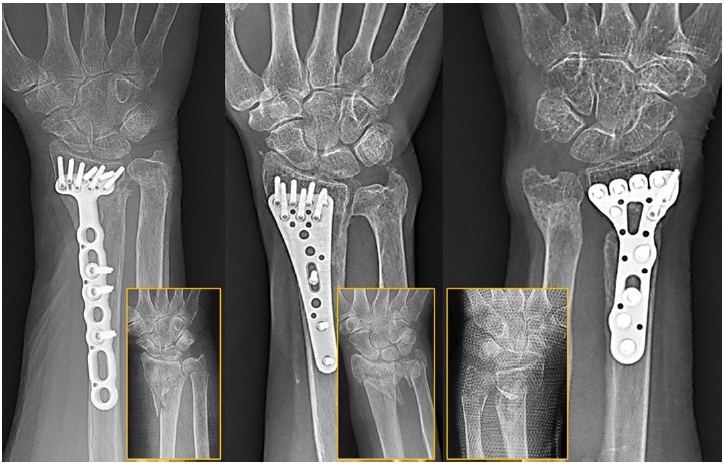
Fig. 4). Although there have been a few comparative studies of materials used to fill comminuted radii in humans [
28-
30], long VLPs can guarantee the restoration of radiological parameters immediately after surgery, regardless of residual metaphyseal defects.
In all patients, concurrent ulnar fractures were treated conservatively in this study. Because many studies have been performed concerning ulnar styloid fractures in DRFs without distal radioulnar joint instability, there is a decreasing need for fixation, especially in older patients [
31,
32]. In this study, a few cases of styloid non-union (Q1) did not affect the final clinical outcomes (
Table 5). Furthermore, the head, neck and metaphysis healed after radius union, following firm VLP fixation. Decisions for conservative treatment of these types of concurrent ulnar fractures, was based on also the several reports since 2010 [
33,
34], thus all concurrent head, neck and metaphyseal ulnar fractures exhibited satisfactory union in this study (
Fig. 5). Patients with Q4 and Q5 ulnar fractures exhibited slight reductions in their pronation-supination arcs, but their daily activities were not limited, and the overall VAS and DASH scores were satisfactory for these patients.
Considering the clinical evaluation, there are two important points related to the older age of our patients. First, some patients had advanced arthritic changes in the radiocarpal joint at the final follow-up, compared with the time of injury. However, their clinical statuses were not compromised. Second, DASH scores revealed incomplete recovery, but the patients’ subjective conditions (including VAS scores) were satisfactory. We presume that these were because most older patients had previously adjusted to physical conditions appropriate for their age, and because of aging-related reductions in demands on the upper extremities [
33].
This study had some limitations. First, it was not a comparative trial. Comparisons among patient groups with similar characteristics (e.g., age, BMD, or fracture pattern) would provide further insight for DRF management. Second, we could not suggest solutions for rare conditions requiring plate removal beyond those described in this article. After plate removal, the cortical defect will be a very vulnerable point for another fracture. Finally, the benefits of inevitable elimination for comminuted fragments rather than fixation or preservation were not compared statistically with control group. Satisfactory radiologic and clinical outcomes with shorter surgery time and easier manipulation should be verified by comparative study in future.
Conclusions
For the maintenance of radiological parameters of the radius, long VLPs are useful for treating elderly patients with DRFs who exhibit metaphyseal comminution, despite concurrent ulnar fractures. The inevitable elimination of irreducible free cortical comminuted fragments does not affect final radiological and clinical outcomes, despite the presence of bony defects in simple radiographs.
Article Information
-
Author contributions
All the work was done by Soo Min Cha.
-
Conflict of interest
None.
-
Funding
This work was supported by the research fund of Chungnam National University.
-
Data availability
Contact the corresponding author for data availability.
Fig. 1.(A) A 73-year-old woman was injured during a fall. A volar cortical metaphyseal fragment with an area of 1.61 cm2 was removed during plating. The defect was filled with demineralized bone matrix. (B) A 78-year-old woman was injured. Two main volar cortical fragments with areas of 1.81 and 1.84 cm2 were removed, and the defects were filled by morselized cancellous bone attached to the corresponding cortex. Min, minimum; Max, maximum; SD, standard deviation.
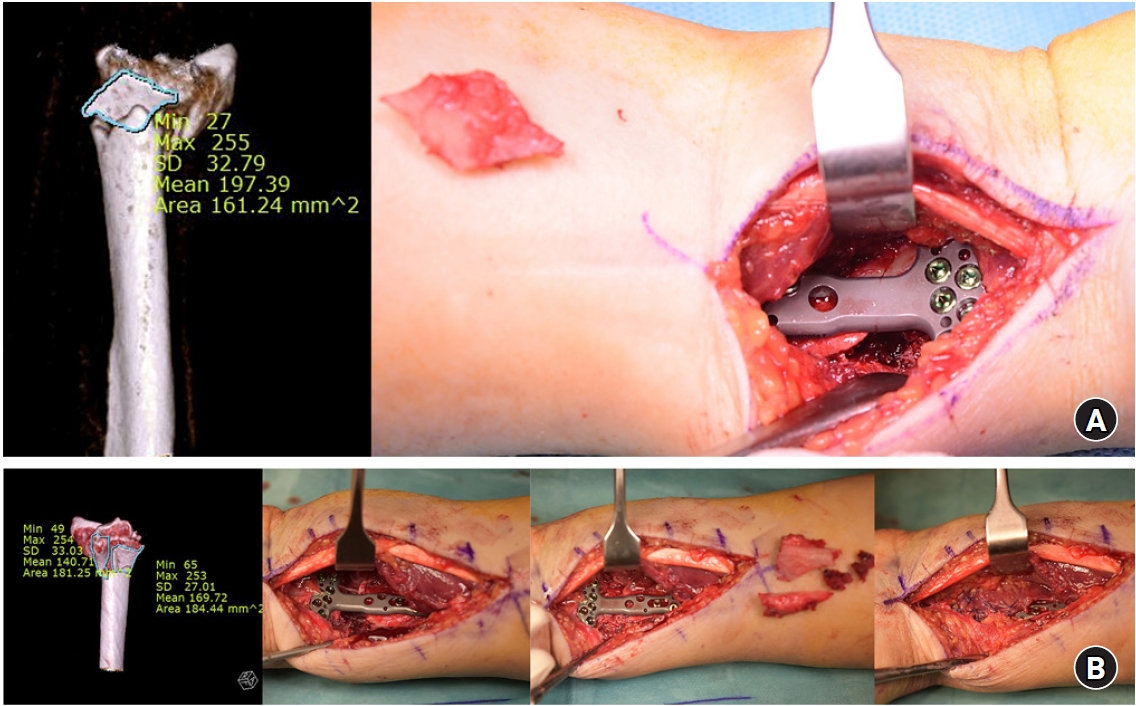
Fig. 2.Intra-articular displacement was manipulated and reduced in the subchondral area through the window generated by the removed volar cortical fragment.

Fig. 3.A3.3 distal radius fracture with multiple comminuted metaphysis. At the final follow-up, the volar tilt and radial inclination was 9° and 20°, respectively, with the plate position of Soong grade 1. The lengths of the distal screws were approximately two-thirds distance from the volar to dorsal surface.
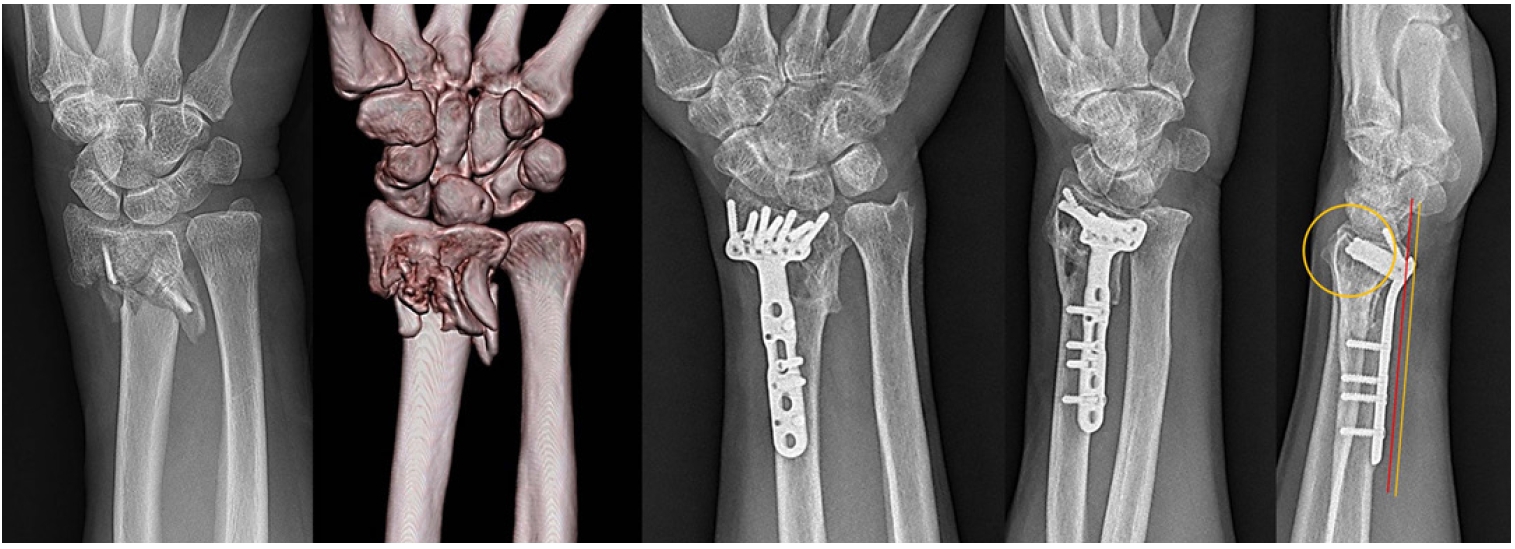
Fig. 4.Cortical defects identified in three patients. Mechanical support from long volar locking plates ensured volar cortex stability.
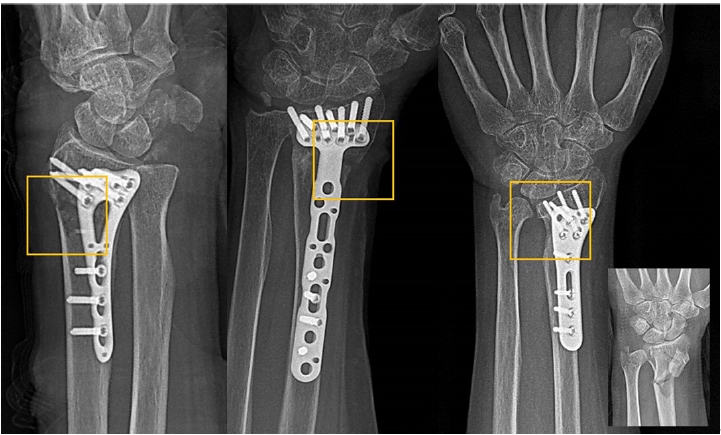
Fig. 5.With the exception of ulnar styloid fractures, satisfactory union at the final follow-up was observed for other types of concurrent ulnar fractures.
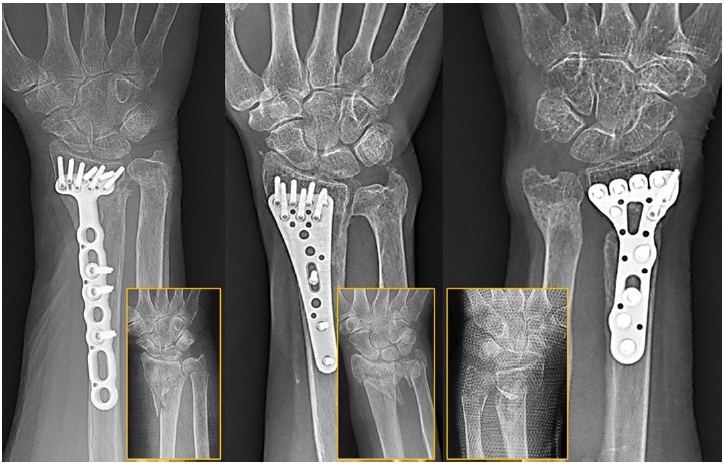
Table 1.Basic demographic, radiological and clinical data
|
Variable |
Value |
|
Age (yr) |
77.3±4.9 |
|
Sex (male:female) |
11:20 |
|
Smoking (yes:no) |
7:24 |
|
Comorbidity (yes:no) |
16:15 |
|
Bone mineral density |
–2.60±0.46 |
|
AO classification (A3.3:C2.2:C2.3:C3.3) |
10:6:9:6 |
|
Area of eliminated fragment (cm2) |
3.30±0.68 |
|
Ratio of largest diameter of eliminated fragment |
0.40±0.15 |
|
Ulnar fracture pattern (Q1:Q2:Q3:Q4:Q5:Q6) |
0:8:7:11:2:3 |
|
Volar tilt at just after surgery (°) |
10.52±1.06 |
|
Radial inclination just after surgery (°) |
20.29±0.82 |
|
Articular step-off just after surgery (mm) |
0.48±0.51 |
|
Ulnar variances just after surgery (mm) |
0.55±0.77 |
|
Follow-up period (mo), median (range) |
26.16±1.97 (24–32) |
|
Volar tilt at final follow-up (°) |
10.35±1.11 |
|
Radial inclination at final follow-up (°) |
20.00±0.97 |
|
Articular step-off at final follow-up (mm) |
0.58±0.62 |
|
Ulnar variances at final follow-up (mm) |
0.71±0.82 |
|
Visual analog scale |
0.23±0.43 |
|
DASH score |
6.41±2.38 |
|
Flexion-extension arc (°) |
124.35±8.34 |
|
Pronation-supination arc (°) |
133.23±8.22 |
Table 2.Correlations between the clinical factors and radiologic outcomes
|
Difference between at final and just after surgery |
Bone mineral density
|
Area of eliminated cortical fragment
|
Ratio of diameter
|
|
r |
P-value |
r |
P-value |
r |
P-value |
|
Volar tilt |
–0.06 |
0.73 |
–0.03 |
0.88 |
0.07 |
0.70 |
|
Radial inclination |
–0.43 |
0.11 |
–0.17 |
0.36 |
0.02 |
0.89 |
|
Articular step-off |
0.24 |
0.19 |
0.03 |
0.86 |
0.14 |
0.45 |
|
Ulnar variances |
–0.06 |
0.77 |
–0.13 |
0.47 |
0.10 |
0.59 |
Table 3.Differences of the union degree according to the area of eliminated cortical fragment
|
Area of eliminated cortical fragment |
Union at postoperative (partial:full)
|
χ2
|
P-value |
|
3 mo |
6 mo |
|
<3.30±0.68 cm2
|
2:10 |
0:12 |
0.63 |
0.507 |
|
>3.30±0.68 cm2
|
2:17 |
0:19 |
Table 4.Clinical outcomes according to the AO classification
|
Variable |
AO classification |
No. |
Mean±SD |
P-value |
|
Visual analog scale |
A3.3 |
10 |
0.20±0.42 |
0.92 |
|
C2.2 |
6 |
0.17±0.41 |
|
C2.3 |
9 |
0.22±0.44 |
|
C3.3 |
6 |
0.33±0.52 |
|
DASH score |
A3.3 |
10 |
6.76±2.62 |
0.20 |
|
C2.2 |
6 |
4.72±1.21 |
|
C2.3 |
9 |
6.38±2.30 |
|
C3.3 |
6 |
7.57±2.51 |
|
Flexion-extension arc (°) |
A3.3 |
10 |
128.00±7.89 |
0.38 |
|
C2.2 |
6 |
120.83±6.65 |
|
C2.3 |
9 |
123.33±9.68 |
|
C3.3 |
6 |
123.33±8.16 |
|
Pronation-supination arc (°) |
A3.3 |
10 |
133.00±9.49 |
0.63 |
|
C2.2 |
6 |
135.00±8.37 |
|
C2.3 |
9 |
130.56±8.08 |
|
C3.3 |
6 |
135.83±6.65 |
Table 5.Clinical outcomes according to the ulnar fracture type
|
Variable |
Ulnar fracture |
No. |
Mean±SD |
P-value |
|
Visual analog scale |
Q1 |
8 |
0.12±0.35 |
0.49 |
|
Q2 |
7 |
0.43±0.53 |
|
Q3 |
11 |
0.27±0.47 |
|
Q4 |
2 |
0.00±0.00 |
|
Q5 |
3 |
0.00±0.00 |
|
DASH score |
Q1 |
8 |
5.48±1.73 |
0.14 |
|
Q2 |
7 |
8.08±2.35 |
|
Q3 |
11 |
6.68±2.58 |
|
Q4 |
2 |
5.58±3.08 |
|
Q5 |
3 |
4.59±0.50 |
|
Flexion-extension arc (°) |
Q1 |
8 |
120.62±10.84 |
0.08 |
|
Q2 |
7 |
126.43±6.27 |
|
Q3 |
11 |
127.27±6.47 |
|
Q4 |
2 |
130.00±0.00 |
|
Q5 |
3 |
115.00±5.00 |
|
Pronation-supination arc (°)a)
|
Q1 |
8 |
138.75±3.54 |
<0.001 |
|
Q2 |
7 |
134.29±5.35 |
|
Q3 |
11 |
135.00±5.92 |
|
Q4 |
2 |
117.50±10.61 |
|
Q5 |
3 |
120.00±0.00 |
References
- 1. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am 2001;26:908-15.ArticlePubMed
- 2. Lee SK, Seo DW, Kim KJ, Yang DS, Choy WS. Volar long locking compression plate fixation for distal radius fractures with metaphyseal and diaphyseal extension. Eur J Orthop Surg Traumatol 2013;23:407-15.ArticlePubMedPDF
- 3. Wei XM, Sun ZZ, Rui YJ, Song XJ, Jiang WM. Minimally invasive percutaneous plate osteosynthesis for distal radius fractures with long-segment metadiaphyseal comminution. Orthop Traumatol Surg Res 2016;102:333-8.ArticlePubMed
- 4. Perren SM, Fernandez Dell'oca A, Regazzoni P. Evolution of AO fracture treatment part 1: the internal fixator. Acta Chir Orthop Traumatol Cech 2017;84:413-7.ArticlePubMed
- 5. Padegimas EM, Zmistowski B, Lawrence C, Palmquist A, Nicholson TA, Namdari S. Defining optimal calcar screw positioning in proximal humerus fracture fixation. J Shoulder Elbow Surg 2017;26:1931-7.ArticlePubMed
- 6. Hammer A. The calcar femorale: a new perspective. J Orthop Surg (Hong Kong) 2019;27:2309499019848778.ArticlePubMedPDF
- 7. Müller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. Springer, 1990.
- 8. Schemitsch EH, Richards RR. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am 1992;74:1068-78.ArticlePubMed
- 9. Oh BH, Heo YM, Yi JW, Kim TG, Lee JS. Atypical fracture of the proximal shaft of the ulna associated with prolonged bisphosphonate therapy. Clin Orthop Surg 2018;10:389-92.ArticlePubMedPMCPDF
- 10. Cha SM, Shin HD. Risk factors for atypical forearm fractures associated with bisphosphonate usage. Injury 2021;52:1423-8.ArticlePubMed
- 11. Tang JB, Giddins G. Why and how to report surgeons’ levels of expertise. J Hand Surg Eur Vol 2016;41:365-6.ArticlePubMedPDF
- 12. Fernandez DL, Jupiter JB. Functional and radiographic anatomy. In: Fernandez DL, Jupiter JB, eds. Fractures of the distal radius: a practical approach to management. 1st ed. Springer US; 1995. p. 53-69.
- 13. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979;86:420-8.ArticlePubMed
- 14. Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas 1973;33:613-9.ArticlePDF
- 15. Cha SM, Shin HD, Kim YK. Comparison of low-profile locking plate fixation versus antegrade intramedullary nailing for unstable metacarpal shaft fractures: a prospective comparative study. Injury 2019;50:2252-8.ArticlePubMed
- 16. Beaton DE, Davis AM, Hudak P, McConnell S. The DASH (Disabilities of the Arm, Shoulder and Hand) outcome measure: what do we know about it now? Br J Hand Ther 2001;6:109-18.ArticlePDF
- 17. Holzbauer M, Bodell LS, Froschauer SM. Wrist hemiarthroplasty for complex intraarticular distal radius fracture in a patient with manifest osteoporosis. Life (Basel) 2022;12:471.ArticlePubMedPMC
- 18. Herzberg G, Walch A, Burnier M. Wrist hemiarthroplasty for irreparable DRF in the elderly. Eur J Orthop Surg Traumatol 2018;28:1499-503.ArticlePubMedPDF
- 19. Lee JK, Lee Y, Kim C, Kim M, Han SH. A 10-year retrospective study. Arch Orthop Trauma Surg 2021;141:1711-9.ArticlePubMedPDF
- 20. Mudgal CS, Jupiter JB. Plate fixation of osteoporotic fractures of the distal radius. J Orthop Trauma 2008;22(8 Suppl):S106-15.ArticlePubMed
- 21. Richard MJ, Katolik LI, Hanel DP, Wartinbee DA, Ruch DS. Distraction plating for the treatment of highly comminuted distal radius fractures in elderly patients. J Hand Surg Am 2012;37:948-56.ArticlePubMed
- 22. Emmert AS, Swenson AK, Matar RN, Ross PR, Stern PJ. Characterization of major complications of bridge plating of distal radius fractures at a level I trauma center. Hand (N Y) 2024;Jun. 13. [Epub]. https://doi.org/10.1177/15589447241257964. Article
- 23. Hevonkorpi TP, Launonen AP, Huttunen TT, Kannus P, Niemi S, Mattila VM. Incidence of distal radius fracture surgery in Finns aged 50 years or more between 1998 and 2016: too many patients are yet operated on? BMC Musculoskelet Disord 2018;19:70.ArticlePubMedPMCPDF
- 24. Gyuricza C, Carlson MG, Weiland AJ, Wolfe SW, Hotchkiss RN, Daluiski A. Removal of locked volar plates after distal radius fractures. J Hand Surg Am 2011;36:982-5.ArticlePubMed
- 25. Tan A, Chong A. Reasons for implant removal after distal radius fractures. J Hand Surg Asian Pac Vol 2016;21:321-5.ArticlePubMed
- 26. Soong M, Earp BE, Bishop G, Leung A, Blazar P. Volar locking plate implant prominence and flexor tendon rupture. J Bone Joint Surg Am 2011;93:328-35.ArticlePubMed
- 27. Lee DY, Park YJ, Park JS. A meta-analysis of studies of volar locking plate fixation of distal radius fractures: conventional versus minimally invasive plate osteosynthesis. Clin Orthop Surg 2019;11:208-19.ArticlePubMedPMCPDF
- 28. Jakubietz MG, Gruenert JG, Jakubietz RG. The use of beta-tricalcium phosphate bone graft substitute in dorsally plated, comminuted distal radius fractures. J Orthop Surg Res 2011;6:24.ArticlePubMedPMC
- 29. Hartigan BJ, Cohen MS. Use of bone graft substitutes and bioactive materials in treatment of distal radius fractures. Hand Clin 2005;21:449-54.ArticlePubMed
- 30. Ladd AL, Pliam NB. The role of bone graft and alternatives in unstable distal radius fracture treatment. Orthop Clin North Am 2001;32:337-51.ArticlePubMed
- 31. Kim JK, Yun YH, Kim DJ, Yun GU. Comparison of united and nonunited fractures of the ulnar styloid following volar-plate fixation of distal radius fractures. Injury 2011;42:371-5.ArticlePubMed
- 32. Sawada H, Shinohara T, Natsume T, Hirata H. Clinical effects of internal fixation for ulnar styloid fractures associated with distal radius fractures: a matched case-control study. J Orthop Sci 2016;21:745-8.ArticlePubMed
- 33. Cha SM, Shin HD, Kim KC, Park E. Treatment of unstable distal ulna fractures associated with distal radius fractures in patients 65 years and older. J Hand Surg Am 2012;37:2481-7.ArticlePubMed
- 34. Kim JK, Kim JO, Koh YD. Management of distal ulnar fracture combined with distal radius fracture. J Hand Surg Asian Pac Vol 2016;21:155-60.ArticlePubMed






 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

