Search
- Page Path
- HOME > Search
Original Articles
- Three-dimensional computed tomography-based differentiation of engaged versus displaced intertrochanteric fractures using the anterior fracture line: a cross-sectional study from Korea
- Jae-Suk Chang, Jin Yeob Park, Sang-Ok Chun, Chul-Ho Kim
- J Musculoskelet Trauma 2026;39(1):30-37. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00318
-
 Abstract
Abstract
 PDF
PDF - Background
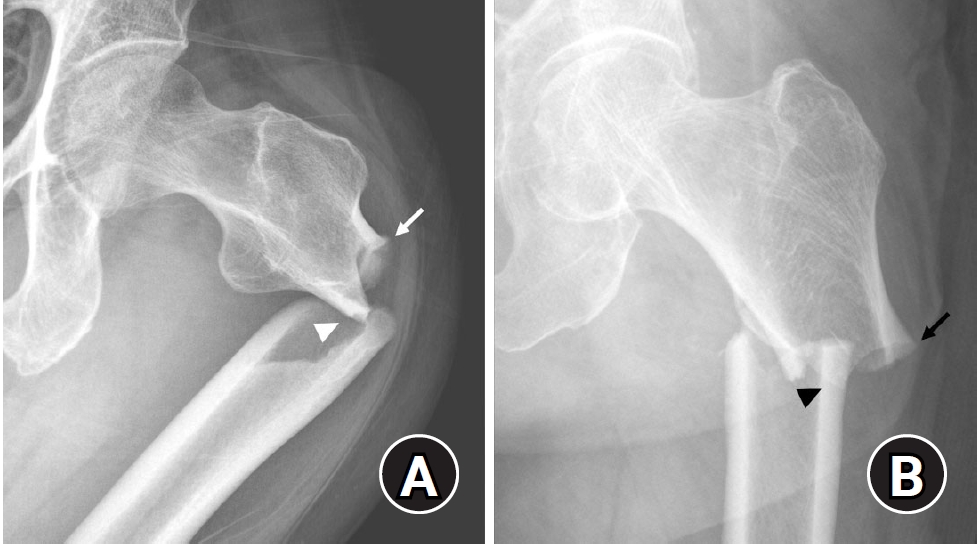
With the advent of an aging society, osteoporotic fractures—particularly hip fractures—are increasing, with a 1-year mortality rate of 17%. Achieving stable fixation that enables early ambulation is essential but remains challenging because complex intertrochanteric (IT) fracture patterns are often underestimated on plain radiographs. Using three-dimensional computed tomography (3D-CT), this study analyzed whether the anterior fracture line lies medial or lateral to the IT line and examined its relationship with displacement or distal medullary canal engagement, highlighting the potential influence of the joint capsule and capsular ligaments on fracture morphology and fixation stability.
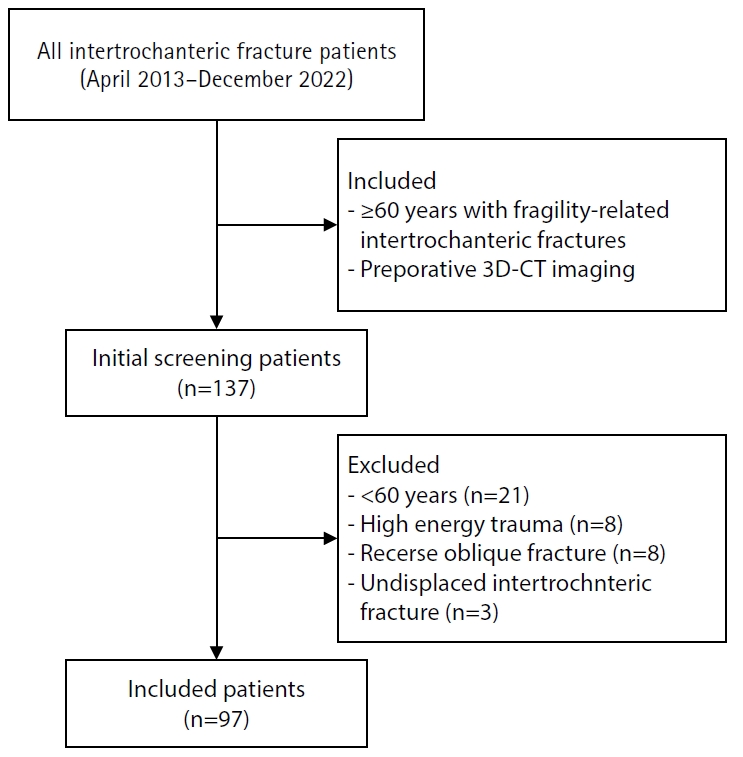
Methods
A retrospective review was conducted on 96 osteoporotic IT fractures in patients aged ≥60 years treated between April 2013 and December 2022 at National Police Hospital and Asan Medical Center, Seoul, Korea. Fractures were classified as engaged, completely displaced, and partially displaced based on 3D-CT findings. The anterior fracture-line position (medial or lateral to the IT line) and the status of the lesser trochanter (LT) were evaluated. The chi-square or Fisher exact test was used for statistical comparisons.
Results
In total, 96 patients were analyzed. Of these, 49 cases (51.0%) were classified as engaged type, 27 cases (28.1%) as completely displaced type, and 20 cases (20.8%) as partially displaced type. When comparing fracture pattern with anterior fracture-line position, the completely displaced type showed a significantly higher proportion of lateral anterior fracture lines than the other two types (P<0.001). However, no significant association was identified between fracture pattern and LT displacement. When the anterior fracture-line position and LT displacement were evaluated together, only the engaged type demonstrated a possible association between a lateral anterior fracture line and LT displacement, though the statistical significance was weak (P=0.047).
Conclusions
Fracture lines lateral to the IT line were strongly associated with displacement in IT fractures; however, their relationship with LT involvement, reflecting iliopsoas tendon traction, was not clearly demonstrated. Although the factors contributing to the engaged-type fracture remain uncertain, the statistical association between fracture pattern and anterior fracture-line position suggests that capsular structures may play a stabilizing role in select fracture configurations. Further studies are needed to clarify these anatomical interactions. Level of evidence:
- 61 View
- 2 Download

- Association between decreased bone mineral density and Pauwels angle in femoral neck fractures: a cross-sectional study
- Soo-Hwan Jung, Yong-Uk Kwon, Ji-Hun Park
- J Musculoskelet Trauma 2026;39(1):20-29. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00269
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Progressive osteoporosis reduces the trabecular structures of the proximal femur, whereas the primary compression trabeculae (PCTs) are relatively preserved. We hypothesize that the loss of the vertically oriented PCTs in osteoporosis, which act as a mechanical barrier, affects fracture line propagation and influences the Pauwels angle. This study investigated the association between bone mineral density (BMD) and Pauwels angles in low-energy femoral neck fractures (FNFs).
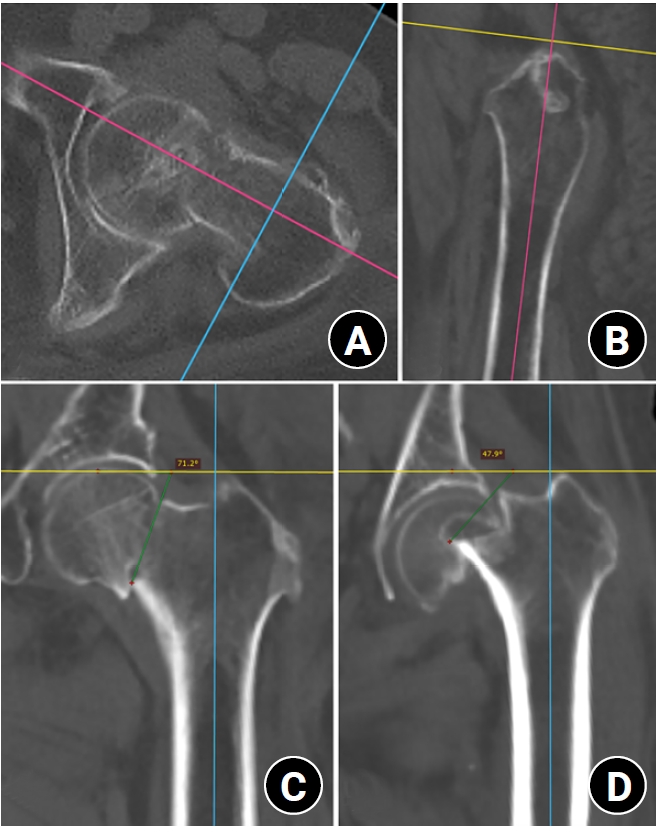
Methods
This cross-sectional study included 150 patients (mean age, 75.3 years; range, 50–94 years) diagnosed with intracapsular FNFs between May 2019 and May 2023. BMD was measured within 1 month of the injury date using dual-energy X-ray absorptiometry, and modified Pauwels angles were assessed using a computed tomography-based multiplanar reconstruction program. Multiple linear regression analysis was performed to evaluate the factors influencing the Pauwels angles. The dependent variable was the Pauwels angle, while the independent variables included sex, age, height, body weight, body mass index, American Society of Anesthesiologists score, Charlson comorbidity index score, smoking status, alcohol use, preinjury walking ability, and femoral neck BMD T-scores.
Results
Higher femoral neck BMD T-scores were significantly associated with increased Pauwels angles (β=3.449, P<0.001). Greater body weight was independently associated with increased Pauwels angles (β=0.213, P=0.007).
Conclusions
The Pauwels angle demonstrated a significant association with BMD, with lower BMD associated with less steep Pauwels angles. In the absence of BMD measurement, the Pauwels angle may indicate osteoporosis severity in patients with low-energy FNFs. Level of evidence: III.
- 70 View
- 3 Download

- Computed tomography plane reformatting to reduce projection error in measuring Pauwels angle of femoral neck fractures: a cross-sectional study
- Gyu Min Kong, Jae-Young Lim, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2026;39(1):38-47. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00038
-
 Abstract
Abstract
 PDF
PDF - Objectives
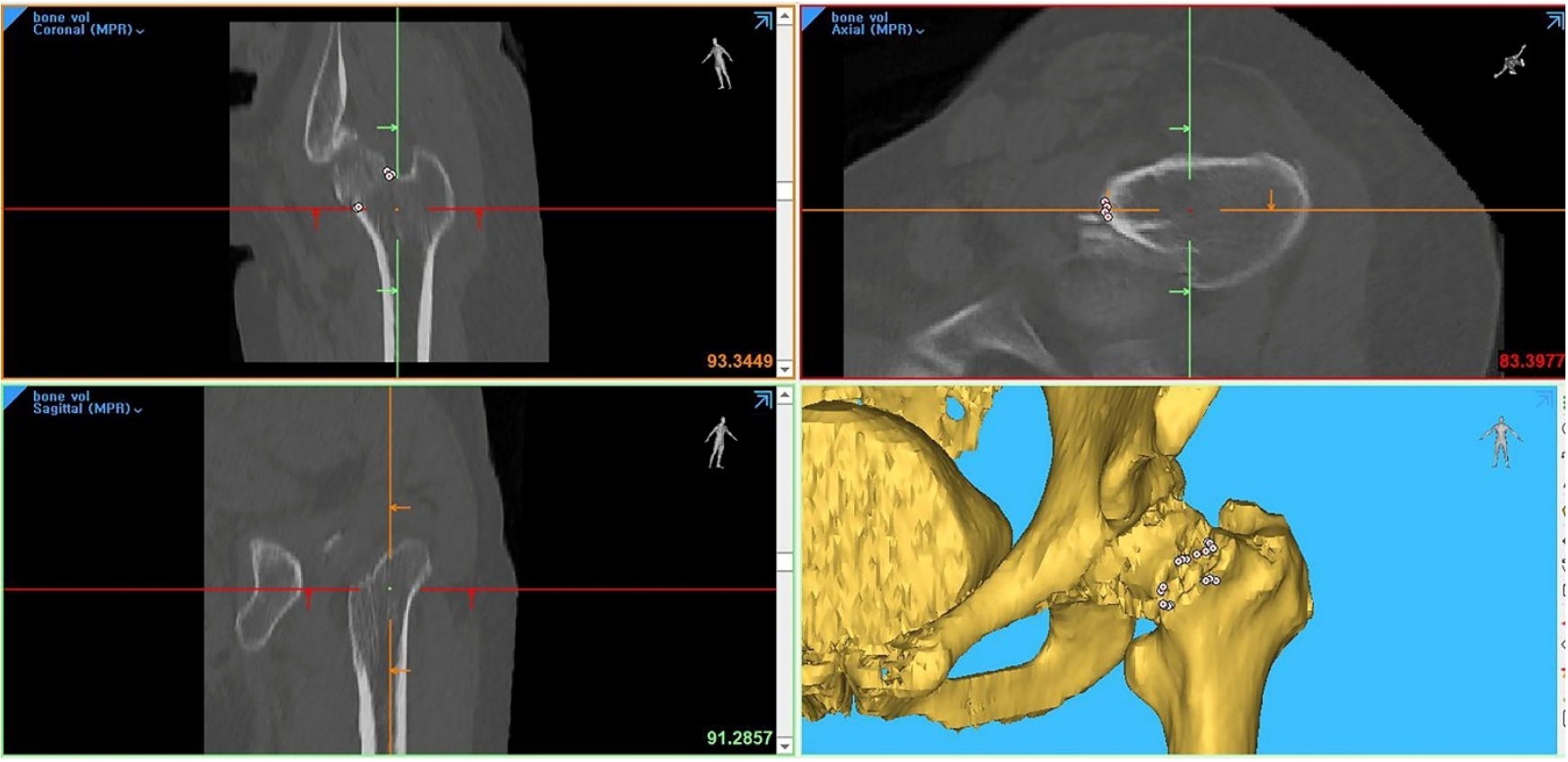
This study aimed to assess fracture verticality in both coronal and axial planes after eliminating projection error in femoral neck fractures among non-older adults, and to demonstrate its clinical utility using computed tomography (CT)-based modeling at actual size.
Methods
This retrospective observational study enrolled 57 patients (30 males and 27 females), aged 20–65 years, with displaced femoral neck fractures. Based on CT images, an actual-size fracture model was constructed. The CT scanning plane was reformatted with the neck-shaft fragment realigned vertically to the ground and parallel to the femoral neck axis. Three consecutive images were used to generate coronal reformats at the centerline and posterior border to measure central and posterior coronal plane verticality as Pauwels’ angle (PA). The central image of the reformatted axial plane was used to assess axial plane verticality. Differences in verticality were analyzed using analysis of variance.
Results
Three coronal morphology types were identified: linear (n=30), concave (n=25), and convex (n=2). Two axial morphology types were observed: cephalad (n=35) and trochanteric (n=22). The mean central PA, posterior PA, and axial verticality were 55.43°±13.79°, 51.44°±11.13°, and 85.74°±18.41°, respectively. Only the central PA showed a significant difference (P<0.001). The PA was significantly higher in the linear coronal type between images (P<0.05) and in the trochanteric axial type (P<0.05).
Conclusions
After reformatting the scanning plane, the central PA showed significant variation between images. Femoral neck fractures of the linear type in the coronal plane and the trochanteric type in the axial plane demonstrated greater verticality than other morphological types. Level of evidence:
- 69 View
- 2 Download

- Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
- Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
- J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00276
-
 Abstract
Abstract
 PDF
PDF - Background
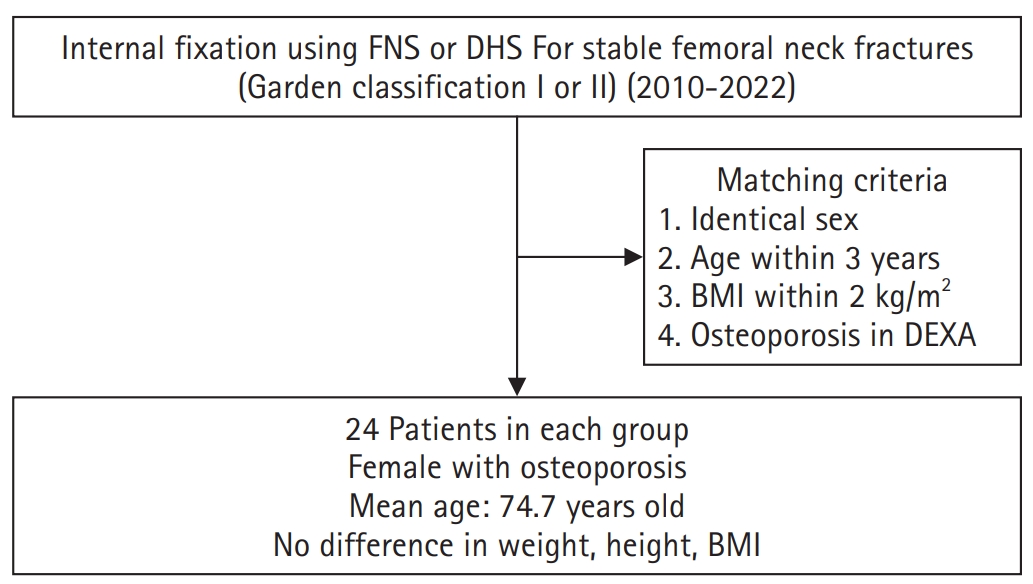
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
Methods
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results. Level of evidence: IV.
- 1,496 View
- 20 Download

- Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
- Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
- J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00157
-
 Abstract
Abstract
 PDF
PDF - Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
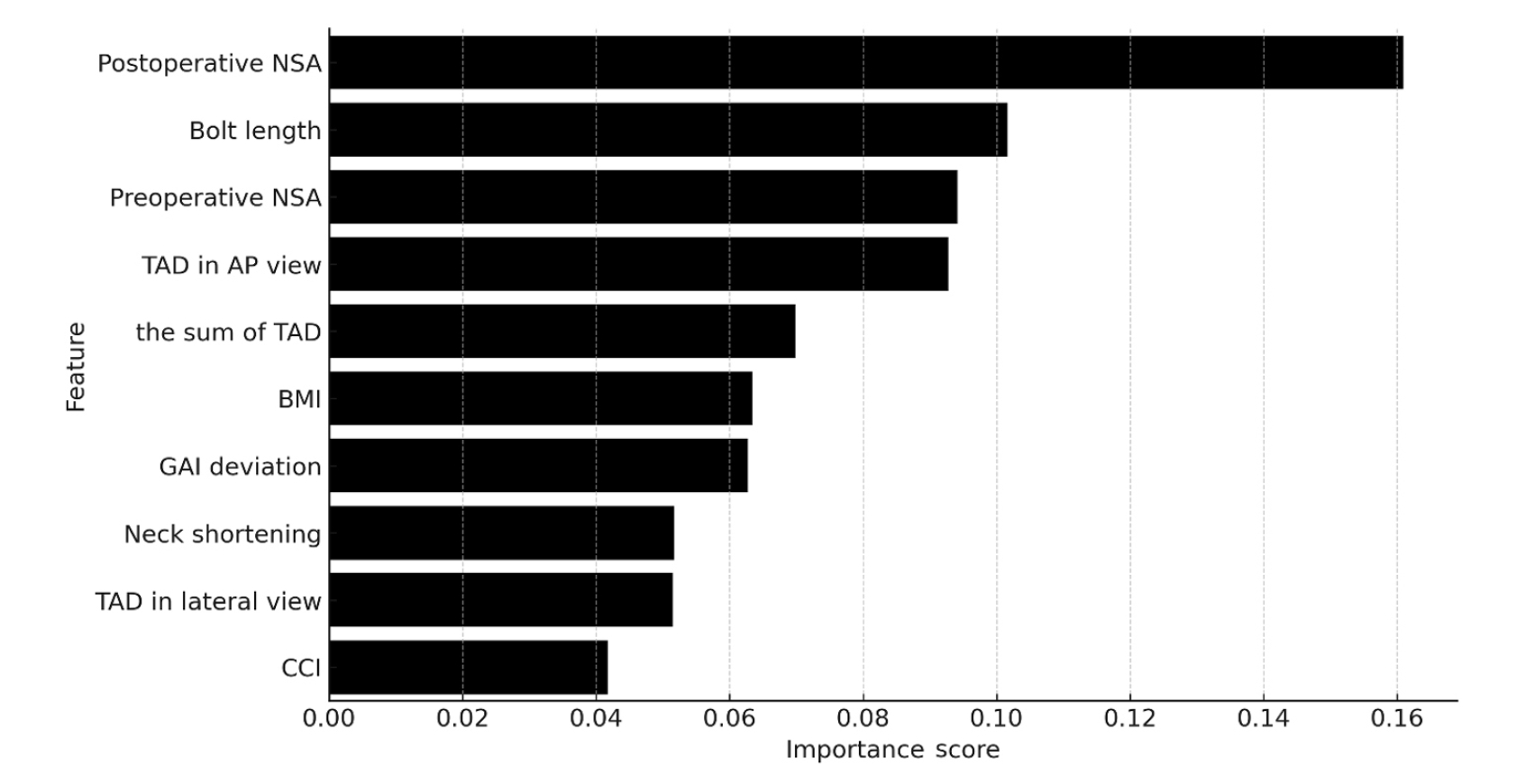
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery. Level of Evidence: III. -
Citations
Citations to this article as recorded by- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
Seonghyun Kang, Wonseok Choi, Jeong Seok Choi, Eic Ju Lim, SungJin Ahn, Jong-Keon Oh, William T. Kent, Whee Sung Son, Jae-Woo Cho
Journal of Orthopaedic Surgery.2026;[Epub] CrossRef
- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
- 1,128 View
- 43 Download
- 1 Crossref

- Lateral marginal fractures of the patella and patellofemoral pain
- Jae-Ang Sim, Chul-Ho Kim, Ji Wan Kim
- J Musculoskelet Trauma 2025;38(3):152-159. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00171
-
 Abstract
Abstract
 PDF
PDF - Background
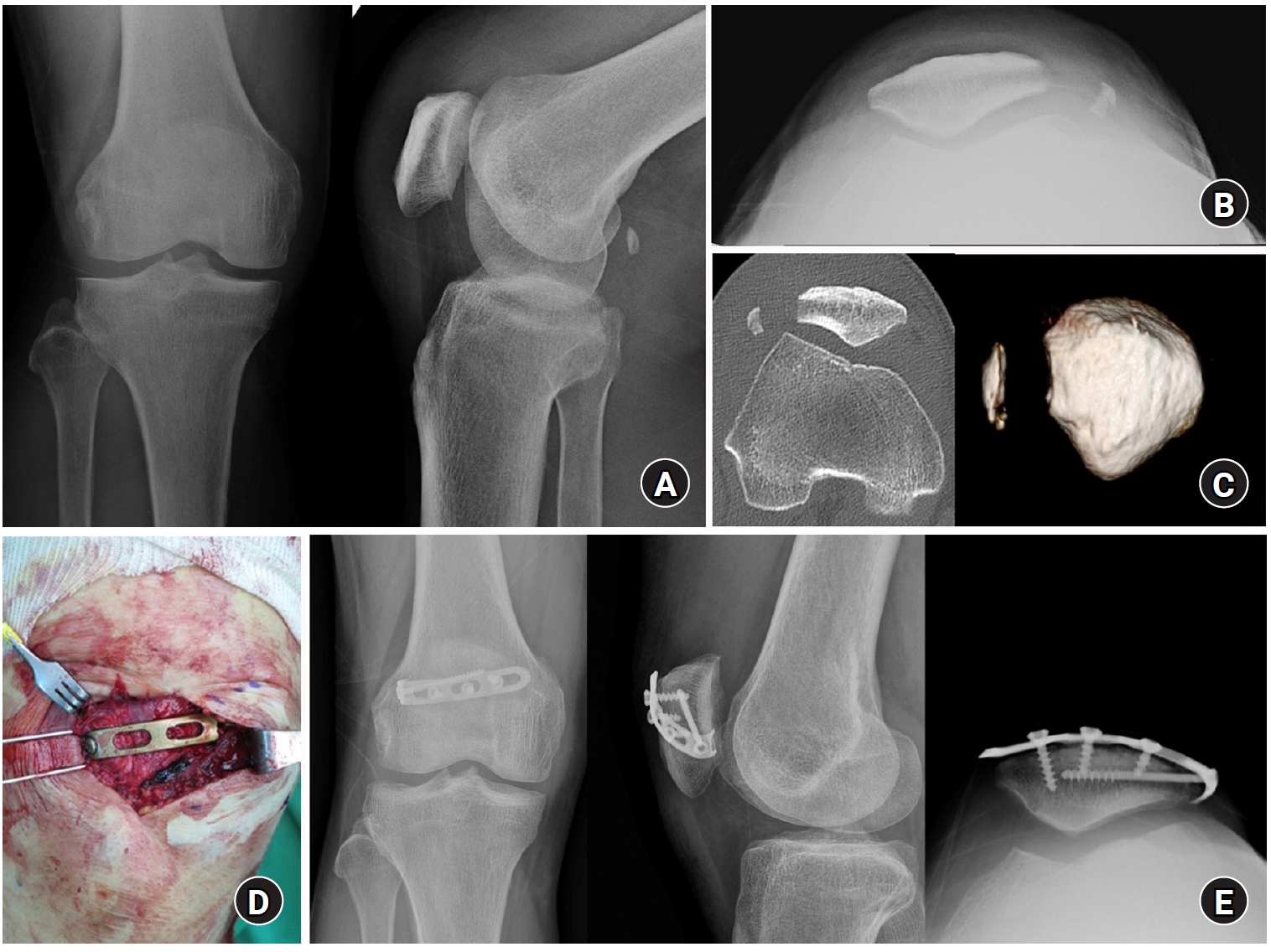
This study investigated the characteristics of lateral marginal fractures of the patella and evaluated the clinical outcomes.
Methods
We retrospectively reviewed all patients with lateral marginal fractures of the patella, defined as a vertical fracture line within 15 mm of the lateral patellar border, from 2008 to 2020. In total, 41 patients were included. Patient characteristics, radiologic findings, and clinical outcomes, including the Lysholm score at 1 year postoperation, were evaluated.
Results
The injury mechanisms were direct in 34 cases and indirect in seven. Furthermore, 85% of patients had a skyline view of the patella at the initial visit, and one medial subluxation of the patella was found. Forty of the 41 patients underwent surgery. Anatomical and nonanatomical (>1-mm displacement or excision) reductions were carried out in 36 cases (88%) and five cases (12%), respectively. The average Lysholm score was 89.1 (range, 67–99). The nonanatomical reduction group had a poorer functional score (79.8 vs. 90.4; P=0.010). Lateral patellar compression syndrome occurred in two patients with nonanatomical reduction.
Conclusions
Lateral marginal fractures of the patella affected patellofemoral stability. Anatomical reduction showed good functional outcomes, while nonanatomical reduction was associated with patellofemoral stability and pain. Therefore, surgeons should perform anatomical reduction with any appropriate fixation method. Level of Evidence: IV
- 1,174 View
- 26 Download

- Biomechanical finite element analysis of a femoral neck system fixation construct for femur neck fractures and clinical implications
- Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):133-142. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00108
-
 Abstract
Abstract
 PDF
PDF - Background
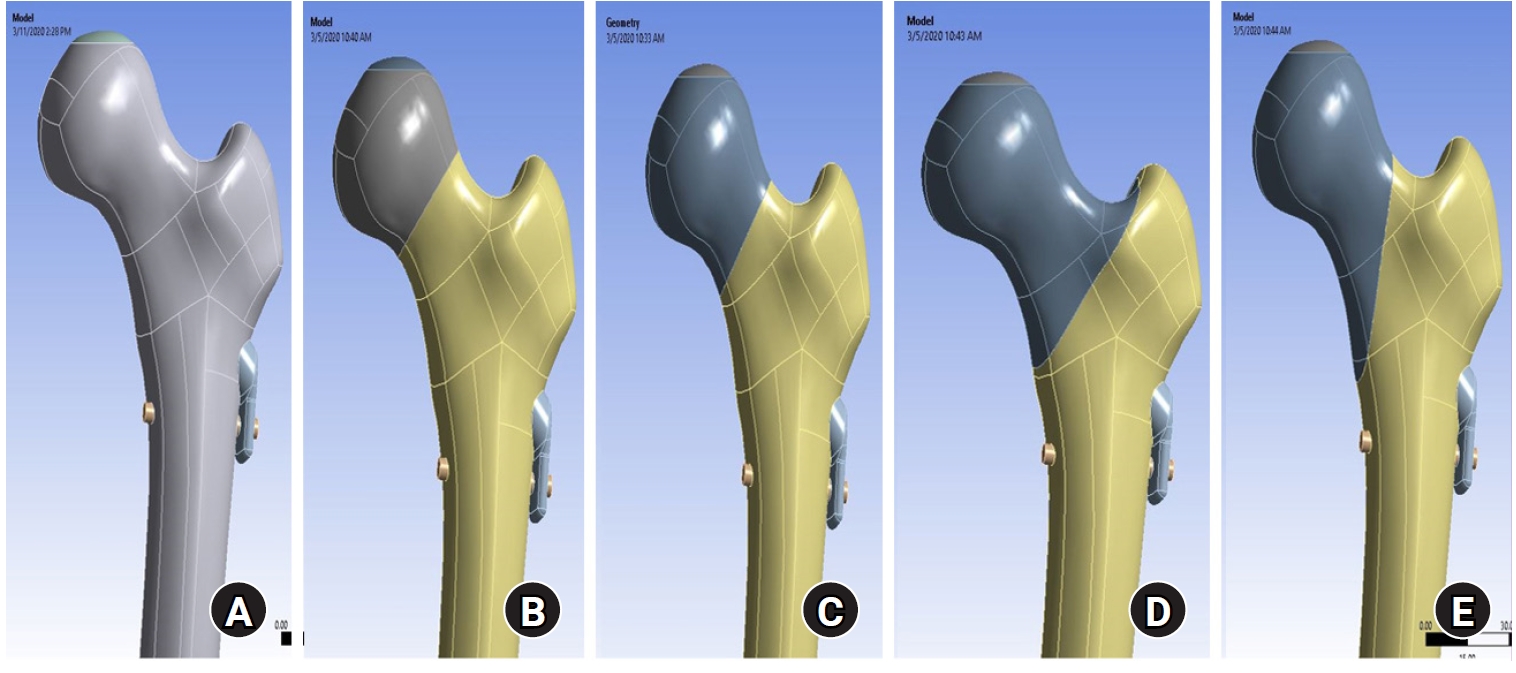
This study assessed the structural/mechanical stability of fixation constructs with a femoral neck system (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications.
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital, 68.56 MPa for a transcervical, 344.54 MPa for a basicervical, and 130.59 MPa for a vertical model. The maximum VMS of FNS was 840.34 MPa for a subcapital, 637.37 MPa for a transcervical, 464.07 MPa for a basicervical, and 421.01 MPa for a vertical model. The stress distribution of basicervical and vertical fractures differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
FNS fixation should be performed with consideration the osseous anchorage in the femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution. Level of evidence: IV.
- 1,816 View
- 82 Download

Review Article
- Atypical femoral fractures: an update
- Won-Tae Cho, Jeong-Hyun Koh, Seungyeob Sakong, Jung-Taek Kim
- J Musculoskelet Trauma 2025;38(2):41-52. Published online March 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00031
-
 Abstract
Abstract
 PDF
PDF - This narrative review provides an up-to-date overview of atypical femoral fractures (AFFs), emphasizing diagnostic criteria, epidemiology, pathophysiology, risk factors, and evaluation with screening strategies. AFFs are rare but significant complications associated with prolonged bisphosphonate (BP) therapy for osteoporosis. Although the pathogenesis of AFFs has not been fully elucidated, its primary mechanism is thought to involve impaired bone remodeling, leading to unhealed microfractures that progress to stress fractures under repetitive loading. AFFs can occur in various regions of the femur, influenced by femoral geometry and the lower limb axis. Other risk factors include prolonged steroid use, arthroplasty, genetic predispositions, and metabolic bone disorders. The diagnosis of AFFs is based on criteria established by the American Society for Bone and Mineral Research. Key radiographic features include lateral cortical transverse fracture lines and localized cortical thickening, typically with minimal or no comminution on the medial cortex. Dual-energy X-ray absorptiometry for screening tests and magnetic resonance imaging as an advanced imaging modality enable the early detection of incomplete fractures. This multi-modal approach facilitates the prompt identification of prodromal cortical changes, reducing the risk of complete fractures in high-risk populations, particularly patients undergoing prolonged BP therapy. Level of Evidence: V
-
Citations
Citations to this article as recorded by- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
Lorenzo Lucchetta, Carmelinda Ruggiero, Samuele Berardi, Alice Franceschi, Michele Bisaccia, Giuseppe Rinonapoli
Journal of Clinical Medicine.2025; 15(1): 25. CrossRef
- Atypical Femur Fractures Without Bisphosphonate Exposure (AFFwB): A Retrospective Report of 21 Cases
- 13,394 View
- 379 Download
- 1 Crossref

Original Articles
- Comparison of Results between Minimally Invasive Plate Fixation and Antegrade Intramedullary Nailing of Recon-Type in Low-Energy Injury Distal Femoral Shaft Fractures
- Hong Moon Sohn, Gwangchul Lee, Ba Rom Kim, Jung Soo Oh
- J Korean Fract Soc 2024;37(2):87-94. Published online April 30, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.2.87
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the outcomes of minimally invasive plate osteosynthesis and antegrade intramedullary nailing for low-energy fracture of the distal femoral shaft.
Materials and Methods
A study was conducted on 30 patients who underwent surgery for low-energy fractures of the distal femoral shaft between January 2016 and April 2022. The study compared 15patients who underwent minimally invasive plate osteosynthesis (Group P) with 15 patients who underwent recon-type antegrade intramedullary nailing (Group N). We evaluated intraoperative blood loss, operative time, C-arm exposure time, bone density, final union status, anatomical reduction, and clinical evaluation. The complications were also examined, and statistical analysis was conducted to compare the two groups.
Results
The blood loss, surgery time, and C-arm time were similar in the two groups. The radiographic assessments and clinical evaluations were also similar in the two groups. The clinical results showed no difference between the groups. Group N had one case of nonunion and one case of delayed union, while Group P had one case of nonunion and one case of peri-prosthetic fracture.
Conclusion
Antegrade intramedullary nailing of the recon-type demonstrated comparable results to minimally invasive plate osteosynthesis. Hence, antegrade intramedullary nailing of the recon-type, which enhances stability by fixing the entire femur and providing additional fixation in the distal portion, is deemed appropriate for treating distal femoral shaft fractures.
- 750 View
- 17 Download

- The Results of Intramedullary Nailing with Sliding Restriction and Dynamization Method in Treating Intertrochanteric Fractures
- Hyun Cheol Oh, Sang Hoon Park, Jae Seok Chae, Han Kook Yoon
- J Korean Fract Soc 2024;37(1):8-14. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.8
-
 Abstract
Abstract
 PDF
PDF - Purpose
To evaluate the results of intramedullary nailing with sliding restriction and dynamization methods in treating intertrochanteric fractures.
Materials and Methods
From August 2016 to March 2019, patients aged 65 years and older who underwent intramedullary nailing in treating intertrochanteric fractures were enrolled in this study. The radiological and clinical results were analyzed in 49 patients who had undergone lag screw sliding re-striction and dynamization of the distal interlocking screw method.
Results
Forty-seven patients achieved union without complications (95.9%). The mean union period was 6.5 weeks (range, 6-9 weeks). Complications occurred in two patients (4.1%), including the cut through of the lag screw in one patient and varus deformity of more than 10° in the other. The preinjury mean Koval grade was 2.8 (range, 1-7). The mean was 3.3 (range, 1-7) at the final follow-up, and the mean difference was 0.5 (range, 0-2).
Conclusion
Intramedullary nailing with a sliding restriction and dynamization method for treating in-tertrochanteric fractures achieved union. The reduction achieved during surgery was maintained with good clinical results. This method is a safe and effective treatment technique for femoral intertrochanteric fractures.
- 616 View
- 12 Download

Review Article
- Osteoporotic Hip Fracture: How We Make Better Results?
- Byung-Chan Choi, Kyung-Jae Lee
- J Korean Fract Soc 2024;37(1):52-59. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.52
-
 Abstract
Abstract
 PDF
PDF - The prevalence of osteoporosis and incidence of osteoporotic fractures is increasing gradually as life expectancy is prolonged and the aged population increases. Osteoporotic hip fractures (femoral neck fractures and femoral intertrochanteric fractures) have high mortality because the patients with these fractures are elderly and have several comorbidities. Thorough preparation and a multidisciplinary approach in the preoperative period are critical, and early surgery is recommended. There are also several principles to treat osteoporotic hip fractures and prevent fixation failures. Many studies have suggested various treatment methods for femoral neck fractures and femoral intertrochanteric fractures. Functional recovery treatment is essential based on the patient’s health and activity levels. Finally, aggressive management of osteoporosis and the prevention of falling is needed to treat osteoporotic hip fractures successfully.
- 610 View
- 24 Download

Original Articles
- Effect of Additional Medial Locking Plate Fixation and Autogenous Bone Graft for Distal Femur Nonunion after Lateral Locking Plate Fixation
- Ho Min Lee, Jong Pil Kim, In Hwa Baek, Han Sol Moon, Sun Kyo Nam
- J Korean Fract Soc 2024;37(1):30-38. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.30
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the outcomes of additional medial locking plate fixation and autogenous bone grafting in the treatment of nonunions that occurred after initial fixation for distal femoral fractures using lateral locking plates.
Materials and Methods
The study involved eleven patients who initially underwent minimally invasive lateral locking plate fixation for distal femoral fractures between January 2008 and December 2020. The initial procedure was followed by additional medial locking plate fixation and autogenous bone grafting for clinically and radiographically confirmed nonunions, while leaving the stable lateral locking plate in situ. A clinical evaluation of the bone union time, knee joint range of motion, visual analog scale (VAS) pain scores, presence of postoperative complications, and functional evaluations using the lower extremity functional scale (LEFS) were performed.
Results
In all cases, bone union was achieved in an average of 6.1 months after the secondary surgery. The range of knee joint motion, weight-bearing ability, and VAS and LEFS scores improved at the final follow-up compared to the preoperative conditions. All patients could walk without walking assistive devices and did not experience pain at the fracture site. On the other hand, three patients complained of pain in the lateral knee joint caused by irritation by the lateral locking plate; hence, lateral hardware removal was performed. One patient complained of mild paresthesia at the anteromedial incision site. Severe complications, such as deep infection or metal failure, were not observed.
Conclusion
For nonunion with stable lateral locking plates after minimally invasive lateral locking plate fixation of distal femur fractures, additional medial locking plate fixation and autogenous bone grafting, while leaving the lateral locking plate intact, can achieve successful bone union.
- 361 View
- 5 Download

- Cephalomedullary Nailing with an Additional Cannulated Screw Fixation in Basicervical Femur Fractures
- Keong-Hwan Kim, Woo Dong Nam, Yeon Sik Heo, Gu-Hee Jung
- J Korean Fract Soc 2024;37(1):22-29. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.22
-
 Abstract
Abstract
 PDF
PDF - Purpose
The purpose of this study is to analyze the clinical results of patients with basicervical fracture undergoing cephalomedullary nailing (CMN) with an additional cannulated screw fixation compared to only performing CMN. We hypothesized that a difference may exist in the clinical outcomes if an ad-ditional screw is fixed with CMN compared to only performing CMN in basicervical fracture.
Materials and Methods
A total of 28 consecutive patients who underwent CMN for basicervical fracture were included. In 9 cases, only CMN was conducted, and in 19 cases, an additional cannulated screw fixation was performed with CMN. Bone union, sliding distance, reduction status, and fixation failure were evaluated by postoperative radiography, and ambulatory ability was evaluated by functional results. These findings were compared between a group of CMN and a group of CMN with an additional cannulated screw.
Results
There were 4 males and 24 females with a mean age of 84 years (range, 69–100 years). No significant difference was found in postoperative reduction, tip-apex distance, bone union, and walking function recovery after surgery between the two groups, but in the sliding distance of the lag screw, the CMN group demonstrated more sliding (6.2 mm [range, 2.5–13.4 mm] vs 3.5 mm [range, 0.1– 9.2 mm]; p=0.045). Among the two groups, only one case of fixation failure at the postoperative four months was observed in the CMN group (p=0.321), and hemiarthroplasty with nail construct removal was performed.
Conclusion
CMN with additional cannulated screw fixation is a safe and reliable surgical option in basicervical fracture. It provided favorable clinical outcomes and may be a good alternative for treating basicervical fracture.
- 1,160 View
- 14 Download

- Bone Union Time of Simple Distal Femur Fractures in the Elderly according to Fracture Gap after Treated with Minimally Invasive Plate Osteosynthesis
- Young Ho Cho, Sangwoo Kim, Jaewook Koo
- J Korean Fract Soc 2023;36(4):133-138. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.133
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the difference in bone union time according to the fracture gap after minimally invasive plate osteosynthesis (MIPO) for simple distal femoral fractures in elderly patients.
Materials and Methods
From January 2010 to December 2019, patients aged 60 years or older who underwent surgical treatment for distal femoral fractures due to a low-energy injury were investigated retrospectively. Forty patients were enrolled in the study. The patients were divided into two groups according to the fracture gap after reduction: no more than 2 mm (Group A) and more than 2 mm (Group B) in the anteroposterior and lateral plane. The demographic, operation time, presence or absence of cerclage wiring, plate screw density, plate span ratio, plate length, bone union period, non-union, and complications were evaluated.
Results
No statistical differences in operation time, cerclage wiring, plate screw density, plate span ratio, and plate length were observed between the two groups, and the bone union was achieved in all patients without complication. The bone union period was 17.24±1.48 weeks in Group A and 24.53± 5.20 weeks in Group B, which was statistically significant (p<0.001).
Conclusion
The bone union time in treating geriatric simple distal femur fractures using the MIPO tech-nique was significantly shorter in the 2 mm or less fracture gap than in the greater than 2 mm group.
- 713 View
- 5 Download

- Risk Factors of Fixation Failure in Femoral Neck Fractures
- Sung Hyun Yoon, Kyu Beom Kim, Hyung Jun Lee, Kyung Wook Kim
- J Korean Fract Soc 2023;36(4):118-124. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.118
-
 Abstract
Abstract
 PDF
PDF - Purpose
Internal fixation after a femoral neck fracture (FNF) is one of the conventional treatment options for the young and active elderly patients. However, fixation failure of internal fixation is a probable complication. The treatment of fixation failure after a primary internal fixation of the FNF remains a challenge.
Materials and Methods
Between July 2002 and March 2017, 83 patients who underwent internal fixation after FNF were retrospectively analyzed. Radiological assessments, including Pauwels’ angle, fracture level, reduction quality, and bone union, were measured, preoperatively and postoperatively. Moreover, intraoperative variables such as time to surgery, surgical time, and estimated blood loss were also evaluated.
Results
The patients were divided into the fixation failure and the non-failure groups. Among the 83 patients, 17 cases (20.5%) of fixation failure after the primary internal fixation of the FNF were identi-fied. When comparing the two groups according to the radiographic data, Pauwels’ angle and the reduction quality based on Garden’s angle showed significant differences (p<0.001). Moreover, when comparing the intraoperative variables, unlike the surgical time and estimated blood loss, significant differences were noted in the time interval from injury to surgery and specifically in whether the surgery was performed within 12 hours after injury (p<0.001).
Conclusion
Pauwels’ angle, reduction quality, and time to surgery are the major factors that can predict the possibility of internal fixation failure of the FNF. Early and accurate anatomical reduction is needed to decrease complications after the internal fixation of the FNF.
- 2,525 View
- 29 Download

- Comparison of Clinical Outcomes for Femoral Neck System and Cannulated Compression Screws in the Treatment of Femoral Neck Fracture
- Jae Kwang Hwang, KiWon Lee, Dong-Kyo Seo, Joo-Yul Bae, Myeong-Geun Song, Hansuk Choi
- J Korean Fract Soc 2023;36(3):77-84. Published online July 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.3.77
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the clinical and radiological results of the femoral neck system (FNS) and cannulated compression screws (CCS) for the fixation of femoral neck fractures.
Materials and Methods
Patients who underwent FNS or CCS internal fixation for femoral neck fractures between January 2016 and January 2022 were analyzed retrospectively. The hip joint function using the Harris hip score (HHS) was evaluated three months and one year after surgery. The operation time, fracture healing time, and associated surgical complications in the two groups were compared and analyzed statistically.
Results
Seventy-nine patients were categorized into 38 FNS and 41 CCS groups. The FNS group had a longer operation time and higher postoperative HHS at three months (p<0.01). Femoral neck shortening was lower in the FNS group (p=0.022). There were no significant differences in the fracture healing time and other complications.
Conclusion
There were no differences in most clinical outcomes and complications between the two groups except for the three-month HHS and femoral neck shortening. This study suggests that FNS could be an alternative to CCS for treating femoral neck fractures.
- 898 View
- 18 Download

Technical Note
- Usefulness of Reduction and Internal Fixation Using a 2.4 mm Hand Plating System in Type AO 33-A3 Distal Femur Fracture - Technical Note -
- Bong-Ju Lee, Ja-Yeong Yoon, Seungha Woo
- J Korean Fract Soc 2023;36(1):25-28. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.25
-
 Abstract
Abstract
 PDF
PDF - Open reduction in an AO 33-A3 class distal femur transverse and comminuted fracture is often difficult due to frequent reduction loss during surgery, leading to longer operative time and increased blood loss intra-operation. In this study, the authors report a case in which the use of an offset grid plate (OsteoMed, USA) using 2.4 mm HPS (hand plating system) eased the process of fracture reduction and achieved a stable internal fixation, ultimately leading to successful osteosynthesis. The authors experienced no need for temporary fixation devices such as K-wires or screws, which are otherwise required to stabilize the reduction. The fracture reduction was stable throughout the primary fixation of the fracture using a locking plate and screws. The authors report that the advantage of the HPS plate is fitting into the cortical contour and providing stable maintenance of fracture reduction intra-operation, which would be beneficial in certain distal femoral fracture patterns.
- 507 View
- 9 Download

Original Articles
- Distal Femur Fractures Treated with Distal Femoral Locking Plate Fixation: A Retrospective Study of One Year Mortality and Risk Factors
- Kwang-Hwan Jung, Yoon-Seok Youm, Seung-Hyun Jung, Jae-Min Oh, Ki Bong Park
- J Korean Fract Soc 2023;36(1):10-16. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.10
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the one-year mortality after locking plate fixation for distal femur fractures and the risk factors related to death.
Materials and Methods
From July 2011 to June 2020, 128 patients who underwent locking plate fixation for distal femur fractures were analyzed retrospectively. Epidemiologic information of the patients, characteristics related to fracture and surgery, and death were investigated. The risk factors related to death were investigated using Cox analysis, and a subgroup analysis was also performed based on the age of 65 years.
Results
The one-year mortality rate after locking plate fixation for distal femur fractures was 3.9%, and the mortality rates in patients younger than 65 years and older than 65 years were 0% and 6.7%, respectively. There were no significant risk factors related to death in the total population. On the other hand, in patients aged 65 years or older, however, high-energy fracture and high comorbidity index increased the risk of death after surgery by 6.9-fold and 1.9-fold, respectively.
Conclusion
The one-year mortality rate for the total patients was 3.9%, but the mortality rate for patients over 65 years of age increased to 6.7%. High-energy fractures and high comorbidity index were risk factors related to death after surgery for distal femur fractures in patients aged 65 years or older.
- 485 View
- 3 Download

- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
- Ju-Yeong Kim
- J Korean Fract Soc 2023;36(1):1-9. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
To identify the biomechanical features for clinical applications through a computational simulation of the fixation of the Femoral Neck System (FNS) with additional cannulated screws for a Pauwels type III femoral neck fractures.
Materials and Methods
Thirty cadaveric femurs underwent computed tomography, and the images were transferred to the Mimics ® program, resulting in three-dimensional proximal femur models. A three-dimensional scan of the FNS and 6.5 mm and 7.0 mm cannulated screws was performed to enable computerized virtual fixation of FNS with additional cannulated screws for unstable femoral neck fractures. Furthermore, the cannulated screw used for additional fixation was modeled and used as a cylinder within the Ansys program. The biomechanical characteristics of these models were investigated by applying a physiological load virtually.
Results
The maximum von Mises stress value at bone was 380.14 MPa in FNS and 297.87 MPa in FNS+7.0 mm full-thread cannulated screw. The maximum von Mises stress value at FNS was 786.83 MPa in FNS and 435.62 MPa in FNS+7.0 mm full-thread cannulated screw. The FNS group showed the highest maximum von Mises stress values at bone and FNS. For total deformation, the maximum deformation value was 10.0420 mm in FNS and 9.2769 mm in FNS+7.0 mm full-thread cannulated screws. The FNS group represented the highest maximum deformation compared to the other groups.
Conclusion
Considering the anatomical spatiality and biomechanical characteristics of the FNS in unstable femoral neck fractures, when one 7.0 mm full thread cannulated screw was also fixed to the anterosuperior portion of the FNS, significant biomechanical stability was demonstrated.
- 714 View
- 10 Download

- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- Min Sung Kwon, Young Bok Kim, Gyu Min Kong
- J Korean Fract Soc 2022;35(4):162-168. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.162
-
 Abstract
Abstract
 PDF
PDF - Purpose
Trochanteric fixation nail advanced (TFNA) was modified to compensate for the shortcomings of proximal femoral nail antirotation-II (PFNA-II). The clinical and radiological outcomes of surgeries us-ing the PFNA-II and TFNA for femoral intertrochanteric fractures were compared.
Materials and Methods
Eighty-two patients who underwent surgeries using PFNA-II or TFNA were analyzed. Only those who were followed up for more than a year were enrolled. Bone union, shortening of the femoral neck, and the tip–apex distance of the intramedullary nail were compared in the radiological findings. Clinical outcomes, including the frequency of complications and gait ability (Koval score), were also assessed.
Results
The mean follow-up periods were 22 and 19 months for the PFNA-II and TFNA groups, re-spectively. In the PFNA-II group, two cases of femoral head cut-out and one case of varus collapse were observed. In the TFNA group, only one case of femoral head cut-out was observed; however, there was no significant difference in the frequency of complications between the two groups (p=0.37). Ad-ditionally, both the shortening of the femoral neck and the decrease in gait ability after surgery showed relative improvement in the TFNA group compared to the PFNA-II group; however, there was no sig-nificant difference between the two groups.
Conclusion
The use of both TFNA and PFNA-II was associated with satisfactory outcomes. In patients who underwent surgeries using TFNA, the recovery of gait ability, frequency of complications, and short-ening of the femoral neck were not significantly different from PFNA-II, suggesting that both are suitable instrument choices for intertrochanteric fracture treatment. However, the clinical significance must be further assessed using a larger group of patients over a longer follow-up period in future studies. -
Citations
Citations to this article as recorded by- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
Jee Young Lee, Gyu Min Kong
Journal of Orthopaedic Trauma.2025; 39(7): 352. CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef
- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
- 3,385 View
- 53 Download
- 2 Crossref

- Intra-Articular Alterations after Suprapatellar Nailing in Tibial Shaft Fractures: An Arthroscopic Evaluation
- GwangChul Lee, Sung Hun Yang, Sung Min Jo, Jeong Min Kook
- J Korean Fract Soc 2022;35(4):129-134. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.129
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study attempted to study the intra-articular changes due to intramedullary nailing through the suprapatellar approach by evaluating the joint cartilage damage and presence of foreign bodies through a comparison of the pre- and post-operative status evaluated by knee arthroscopy.
Materials and Methods
This retrospective study analyzed fifteen patients who underwent intramedullary nailing through the suprapatellar approach for proximal tibial shaft fracture from January 2017 to March 2020. The condition of the joint cartilage and the presence of foreign substances in the patellofemoral joint were evaluated. The cartilage status of the patellofemoral joint was evaluated using the International Cartilage Repair Society (ICRS) grading system. Data from the ICRS grading and the visual analogue scale (VAS) scores of the femoral and patellar cartilage were compared to each independent variable surveyed.
Results
All the intra-articular structures before nailing were normal. In all cases after nailing, articular cartilage damage of the patellofemoral joint and intra-articular debris were observed. The average VAS score was 0.6 (0-1) before surgery and 2.27 (0-4) after surgery. There were no statistically significant differences except for the correlation in the diameter of the tibia nail and femoral ICRS grade (p=0.001) and the damage to the cartilage was greater in the femoral cartilage than that to the patella (p=0.001).
Conclusion
Intra-articular damage appears to be unavoidable in suprapatellar nailing. Further research is needed on the long-term effects of intra-articular damage and on methods to reduce this damage.
- 449 View
- 10 Download

Case Report
- Insufficiency Fracture of Simultaneously Bilateral Femur Neck in Patient Treated with Long-Term Bisphosphonate Treatment - A Case Report -
- Seong Kee Shin, Hyung Gon Ryu, Dae Won Shin, Beom Su Han
- J Korean Fract Soc 2022;35(3):109-113. Published online July 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.3.109
-
 Abstract
Abstract
 PDF
PDF - Bisphosphonate is used widely for osteoporosis management. On the other hand, some studies have reported that prolonged use of bisphosphonate without a proper resting period can cause insufficiency fracture and, in rare cases, fractures on the femur neck. This paper reports a case of an elderly patient who suffered bilateral femur neck insufficiency fractures induced by non-stopped long-term bisphosphonate therapy. The patient complained of pain in her buttocks at the first visit. During the admission period, inguinal area pain newly developed. Both a femur neck insufficiency fracture was observed on the hip radiographic image. Hip pinning and postoperative parathyroid hormone treatment were performed. The patient was discharged without specific complications and reported improvement in symptoms on the last follow-up. Several authors have reported one-sided femoral neck insufficiency fractures due to bisphosphonate use, but the present case is uncommon in that it occurred simultaneously in both femur necks. In addition, in the case of bilateral femur fractures, the walking ability after surgery is lower than that of one-sided fracture cases, so active rehabilitation is necessary.
- 523 View
- 2 Download

Original Article
- Mortality-Related Risk Factors in Total Hip Arthroplasty for Femoral Neck Fractures in Elderly Patients
- Jae Sung Suh, Hyung Gon Ryu, Young Ju Roh, Dae Won Shin
- J Korean Fract Soc 2022;35(2):51-56. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.51
-
 Abstract
Abstract
 PDF
PDF - Purpose
Total hip arthroplasty (THA) using dual mobility components (DMC) is a reasonable surgical option for displaced femoral neck fractures in elderly patients, resulting in lower dislocation rates and improved stability. The purpose of this study was to investigate the clinical outcomes and risk factors responsible for mortality in elderly patients who were diagnosed with a displaced femoral neck fracture and had undergone DMC-THA.
Materials and Methods
Out of 147 cases of THA from December 2018 to June 2020, a total of 79 cases were enrolled in this study, with the following characteristics: (1) Garden stage III or IV, (2) over 75 years of age, and (3) over 1 year of follow-up. All the patients received DMC-THA surgery using the anterolateral approach.
Results
The mean follow-up period was 15.0±8.43 months and a total of one dislocation case was observed. The mortality rate was 17.7% (14/79), and it was especially higher in patients with a past medical history of malignancy (odds ratio [OR]=7.18, p=0.03) or a cognitive disorder such as dementia (OR=5.48, p=0.03). Preoperative low initial hemoglobin levels (OR=0.65, p=0.04) and low UCLA (Uni-versity of California at Los Angeles) score (OR=0.47, p=0.02) were also associated with mortality.
Conclusion
When considering THA as a treatment approach in elderly patients with a displaced femoral neck fracture, a high mortality rate is expected in patients with low preoperative hemoglobin levels or a history of malignancy or cognitive disorders. Hence, thorough monitoring and management should be undertaken before and after surgery. -
Citations
Citations to this article as recorded by- Comparison of Operation Time, Vital Signs, Bleeding Tendency, and Recovery Time Based on Anesthesia Methods in Patients Undergoing Hip Fracture Surgery
Je Bog Yoo, Woo Young In, Chang Ok Pyo, Jeung Hee Kwon, Min Ji Lee, Kwang Hee Kim, Kyoung Ok Kim, Mi Yu
Journal of PeriAnesthesia Nursing.2025;[Epub] CrossRef
- Comparison of Operation Time, Vital Signs, Bleeding Tendency, and Recovery Time Based on Anesthesia Methods in Patients Undergoing Hip Fracture Surgery
- 404 View
- 26 Download
- 1 Crossref

Case Report
- Recurrent Treatment Failure in Vancouver Classification Type C Periprosthetic Fractures around a Well Fixed Short Femoral Stem
- Byeong Yeol Choi, Hong-Man Cho, Jiyeon Park
- J Korean Fract Soc 2022;35(1):16-20. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.16
-
 Abstract
Abstract
 PDF
PDF - A short femoral stem (type 1 cementless stem) is being increasingly used to perform total hip arthroplasty; however, various types of intra- or postoperative periprosthetic fractures have been reported in recent times. A 66-year-old woman with a history of bilateral total hip arthroplasties using a type 1B femoral stem was admitted 2 months post-operation for a Vancouver type C periprosthetic fracture. She underwent open reduction and internal fixation; however, we observed recurrent non-union and plate breakage at the same site. In this case report, we discuss the factors associated with treatment failure in patients with a Vancouver type C periprosthetic fracture following type 1 femoral stem im-plantation.
- 344 View
- 0 Download

Original Articles
- Surgical Treatment of AO/OTA 33-C Intra-Articular Distal Femoral Fractures through Parapatellar Approach
- Suk Kyu Choo, Sung Tan Cho, Hyoung Keun Oh
- J Korean Fract Soc 2022;35(1):1-8. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
To report the surgical results of the parapatellar approach for AO/OTA 33-C distal femoral intra-articular fractures.
Materials and Methods
Twenty-one patients with AO/OTA 33-C distal femoral intra-articular fracture were included. There were 11 cases of C2 and 10 cases of C3 fractures. The time of union and the coronal alignment were radiographically investigated. The complications related to surgery were clinically investigated, and a functional evaluation using the range of motion and Oxford knee score was performed to compare the surgical results according to fracture classification.
Results
In all cases, sufficient articular exposure and anatomical reduction were achieved with the parapatellar approach. No cases of coronal malalignment, loss of reduction, and plate failure were noted. On the other hand, in four cases (19.0%), an autogenous bone graft was performed due to delayed union on the meta-diaphyseal fracture site. There were no differences in the radiological and clinical outcomes of the C2 and C3 fractures. The knee joint pain and Oxford knee score were poorer in the delayed union group than the normal union group.
Conclusion
The parapatellar approach is useful for achieving an anatomical reduction of the articular surface of the distal femur and minimally invasive plating technique. Although satisfactory surgical results could be obtained regardless of the degree of articular comminution, a study of the risk factors of delayed metaphyseal fusion may be necessary.
- 491 View
- 5 Download

- Comparing Outcomes of Retrograde Intramedullary Nail and Locking Plate Fixation in Distal Femoral Fractures
- Byung-Ho Yoon, Bo Kwon Hwang, Hyoung-Keun Oh, Suk Kyu Choo, Jong Min Sohn, Yerl-Bo Sung
- J Korean Fract Soc 2021;34(4):131-136. Published online October 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.4.131
-
 Abstract
Abstract
 PDF
PDF - Purpose
We compared the radiological and clinical results of fixation for distal femoral fracture (DFF) using a locking compression plate (LCP) or a retrograde intramedullary nail (RIN).
Materials and Methods
From October 2003 to February 2020, 52 cases of DFF with a minimum 1-year follow-up (with a mean follow-up of 19.1 months) were included: 31 were treated with LCP and 21 with RIN. The operation time, blood loss, and hospitalization period were compared, and the incidence of postoperative nonunion, malunion, delayed union and metal failure and other post-operative complications were evaluated and compared.
Results
There was no significant difference in the operating time between the two groups, but the mean blood loss was significantly higher in the LCP group (LCP 683.5 ml vs RIN; 134.9 ml; p=0.015). In 49 out of 52 cases, bone union was achieved without additional surgery in an average of 6.8 months, and a complete union was achieved after additional surgery in three cases of nonunion (LCP 2 cases vs RIN 1 case; p=0.065). One case of malunion and superficial infection was confirmed in each group.
Conclusion
Internal fixation using LCP and RIN give good outcomes with a low complication rate and can therefore be considered useful surgical treatments for DFF.
- 447 View
- 5 Download

Case Report
- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture
- Soon Ho Huh, Hong-Man Cho, Ji-Yeon Park
- J Korean Fract Soc 2021;34(3):112-116. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.112
-
 Abstract
Abstract
 PDF
PDF - A helical blade type of hip screw is used widely for the operative management of femoral trochanteric fractures. A 73-year-old female patient was admitted for femoral trochanteric fracture AO/OTA type 31A2.2. A helical blade locking sleeve dissembled 18 weeks after surgery did not achieve accurate reduction. The patient underwent bipolar hip hemiarthroplasty because the fracture reduction was lost, and it was impossible to remove the remaining helical blade without bone loss. The authors report this case of a rare complication of helical blade.
- 534 View
- 3 Download

Original Article
- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
- J Korean Fract Soc 2021;34(3):105-111. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.105
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the clinical and radiological outcomes of TFNA (Trochanteric Fixation NailAdvanced; Depuy Synthes) for the treatment of proximal femur fractures.
Materials and Methods
This was a retrospective study of 64 patients diagnosed with a proximal femur fracture from January 2019 to November 2019. The patient’s demographic data, preoperatively and postoperatively Koval grade, modified Harris hip score, EQ-5D (Euro-Qol-5 Dimension), sliding and advancement of the blade, radiologic outcome, and complications were investigated.
Results
Fifty patients were available for evaluation at one year postoperatively. The patients reported the following: the Koval grade decreased after surgery; the modified Harris hip score decreased from 78.56±8.88 to 72.74±6.59 (p=0.149); the mean EQ-5D decreased from 0.75±0.09 to 0.72±0.06 (p=0.000). Satisfactory reduction was achieved on a postoperative radiographic examination in 47 patients in six months. Complications occurred in seven cases.
Conclusion
TFNA is considered an appropriate implant for treating intertrochanteric fractures of the femur with a minimum follow-up of one year. -
Citations
Citations to this article as recorded by- Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
Ramprasad Jasti, Prithvi Mohandas, Mahesh K Ragavan, Sunil D Magadam, Umesh Kannadasan
Cureus.2025;[Epub] CrossRef - GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
Seungcheol Kwon, Minjae Lee, Heeyeon Lee, Jihyo Hwang
Journal of Clinical Medicine.2023; 12(21): 6720. CrossRef - Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef
- Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
- 1,014 View
- 18 Download
- 3 Crossref

Case Reports
- Delayed Pseudoaneurysm of Deep Femoral Artery Caused by Migration of Lesser Trochanter, Subsequent to an Intertrochanteric Fracture Surgery - A Case Report -
- Bum-Soo Kim, Seong-Tae Kim, Seungyup Shin, Chang Geun Yu
- J Korean Fract Soc 2021;34(2):76-79. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.76
-
 Abstract
Abstract
 PDF
PDF - The lesser trochanteric fracture is commonly found amongst intertrochanteric fractures, where pseudoaneurysm of the femoral artery is a rare complication. A pseudoaneurysm could develop due to the penetration injury of the artery by the bone fragment during occurrence of the fracture, or by the insertion of screws during the surgical procedure. Minimal complication is seen when the lesser trochanter is not fixed during the intertrochanteric fracture surgery. However, in the current case, the authors experienced appearance of a delayed pseudoaneurysm of the deep femoral artery caused by migration of the lesser trochanter, which was successfully treated by excision.
- 592 View
- 5 Download

- Injury of the Ascending Branch of the Lateral Femoral Circumflex Artery Caused by a Spike of the Displaced Lesser Trochanter in an Intertrochanteric Femoral Fracture - A Case Report -
- Soon Ho Huh, Hong-Man Cho, Jiyeon Park
- J Korean Fract Soc 2021;34(2):71-75. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.71
-
 Abstract
Abstract
 PDF
PDF - Although vascular injuries associated with femoral intertrochanteric fractures have been reported infrequently, bleeding due to vascular injury can lead to severe complications that can be potentially life and limb-threatening. The authors report a case of an injury of the ascending branch of the lateral femoral convolutional artery in a patient who underwent surgical treatment for a femoral intertrochanteric fracture. Vascular injury occurred due to the sharp margin of displaced lesser trochanter five weeks after surgery. Percutaneous transcatheter embolization was done and improved without additional complications. Therefore, the surgeons need to be aware of possible associated vascular injuries caused by displaced lesser trochanter fragments in femoral intertrochanteric fractures.
-
Citations
Citations to this article as recorded by- Delayed Deep Femoral Artery Injury Secondary to Migrated Lesser Trochanter Fragment After Intertrochanteric Fracture Fixation: A Case Report and Updated Literature Review
Slavko Čičak, Josip Kocur, Vedran Farkaš, Petra Čičak, Stjepan Ištvanić, Marko Lovrić, Marko Perić, Nenad Koruga, Tomislav Ištvanić
Geriatric Orthopaedic Surgery & Rehabilitation.2025;[Epub] CrossRef - Vascular Complications Following Trans-Trochanteric Fracture: Case Report and Literature Review
Robert Bot, Adrian Tirla, Simona Daniela Cavalu
Reports.2025; 8(4): 191. CrossRef
- Delayed Deep Femoral Artery Injury Secondary to Migrated Lesser Trochanter Fragment After Intertrochanteric Fracture Fixation: A Case Report and Updated Literature Review
- 562 View
- 2 Download
- 2 Crossref

Original Articles
- Comparison of Reductions of Left and Right Proximal Portions of Intertrochanteric Fractures Treated by Intramedullary Nailing
- Hyun Cheol Oh, Joong Won Ha, Yung Park, Sang Hoon Park, Han Kook Yoon
- J Korean Fract Soc 2021;34(2):64-70. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.64
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the effect of lag screw insertion on proximal fragments by separating the right and left sides of intertrochanteric fractures in elderly patients that underwent intramedullary nailing.
Materials and Methods
Patients aged ≥65 years that underwent intramedullary nailing after a diag-nosis of intertrochanteric fractures during the period February 2012 to May 2016 were included in the study. The subjects were divided into right and left side groups. The effect of the clockwise rotational force generated when a lag screw was inserted on the proximal fragment was evaluated in both groups.
Results
In the right and left groups, most proximal fragments were located in the intramedullary canal after surgery (45 cases [75.0%] and 67 cases [73.6%], respectively). Clockwise rotation due to lag screw placement in the right group occurred in two cases (3.3%), which both showed internal rotation, and in four cases (4.4%) in the left group, all of which showed external rotation.
Conclusion
After intramedullary nailing of intertrochanteric fractures in elderly patients, proximal fragments were mostly located in the intramedullary cavity. The results obtained confirmed that the clockwise rotational force generated by lag screw insertion did not affect left or right sides. -
Citations
Citations to this article as recorded by- Which side should be taken care of when positioning a lag screw in intertrochanteric femoral fracture: right or left?
Min Uk Do, Kyeong Baek Kim, Sang-Min Lee, Hyun Tae Koo, Won Chul Shin
European Journal of Trauma and Emergency Surgery.2025;[Epub] CrossRef - Midterm Outcomes of Intramedullary Fixation of Intertrochanteric Femoral Fractures Using Compression Hip Nails: Radiologic and Clinical Results
You-Sung Suh, Jae-Hwi Nho, Min Gon Song, Dong Woo Lee, Byung-Woong Jang
Clinics in Orthopedic Surgery.2023; 15(3): 373. CrossRef
- Which side should be taken care of when positioning a lag screw in intertrochanteric femoral fracture: right or left?
- 634 View
- 3 Download
- 2 Crossref

- Comparison of the U-Blade Gamma3 Nail and the Zimmer Natural Nail for the Treatment of Intertrochanteric Fracture
- Jae Sung Suh, Hyung-Gon Ryu, Young Ju Roh, Dae Won Shin, Sang-Min Kim
- J Korean Fract Soc 2021;34(2):57-63. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study was performed to compare the clinical results and radiological follow-up differences between intertrochanteric fractures treated with the U-blade Gamma3 nail or the Zimmer natural nail (ZNN).
Materials and Methods
The medical records of 129 cases diagnosed with an intertrochanteric frac-ture (90 cases of U-blade Gamma3 nail, 39 cases of ZNN) from July 2015 to December 2018 were reviewed. Patients were assigned to a U-blade Gamma3 nail (n=39) or a ZNN (n=39) group. To reduce selective bias, groups were subjected to Propensity score matching by age, body mass index, bone mineral density, and fracture type. Patients that met the following criteria were excluded; age <65 years, non-ambulatory, high energy or pathologic fracture, and a follow-up of <6 months. Operation times, estimated blood losses, preoperative and postoperative Koval grades, Harris hip score and radiological lag screw positions in the femoral head, reduction quality, cut-out, tip-apex distance (TAD), lag screw sliding distances, and times to union were compared.
Results
Clinical results were similar in the two groups, but lag screw TAD was significantly greater in Ublade Gamma3 nail group (23.4 mm vs. 21.0 mm) (p=0.042). One case of cut-out occurred in the Ublade Gamma3 nail group, but no other nail-related postoperative complication was noted.
Conclusion
No significant difference was observed between the outcomes of U-blade Gamma3 nail or ZNN treatments of intertrochanteric fractures. We conclude that the U-blade confers no specific advan-tage.
- 1,394 View
- 8 Download

Review Article
- Pediatric Femoral Neck Fracture
- Joo Hyung Han, Hoon Park
- J Korean Fract Soc 2021;34(1):34-43. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.34
-
 Abstract
Abstract
 PDF
PDF - Pediatric femoral neck fracture is an uncommon injury with a high complication rate, regardless of the appropriate diagnosis and management. The bony anatomy and blood supply of the proximal femur in a skeletally immature patient differ from those in adult patients. Generally, these fractures result from high-energy trauma, but pathologic hip fractures also occur, usually from low-energy trauma. Pediatric femoral neck fractures are categorized using the Delbet classification system. This classification guides management and aids clinicians in determining the risk of avascular osteonecrosis. The ideal surgical treatment is determined by the fracture type and the age of the patient. Reduction, which is achieved using a closed or open procedure, combined with stable fixation and/or cast immobilization, is recommended for most of these fractures. Anatomical reduction within 24 hours from the injury may result in a good surgical outcome. Although the effects of capsular decompression after reduction and fixation have not been established, decompression is easy to perform and may reduce the risk of avascular necrosis. Despite appropriate management, osteonecrosis can occur after all types of pediatric femur neck fractures. Other complications include coxa vara, nonunion, and premature physeal arrest.
- 1,312 View
- 27 Download

Original Articles
- Clinical Outcomes and Radiologic Characteristics of Insufficiency Femoral Neck Fracture in Elderly Patients
- Hee-Uk Ye, Kyung-Jae Lee, Byung-Woo Min, Kyung-Hwan Lim, Beom-Soo Kim, Young-Hoon Kim
- J Korean Fract Soc 2021;34(1):1-7. Published online January 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
In elderly patients, femoral neck insufficiency fractures that occur without a history of trauma are difficult to diagnose and treat, so it is emphasized that early suspicion of fractures and additional diagnostic tests are conducted. Materials and Methods: Between December 2010 to December 2019, 12 femoral neck insufficiency fractures (group 1) were evaluated by comparing them with 50 traumatic femoral neck fractures of a similar age. Along with demographic data, neck cortical thickness, shaft cortical thickness, head diameter, neck width, trochanter width, shaft width, neck-shaft angle, hip axis length, femoral neck index on the simple radiographic image were compared. Results: Seven of the 12 cases were non-displaced fractures, and it took an average of 19.2 days to diagnose the fracture after the symptoms occurred. The height was smaller than the control group at 149.1 cm in group 1 and 157.2 cm in group 2 (p<0.001). The cortical thickness of the medial femoral neck showed significant differences between the two groups: 3.16 mm in group 1 and 4.11 mm in group 2 (p=0.004). There was no statistical difference in the other measurements. Conclusion: Femoral neck insufficiency fracture often has a delayed diagnosis because of the characteristics of the fracture. The cortical thickness of the medial femoral neck in simple radiographic images can help suspect femoral insufficiency fractures in elderly patients when considered with detailed medical history taking and a physical examination.
- 601 View
- 11 Download

- Comparison of the Clinical and Radiographic Results between 125° and 130° Caput-Collum-Diaphyseal Angle Proximal Femoral Nail Anti-Rotation II in Patients with Intertrochanteric Fracture
- Soo Jae Yim, Yong Bok Park, Hyun Kwon Kim, Sin Hyung Park
- J Korean Fract Soc 2020;33(4):210-216. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.210
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the clinical and radiographic results of two proximal femoral nail antirotation II (PFNA-II) angled by 125° and 130° in patients with intertrochanteric fractures.
Materials and Methods
From March in 2015 to September in 2016, 65 patients who underwent a closed reduction and internal fixation with PFNA-II for a femoral intertrochanteric fracture were evaluated retrospectively. The minimum follow-up period was two years. Of those, 30 and 35 patients underwent 125° angled PFNA-II and 130° angled PFNA-II, respectively. The clinical performance was evaluated using the Harris hip score, WOMAC (Western Ontario and McMaster Universities Osteoarthrtis Index), and UCLA (University of California Los Angeles) score. Radiographic analyses were performed using standardized anteroposterior and lateral radiographs to assess the implant position and quality of reduction. The blade length, distance between the blade tip and the tip of the greater trochanter, and distance between the blade tip and the most lateral protrusion point of the greater trochanter in the two groups were measured and compared.
Results
The clinical results, including the Harris hip score, WOMAC, and UCLA, were similar in the two groups at the last follow-up postoperatively. In the radiography evaluation, the implant position, quality of reduction, and the blade length were similar in the two groups. The distances between the blade tip and the tip of the greater trochanter were 52.60±3.53 mm and 58.07±5.54 mm in the 125° angled PFNA-II and 130° angled PFNA-II groups, respectively. The distance between the blade tip and the most lateral protrusion point of greater trochanter were 16.48±2.54 mm and 21.19±4.43 mm in the 125° angled PFNA-II and 130° angled PFNA-II groups, respectively. The differences were significant (p=0.031, p=0.012).
Conclusion
The operation with the 125° angled PFNA-II showed a more superior and lateral position of the blade than that with the 130° angled PFNA-II. Nevertheless, lateral thigh pain can occur when the blade is positioned superolaterally.
- 557 View
- 2 Download

- Risk Factors Affecting the Early Complications of Femoral Head Fractures
- HoeJeong Chung, Jin-Woo Lee, Dong Woo Lee, Hoon-Sang Sohn
- J Korean Fract Soc 2020;33(4):204-209. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.204
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study analyzed the prognostic factors in patients with femoral head fractures by comparing two groups with and without complications.
Materials and Methods
A retrospective study was performed on femoral head fracture patients who visited two different level-1 trauma centers from January 1, 2014 to June 30, 2018. Thirty-three patients with a follow-up period of more than one year were included. Early complications were defined as fair or poor in the Thompson–Epstein clinical evaluation criteria and grades 3 or 4 in the Kellgren– Lawrence classification within one year after the fracture. The patients were divided into two groups, with and without early complications. Statistical analysis was performed for the nominal variables with a Fisher’s exact test and continuous variables using a Mann–Whitney U test.
Results
Nine patients (27.3%) had early complications, and there were no significant differences according to age, sex, treatment method, combined fractures, Pipkin classification, and AO/OTA classification between the two groups.
Conclusion
The prognosis in femoral head fractures is difficult to predict. Therefore, the validation of existing classifications or a new classification is necessary.
- 515 View
- 1 Download

- Treatment of Proximal Femur Fracture with a Newly Designed Nail: Trochanteric Fixation Nail-Advanced (TFNA)
- Jae Youn Yoon, Ji Wan Kim
- J Korean Fract Soc 2020;33(4):189-195. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.189
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the clinical results and implant safety of a newly developed implant, Trochanteric Fixation Nail-Advanced (TFNA; DePuy Synthes), in the treatment of proximal femur fractures.
Materials and Methods
This was a retrospective cohort study of 26 patients diagnosed with proximal femur fracture and treated surgically with TFNA. The patients’ demographic data, surgical data, radiologic findings, and functional outcomes, including complications, were evaluated.
Results
The mean age of the patients was 71.2 years (95% confidence interval [CI], 68.2-74.2); 65.4% were female. The mean Carlson comorbidity index score was 5.4, and the mean Koval grade before fracture was 2.1. Fracture classification included four cases of AO/OTA 31.A1, nine cases of A2, six cases of A3, and seven cases of 32A including six cases of atypical femoral fractures. The mean operating time was 53.3 minutes (95% CI, 43.6-63.1). There were no early postoperative complications, such as postoperative infection, deep vein thrombosis, pulmonary embolism, or in-hospital death, except one case of pneumonia. The mean Koval score at the postoperative six-month follow-up was 2.9. EuroQol-5 Dimension (EQ-5D) increased from 0.05 to 0.54 after three months and 0.72 at six months postoperatively. Bone union was observed in all cases with a mean union time of 12.9 weeks. No implant failure occurred, and no cases required secondary revision surgery.
Conclusion
A new intramedullary nail system, TFNA, showed excellent outcomes and safety in the surgical treatment of proximal femur fractures. -
Citations
Citations to this article as recorded by- Intermediate Length Cephalomedullary Nails in Proximal Femoral Fractures: Review of Indications and Outcomes
Daniel Scott Horwitz, Ahmed Nageeb Mahmoud, Michael Suk
Journal of the American Academy of Orthopaedic Surgeons.2025; 33(19): 1071. CrossRef - Outcomes of Intertrochanteric Fracture Fixation Using the Trochanteric Fixation Nail Advanced (TFNA): A Retrospective Analysis
Ramprasad Jasti, Prithvi Mohandas, Mahesh K Ragavan, Sunil D Magadam, Umesh Kannadasan
Cureus.2025;[Epub] CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef - Prospective randomized multicenter noninferiority clinical trial evaluating the use of TFN-advancedTM proximal femoral nailing system (TFNA) for the treatment of proximal femur fracture in a Chinese population
Lidan Zhang, Zhijun Pan, Xiaohui Zheng, Qiugen Wang, Peifu Tang, Fang Zhou, Fan Liu, Bin Yu, Frankie K. L. Leung, Alex Wu, Suzanne Hughson, Zhuo Chen, Michael Blauth, Anthony Rosner, Charisse Sparks, Manyi Wang
European Journal of Trauma and Emergency Surgery.2023; 49(3): 1561. CrossRef - Risk of shortening in operatively treated proximal femur fractures with cephalomedullary nails with dynamically versus statically locked helical blades
Nathan Cherian, Lasun Oladeji, Cole Ohnoutka, Dan Touhey, Madeline Sauer, Kyle A. Schweser, Mauricio Kfuri, James L. Cook, Gregory J. Della Rocca, Brett D. Crist
Injury.2023; 54(2): 669. CrossRef - GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
Seungcheol Kwon, Minjae Lee, Heeyeon Lee, Jihyo Hwang
Journal of Clinical Medicine.2023; 12(21): 6720. CrossRef - Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef - Analysis of Clinical and Functional Outcomes according to the Blood Sugar Control Status at the Time of Ankle Fractures Resulting from Rotational Injuries
Jun Young Lee, Dong Seop Lim, Seung Hyun Lee, Seo Jin Park
Journal of the Korean Fracture Society.2022; 35(4): 135. CrossRef - Conventional versus helical blade screw insertion following the removal of the femoral head screw: a biomechanical evaluation using trochanteric gamma 3 locking nail versus PFN antirotation
Hong Man Cho, Kwang Min Park, Tae Gon Jung, Ji Yeon Park, Young Lee
BMC Musculoskeletal Disorders.2021;[Epub] CrossRef - Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
Journal of the Korean Fracture Society.2021; 34(3): 105. CrossRef
- Intermediate Length Cephalomedullary Nails in Proximal Femoral Fractures: Review of Indications and Outcomes
- 2,312 View
- 22 Download
- 10 Crossref

- Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
- Se Jin Kim, Hong Man Cho, Jiyeon Park, Ki Yong An, Young Woo Chung, Woojin Shin
- J Korean Fract Soc 2020;33(4):179-188. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.179
-
 Abstract
Abstract
 PDF
PDF - Purpose
Intertrochanteric fractures can be treated using proximal femoral nail antirotation (PFNA). This study examined the clinical and radiological results of the intraoperative fracture compression.
Materials and Methods
Ninety-four patients underwent intraoperative compression (Group I), and 88 patients underwent natural sliding only (Group II). The patients were followed-up for more than two years. All patients met the following seven conditions: (1) AO/OTA 31-A1, A2 type intertrochanter fracture, (2) availability of compression of more than one cortical bone in the anterior or medial region of the fracture site under the preoperative imaging test, (3) Singh index grade ≥3, (4) blade position: center-center, center-inferior, (5) tip-apex distance <25 mm, (6) reduction status of good or very good, and (7) positive or neutral medial cortical support position with slightly valgus reduction.
Results
A slight tendency toward significant differences in acute phase pain between the two groups was observed at six weeks postoperatively (p=0.073). Twenty-four months after surgery, lateral extension of the PFNA helical blade between the two groups showed significant differences (p=0.017). Fracture gaps measured immediately after surgery showed significant differences (p=0.001), and a clear tendency for a significant difference in the average fracture union time was found (p=0.065).
Conclusion
Intraoperative fracture compression, intraoperative fracture compression appears beneficial to achieve a successful union of trochanteric fractures provided that all conditions are met to apply the method safely. -
Citations
Citations to this article as recorded by- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
Journal of the Korean Fracture Society.2022; 35(4): 151. CrossRef
- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- 726 View
- 3 Download
- 1 Crossref

Case Reports
- Rendezvous Surgery for Peri-Implant Fractures around Locking Compression Plate on Anterolateral Bowed Femur - A Case Report -
- Hong Man Cho, Jiyeon Park
- J Korean Fract Soc 2020;33(3):159-163. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.159
-
 Abstract
Abstract
 PDF
PDF - An 84-year-old female visited with an intertrochanteric femoral fracture. The patient had undergone an open reduction and internal fixation with a compressive plate and elastic nail in an ipsilateral atypical diaphyseal femoral fracture in the past. Compressive plate and elastic nail remained, and anterolateral bowing was presented. To treat the periprosthetic trochanteric fracture, a proximal femoral nail was used without removing the previously inserted compressive plate. Under the “rendezvous” technique, using a combination of fixating intramedullary nail and compressive plate simultaneously, the distal screw was fixed, and a femoral head lag screw was inserted after reducing the fracture. Complete union of the fracture was achieved 16 months after the operation, and a decrease in mobility function was not found postoperatively. The authors report this case for the “rendezvous” technique as a treatment option for elderly patients with periprosthetic trochanteric fractures, who had previously undergone surgical treatment for ipsilateral atypical diaphyseal femoral fractures with anterolateral bowing.
- 453 View
- 3 Download

- Rare Experience of Bilateral Femoral Neck and Shaft Fractures - A Case Report -
- DaeHyun Choe, Jae-Ho Lee, Ki-Chul Park
- J Korean Fract Soc 2020;33(3):154-158. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.154
-
 Abstract
Abstract
 PDF
PDF - Ipsilateral fractures of the femoral neck and shaft are relatively common injuries and accompany 2% to 9% of all femoral shaft fractures. On the other hand, it is extremely rare for these injuries to occur bilaterally. This paper reports the authors’ experience of a case with bilateral femoral neck and shaft fractures. The patient sustained multiple injuries, including liver laceration with hemoperitoneum, bilateral open fractures of the tibia, and bilateral femoral neck, and shaft fractures caused by a high-speed motor vehicle accident. Under the circumstances, damage-control orthopedic principles were applied, and external fixators were initially placed. After the patient’s general condition showed improvement, both femurs were fixed with a reconstruction nail. Fracture healing was achieved without complications, such as avascular necrosis of the femoral head. Despite the rare occurrence, this paper describes this case because these injuries must be managed with meticulous attention.
- 494 View
- 8 Download

Original Articles
- Does the Use of a Silicone Ring Tourniquet Help Reduce Bleeding in the Minimally Invasive Internal Fixation with Locking Plate for Distal Femoral Fractures?
- Ki-Bong Park, Hong-Ki Jin, Il-Yeong Hwang, Sung-Who Chang, Sung-Cheon Na
- J Korean Fract Soc 2020;33(3):148-153. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.148
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the usefulness of a silicone ring tourniquet by analyzing the changes in the perioperative hemoglobin (Hb) levels or amount of perioperative bleeding compared to those of a pneumatic tourniquet or no usage during minimally invasive plate fixation for distal femoral fractures.
Materials and Methods
From January 2017 to December 2019, 30 patients who underwent minimally invasive plate fixation using a locking compression plate for distal femoral fractures were evaluated and classified as a silicone ring tourniquet (Group 1), a pneumatic tourniquet (Group 2), and no usage (Group 3). The variables for analysis were age, sex, preoperative Hb (preHb), postoperative 72-hour Hb (postHb), differences between preHb and postHb (preHb-postHb), amount of intraoperative and overall transfusion, estimated unit of transfusion corrected by preHb-postHb and total transfusion (Hb-lost), amount of intraoperative and postoperative and total bleeding. One-way ANOVA was used to identify the differences between the groups.
Results
The age, sex, operation time, preHb, preHb-postHb, amount of intraoperative and overall transfusion and Hb-lost were similar in the two groups. The amount of intraoperative bleeding was significantly lower in Group 1 than Group 3 (p=0.004), but there was no difference in the amount of postoperative and total bleeding between the two groups.
Conclusion
The use of a silicone ring tourniquet in the minimally invasive plate fixation for distal femoral fractures decreased the amount of intraoperative bleeding compared to no use of a tourniquet. -
Citations
Citations to this article as recorded by- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
Tae sung Lee, Kwan Kyu Park, Byung Woo Cho, Woo-Suk Lee, Hyuck Min Kwon
BMC Musculoskeletal Disorders.2023;[Epub] CrossRef
- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
- 909 View
- 6 Download
- 1 Crossref

- Clinical and Radiological Outcomes of Polished Cemented Bipolar Hemiarthroplasty for Intertrochanteric Fractures in Elderly Patients
- Suc-Hyun Kweon, Chang-Hyun Shin, Yeong-Chang Lee, Min-Woo Kim, Tae-Ho Kim
- J Korean Fract Soc 2020;33(3):134-141. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.134
-
 Abstract
Abstract
 PDF
PDF - Purpose
To evaluate the clinical and radiological outcomes of bipolar hemiarthroplasty using a polished cemented femoral stem for intertrochanteric fractures in elderly patients.
Materials and Methods
From July 2005 to May 2015, 48 patients diagnosed with intertrochanteric fractures underwent bipolar hemiarthroplasty. The mean age and follow-up period were 80.5 years and 30.5 months, respectively. The postoperative results were evaluated clinically and radiologically.
Results
The mean operation time was 100 minutes (range, 90-120 minutes), and the mean amount of blood loss was 334 ml (range, 170-500 ml). At the last follow-up, the mean Harris hip score (HHS), visual analogue scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores were 82.2 (range, 76-90), 0.8 (range, 1-3), and 36 (range, 30-40), respectively. Walking was initiated using a walker for partial weight-bearing, and the mean walking time was 5.8 days (range, 3-14 days). Ambulatory ability was restored to a walking state before the injury in 36 cases (75.0%), and wheelchair ambulation was possible in 12 cases (25.0%). The instrumental activities of daily living (IADLs) were 17 patients (35.4%), and the basic activities of daily living (BADLs) were 31 patients (64.6%).
Conclusion
Polished cemented bipolar hemiarthroplasty can achieve secure fixation with no postoperative thigh pain. Restoring the preoperative walking ability will be more helpful for intertrochanteric fractures in elderly patients.
- 629 View
- 4 Download

Case Report
- Femoral Head Fracture with Hip Dislocation Treated by Autologous Osteochondral Transfer (Mosaicplasty) - A Case Report -
- Eui-Sung Choi, Hyun-Chul Shon, Ho-Seung Jeong, Jae-Young Yang, Seok-Hyun Hong, Byung-Hyun Ahn
- J Korean Fract Soc 2020;33(2):96-100. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.96
-
 Abstract
Abstract
 PDF
PDF - Femoral head fractures combined with hip dislocation are very rare injuries. In most cases, they result from high-energy trauma to the hip or lower extremity during traffic accidents. Various therapy options have been suggested to treat these injuries. Especially, different joint-preserving surgical options have been described for the treatment of traumatic osteochondral injury of the femoral head in young, active patients. In this report, we present a case that a traumatic osteochondral lesion to the femoral head after hip dislocation was treated with osteochondral autografts (OATS) from the non-weight-bearing area of the ipsilateral inferior femoral head through a surgical hip dislocation. After 1 year, the clinical and radiological outcome was satisfactory with no evidence of posttraumatic osteoarthritis and no pain of patients.
-
Citations
Citations to this article as recorded by- Femoral head fracture with large crushed defect in weight-bearing area treated with autologous osteochondral transplantation (repositionplasty): A case report
Hyun-Chul Shon, Eic-Ju Lim, Jae-Young Yang, Seung-Jun Jeon
Medicine.2022; 101(52): e32569. CrossRef
- Femoral head fracture with large crushed defect in weight-bearing area treated with autologous osteochondral transplantation (repositionplasty): A case report
- 680 View
- 2 Download
- 1 Crossref

Original Articles
- Three-Dimensional Analysis of the Morphological Features in the Femur of Atypical Fracture and Practical Implications of Intramedullary Nailing
- Yong Uk Kwon, Kyung-Jae Lee, Joo Young Choi, Gu-Hee Jung
- J Korean Fract Soc 2020;33(2):87-95. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.87
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study analyzed the morphological features of the contralateral femur without an atypical fracture by constructing a three-dimensional model with an actual size medullary canal.
Materials and Methods
Lateral and anterior bowing of the shaft were measured for 21 models, and the shape of the medullary canal was analyzed. To eliminate the projection error, the anteroposterior (AP) femur was rotated internally to the extent that the centerline of the head and neck, which is the ideal position of cephalomedullary nail screw, was neutral, and the lateral femur matched the medial and lateral condyle exactly.
Results
The lateral bowing and anterior bowing was an average of 5.5° (range, 2.8°-10.7°; standard deviation [SD], 2.4°) and 13.1° (range, 6.2°-21.4°; SD, 3.2°), respectively. In the area where lateral bowing increased, the lateral cortex became thicker, and the medullary canal was straightened. On the lateral femur, the anterior angle was increased significantly, and the diameter of curvature averaged 1,370.2 mm (range, 896-1,996 mm; SD, 249.5 mm).
Conclusion
Even if the anterolateral bowing increases in the atypical femur, the medullary canal tends to be straightened in the AP direction. So, it might be considered as a reference to the modification of an intramedullary nail to increase the conformity.
- 454 View
- 5 Download

- Analysis of the Changes in Femoral Varus Bowing and the Factors Affecting Nonunion for the Treatment of Femoral Shaft Fractures over 60 Years Old Using Piriformis Fossa Insertion Intramedullary Nailing
- Yonghan Cha, Chan Ho Park, Jun-Il Yoo, Jung-Taek Kim, WooSuk Kim, Ha-Yong Kim, Won-Sik Choy
- J Korean Fract Soc 2020;33(2):65-71. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.65
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the bony morphological changes to analyze the factors affecting bony union in the treatment of elderly femoral shaft fractures with varus bowing using piriformis fossa insertion intramedullary nailing.
Materials and Methods
This study included 26 patients over 60 years of age, who were admitted for femoral shaft fractures between January 2005 and December 2014 and treated with piriformis fossa insertion intramedullary nailing. Age, sex, height, weight, bone mineral density, injury mechanism, fracture type, diameter and length of the nail, postoperative lengthening of the femur, postoperative change in varus angle, contact between the lateral and anterior cortex, and the gap between the fracture line and the bony union were checked. The patients were divided into a varus group and nonvarus group, as well as a bone union group and nonunion group. Logistic regression analysis was performed to analyze the factors affecting nonunion.
Results
The patients were classified into 11 in the varus group and 15 in the non-varus group and 24 in the union group and 2 in the nonunion group. The varus group showed a larger increase in leg length and varus angle reduction than the non-varus group (p<0.05). The union group had more contact with the lateral cortical bone than that of the nonunion group (p<0.05). The factor affecting bone union in regression analysis was contact of the lateral cortical bone (p<0.05).
Conclusion
Treatment of a femoral shaft fracture in elderly patients with a varus deformity of the femur using piriformis fossa insertion intramedullary nail increases the length of the femur and decreases the varus deformity. For bony union, the most important thing during surgery is contact of the lateral cortical bone with the fracture site. -
Citations
Citations to this article as recorded by- Straight nail insertion through a laterally shifted entry for diaphyseal atypical femoral fractures with bowing: good indications and limitations of this technique
Seong-Eun Byun, Young-Ho Cho, Young-Kyun Lee, Jung-Wee Park, Seonguk Kim, Kyung-Hoi Koo, Young Soo Byun
International Orthopaedics.2021; 45(12): 3223. CrossRef
- Straight nail insertion through a laterally shifted entry for diaphyseal atypical femoral fractures with bowing: good indications and limitations of this technique
- 976 View
- 4 Download
- 1 Crossref

Review Article
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty
- Jung Hoon Choi, Jong Hyuk Jeon, Kyung Jae Lee
- J Korean Fract Soc 2020;33(1):43-51. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.43
-
 Abstract
Abstract
 PDF
PDF - Although the incidence of postoperative periprosthetic femoral fractures after hip arthroplasty is expected to increase, these complex fractures are still challenging complications. To obtain optimal results for these fractures, thorough clinical and radiographic evaluation, precise classification, and understanding of modern management principles are mandatory. The Vancouver classification system is a simple, effective, and reproducible method for planning proper treatments of these injuries. The fractures associated with a stable femoral stem can be effectively treated with osteosynthesis, though periprosthetic femoral fractures associated with a loose stem require revision arthroplasty. We describe here the principles of proper treatment for the patients with periprosthetic femoral fractures as well as how to avoid complications.
- 1,430 View
- 10 Download

Original Articles
- Failure of Intramedullary Nailing for Subtrochanteric Atypical Femoral Fractures Caused by Endosteal Cortical Thickening
- Young Ho Roh, Kimoon Kang, Hee Joong Kim, Kwang Woo Nam
- J Korean Fract Soc 2019;32(4):211-221. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.211
- Correction in: J Musculoskelet Trauma 2020;33(1):63
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Recent literature has noted incidences of subtrochanteric atypical femoral fractures (AFFs) in patients who have taken long-term bisphosphonates (BPs). Most cases of subtrochanteric AFFs have been treated with intramedullary nailing and cases of delayed union have been reported. On the other hand, there is no data available on the complications associated with endosteal thickening or cortical thickening. This study evaluated the results of surgical treatment according to the endosteal thickening of the lateral cortex in subtrochanteric AFFs.
MATERIALS AND METHODS
Investigation was performed at the Department of Orthopaedic Surgery, Jeju National University Hospital. The study consisted of patients with subtrochanteric AFFs, defined by the American Society for Bone and Mineral Research (ASBMR) major criteria, who underwent intramedullary nailing from March 2012 to October 2014. The cases were categorized into two groups based on the presence of endosteal thickening. The evaluation included the demographic data, radiographic data of initial reduction state, and duration of BPs.
RESULTS
The demographic data and duration of BPs were similar in the two groups. On the other hand, varus reduction (Group I: 12.5% vs. Group II: 78.9%; p=0.001), delayed union (Group I: 0% vs. Group II: 70.0%; p=0.003), nonunion (Group I: 0% vs. Group II: 47.4%; p=0.017), and union time (Group I: 5.5 months vs. Group II: 8.3 months; p<0.001) were significantly different in the two groups.
CONCLUSION
Endosteal thickening of the lateral cortex in subtrochanteric AFFs was identified as an independent factor that decides the reduction of the fracture and nonunion. The endosteal thickening should be removed to obtain anatomical alignment for successful surgical results. -
Citations
Citations to this article as recorded by- Controlled bending of proximal femoral nails used in fractures of bowed femurs: biomechanical study with clinical application
Hong Moon Sohn, Suenghwan Jo
Medical Biological Science and Engineering.2022; 5(2): 63. CrossRef
- Controlled bending of proximal femoral nails used in fractures of bowed femurs: biomechanical study with clinical application
- 1,074 View
- 5 Download
- 1 Crossref

- Outcomes following Treatment of Geriatric Distal Femur Fractures with Analyzing Risk Factors for the Nonunion
- Soo young Jeong, Jae Ho Lee, Ki Chul Park
- J Korean Fract Soc 2019;32(4):188-195. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.188
- Correction in: J Musculoskelet Trauma 2020;33(1):62
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Many international journals have published studies on the results of distal femoral fractures in elderly people, but only a few studies have been conducted on the Korean population. The aim of this study was to determine the factors that are associated with the outcomes and prognosis of fixation of distal femur fractures using the minimally invasive plate osteosynthesis (MIPO) technique in elderly patients (age≥60) and to determine the risk factors related witht he occurrence of nonunion.
MATERIALS AND METHODS
This study is a retrospective study. From January 2008 to June 2018, distal femur fracture (AO/OTA 33) patients who underwent surgical treatment (MIPO) were analyzed. A total of 52 patients were included in the study after removing 121 patients that met with the exclusion criteria. Medical records, including surgical records, were reviewed to evaluate the patients' underlying disease, bone mineral density, the number of days delayed from surgery, complications and mortality. In addition, follow-up radiographs were used to determine bone union, delayed union and nonunion.
RESULTS
The average time to achieve bone union was 19.95 weeks, the rate of nonunion was 20.0% (10/50) and the overall mortality was 3.8% (2/52). There were no significant differences in the clinical and radiological results of those patients with or without periprosthetic fracture. On the univariate analysis, which compared the union group vs. the nonunion group, no factors were identified as significant risk factors for nonunion. On the multiple logistic regression analysis, medical history of cancer was identified as a significant risk factor for nonunion (p=0.045).
CONCLUSION
The rate of nonunion is high in the Korean population of elderly people suffering from distal femur fracture, but the mortality rate appears to be low. A medical history of cancer is a significant risk factor for nonunion. Further prospective studies are required to determine other associated factors. -
Citations
Citations to this article as recorded by- Comparison of Clinical Outcomes for Femoral Neck System and Cannulated Compression Screws in the Treatment of Femoral Neck Fracture
Jae Kwang Hwang, KiWon Lee, Dong-Kyo Seo, Joo-Yul Bae, Myeong-Geun Song, Hansuk Choi
Journal of the Korean Fracture Society.2023; 36(3): 77. CrossRef
- Comparison of Clinical Outcomes for Femoral Neck System and Cannulated Compression Screws in the Treatment of Femoral Neck Fracture
- 1,047 View
- 8 Download
- 1 Crossref

- Safety and Effectiveness of the Anchor Augmentation with Bone Cement on Osteoporotic Femoral Fracture: A Systematic Reviews
- So Young Kim
- J Korean Fract Soc 2019;32(2):89-96. Published online April 30, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.2.89
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This paper reviewed the safety and effectiveness of anchor augmentation with bone cement in osteoporotic femoral fractures.
MATERIALS AND METHODS
A systematic review was conducted by searching multiple databases including five Korean databases, Ovid-MEDLINE, Ovid-EMBASE, and Cochrane Library. Safety was assessed through the incidence of complication. The effectiveness was assessed through the failure rate of anchor fixation, improvement of function and radiological assessment (sliding distance of lag screw and cutout). The safety and effectiveness of anchor augmentation with bone cement were assessed by reviewing all articles reporting on the treatment. Two researchers carried out independently each stage from the literature search to data extraction. The tools of Scottish Intercollegiate Guidelines Networks were used to assess the quality of studies.
RESULTS
Six studies were considered eligible. The safety results revealed a small amount of cement leakage (1 case), but no other severe complications were encountered. Regarding the effectiveness, the failure rate of anchor fixation was 16.7% and the Harris's hip score showed no significant improvement. The sliding distance of the anchor was similar in the cement augmentation group and non-cement group but there was no cutout.
CONCLUSION
The results of the assessment suggest that the safety is acceptable, but further research will be needed to verify the effectiveness of the treatment.
- 680 View
- 5 Download

- Results of Exchange Nailing in Hypertrophic Nonunion of Femoral Shaft Fracture Treated with Nailing
- Suenghwan Jo, Gwang Chul Lee, Sang Hong Lee, Jun Young Lee, Dong Hwi Kim, Sung Hae Park, Young Min Cho
- J Korean Fract Soc 2019;32(2):83-88. Published online April 30, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.2.83
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
This study examined the outcomes of exchange nailing for the hypertrophic nonunion of femoral shaft fractures treated with intramedullary nailing as well as the factors affecting the treatment outcomes.
MATERIALS AND METHODS
From January 1999 to March 2015, 35 patients, who had undergone intramedullary nailing with a femoral shaft fracture and underwent exchange nailing due to hypertrophic nonunion, were reviewed. This study investigated the time of union and complications, such as nonunion after exchange nailing, and analyzed the factors affecting the results.
RESULTS
Bone union was achieved in 31 cases (88.6%) after exchange nailing and the average bone union period was 22 weeks (14–44 weeks). Complications included persistent nonunion in four cases, delayed union in one case, and superficial wound infection in one case. All four cases with nonunion were related to smoking, three of them were distal shaft fractures, and one was a midshaft fracture with underlying disease.
CONCLUSION
Exchange nailing produced satisfactory results as the treatment of hypertrophic nonunion after intramedullary nailing. Smoking is considered a factor for continuing nonunion even after exchange nailing. In the case of a distal shaft, where the intramedullary fixation is relatively weak, additional efforts are needed for stability.
- 768 View
- 7 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


