Search
- Page Path
- HOME > Search
Review Article
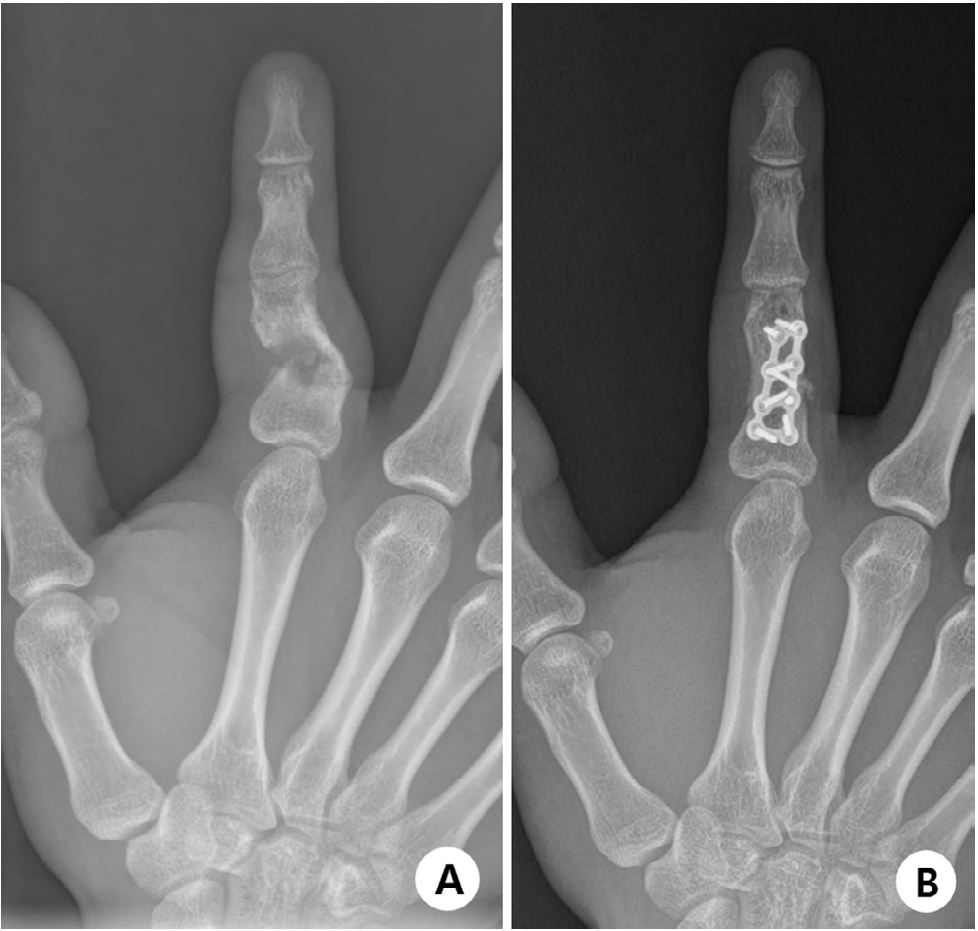
- Complications of hand fractures: strategies for prevention and management
- Jong Woo Kang
- J Musculoskelet Trauma 2026;39(1):1-11. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00304
-
 Abstract
Abstract
 PDF
PDF - Various complications can occur after hand fractures. Among them, joint stiffness and malunion are the most common and significant complications, which are often accompanied by tendon adhesions and joint contracture. Careful evaluations of injury characteristics, such as fracture patterns, alignment, and soft tissue injury, are the first step to select appropriate management strategies and prevent complications of hand fractures. Close observation of its clinical prognosis is also essential for early detection and preemptive management of complications. Management of complications includes immobilization, rehabilitation, and various surgical techniques such as tenolysis or capsular release for joint stiffness, corrective osteotomy for malunion, and revisional fixation with bone graft for nonunion. The authors discuss prevention, early recognition, and management strategies for complications of hand fractures in this review.
- 208 View
- 9 Download

Original Articles
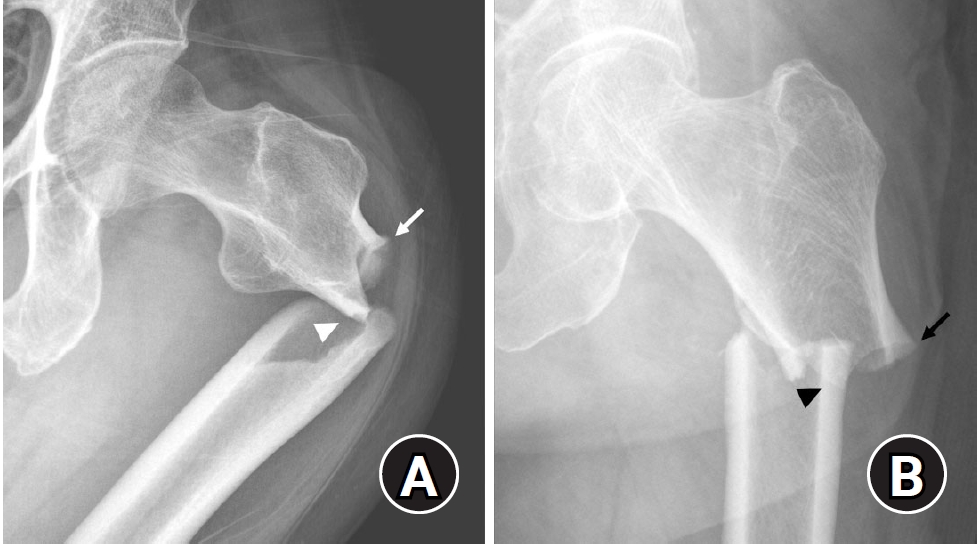
- Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
- Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
- J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00157
-
 Abstract
Abstract
 PDF
PDF - Background
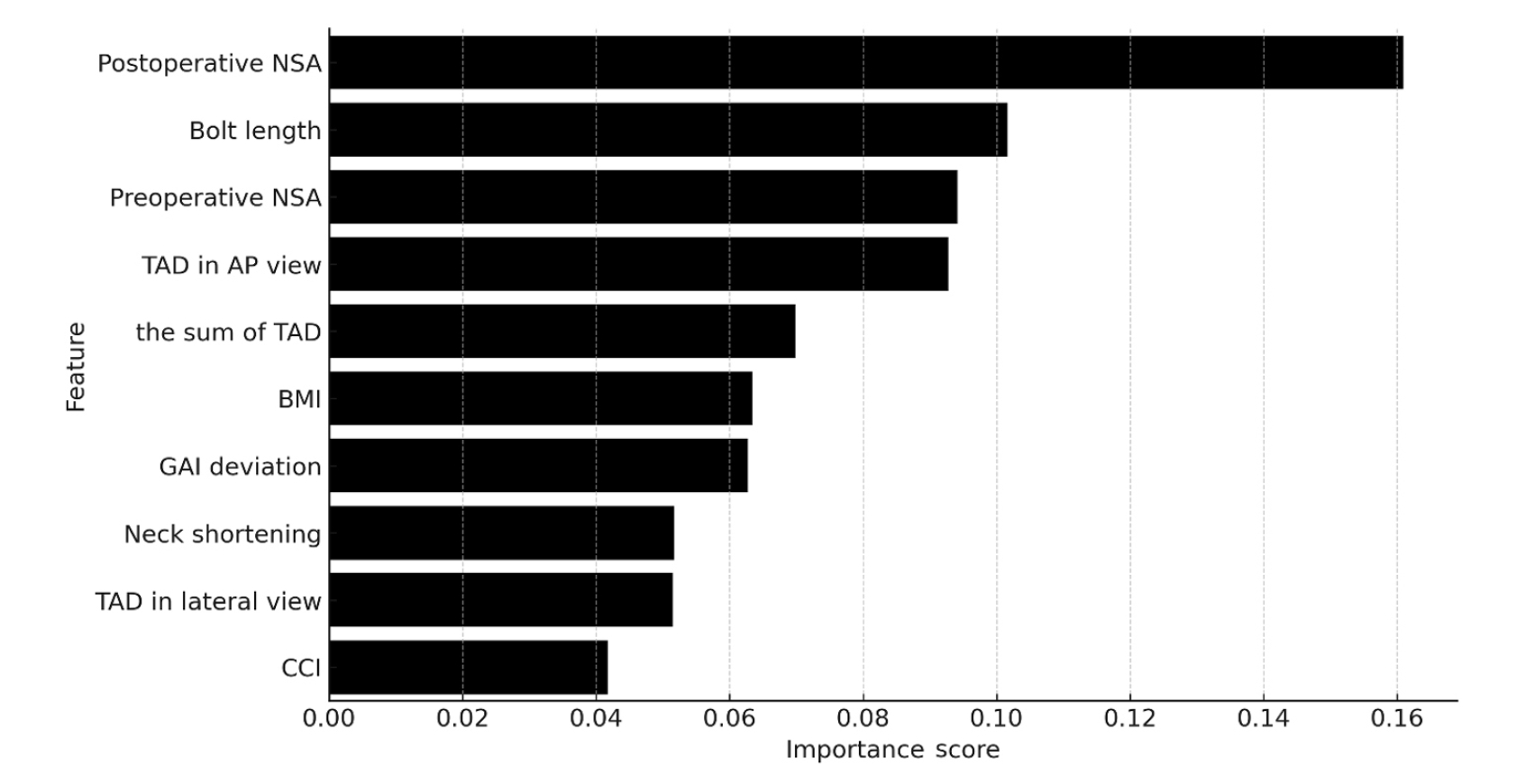
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery. Level of Evidence: III. -
Citations
Citations to this article as recorded by- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
Seonghyun Kang, Wonseok Choi, Jeong Seok Choi, Eic Ju Lim, SungJin Ahn, Jong-Keon Oh, William T. Kent, Whee Sung Son, Jae-Woo Cho
Journal of Orthopaedic Surgery.2026;[Epub] CrossRef
- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
- 1,191 View
- 43 Download
- 1 Crossref

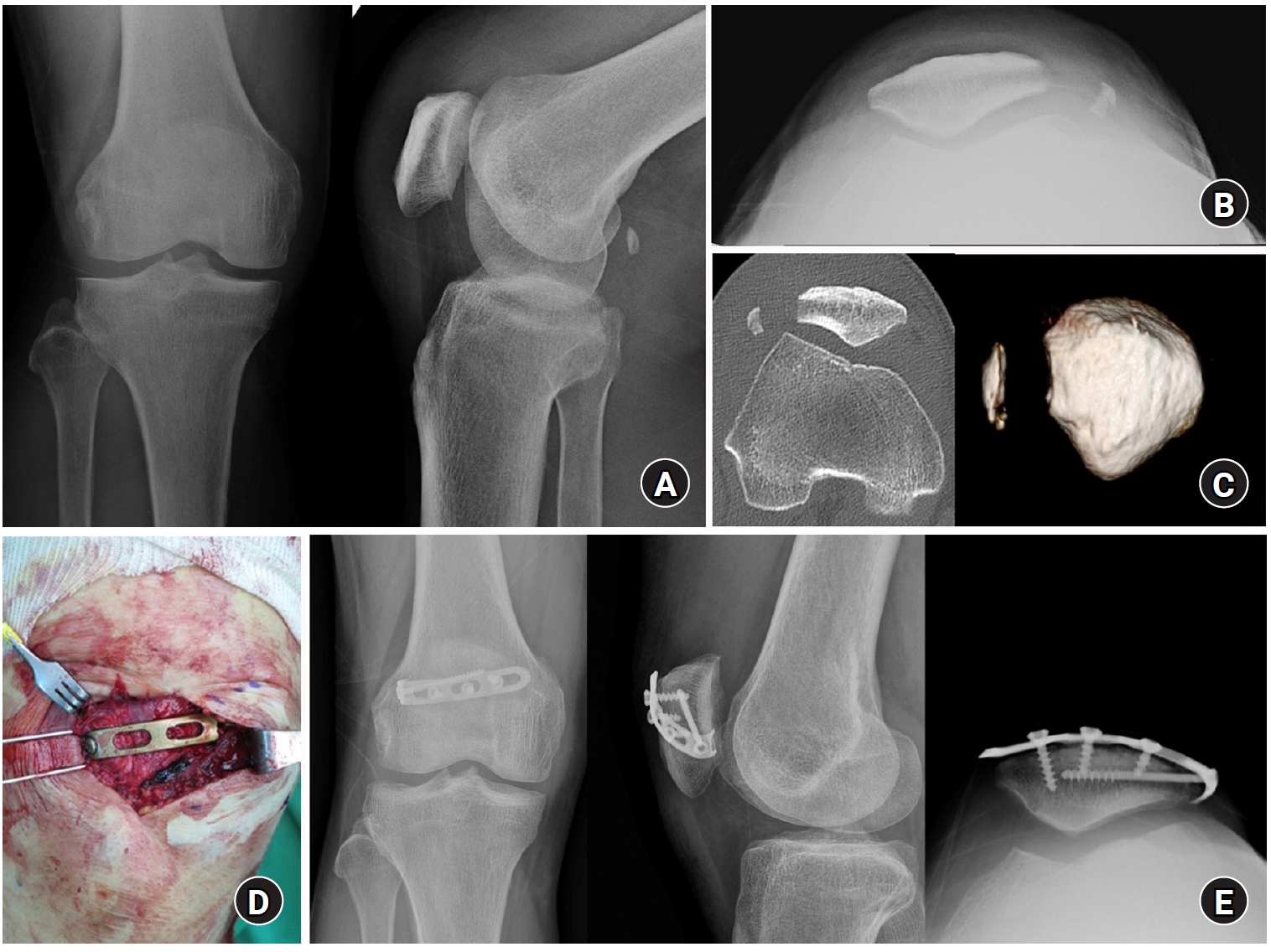
- Lateral marginal fractures of the patella and patellofemoral pain
- Jae-Ang Sim, Chul-Ho Kim, Ji Wan Kim
- J Musculoskelet Trauma 2025;38(3):152-159. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00171
-
 Abstract
Abstract
 PDF
PDF - Background
This study investigated the characteristics of lateral marginal fractures of the patella and evaluated the clinical outcomes.
Methods
We retrospectively reviewed all patients with lateral marginal fractures of the patella, defined as a vertical fracture line within 15 mm of the lateral patellar border, from 2008 to 2020. In total, 41 patients were included. Patient characteristics, radiologic findings, and clinical outcomes, including the Lysholm score at 1 year postoperation, were evaluated.
Results
The injury mechanisms were direct in 34 cases and indirect in seven. Furthermore, 85% of patients had a skyline view of the patella at the initial visit, and one medial subluxation of the patella was found. Forty of the 41 patients underwent surgery. Anatomical and nonanatomical (>1-mm displacement or excision) reductions were carried out in 36 cases (88%) and five cases (12%), respectively. The average Lysholm score was 89.1 (range, 67–99). The nonanatomical reduction group had a poorer functional score (79.8 vs. 90.4; P=0.010). Lateral patellar compression syndrome occurred in two patients with nonanatomical reduction.
Conclusions
Lateral marginal fractures of the patella affected patellofemoral stability. Anatomical reduction showed good functional outcomes, while nonanatomical reduction was associated with patellofemoral stability and pain. Therefore, surgeons should perform anatomical reduction with any appropriate fixation method. Level of Evidence: IV
- 1,259 View
- 26 Download

Review Article
- Atypical femoral fractures: an update
- Won-Tae Cho, Jeong-Hyun Koh, Seungyeob Sakong, Jung-Taek Kim
- J Musculoskelet Trauma 2025;38(2):41-52. Published online March 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00031
-
 Abstract
Abstract
 PDF
PDF - This narrative review provides an up-to-date overview of atypical femoral fractures (AFFs), emphasizing diagnostic criteria, epidemiology, pathophysiology, risk factors, and evaluation with screening strategies. AFFs are rare but significant complications associated with prolonged bisphosphonate (BP) therapy for osteoporosis. Although the pathogenesis of AFFs has not been fully elucidated, its primary mechanism is thought to involve impaired bone remodeling, leading to unhealed microfractures that progress to stress fractures under repetitive loading. AFFs can occur in various regions of the femur, influenced by femoral geometry and the lower limb axis. Other risk factors include prolonged steroid use, arthroplasty, genetic predispositions, and metabolic bone disorders. The diagnosis of AFFs is based on criteria established by the American Society for Bone and Mineral Research. Key radiographic features include lateral cortical transverse fracture lines and localized cortical thickening, typically with minimal or no comminution on the medial cortex. Dual-energy X-ray absorptiometry for screening tests and magnetic resonance imaging as an advanced imaging modality enable the early detection of incomplete fractures. This multi-modal approach facilitates the prompt identification of prodromal cortical changes, reducing the risk of complete fractures in high-risk populations, particularly patients undergoing prolonged BP therapy. Level of Evidence: V
-
Citations
Citations to this article as recorded by- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
Lorenzo Lucchetta, Carmelinda Ruggiero, Samuele Berardi, Alice Franceschi, Michele Bisaccia, Giuseppe Rinonapoli
Journal of Clinical Medicine.2025; 15(1): 25. CrossRef
- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
- 14,592 View
- 399 Download
- 1 Crossref

Original Articles
- Does the Operator’s Experience Affect the Occurrence of Complications after Distal Radius Fracture Volar Locking Plate Fixation? A Comparative Study of the First Four Years and Thereafter
- Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
- J Musculoskelet Trauma 2024;37(4):175-183. Published online October 25, 2024
- DOI: https://doi.org/10.12671/jmt.2024.37.4.175
- Correction in: J Musculoskelet Trauma 2025;38(1):40
-
 Abstract
Abstract
 PDF
PDF - Purpose
The management of distal radius fractures (DRFs) has evolved with the introduction of volar locking plate (VLP) fixation, offering stable fixation and better outcomes. Nevertheless, the impact of the surgeon’s experience on the complication rates in VLP fixation remains to be determined, particularly for less-experienced surgeons. This study compared the complication rates during the initial four years and subsequent two years of a hand surgeon’s practice of VLP fixation for DRFs.
Materials and Methods
The data between March 2016 and December 2022 were analyzed retrospectively under the Institutional Review Board approval. A single surgeon performed all VLP fixation surgeries after finishing regular hand surgery training, with the first four years representing the less experienced phase (Group 1) and the following two years indicating the experienced phase (Group 2). The patients’ characteristics, operation-related factors, and postoperative complications, including tendon injuries, nerve-related complications, fixation and instrument-related issues, osteosynthesis-related problems, and infections, were compared. In addition, the authors compared the data with a large multicenter study conducted by experienced hand surgeons.
Results
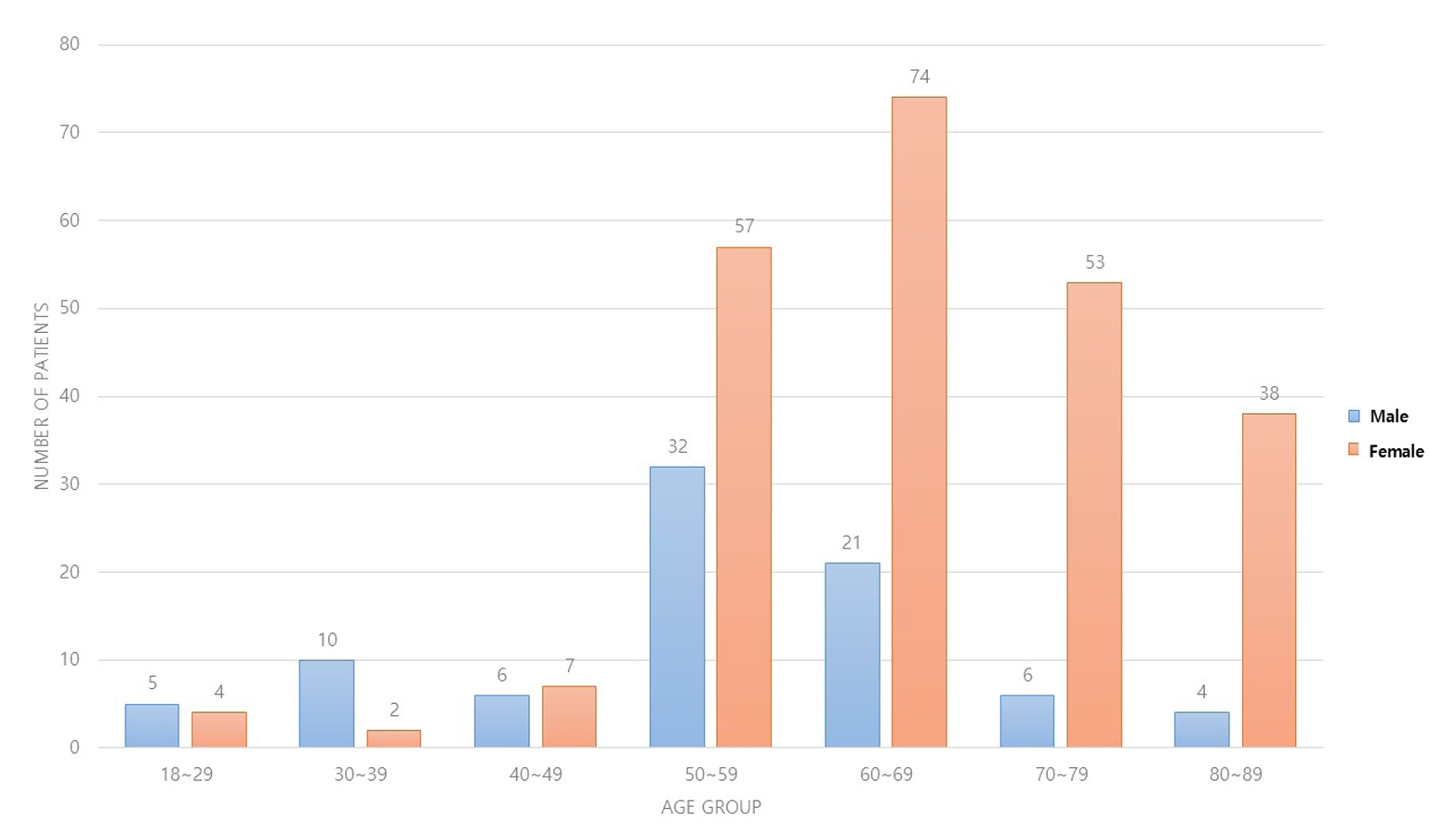
Three hundred and nineteen patients (321 wrists) were included. The mean age was 63.3 years, and 26.3% were male and 73.7% were female. The operation time was 53.7±14.5 minutes and 74.4±26.5 minutes in groups 1 and 2, respectively, which was statistically significantly shorter (p<0.001). The complication rates between the two groups were similar, except for the higher implant removal rates in Group 1. A comparison with a previous multicenter study revealed higher reduction losses and carpal tunnel syndrome in this study, but the overall complication rate was low.
Conclusion
In DRF management, when the operating surgeon has completed an accredited training course, VLP fixation is a good treatment method that can be performed effectively even by less experienced surgeons with low complication rates. -
Citations
Citations to this article as recorded by- Epidemiological changes and surgical trends of distal radius fractures in adults over 50 years during the COVID-19 pandemic in Korea: a nationwide repeated cross-sectional study
Han-Kook Yoon, So Ra Yoon, Kee-Bum Hong, Youngsu Jung, SeongJu Choi, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2026; 39(1): 12. CrossRef - Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2025; 38(1): 40. CrossRef - Characteristics of patients with distal radius fracture requiring arthroscopic foveal repair after bone union
Min Jung Park, Cheungsoo Ha, Hyun Tak Kang, Yong Hyun Yoon, Jun-Ku Lee, Soo-Hong Han
Arthroscopy and Orthopedic Sports Medicine.2025; 12(2): 70. CrossRef
- Epidemiological changes and surgical trends of distal radius fractures in adults over 50 years during the COVID-19 pandemic in Korea: a nationwide repeated cross-sectional study
- 2,701 View
- 53 Download
- 3 Crossref

- Acute Compartment Syndrome of Thigh: Ten-Year Experiences from a Level I Trauma Center
- Hyung Keun Song, Won-Tae Cho, Wan-Sun Choi, Seung-Yeob Sakong, Sumin Im
- J Musculoskelet Trauma 2024;37(4):171-174. Published online October 25, 2024
- DOI: https://doi.org/10.12671/jmt.2024.37.4.171
-
 Abstract
Abstract
 PDF
PDF - Purpose
To assess the demographics, injury mechanisms, treatments, and outcomes of traumatic acute compartment syndrome in the thigh.
Materials and Methods
Patients diagnosed with thigh compartment syndrome were analyzed retrospectively at the authors’ level I trauma center from March 2012 to February 2022. Data were collected from medical and radiological records, focusing on demographics, injury details, treatment timelines, and clinical outcomes.
Results
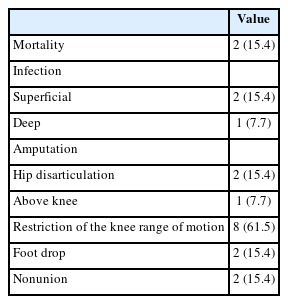
The cohort included 13 patients (11 males and 2 females) with a mean age of 46 years. Injuries primarily resulted from falls (6 patients) and vehicle accidents (5 patients). Fractures were noted in 11 patients, with seven involving the lower extremities and seven having open fractures; three of these were severe enough to be classified as Gustilo–Anderson type IIIc with associated femoral artery injuries. Time from the injury to fasciotomy ranged from within six hours to more than 24 hours. Fasciotomies were mainly single-sided (10 patients), targeting primarily the anterior compartments, and bilateral in three cases. Wound closures were performed using delayed primary closure (four patients) and partial- thickness skin grafts (five patients). Two patients died from multi-organ failure; other complications included infections (three patients), amputations (three patients), and long-term disabilities like drop foot (two patients), sensory deficits, joint stiffness (eight patients), and fracture non-unions requiring additional surgery (two patients).
Conclusion
Thigh-compartment syndrome, though infrequent, poses significant risks of mortality and chronic disability. This underscores the importance of prompt diagnosis and intervention.
- 1,846 View
- 52 Download

Review Articles
- Complications of Hand Fractures and Its Prevention
- Jong Woo Kang
- J Korean Fract Soc 2024;37(1):46-51. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.46
-
 Abstract
Abstract
 PDF
PDF - Complications of hand fractures occur regardless of the methods used for their treatment. The treatment is also challenging. The most common and troublesome complications of hand fractures are malunion, finger stiffness, and consequent functional impairment. Early recognition and meticulous treatment of these complications is essential for improvement in hand function and satisfaction. Most of all, surgeons should clearly understand that prevention of complications is the easiest way to ensure a satisfactory outcome in hand fractures.
- 671 View
- 19 Download

- Fracture-Related Complications: What You Can Do to Prevent Infection
- HoeJeong Chung, Jin Woo Lee, Sang-Ho Lee, Hoon-Sang Sohn
- J Korean Fract Soc 2023;36(4):139-147. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.139
-
 Abstract
Abstract
 PDF
PDF - Fracture-related infections (FRI) can occur when bacteria enter the wound during a traumatic injury. All efforts should be made to prevent FRI-associated complications due to the complexity of treatment at the time of onset and poor treatment outcomes. The risk factors for FRIs vary and several preoperative, perioperative, and postoperative measures can be implemented to prevent infections. Preoperative measures include blood sugar control, nutritional support, discontinuation of steroids and immunosuppressants, treatment of accompanying pre-existing infections, and decolonization of pathogens, specifically Staphylococcus aureus. The perioperative and postoperative measures include the use of prophylactic antibiotics, proper surgical site preparation (hair removal, preoperative washing, skin antisepsis), suitable surgical environment (operating room ventilation system, behavioral interventions in the operating room), correct surgical techniques (debridement, irrigation, wound closure, and negative pressure wound therapy). All medical staff should pay careful attention and ensure the implementation of the correct preventive measures.
- 779 View
- 26 Download

- Hip Fractures in the Elderly: Perioperative Management and Prevention of Medical Complications
- Keong-Hwan Kim
- J Korean Fract Soc 2023;36(1):39-44. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.39
-
 Abstract
Abstract
 PDF
PDF - Elderly patients with hip fractures are at an increased risk of developing medical complications with higher mortality rates. Most patients require surgical treatment, and an early surgical intervention can reduce complications and lower mortality risk. A restrictive red blood cell transfusion strategy is usually applied, and the amount of transfusion can be reduced through medications such as tranexamic acid. Delirium can be prevented using non-pharmacological methods. In addition, it is necessary to prevent venous thromboembolism through mechanical or chemical prophylaxis. A multidisciplinary approach using the ERAS (Enhanced Recovery After Surgery) protocol and orthogeriatric care can help to reduce medical complications and mortality.
-
Citations
Citations to this article as recorded by- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
Jee Young Lee, Gyu Min Kong
Journal of Orthopaedic Trauma.2025; 39(7): 352. CrossRef - Comparison of Operation Time, Vital Signs, Bleeding Tendency, and Recovery Time Based on Anesthesia Methods in Patients Undergoing Hip Fracture Surgery
Je Bog Yoo, Woo Young In, Chang Ok Pyo, Jeung Hee Kwon, Min Ji Lee, Kwang Hee Kim, Kyoung Ok Kim, Mi Yu
Journal of PeriAnesthesia Nursing.2025;[Epub] CrossRef
- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
- 1,391 View
- 40 Download
- 2 Crossref

- Current Management of Talar Fractures
- Gun-Woo Lee, Keun-Bae Lee
- J Korean Fract Soc 2022;35(1):31-37. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.31
-
 Abstract
Abstract
 PDF
PDF - Talar fracture management is one of the most challenging tasks for orthopedic surgeons. High complication rates and functional impairments after talar fractures have been well documented, and thus, surgical strategies capable of perfect anatomic reduction and stable fixation are important. The current review was undertaken to provide recommendations regarding updated surgical strategies that include surgical timing, approach, fixation methods, and the prevention and treatment of possible complications.
- 582 View
- 6 Download

- Ankle Fractures in Children: Classification and Treatment
- Ha-Yong Kim, Yong-Han Cha, Woo-Suk Kim, Won-Sik Choy
- J Korean Fract Soc 2021;34(2):87-95. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.87
-
 Abstract
Abstract
 PDF
PDF - Pediatric ankle fractures are defined as damage to the metaphysis, epiphyseal plate, and epiphysis of the distal tibia and fibula. Although the injury mechanism could be similar, the fracture patterns and treatment of pediatric ankle fractures are different from those of adults. In children, growth plate injuries are more common with a force that would cause sprains in adults because the ligaments are stronger than the growth plate cartilage in children. In the adolescent period, unique fractures, called “transitional fractures”, occur while the physis is closed. For a diagnosis, plain images of the anteroposterior, lateral, and mortise views are essential. Stress radiographs, ultrasound, and magnetic resonance imaging can be used for suspected ligament injuries. The treatment goal is to restore the articular congruity, normal bony alignment, and preserve the epiphyseal plate to ensure normal growth. Pediatric ankle fractures frequently lead to premature physeal arrest, angular deformities, malunion, and posttraumatic arthritis even after anatomic reduction. Treating surgeons should follow-up children for a sufficient time and explain to the caregiver the possible complications before treatment.
- 1,691 View
- 39 Download

- Fixation Options of Unstable Posterior Pelvic Ring Disruption: Ilio-Sacral Screw Fixation, S2AI Fixation, Posterior Tension Band Plate Fixation, and Spino-Pelvic Fixation
- Dong Hee Kim, Jae Hoon Jang, Myungji Shin, Gu Hee Jung
- J Korean Fract Soc 2019;32(4):240-247. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.240
-
 Abstract
Abstract
 PDF
PDF - The fixation methods that can be used for unstable posterior pelvic ring injuries have undergone many innovative changes due to the recent development of surgical and imaging techniques. After understanding the appropriate indications of first and second sacroiliac screw fixation and spinopelvic fixation, innovative methods, including the trans-sacral screw fixation, posterior tension-band plate fixation, and the S2AI screw, would be chosen and applied. Considering the anatomical complexity and proximity to the surrounding vessels and nerves in the posterior fixation, the safe zone according to the fixation options should be well understood in preoperative planning. Moreover, the functional reduction of the posterior pelvic ring through the reduction and fixation of the anterior lesion should be achieved before placing the implant to reduce the number of malposition-related complications.
-
Citations
Citations to this article as recorded by- Clinical Research through Computational Anatomy and Virtual Fixation
Ju Yeong Kim, Dong-Geun Kang, Gu-Hee Jung
Journal of the Korean Orthopaedic Association.2023; 58(4): 299. CrossRef
- Clinical Research through Computational Anatomy and Virtual Fixation
- 1,035 View
- 13 Download
- 1 Crossref

- Locked Plating in Elderly Patients with Distal Femur Fracture: How to Avoid Complications?
- Chul Young Jang, Je Hyun Yoo
- J Korean Fract Soc 2019;32(2):112-119. Published online April 30, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.2.112
-
 Abstract
Abstract
 PDF
PDF - Distal femur fractures in elderly patients with osteoporosis are complicated because poor bone quality makes screw purchase and fixation less secure, presenting many clinical challenges to the orthopedic surgeon. Minimally invasive locked plating using an angularly stable locking compression plate has become an integral tool for achieving secure fixation in osteoporotic distal femur fractures with improved biomechanical performance. On the other hand, complications, such as implant failure and periplate fracture, have still occurred. This paper describes the principles of internal fixation in minimally invasive lateral locked plating in elderly patients with osteoporotic distal femur fractures as well as how to avoid complications.
- 922 View
- 13 Download

Case Report
- Bilateral Gluteal Necrosis and Deep Infection after Transarterial Embolization for Pelvic Ring Injury in Patient with Hemodynamic Instability: A Case Report
- Sung Jin Park, Chang Ho Jeon, Nam Hoon Moon, Yong Geon Park, Jae Hoon Jang
- J Korean Fract Soc 2019;32(1):56-60. Published online January 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.1.56
-
 Abstract
Abstract
 PDF
PDF - Transarterial embolization is accepted as effective and safe for the acute management in hemodynamically unstable patients with pelvic ring injury. However, transarterial embolization has potential complications, such as gluteal muscle/skin necrosis, deep infection, surgical wound breakdown, and internal organ infarction, which are caused by blocked blood flow to surrounding tissues and organs, and many studies on the complications have been reported. Here, we report an experience of the management of gluteal necrosis and infection that occurred after transarterial embolization, with a review of the relevant literature.
- 814 View
- 0 Download

Review Articles
- Pelvis/Acetabular Fractures in the Elderly: When and How to Fix?
- Kyeong Hyeon Park, Chang Wug Oh, Joon Woo Kim
- J Korean Fract Soc 2018;31(3):102-113. Published online July 31, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.3.102
-
 Abstract
Abstract
 PDF
PDF - Owing to the increase in life expectancy, the incidence of osteoporotic fracture of the pelvis and acetabulum is increasing. Fractures in the elderly population is different from those in younger patients. Pelvic ring and acetabular fractures in geriatric patients are more likely the result of low-energy trauma, but the outcomes are generally poorer than those of the younger population. Multiple management options are available, but no intervention has become the standard of care for these fractures in the elderly. A treatment strategy should be established depending on the state of the individual patient. Regardless of whether nonsurgical or surgical treatment is selected, early ambulation should be considered to avoid the complications associated with prolonged immobilization.
-
Citations
Citations to this article as recorded by- Effect of Korean Medicine Treatments for Pain Reduction in Patients with Hip Fracture : A Retrospective Observational Study
Nam Hoon Kim, Min Seok Oh
Journal of Physiology & Pathology in Korean Medicine.2020; 34(5): 263. CrossRef
- Effect of Korean Medicine Treatments for Pain Reduction in Patients with Hip Fracture : A Retrospective Observational Study
- 513 View
- 6 Download
- 1 Crossref

- Hand Fractures
- Seokwon Yang, Jong Pil Kim
- J Korean Fract Soc 2018;31(2):61-70. Published online April 30, 2018
- DOI: https://doi.org/10.12671/jkfs.2018.31.2.61
-
 Abstract
Abstract
 PDF
PDF - Hand fractures are the second most common fracture in the upper extremities after the distal radius, and patients with these injuries may be experienced in hand surgery clinics. On the other hand, during the treatment of hand fractures, complications can occur due to complex functions of the hand and small-sized injuries to the bone and soft tissues. This review focused on the principles of management of these fractures, including injury mechanism, evaluations and recent treatment options. Minimally invasive surgery in various types of hand fractures, including the phalanx and metacarpal bone, is preferred because early mobilization after surgery has been emphasized to reduce complications, such as stiffness.
-
Citations
Citations to this article as recorded by- A novel finger brace for preventing finger stiffness after trauma or surgery: a preliminary report with a case series
Dae-Geun Kim, Hyo Jun Park
Archives of Hand and Microsurgery.2023; 28(4): 239. CrossRef
- A novel finger brace for preventing finger stiffness after trauma or surgery: a preliminary report with a case series
- 584 View
- 2 Download
- 1 Crossref

- Fracture of the Talus
- Tae Jung Bang, Sun Kyu Kim, Hyung Jin Chung
- J Korean Fract Soc 2016;29(3):213-220. Published online July 31, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.3.213
-
 Abstract
Abstract
 PDF
PDF - Although talus fractures are uncommon, proper management is important because they are often associated with severe complications. Talar neck and body fractures occupy most of the talar fractures. It remains controversial whether talar neck fractures require emergent or elective treatment. Elective definitive fixation, however, may reduce risks of wound complications. Many surgeons recommend dual surgical approaches—anteromedial and anterolateral—to allow accurate visualization and anatomic reduction. Although there are various methods of fixation, the use of plates is necessary in comminuted talar fractures. Outcomes may vary and will be dependent on the degree of the initial fracture displacement. It is necessary to restore articular congruency and axial alignment for normalizing hindfoot function. Common complications include posttraumatic arthritis, avascular necrosis, malunion, and nonunion.
- 973 View
- 18 Download

- Current Concepts of Fractures and Dislocation of the Hand
- Yong Cheol Yoon, Jong Ryoon Baek
- J Korean Fract Soc 2016;29(2):143-159. Published online April 30, 2016
- DOI: https://doi.org/10.12671/jkfs.2016.29.2.143
-
 Abstract
Abstract
 PDF
PDF - Fractures and dislocation of the hand is a body injury involving complex structures and multiple functions, which frequently occur as they represent 10%-30% of all fractures. Such fractures and dislocation of the hand should be treated in the context of stability and flexibility; and tailored treatment is required in order to achieve the most optimal functional performance in each patient since deformation may occur if not treated, stiffness may occur with unnecessarily excessive treatment, and both deformation and stiffness may occur coincidently with inappropriate treatment. Stable injuries can be fixed with splintage whereas surgery is actively considered for unstable injuries. In addition, surgeons should keep in mind that as the surgical intervention is done aggressively, aggressive rehabilitation must be followed in correspondence with the surgical intervention. Successful outcome requires effort to prevent any potential complication including nerve hypersensitivity and infection. Finally, it is also important that the patient to know that swelling, stiffness, and pain may last for a long period of time until the recovery of fractures and dislocation of the hand.
-
Citations
Citations to this article as recorded by- Current concepts in the management of phalangeal fractures in the hand
Hyun Tak Kang, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2025; 38(3): 109. CrossRef - Current Concepts in Management of Phalangeal Fractures
Yohan Lee, Sunghun Park, Jun-Ku Lee
Journal of the Korean Fracture Society.2022; 35(4): 169. CrossRef
- Current concepts in the management of phalangeal fractures in the hand
- 1,147 View
- 18 Download
- 2 Crossref

Original Article
- Clinical Outcomes of Fasciotomy for Acute Compartment Syndrome
- Ji Yong Park, Young Chang Kim, Ji Wan Kim
- J Korean Fract Soc 2015;28(4):223-229. Published online October 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.4.223
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study is to evaluate clinical outcomes and complications after fasciotomy in acute compartment syndrome.
MATERIALS AND METHODS
Seventeen cases diagnosed as compartment syndrome and underwent fasciotomy from January 2011 to February 2015 were evaluated retrospectively. We investigated the causes and regions of acute compartment syndrome, the methods of wound management, the necessity of skin graft, and the complications including amputation and infection.
RESULTS
According to the causes of acute compartment syndrome, there were 7 fractures, 1 traumatic hematoma, 6 reperfusion injury, and 3 rhabdomyolysis. The regions of acute compartment syndrome were 3 cases of thigh, 10 cases of leg, and 3 cases of foot. One case had acute compartment syndrome involving thigh, leg, and foot. Of 17 cases, 3 cases died due to reperfusion injury and one case with severe necrosis of soft tissues underwent amputation. Among the 13 cases excluding 4 cases with death or amputation, 3 cases underwent split thickness skin graft. Shoelace technique and/or vacuum-assisted closure (VAC) was used for 9 cases, and wound closure without skin graft was achieved in all except one case, while 2 cases required skin graft among 4 cases without shoelace technique or VAC. There were 2 cases of infection.
CONCLUSION
Acute compartment syndrome caused by reperfusion injury had poor outcomes. Shoelace technique and/or VAC were useful for management of wound after fasciotomy.
- 587 View
- 5 Download

Case Report
- Acute Rupture of Subclavian Artery Pseudoaneurysm after Delayed Osteosynthesis of Clavicular Fracture: A Case Report
- Oog Jin Shon, Jee Hoon Kim, Kang Hyun Park
- J Korean Fract Soc 2014;27(1):82-87. Published online January 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.1.82
-
 Abstract
Abstract
 PDF
PDF - Subclavian vessels are well protected by muscles, fascia and sheaths, so vascular complications associated with clavicular fractures are rare. Pseudoaneurysms after clavicular fractures have been reported, and the occurrence or rupture of pseudoaneurysm has been reported rarely as a late complication. However, cases of pseudoaneurysm after rupture of the clavicular fracture following delayed osteosynthesis of the clavicular fracture have not been reported. A 58-year-old female that presented with a right clavicular shaft fracture obtained conservative treatment. Surgery was performed after 4 months because of non-union in the local medical center. After operation, rupture of the subclavian pseudoaneurysm occurred following osteosynthesis of the clavicular shaft fracture. We report this case here with a review of the literature.
- 474 View
- 1 Download

Original Articles
- Neurologic Injury within Pelvic Ring Injuries
- Ji Wan Kim, Dong Hoon Baek, Jae Hyun Kim, Young Chang Kim
- J Korean Fract Soc 2014;27(1):17-22. Published online January 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.1.17
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the incidence of neurologic injury in pelvic ring injuries and to assess the risk factors for neurologic injury related to pelvic fractures.
MATERIALS AND METHODS
Sixty-two patients with the pelvic ring injury were enrolled in the study from March 2010 to May 2013. When the neurologic injury was suspected clinically, the electro-diagnostic tests were performed. Combined injuries, fracture types, and longitudinal displacements were examined for correlations with the neurologic injury.
RESULTS
There were 7 cases of AO/OTA type A, 37 cases of type B, and 18 cases of type C. Among them, 25 patients (40%) had combined spine fractures, and the average of longitudinal displacement was 7 mm (1-50 mm). Of the 62 patients, 13 (21%) had neurologic injury related with pelvic fractures; 5 with lumbosacral plexus injury, 5 with L5 or S1 nerve injury, 2 with obturator nerve injury, and 1 case of lateral femoral cutaneous nerve injury. There were no relationships between the neurologic injuries and fracture types (p=0.192), but the longitudinal displacements of posterior ring and combined spine fractures were related to the neurologic injury within pelvic ring injury (p=0.006, p=0.048).
CONCLUSION
The incidence of neurologic injury in pelvis fracture was 21%. In this study, the longitudinal displacements of posterior ring and combined spine fractures were risk factors for neurological injury in pelvic ring injury. -
Citations
Citations to this article as recorded by- Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
Kwang Hee Yeo, Nam Hoon Moon, Jae Min Ahn, Jae Yoon Jeong, Jae Hoon Jang
Journal of the Korean Fracture Society.2018; 31(1): 9. CrossRef
- Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
- 599 View
- 4 Download
- 1 Crossref

- Complications of Hook-Plate Fixation for Distal Clavicle Fractures
- Su Han An, Hyung Chun Kim, Kwang Yeol Kim, Ji Hoon Lee, Seung Hyun Yoon
- J Korean Fract Soc 2012;25(1):38-45. Published online January 31, 2012
- DOI: https://doi.org/10.12671/jkfs.2012.25.1.38
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To report on the complications of hook-plate fixation for distal clavicle fractures.
MATERIALS AND METHODS
Eighteen patients who underwent surgery for distal clavicle fracture with a hook-plate from April 2008 to April 2011 were enrolled with a minimum of 4 months follow-up. The reduction was qualified and evaluated according to the radiologic findings. We analyzed the results by UCLA score, Kona's functional evaluation, and VAS pain score.
RESULTS
By radiologic evaluation, 17 of 18 cases showed anatomical reduction and solid unions. Although satisfactory results were found in the clinical study as shown by the UCLA score, Kona's functional evaluation, and VAS pain score, complications arose in 7 cases, including osteolysis of the acromion in 2 cases, nonunion in 1 case, periprosthetic fracture in 2 cases, subacromial pain in 1 case, and skin irritation in 1 case. 2 cases of all required reoperation.
CONCLUSION
To reduce the complications of the hook-plate, a precise surgical technique and the choice of an appropriate size for the hook-plate are needed. We suggest that early removal of the plate is necessary to decrease the risk of subacromial impingement and erosion in hook-plate fixation. -
Citations
Citations to this article as recorded by- Clinical outcomes of bending versus non-bending of the plate hook in acromioclavicular joint dislocation
Min Su Joo, Hoi Young Kwon, Jeong Woo Kim
Clinics in Shoulder and Elbow.2021; 24(4): 202. CrossRef - Surgical Treatment of Unstable Distal Clavicle Fractures: Comparison of Transacromial Pin Fixation and Hook Plate Fixation
Young Sung Kim, Ho Min Lee, Han Gil Jang
The Journal of the Korean Shoulder and Elbow Society.2013; 16(2): 123. CrossRef
- Clinical outcomes of bending versus non-bending of the plate hook in acromioclavicular joint dislocation
- 1,631 View
- 18 Download
- 2 Crossref

Case Reports
- Bowel Entrapment by Fragments of Acetabular Fracture: A Case Report
- Ji Wan Kim, Jung Jae Kim, Suk Kyung Hong, Kyu Hyuk Kyung, Jin Hee Kim
- J Korean Fract Soc 2010;23(4):373-376. Published online October 31, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.4.373
-
 Abstract
Abstract
 PDF
PDF - Abdominal injuries are common in patients with pelvic or acetabular fracture. However intestinal entrapment or perforation caused by fragments of a pelvic or acetabular fracture is rare and to date there has been no report of this occurring in Korea so far. As it is difficult to diagnose intestinal entrapment caused by fragments of pelvic or acetabular fracture, the entrapment therefore results in intestinal perforation, sepsis, and a high mortality rate in the absence of early detection. We present a case of intestinal entrapment and perforation caused by fragments of acetabular fracture as well as a literature review.
- 369 View
- 0 Download

- Bursting Fracture of the Proximal Femur during Insertion of Unreamed Femoral Nail for Femur Shaft Fracture: A Case Report
- Ji Wan Kim, Seong Eun Byun, Won Hyuk Oh, Jung Jae Kim
- J Korean Fract Soc 2010;23(2):227-231. Published online April 30, 2010
- DOI: https://doi.org/10.12671/jkfs.2010.23.2.227
-
 Abstract
Abstract
 PDF
PDF - When treating femur shaft fracture in adults, undreamed nail can be an option in order to avoid systemic complications. To appropriately insert unreamed intramedullary nail, an accurate entry point and sufficient reaming of the entry portal is essential. The intramedullary canal of the proximal femur must be reamed over than the diameter of the proximal end of the nail. If the proximal reaming is not sufficient, complications such as bursting fracture of proximal femur can occur. We present two cases of bursting fracture of proximal femur following insertion of undreamed intramedullary nail as well as a literature review.
-
Citations
Citations to this article as recorded by- Risk Factors Associated with Intraoperative Iatrogenic Fracture in Patients Undergoing Intramedullary Nailing for Atypical Femoral Fractures with Marked Anterior and Lateral Bowing
Yong Bum Joo, Yoo Sun Jeon, Woo Yong Lee, Hyung Jin Chung
Medicina.2023; 59(4): 735. CrossRef - Results of Intramedullary Nailing of Femoral Shaft Fracture - Trochanteric Entry Portal (Sirus Nail) versus Piriformis Entry Portal (M/DN Nail) -
Sang Ho Ha, Woong-Hee Kim, Gwang Chul Lee
Journal of the Korean Fracture Society.2014; 27(1): 50. CrossRef - Iatrogenic Femur Proximal Shaft Fracture during Nailing Using Lateral Entry Portal on Femur Shaft Fracture
Hong Moon Sohn, Gwang Chul Lee, Chae Won Lim
Journal of the Korean Orthopaedic Association.2014; 49(4): 272. CrossRef
- Risk Factors Associated with Intraoperative Iatrogenic Fracture in Patients Undergoing Intramedullary Nailing for Atypical Femoral Fractures with Marked Anterior and Lateral Bowing
- 858 View
- 2 Download
- 3 Crossref

Original Articles
- Complications of Femoral Peritrochanteric Fractures Treated with the Gamma Nail
- Seok Hyun Kweon, Churl Hong Chun, Jung Hwan Yang, Jin Young Park, Kyu Hwan Bae
- J Korean Fract Soc 2009;22(2):85-90. Published online April 30, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.2.85
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We analyzed the complications of femoral peritrochanteric fractures treated with the Gamma nail to reduce its complications.
MATERIALS AND METHODS
We evaluated the complications among the 96 patients who were treated with the Gamma nail from January 2000 to May 2005. Mean follow-up period was 17.8 months and mean age was 75.2 years. We analysed the relationship between the complication and the fracture pattern, postoperative reduction status, position of the lag screw, bone density, displacement and tip-apex index (TAD).
RESULTS
The complications were presented in 12 cases (12.5%). Cut-out of lag screw were in 5 cases, varus deformity with short lag screw in 2 cases, metal breakage of distal screw in 1 case, breakage of drill bit intraoperatively in 1 case, superficial infection in 2 cases and deep infection in 1 case. 5 cases (4.2%) were required reoperation. All of the cut-out of lag screw showed increased TAD (tip apex distance) above 25 mm.
CONCLUSION
To reduce the complications of the Gamma nail, we need exact surgical technique, good positioning of the lag screw and choice of appropriate length for the lag screw. -
Citations
Citations to this article as recorded by- Effectiveness of the Valgus Reduction Technique in Treatment of Intertrochanteric Fractures Using Proximal Femoral Nail Antirotation
Ji-Kang Park, Hyun-Chul Shon, Yong-Min Kim, Eui-Sung Choi, Dong-Soo Kim, Kyoung-Jin Park, Byung-Ki Cho, Jung-Kwon Cha, Sang-Woo Kang
Journal of the Korean Orthopaedic Association.2013; 48(6): 441. CrossRef
- Effectiveness of the Valgus Reduction Technique in Treatment of Intertrochanteric Fractures Using Proximal Femoral Nail Antirotation
- 827 View
- 1 Download
- 1 Crossref

- Factors Predicting Complications after Internal Fixation of Femoral Neck Fractures
- Tae Ho Kim, Jong Oh Kim, Sung Sik Kang
- J Korean Fract Soc 2009;22(2):79-84. Published online April 30, 2009
- DOI: https://doi.org/10.12671/jkfs.2009.22.2.79
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the factors predicting complications after internal fixation using multiple cannulated screws in the patients with femoral neck fracture, the authors performed a comparative study of a success group and a failure group and reviewed the literature.
MATERIALS AND METHODS
Sixty-eight patients with intracapsular femoral neck fractures were treated by multiple pinning from January 2000 to July 2007 and followed up more than one year. Relationships between the complications such as failure of union, collapse of femoral head due to osteonecrosis of femoral head and several affecting factors including the degree of displacement by Garden stage, state of reduction, position of screws, patient's age, time interval from injury to operation, anatomical fracture site and two weeks postoperative (99m)Tc-MDP bone scan were analyzed.
RESULTS
Statistically significant factors were the degree of displacement by Garden stage (p<0.001), reduction state (p<0.001) and postoperative two weeks (99m)Tc-MDP bone scan (p<0.001).
CONCLUSION
An accurate anatomical reduction is needed to decrease complications with multiple cannulated screws fixation of femoral neck fracture. Displacement of fracture by Garden stage and (99m)Tc-MDP bone scan are major factors predicting complications.
- 913 View
- 1 Download

- Complications of Femoral Pertrochanteric Fractures Treated with Proximal Femoral Nail (PFN)
- Kee Byoung Lee, Byung Taek Lee
- J Korean Fract Soc 2007;20(1):33-39. Published online January 31, 2007
- DOI: https://doi.org/10.12671/jkfs.2007.20.1.33
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We analyzed the complications of femoral pertrochanteric fractures treated with proximal femoral nail (PFN®) to reduce the its complications.
MATERIALS AND METHODS
We evaluated the complications among 198 patients who were treated with PFN® from June 2001 to August 2005 in our hospital.
RESULTS
The complications were presented in 28 cases (14.1%). Cut-out of lag screw was in 1 case, cut-out of lag screw and antirotation screw were in 3 cases, cut-out of antirotation screw in 3 cases, of these femoral head fracture was in 1 case. Femoral neck fracture in 1 case, Osteonecrosis of femoral head in 1 case, cortical fracture during the insertion of distal interlocking screw in 1 case, breakage of drill bit intraoperatively in 1 case, fibrous union in 2 case, thigh skin irritation due to screw back-out in 3 cases, periprosthetic fractures in 2 cases, varus collapse more than 10 degrees in 4 cases, superficial and deep infections in 3 cases, breakage of nail in 1 case, varus collapse after PFN removal in 1 case, persistent thigh pain in 1 case. Of all these cases, 9 cases (4.5%) were required reoperation with general or spinal anesthesia. Complications related with screws or fracture reduction were 19 cases (9.6%) and, of these, 17 cases (89.5%) showed increased TAD (tip apex distance) or nonanatomical reduction.
CONCLUSION
To reduce the complications of PFN®, we need to exact surgical technique and anatomical reduction and consider the modification of implant design to prevent of cut-out of screws. -
Citations
Citations to this article as recorded by- Intraoperative Abdominal Penetration of the Lag Screw: A Rare Complication During Proximal Femoral Nail Anti‐Rotation Surgery
Mohammad Javad Dehghani Firoozabadi, Ramin Bozorgmehr, Fatemeh Bastan, Maryam Rashidian
Clinical Case Reports.2026;[Epub] CrossRef - Proximal Femoral Nail Mechanical Failure: A Case Report and Biomechanical Study
Dimitrios Papanikolopoulos, Christos Kalligeros, Apostolos Polyzos, Vasileios Spitas, Vasileios Soranoglou
Cureus.2022;[Epub] CrossRef - Clinical and radiological outcomes of patients treated with the talon distalfix proximal femoral nail for intertrochanteric femur fractures
Furkan Yapici, Hanifi Ucpunar, Yalkin Camurcu, Necati Emirhan, Oguzhan Tanoglu, Ismail Tardus
Injury.2020; 51(4): 1045. CrossRef - Implant Fracture Analysis of the TFNA Proximal Femoral Nail
Anton Lambers, Bertram Rieger, Alan Kop, Peter D’Alessandro, Piers Yates
Journal of Bone and Joint Surgery.2019; 101(9): 804. CrossRef - Radiographic Outcomes of Osteosynthesis Using Proximal Femoral Nail Antirotation (PFNA) System in Intertrochanteric Femoral Fracture: Has PFNA II Solved All the Problems?
Won Chul Shin, Jung Dong Seo, Sang Min Lee, Nam Hoon Moon, Jung Sub Lee, Kuen Tak Suh
Hip & Pelvis.2017; 29(2): 104. CrossRef - Avascular necrosis of the femoral head following trochanteric fractures in adults: A systematic review
Antonio Barquet, Gabriel Mayora, Joao Matheus Guimaraes, Roberto Suárez, Peter V. Giannoudis
Injury.2014; 45(12): 1848. CrossRef - Anatomical Measurement of Normal Korean Proximal Femur Using Plain Radiography: A Problem when using Proximal Femoral Nail Anti-rotation
Jong-Seok Park, Woo-Jong Kim, Jae-Wan Soh, Byung-Woong Jang, Tae-Heon Kim, You-Sung Suh
Hip & Pelvis.2011; 23(4): 303. CrossRef - PFNA and PFN in Intertrochanteric Fractures - Comparison Study of Sliding -
Suk Kyu Choo, Hyoung Keun Oh, Jun Young Choi
Hip & Pelvis.2010; 22(1): 79. CrossRef
- Intraoperative Abdominal Penetration of the Lag Screw: A Rare Complication During Proximal Femoral Nail Anti‐Rotation Surgery
- 1,475 View
- 16 Download
- 8 Crossref

Case Report
- Spontaneous Intramuscular Hematoma associated with Acute Compartment Syndrome after Treatment of Low Molecular Weight Heparin: A Report of Two Cases
- Keun Woo Kim, Woo Dong Nam, Kee Hyung Rhyu, Byung Ryul Cho, Yong Hoon Kim, Soo Ik Awe
- J Korean Fract Soc 2006;19(1):89-92. Published online January 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.1.89
-
 Abstract
Abstract
- Low-molecular-weight heparin (LMWH) has been considered superior to unfractionated heparin in several facets such as more effective anticoagulant, more predictable bioavailability, and less bleeding complications. We report two cases of LMWH, enoxaparin-induced spontaneous intramuscular hematoma with compartment syndrome of the lower extremity in patients with cardiac problems. The patients were treated with enoxaparin (LMWH) as bridging anticoagulation before use of warfarin due to cardiac problems. At the average 3 days of enoxaparin treatment, large and painful swelling was noticed in the lower extremities without intramuscular injection or trauma. The patients were diagnosed as having compartment syndrome with large intramuscular hematoma by CT. The patients underwent immediate fasciotomy and hematoma evacuation, and recovered without any complications.
- 624 View
- 0 Download

Original Articles
- Elbow Function and Complications after Internal Fixation for Fractures of the Distal Humerus
- Hyug Soo Ahn, Young Ho Cho, Young Soo Byun, Do Yop Kwon, Seung Oh Nam, Dong Young Kim
- J Korean Fract Soc 2006;19(1):56-61. Published online January 31, 2006
- DOI: https://doi.org/10.12671/jkfs.2006.19.1.56
-
 Abstract
Abstract
- PURPOSE
To evaluate the functional results of the elbow and the complications after internal fixation for distal humeral fractures.
MATERIALS AND METHODS
We reviewed 38 distal humeral fractures; 12 type A, 7 type B and 19 type C by AO classification. There were six low columnar fractures in type A and nine in type C. Six type C fractures were open. The fracture healing and complications were assessed and the functional result was evaluated by rating system of Jupiter et al.
RESULTS
Type A fractures were healed in an average of 10.6 weeks, type B 7.7 weeks and type C 11.5 weeks. Ulnar neuropathy occurred in six cases, loss of fixation in two cases, nonunion in one case, heterotopic ossification in one case and traumatic arthritis in one case. The functional result showed excellent or good in 34 cases (89%) and fair or poor in 4 cases (11%). Open fractures showed significantly worse result than closed fractures.
CONCLUSION
To obtain the satisfactory results, stable fixation followed by early motion is required in most distal humeral fractures. Ulnar neuropathy occurs postoperatively in high incidence and the result of open fractures is worse than that of closed fractures. -
Citations
Citations to this article as recorded by- Comparison of Shoulder Range of Motion, Pain, Function, Scapular Position Between Breast Cancer Surgery and Shoulder Surgery Female Patients
Min-ji Lee, Suhn-yeop Kim, Jae-kwang Shim
Physical Therapy Korea.2015; 22(1): 9. CrossRef - Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate
Hyoung Keun Oh, Suk Kyu Choo, Jung Il Lee, Dong Hyun Seo
Journal of the Korean Fracture Society.2012; 25(4): 305. CrossRef - Nonunion of Humeral Intercondylar Comminuted Fracture Treated with Fibular Graft - A Case Report -
Jin Rok Oh, Chang Ho Lee, Ki Yeon Kwon, Hoi Jeong Chung
Journal of the Korean Fracture Society.2010; 23(1): 118. CrossRef - Double Parallel Plates Fixation for Distal Humerus Fractures
Young Hak Roh, Moon Sang Chung, Goo Hyun Baek, Young Ho Lee, Hyuk-Jin Lee, Joon Oh Lee, Kyu-Won Oh, Hyun Sik Gong
Journal of the Korean Fracture Society.2010; 23(2): 194. CrossRef
- Comparison of Shoulder Range of Motion, Pain, Function, Scapular Position Between Breast Cancer Surgery and Shoulder Surgery Female Patients
- 598 View
- 0 Download
- 4 Crossref

- Early Postoperative Complications of Calcaneal Fractures Following Operative Treatment by a Lateral Extensile Approach
- Young Soo Byun, Young Ho Cho, Jun Woo Park, Jin Seok Lee, Ji Hwan Kim
- J Korean Fract Soc 2004;17(4):323-327. Published online October 31, 2004
- DOI: https://doi.org/10.12671/jkfs.2004.17.4.323
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze early postoperative complications of calcaneal fractures operated by a lateral extensile approach and to identify risk factors for wound complications.
MATERIALS AND METHODS
From July 1990 to February 2003, 116 calcaneal fractures in 104 patients were treated by open reduction and internal fixation through a lateral extensile approach. The patient's records were reviewed for early postoperative complications. Statistical analysis was performed to determine significant relationships between predicted variables and the development of wound complications.
RESULTS
Fourteen fractures (12.0%) developed infection. Ten of them were superficial infection and four were deep infection that required surgical treatment. Eight fractures (6.9%) developed skin necrosis. Six of them were marginal skin necrosis and two were flap necrosis that required surgical treatment. Seven fractures (6.0%) developed sural nerve injury, but their symptoms were improved without additional treatment. Open fracture (p=0.003) and prolonged operating time (p=0.049) increased significantly the rate of wound complications.
CONCLUSION
The rate of early postoperative complications of calcaneal fractures operated by a lateral extensile approach is high. These complications can be reduced by meticulous treatment of an open wound, reduced operating time within 90 minutes through preoperative planning and skillful technique, and correct incision to avoid damage of the sural nerve. -
Citations
Citations to this article as recorded by- Results in Operative Treatment of Open Calcaneal Fracture
Ba Rom Kim, Jun Young Lee, Donghyuk Cha
Journal of Korean Foot and Ankle Society.2021; 25(3): 133. CrossRef - Bilateral Open Transcalcaneal Fracture with Talonavicular Dislocation - A Case Report -
Hun Park, Sung Jin Shin, Sang Rim Kim, Kwang Woo Nam, Sung Wook Choi, Kyu Bum Seo, Jun Young Seo
Journal of the Korean Fracture Society.2011; 24(1): 87. CrossRef - Treatment of Intra-articular Calcaneal Fractures Using Minimally Invasive Sinus Tarsi Approach in Diabetic Patients
Hong-Moon Sohn, Sang-Ho Ha, Sang-Hong Lee, Jun-Young Lee, Jeong-Ho Kim, Sang-Jun Lee
Journal of the Korean Fracture Society.2008; 21(3): 195. CrossRef
- Results in Operative Treatment of Open Calcaneal Fracture
- 521 View
- 1 Download
- 3 Crossref

- A Clinical Study about Postoperative Wound Complications In Liver Cirrhotic Patients
- Seung Woo Suh, Seok Hyun Lee, Jun Kyu Moon, Young Jin Roh, Chang Woo Seok
- J Korean Soc Fract 2003;16(4):577-584. Published online October 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.4.577
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study undertaken to evaluate the postoperative wound complications between Child class A liver cirrosis patients and Child class B liver cirrhosis patients.
MATERIALS AND METHODS
In a retrospective study from 1998 to 2003, fifteen patients who underwent surgical intervention for fractures were evaluated the period of wound healing, hopital day, infection, wound complications (swelling, hematoma formation, wound discharge).
RESULTS
The cases of wound complication are 6/15 (40%), in which Child class A LC patients are two (14%), and Child class B LC patients are four (50%). The cases of wound Infection are 2/15 (13%), in which Child class A LC patient is one (14%), and Child class B LC patient is one (12.5%). The average of hospital day is 28 days.
CONCLUSION
The clinical results of postoperative complications is associated with Child classification, but the ralationship between postoperative wound infection and Child classification is not observed. We thought that careful wound management needs in liver cirrhosis patients.
- 346 View
- 0 Download

- Factors Predisposing to Complications After Internal Fixation of Femoral Neck Fracture
- Sang Won Park, Chang Yong Hur, Jong Ryoon Baek, Seong Jun Park
- J Korean Soc Fract 2003;16(4):441-446. Published online October 31, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.4.441
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the factors predisposing to complications after internal fixation of femoral neck fracture.
MATERIALS AND METHODS
We reviewed retrospectively the results of percutaneous internal fixation of femoral neck fracture using multiple pinning, in 52 cases who were treated from Jan. 1996 to Dec. 2001. Relationship between the complications and several factors such as the age, sex, time interval from injury to operation, Garden stage, Singh index, internal fixation device and state of redction were analyzed.
RESULTS
The functional results by Lunceford criteria were excellent in 23 cases (44%), good in 15 cases (29%), fair in 2 cases (3.8%) and poor in 12 cases (23.1%). The avascular necrosis of the femoral head were occured in 14 cases (26.9%). Among these, 1 case of non-union, 2 cases of mal-union were accompanied. No stastically significant relationship between the age, sex, time interval from injury to operation, Garden stage, Singh index, internal fixation device, state of redction and complication. However, there was 4 times higher complication rate in Garden stage 3 or 4 group than its rate in Garden stage 1 (odds ratio 3.889), and 3 times higher complication rate in non-anatomical reduction group (odds ratio 3.22).
CONCLUSION
Factors predisposing to complications after internal fixation of femoral neck fracture seemed to closely relate with Garden stage and state of reduction. -
Citations
Citations to this article as recorded by- Bipolar Hemiarthroplasty for the Femoral Neck Fractures in Elderly Patients
Woong-Kyo Jeong, Sang-Won Park, Soon-Hyuck Lee, Jong-Hoon Park, Suk-Ha Lee, Ji-Hoon Kang, Gi-Won Choi, Won Noh
Journal of the Korean Fracture Society.2008; 21(1): 8. CrossRef
- Bipolar Hemiarthroplasty for the Femoral Neck Fractures in Elderly Patients
- 575 View
- 0 Download
- 1 Crossref

- The Correlation between Surgical Timing and Perioperative Complications in the Treatment of Displaced Supracondylar Humeral Fractures of Children
- Soo Hong Han, Duck Yun Cho, Hyung Ku Yoon, Byung Soon Kim, Jae Hwa Kim, Hyung Kun Park, Se Hyen Kim
- J Korean Soc Fract 2003;16(2):278-283. Published online April 30, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.2.278
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Even though emergent percutaneous pinning after closed reduction is the popularized treatment of the displaced type II and type III pediatric supracondylar fractures of the humerus, the timing of pinning still presents controversy. The purpose of this study is to suggest an appropriate surgical time without significant perioperative complications.
MATERIALS AND METHODS
From April 1995 to January 2002, 179 consecutive patients who had undergone surgical treatment were selected. They were divided to 5 groups [A group: 8 hours or less following injury (24 cases), B group: from 9 to 16 hours (63 cases), C group: from17 hours to 24 hours (63 cases), D group: from 25 hours to 48 hours (18 cases), and E group: from 49 hours to 72 hours (11 cases)] and reviewed retrospectively to analyze perioperative complications and operation time.
RESULTS
There was no significant difference between each group with respect to surgical wound infection, iatrogenic ulnar nerve injury, VIC, operation time and the necessity of reoperation (p>0.05).
CONCLUSION
Within the parameters outlined in our study, we could not find the any meaningful correlation between surgical timing and occurrence of perioperative complications and also, we think that the timing of percutaneous pinning can be delayed to the time when a surgeon considers it appropriate.
- 398 View
- 0 Download

- Management of Both Tibia Fracture
- Kyung Jin Song, Sang Hun Song, Jong Hyuk Park
- J Korean Soc Fract 2003;16(2):186-193. Published online April 30, 2003
- DOI: https://doi.org/10.12671/jksf.2003.16.2.186
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The purpose of this study was to analyze the associated injury, difficulties in management and complications with surgery, and to suggest the guideline according to the severity and type of injury in the management of both tibia fractures. MATERIAL AND METHOD: We analyzed 12 patients, 8 men and 4 women and their age was 43.4 years old in average. The cause of injury was traffic accident in 10, autobike in 1 and farm machine injury in 1 case. There were both open tibia fracture in 6, one side open fracture in 2 and both closed fracture in 4 cases. We analyzed the average interval from injury to operation, duration of hospitalization, duration of both side bone union and complications.
RESULTS
In both open tibia fracture, the average interval from injury to operation was 12.5 days, average duration of hospitalization was 3.2 months, and average duration of bone union was 14.5 months. In one side open fracture, the average interval to operation was 25 days, average duration of hospitalization was 3.75 months, and average duration of bone union was 8.7 months. In both closed fracture, the average interval to operation was 15 days, average duration of hospitalization was 1.92 months, and average duration of bone union was 4.8 months.
CONCLUSION
Both tibia fractures were caused by high energy and also associated with multiple injury, and fracture stability and soft tissue damage should be evaluated thoroughly before surgery. Anatomical reduction and rigid fixation should be necessary to reduce the post-surgical complications.
- 373 View
- 0 Download

- Neurologic Complications of Elbow Fractures in Children
- Suk Kyu Choo, Gyu Won Park
- J Korean Soc Fract 2002;15(4):595-600. Published online October 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.4.595
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We analyzed neurologic complications of the elbow fractures in children and evaluated clinical results of type of fractures, frequency of nerve injuries and displacement of fracture fragments and spontaneous recovery of each nerve injuries.
MATERIALS AND METHODS
We analyzed 17 child-patients (20cases) with nerve injuries who were treated conservatively and follewed up for at least 1 year since December 1999. and we analyzed type of fractures, differences between fracture type and nerve injuries, frequency of each nerve injuries and periods of spontaneous recovery of each nerves.
RESULTS
There were all 148 elbow fractures in children. Children with neurologic complications were 17(20 nerves) and 14 in supracondylar and 3 in medial epicondylar fractures. There were 6 in radial nerve, 8 in ulnar nerve, 3 in median nerve and 3 in anterior interosseous nerve. Both ulnar and median nerve injuries were 3 patients. They were recovered spontaneously and mean periods of recovery was 7.3 weeks, 6.5 weeks in radial nerves, 7.0 in median nerves, 7.6 in anterior interosseous nerves, 7.8 in ulnar nerves and radial nerve recovery was most fast than any others. One patient with ulnar nerve injury who was diagnosed medial epicondylar fracture recovered 2 weeks after excision of nonuioned fragment. Among 14 supracondylar fractures, there was 11 posteromedial displacement, 1 posterolateral and 2 posterior. Most of them was displaced posteromedially.
CONCLUSION
All nerve injuries happened in supracondylar and medial condylar fractures and almost recovered. Nerve injuries in the supracondylar fractures was displaced fractures than nondisplaced simple fractures and displacement of fracture fragment and nerve injuries was not agreed with previous published books or papers. We recommand that observation is the appropriate way to manage these nerve injuries in most cases than immediate operation for excision.
- 417 View
- 1 Download

- The Significance of Posterior Cortex in Complicated Femoral Neck Fractures which were Internal Fixated
- You Sung Suh, Seok Bong Jung, Soo Jae Yim, Jong Seok Park, Byung Ill Lee
- J Korean Soc Fract 2002;15(4):511-518. Published online October 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.4.511
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
When a surgeon carries out an operative treatment on a patient who has fractures of the femoral neck, he decides to do either the internal fixation for bony union or the aggressive treatment according to his experience and preparation, not according to the objective standard. The aim of this retrospective study is to prepare a guideline for the operative method.
MATERIALS AND METHODS
We analyse possible factors of the patient who has nonunion, avascular necrosis and loss of fixation after doing internal fixation in femoral neck fractures RESULTS: In this treated case of femoral neck, the appearance of complications are influenced by the maintenance of internal fixation, shape of fractures, osteoporosis, and the position of fixations; but in the complicated cases without the loss of fixation, the shape of fractures always have posterior cortical communition.
CONCLUSION
When we choose between simple fixation and aggressive treatments in cases of fractures of the femoral neck, we must treat according to the patient 's condition, displacement of the fracture, operative technique and existence of a posterior cortical comminuted fracture.
- 393 View
- 0 Download

- Adverse Effect of the Absorbable Rods in Treatment of the Radial Head & Neck Fractures
- Weon Ik Lee, Jun Dong Chang, Soo Joong Choi, Byeong Kook Lee, Young Jin Seo, Chang Ju Lee
- J Korean Soc Fract 2002;15(3):414-420. Published online July 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.3.414
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We report complications occurred from 6 patients among 14 patients who received the operation for their radial head and neck fractures by using the absorbable rod made by poly-glycolic acid(PGA).
MATERIALS AND METHODS
We analyze the postoperative results of 14 patients who recieved fixation by absorbable rod for the radial head and neck fractures from March 1991 to March 2000. All of the fractures were are reducible and modified Mason 's type II.
RESULTS
After average 15 months follow up, flexion contracture was average 20 degrees and full flexion was average 130 degrees. Complications were occurred in 6 cases. Osteolysis was occurred in 3 cases and in 2 cases among theses 3 cases, radial head excision was performed. Synovitis was occured in other 3 cases and in one case joint fluid was drainaged from operation wound for 2 weeks and in other 2 cases, synovitis was progressed to arthritis.
CONCLUSION
The absorbable rod made of PGA in radial head and neck fracture have relatively high rate of adverse tissue responses. So surgeon should consider adverse tissue response of PGA. Development of more biocompatible absorbable and slow degrading material should be needed.
- 462 View
- 0 Download

- Complications and Affecting Factors for Intracapsular Femoral Neck Fractures Treated by Multiple Pinning
- Sung Jung Kim, Shin Yoon Kim, Gi Bong Cha, Chang Wug Oh, Il Hyung Park, Joo Chul Ihn
- J Korean Soc Fract 2002;15(2):201-208. Published online April 30, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.2.201
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To investigate the relationship between the complications of intracapsular femoral neck fractures treated by multiple pinning and several affecting factors.
MATERIALS AND METHODS
Sixty-eight patients with intracapsular femoral neck fractures were treated by multiple pinning from March 1993 to January 2000 and followed at more than one year. Relationship between the complications such as failure of union, collapse of femoral head due to osteonecrosis of femoral head and several affecting factors including displacement of fracture according to Garden stage, state of reduction, position of screws, time interval from injury to operation, and fracture level were analyzed. The Fisher exact test, chi-square test, and multivariate logistic regression analysis were used to find the relevant factors influencing incidence of complications. Statistical significance was set at p < 0.05.
RESULTS
Position of screw was the most important single factor affecting the results of treatment of intracapsular femoral neck fracture (p=0.046). Moreover, the Garden stage and position of screw were revealed affecting the incidence of complications together with other factors (each p value was 0.028 and 0.027).
CONCLUSION
We considered that satisfactory position of screw was important to reduce complications after multiple pinning for intracapsular femoral neck fracture. And the results of operation also seemed to closely relate with multiple factors including Garden stage and status of reduction. -
Citations
Citations to this article as recorded by- Factors Predicting Complications after Internal Fixation of Femoral Neck Fractures
Tae-Ho Kim, Jong-Oh Kim, Sung-Sik Kang
Journal of the Korean Fracture Society.2009; 22(2): 79. CrossRef
- Factors Predicting Complications after Internal Fixation of Femoral Neck Fractures
- 514 View
- 0 Download
- 1 Crossref

- The Complications during Treatment of Femoral Neck Fracture in Children - Coxa Vara, SCFE and Avascular Necrosis
- Myung Rae Cho, Won Jae Song, Jeong Hwan Son, Jeong Ho Park
- J Korean Soc Fract 2002;15(1):1-6. Published online January 31, 2002
- DOI: https://doi.org/10.12671/jksf.2002.15.1.1
-
 Abstract
Abstract
 PDF
PDF - Femur neck fractures in children are relatively rare by comparison with the incidence in adults and can occur by high-energy trauma. The common complications of femoral neck fracture are avascuar necrosis, coxa vara, premature physeal closure and nonunion. The femoral neck fracture by traffic accident in 7-years-old girl was reduced closely and fixed internally. After 1 year later, varus deformity, slipped capital femoral epiphysis and avascular necrosis occurred. Valgus osteotomy and epiphysiodesis were done. There are many series of complications after femoral neck fractures in children, but the case followed by varus deformity, slipped capital femoral epiphysis and avascular necrosis as complications is rare. We report the clinical and radiologic finding of this case with pertinent literature.
- 532 View
- 0 Download

- Complications after treatment of tibial Non fracture
- Ki Do Hong, Sung Sik Ha, Hyun Jong Cha
- J Korean Soc Fract 2001;14(4):668-676. Published online October 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.4.668
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Aim of this study was to find the treatment and preventive method of the complication occurred after treatment of tibial pilon fracture. MATERIAL AND METHODS: 10 cases of complication, which has required the unplanned operative treatment among 25 cases of tibial pilon fracture from 1994 to 1999 were analyzed rertrospectively according to the Ruedi-Allgower classification, open or closed fracture, isolated or polytrauma , type of complication, type of procedure, primary or delayed wound closure.
RESULTS
There were 1 type I, 3 type II, and 6 type III Ruedi-Allgower fracture type, 3 open fracture, 7 isolated and 3 polytrauma. 6 required plastic surgery procedure such as pedicle flap or full thickness skin graft and 7 required orthpaedic procedure such as osteotomy, cancellous bone graft, metal removal and currettage, debridement of ankle.
CONCLUSION
The complications after treatment of tibial pilon fracture are classified to intraoperative, early and late postoperative complication. Intraoperative complication include penetration of the joint by screw and inadequate reconstitution of the articular surface which can be avoided by taking intraoperative roetgenograms, early complication include wound necrosis which can be minimized by good soft tissue technique, late complication include nonunion, joint stiffness and posttraumatic arthritis can be treated by osteotomy, cancellous bone graft and anatomic reduction with early motion.
- 356 View
- 0 Download

- Ipsilateral Femoral Neck and Shaft Fracture: Secondary Avascular Necrosis of Femoral Head
- Sung Taek Jung, Keun Bae Lee, Taek Lim Yoon, Sang Don Shim, Myung Seon Kim
- J Korean Soc Fract 2001;14(4):609-615. Published online October 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.4.609
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the prognostic variables that influence the incidence of complication such as avascular necrosis of femoral head, nonunion of neck after the treatment of ipsilateral femoral neck and shaft fracture by the results and long term follow up. MATERIAL AND METHODS: We studied the 18 cases of 17 patients that could be follow up over 2 years among the patients received the treatment of ipsilateral femoral neck and shaft fracture from 1987 to 1998. The average follow up duration was 54.3 months (24-120) and all patients was men. The average age was 38.2 yrs(20-60). Fifteen cases of femoral neck fracture were treated with multiple pinning and 3 cases with the compression hip screw, 12 cases of femoral shaft fracture were treated with DCP, 5 cases by interlocking IM nailing and 1 case, open fracture, by external fixator. We evaluated the bone union and complication such as avascular necrosis of femoral head and nonunion.
RESULTS
For femoral neck fracture, resection arthroplasty was performed in 1 case and nonunion in 1 case. Bone union was obtained at average 4 months in 16 cases of femoral neck fracture, at 9 months in all cases of shaft fracture. The avascular necrosis of femoral head in 5 cases included 1 case of nonunion was found at minimal 20 months to maximal 59 months follows up.
DISCUSSION
All prognostic variables of the ipsilateral femoral neck and shaft fracture, that is the Garden stage, Pauwels classification, delayed time to operation. had no statistical correlation with complication. Whenever possible the patients should be followed for a minimum 5 years to rule out avascular necrosis of femoral head.
- 392 View
- 1 Download

- Complications after Surgical Treatment in Fracture of The Neck of Humerus
- Ho Jung Kang, Sang Jin Shin, Dae Eui Lim, Eung Shick Kang
- J Korean Soc Fract 2001;14(1):91-98. Published online January 31, 2001
- DOI: https://doi.org/10.12671/jksf.2001.14.1.91
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
The causes and risk factors of complications following operative treatment of fracuture of neck of humerus were analysis. MATERIALS & METHODS: From 1995 to 1998, 32 cases of fracture of neck of humerus on which operative treatment have been taken were reviewed. The average age was 48.3 years. There were 13 cases of two part fracture, 11 cases of three part fracture and 8 cases of four part fracture, with 4 cases associated with comminution. Closed reduction and pinning was performed in 11 cases. An external fixator was applied in 1 case. Other 18 cases underwent open reduction using various fixation method including 4 K-wires, 2 cannulated screws, 5 plates, 1 Ender nail and 6 tension band wirings combined with screws each. 2 cases were underwent hemiarthroplasty.
RESULTS
Thirteen patients (41%) had postoperative complications. There were 3 nonunion, 2 pin site infection, 2 inferior subluxation of humeral head, 3 impingement syndrome, 1 hardware failure, 1 avascular necrosis of humeral head and 1 glenoid rim erosion. The incidence of postoperative complication was high in ages older than 40 years and the four part and comminuted fractures. The insufficient fixation due to osteoporosis, incomplete reduction, surgical technique and use of inappropriate implant were considered as related causative factures.
CONCLUSION
The patient's age, the quality of bone, severity of fracture and methods of fixation are all important contributing factors for postoperative complications.
- 462 View
- 4 Download

- Ender Nailing of Tibial Shaft Fractures
- In Young Ok, Yang Guk Chung, Tec Soo Kim
- J Korean Soc Fract 2000;13(1):87-95. Published online January 31, 2000
- DOI: https://doi.org/10.12671/jksf.2000.13.1.87
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Though Ender nailing in tibial shaft fractures is a good method of treatment, there were several reports about complications such as angulation or shortening. Most of those complications were associated with improper surgical technique and might be avoidable. So, we analyzed the results of tibial Ender nailing in view of the complications and their contributing factors. MATERIAL AND METHOD: Thirty-five tibial shaft fractures were treated with Ender nailing and followed up for 12 to 51 months. We evaluated the bony union, angulation, shortening, proximal migration of nail and infection, and analyzed the results in association with the type and the location of fractures, the number and the length of nails and the divergency of distal tip of nails.
RESULTS
Average bony union time was 18.5 weeks and there were 2 delayed unions, 2 nonunions, 5 angulations, 1 shortening, 3 soft tissue irritations by proximal tips of nails, 1 proximal migrations of nails and one nail breakage. Most of them were associated with technical faults such as few number, short length or insufficient divergency of nails. According to the type of fractures, the highest rate of complications was seen in segmental fractures.
CONCLUSION
Performed by proper surgical technique based on detailed fracture analysis, most of the complications of Ender nailing for tibial shaft fractures might be avoidable. Therefore, Ender nailing is one of the useful alternatives for tibial shaft fractures. -
Citations
Citations to this article as recorded by- Manoeuvring Distal Tibial Shaft Fractures with Ender’s Nailing: Case Series
Aditya Pundkar, Chandrashekar Kulkarni
Journal of Datta Meghe Institute of Medical Sciences University.2023; 18(3): 481. CrossRef
- Manoeuvring Distal Tibial Shaft Fractures with Ender’s Nailing: Case Series
- 573 View
- 0 Download
- 1 Crossref

- Comparison between results of treatment of the Femoral Neck and Intertrochanteric Fractures : Focused on Mortality rate and Complications
- Chung Soo Hwang, Phil Hyun Chung, Suk Kang, Tae Hoon Kim, Han Chul Kim, Yong Soon Kim
- J Korean Soc Fract 1999;12(4):792-802. Published online October 31, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.4.792
-
 Abstract
Abstract
 PDF
PDF - The incidence of femoral neck and intertrochanteric fractures has steadily increased with lengthening of the life span. It is well known that anatomical characteristics of femoral neck may evoke complications such as nonunion and avascular necrosis. And there are many problems in the treatment of femoral intertrochanteric fractures due to osteoporosis, unstable pattern of fracture and poor general condition in elderly patients. The author analyzed 56 cases(56 patients) of femoral neck fractures and 63 cases(61 patients) of femoral intertrochanteric fractures which we have been able to follow up more than 1 year from March 1991 to March 1997. The purpose of this study is 1) to analyze results of treatment, predisposing factors, complications and mortality rates, and so 2) to reduce the mortality rate and complication in these fractures. The results were as follows , 1. The difference in union time between both type of fractures was not significant. 2. The mortality rate during admission was 1.8% in femoral neck fractures and 6.3% in intertrochanteric fractures. 3. The mortality rate during 1 years was 3.6% in femoral neck fractures and 9.5% in femoral intertrochanteric fractures. 4. The predisposing factors associated with postoperative mortality rate were malnutrition. chronic obstructive pulmonary disease, previous contralateral hip fracture, and operation within 3 days.
-
Citations
Citations to this article as recorded by- Anesthetic considerations for surgical treatment of geriatric hip fracture
Dong Kyu Lee, Seunguk Bang, Sangseok Lee
Anesthesia and Pain Medicine.2019; 14(1): 8. CrossRef - A Comparison of Clinical Results between Compression Hip Screw and Proximal Femoral Nail as the Treatment of AO/OTA 31-A2.2 Intertrochanteric Femoral Fractures
Phil Hyun Chung, Suk Kang, Jong Pil Kim, Young Sung Kim, Ho Min Lee, In Hwa Back, Kyeong Soo Eom
Journal of the Korean Orthopaedic Association.2016; 51(6): 493. CrossRef - Postoperative Mortality and the Associated Factors in Elderly Patients with Hip Fracture
You-Sung Suh, Yong-Beom Kim, Hyung-Suk Choi, Hong-Kee Yoon, Gi-Won Seo, Byung-Ill Lee
Journal of the Korean Orthopaedic Association.2012; 47(6): 445. CrossRef - One-Year Mortality Rate of Patients over 65 Years Old with a Hip Fracture
Phil Hyun Chung, Suk Kang, Jong Pil Kim, Young Sung Kim, Ho Min Lee, Young Hwa Choi
Hip & Pelvis.2011; 23(2): 137. CrossRef
- Anesthetic considerations for surgical treatment of geriatric hip fracture
- 1,126 View
- 2 Download
- 4 Crossref

- The Problems of Locked Intramedullary Nailing in the Proximal Shaft Fractures of the Tibia
- Jin Woo Kwon, Kyoung Tae Sohn, Seung Ho Shin, Jae Il Kim
- J Korean Soc Fract 1999;12(1):76-82. Published online January 31, 1999
- DOI: https://doi.org/10.12671/jksf.1999.12.1.76
-
 Abstract
Abstract
 PDF
PDF - Proximal shaft fractures of the tibia have a high incidence of complication and often result in poor outcomes. Plate fixation and locked intramedullary nailing are the most common methods of treatment, but now the latter is more popular because of soft tissue problem, osteomyelitis etc.. The purpose of this study is to evaluate the results of locked intramedullary nailing in the treatment of proximal shaft fractures of the tibia and to draw a conclusion that what type of fracture patterns are the appropriate indication of nailing. We analyzed 18 proximal shaft fractures of the tibia which were treated by locked intramedullary nailing from October 1991 to March 1997 and followed more than 12 months. The results were as follows ; The complications were occurred in 12 cases(66.6%); 4 cases of delayed or non-union, 8 of angular deformity, 1 of leg length discrepancy. Delayed or non-unions were caused by fracture site comminution and bone defect. 5 anterior angular deformities were due to the pulling of the knee extensor mechanism and 3 valgus deformities were due to medially located entry portal. In conclusion, since locked intramedullary nailing in proximal tibial fractures causes a high incidence of complications, it is recommended in transverse or undisplaced fractures. And plate fixation and bone graft will be recommended in comminuted or displaced oblique fractures, if soft tissue condition is permitted.
- 375 View
- 1 Download

- Surgical Treatment of Displaced Acetabular Fractures - focused on Complications after open reduction -
- Chung Nam Kang, Jong Oh Kim, Kong Uk Kim, Yeong Do Koh, Byeong Geun Kim
- J Korean Soc Fract 1998;11(3):477-486. Published online July 31, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.3.477
-
 Abstract
Abstract
 PDF
PDF - Management of displaced fractures of the acetabulum represents one of the greatest challenges in fracture surgery. The results had been proved to be successful after anatomical reduction and stable internal fixation. The purpose of this study is to analyze the clinical results and complications of open reduction of the displaced acetabular fractures to minimize the complications, and to present suggestions for the treatment of these fractures. We reviewed our experience with 23 displaced acetabular fractures which had been treated by open reduction to evaluate the clinical results and complications. The results were as follows; 1. The most common type of elementary fractures was posterior wall fractures according to Letournel's classification. 2. Excellent or good results were obtained in 88% among the satisfactory reduction group, and it means that accurate reduction was the most reliable factors contributing to successful clinical outcomes. 3. Complications were 1 deep infection, 2 ectopic bone formation, 1 intraarticular hardware, and 1 chondrolysis. 4. In the treatment of displaced acetabular fractures, careful initial assessment using radiograph, angiogram and 3-D CT, appropriate selection of surgical approach and accurate surgical clinical outcome and minimize the complication rate.
- 392 View
- 0 Download

- Complications of Interlocking Intramedullary Nailing for the Humeral Shaft Fractures
- Choong Gil Lee, Jin Woo Kwon, Kyoung Tae sohn, Seung Ho Shin, Jong Cheon Park
- J Korean Soc Fract 1998;11(2):254-261. Published online April 30, 1998
- DOI: https://doi.org/10.12671/jksf.1998.11.2.254
-
 Abstract
Abstract
 PDF
PDF - Locked intramedullary nailing has been used as a popular method in treating humeral shaft fracture because of relatively less invasive procedure, good stability and allowing early rehabilitation. However many problems such as rotator cuff injury, iatrogenic fracture, difficult distal locking at operation and painful limitation of shoulder motion due to protrusion of the nail above the greater tuberosity, frequent delayed or nonunion were reported. We reviewed our experience with 26 cases of humeral shaft fractures that were treated by interlocking intramedullary nailing to evaluate the pitfalls and the complications of this technique. the results were as follows. 1. In five cases(19.2%) iatrogenic fractures occured during nail insertion. Three were in the site of inlet and two were in the original fracture site. 2. In four cases(15.4%) painful limitation of shoulder motion was persisted for 2 months. Two were caused by subacromial impingement due to nail protrusion and two were by intraoperative rotator cuff injury. 3. Nonunion occured in two cases(7.7%) which were middle one third transverse fractures and were not fixed with distal locking screws. 4. Intraoperative and postoperative complication rate was 42.3%.
- 489 View
- 1 Download

- Complications of Interlocking Intramedullary Nailing for the Humeral Shaft Fracture
- Chung Nam Kang, Jong Oh Kim, Dong Wook Kim, Young Do Koh, Jong Keon Oh, Sang Hun Ko, Seung Wook Jeong
- J Korean Soc Fract 1997;10(3):669-677. Published online July 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.3.669
-
 Abstract
Abstract
 PDF
PDF - Several advantages of intramedullary nails over plates and external fixators have led to an anpansion of the surgical indications for humeral shaft tractures. But, various morbidities due to proximity of several important structures, such as rotator cuff and radial nerve, follwed the operation. We reviewed our experience with 23 cases of humeral shaft fractures that were treated by interlocking intramedullary nailing to evaluate the pitfalls and the complications of this technique. Fifteen men and 8 women were followed for average 19.5 months. Twenty one (91.3%) of them had midshaft fractures. According to AO/ASIF classification, type A was most common(60.9%), and followed by type B(26.1%) and type C(13.O%). Eighteen of them had associated injuries - 5 radial nerve palsies, 1 Volkmans ischemic contracture, and 14 had fracture of other sites. Indications for interlocking intramedullary nailing were unsatisfactory reduction after closed reduction, fracture of the ipsilateral upper extremity, segmental fractures, and multiple injuries. The operation was performed average 6.7 days after injury. The final results were evaluated with radiographs for quality of union and with physical examination for functional status of the shoulder. There were four cases of complication associated with increase morbidity. A post operative radial verve palsy, associated with the distal interlocking screw fixation was developed due to inappropriately short nail insertion. And in one case, fracture healing was delayed due to distraction of the fracture gap after nailing. In another case subacromial impingement was developed secondary to protruded nail tip because the length was thought be the common underlying causative factor. Finally there was a case of iatrogenic fracture at the site of distal interlocking screw fixation and it was thought to be a technical problem. The results gave us the conclusion that inappropriate nail length was the common underlying causative factor of the complications. Therefore in the interlocking IM nailing for the humeral shaft fractures, accurate measurment of nail length is one of the most cirtical factor for the good final result.
- 385 View
- 1 Download

- Treatment and Complications of Lateral Humeral Condylar Fractures in Children
- Young Bae Pyo, Sang Ho Ha, Byoung Ho Lee, Gyoo Bum Cho
- J Korean Soc Fract 1997;10(1):188-194. Published online January 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.1.188
-
 Abstract
Abstract
 PDF
PDF - In dealing with lateral humeral condylar injuries, the chance of having a poor functional result with inappropriate management is much greater. Therefore, careful attention in treatment is required in order to reduce additional damage caused by excessive manipulation and firm internal fixation with accurate anatomical reduction is recommended for the prevention of complications even if displacement is not severe. The authors analyzed 29 fractures of the lateral condyle of humerus in children who were treated from Jan. 1990 to Dec. 1994. The results were as follows ; 1. All of fractures were Milch type II and Jakobs stage II was most common in 14 cases(48.3%). 2. They were treated with cast immobilization in 5 cases(17.2%), with percutaneous K-wires pinning in 5 cases(17.2%) and with open reduction and internal fixation in 19 cases(65.5%). 3. The complications were 12 cases of bony spur, 8 cases of bony overgrowth. 2 cases of premature epiphyseal fusion, 1 case of cubitus valgus with extension limitation, 1 case of pin site infection. 4. According to the criteria of Hardacre, we obtained excellent result in 10 cases(34.5%), good result in 17 cases(58.6%) and poor result in 2 case(6.9%).
- 406 View
- 0 Download

- Problems of Interlocking Intramedullary Nailing for Fracture Treatment
- Bu Hwan Kim, Jong In In, Yi Chul Kim
- J Korean Soc Fract 1997;10(1):142-149. Published online January 31, 1997
- DOI: https://doi.org/10.12671/jksf.1997.10.1.142
-
 Abstract
Abstract
 PDF
PDF - With the introduction of image intensifier in orthopaedic surgery, interlocked intramedullary nailing is one of the most prevailing method in the treatment of long bone fracture especially in femur and tibia. Advantages of this method are rigid fixation of fracture fragment resistant to rotational force, low infection rate, possible early post-operative motion and weight bearing and bone graft effect by medullar reaming procedure. But we had encountered variable complications during and after operation of 63 cases in 59 patients who had undergone interlocking nailing for femur or tibia fractures from Mar 1990 to Feb 1992 at Dae Dong General Hospital. The results were as follows : 1. Delayed union and nonunion developed in nine cases and infection was noted in nine cases, seven of them were superficial infections. 2. Operative complication were encountered with four cases of new fracture, three cases of angolation deformity, four cases of shortening. 3. Four cases of nail profusion was developed because of inadequate implant length. Postoperative metallic failure was found in three cases. 4. Sufficient preoperative planning and skillful technique can decrease the complications.
- 376 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


