Articles
- Page Path
- HOME > J Korean Fract Soc > Volume 37(1); 2024 > Article
- Original Article Triplane Fracture Management: Prediction of Periosteal Entrapment and the Need for Open Reduction by Measurements of the Physeal Fracture Gap in Preoperative Computed Tomography Scans
- Dae Hee Lee, Joo Han Kwon, Jae Uk Jung
-
Journal of The Korean Orthopaedic Trauma Association 2024;37(1):1-7.
DOI: https://doi.org/10.12671/jkfs.2024.37.1.1
Published online: January 31, 2024
- 1,393 Views
- 20 Download
- 1 Crossref
- 0 Scopus
Abstract
Purpose
This study measured the physeal fracture gap on preoperative ankle computed tomography (CT) to predict the periosteal entrapment that requires an open reduction in distal tibia triplane fractures.
Materials and Methods
This study retrospectively reviewed patients who had undergone internal fixation for a triplane fracture from April 2004 to September 2022. The demographic data, including age,body mass index, and past medical history, were analyzed. In the radiographic evaluations, ankle CT and ankle simple radiographs, including anteroposterior (AP), lateral, and mortise views, were taken preoperatively. Postoperatively, simple ankle radiographs were obtained periodically, including AP, mortise, and lateral views. The physeal fracture gap was measured on ankle CT, and the larger gap between the coronal and sagittal view of CT was selected. The residual physeal gap <2 mm was considered an adequate reduction.
Results
Of 17 cases, three demonstrated successful reduction using closed reduction techniques. Periosteal entrapment was observed in 14 cases open reduction cases. In all three closed reduction cases, the physeal gap estimated on preoperative ankle CT was under 3 mm with a mean gap of 2.4±0.2 mm (range, 2.1-2.5 mm). In the remaining 14 open reduction cases, the measured physeal gap was over 3 mm, averaging 5.0±2.7 mm (range, 3.1-12.2 mm). There was a significant difference in the preoperative physeal gap between the two groups (p<0.01). Overall, good reduction was achieved in all 17 cases; the postoperative physeal gap was under 2 mm with a mean of 1.0±0.5 mm (closed reduction group, 0.5±0.2 mm; open reduction group, 1.1±0.5 mm).
Conclusion
Open reduction is strongly recommended for triplane fractures with a physeal fracture gap of 3 mm or more in preoperative ankle CT, suggesting the possibility of an entrapped periosteum in the fracture gap.
Published online Jan 24, 2024.
https://doi.org/10.12671/jkfs.2024.37.1.1
Abstract
Purpose
This study measured the physeal fracture gap on preoperative ankle computed tomography (CT) to predict the periosteal entrapment that requires an open reduction in distal tibia triplane fractures.
Materials and Methods
This study retrospectively reviewed patients who had undergone internal fixation for a triplane fracture from April 2004 to September 2022. The demographic data, including age, body mass index, and past medical history, were analyzed. In the radiographic evaluations, ankle CT and ankle simple radiographs, including anteroposterior (AP), lateral, and mortise views, were taken preoperatively. Postoperatively, simple ankle radiographs were obtained periodically, including AP, mortise, and lateral views. The physeal fracture gap was measured on ankle CT, and the larger gap between the coronal and sagittal view of CT was selected. The residual physeal gap <2 mm was considered an adequate reduction.
Results
Of 17 cases, three demonstrated successful reduction using closed reduction techniques. Periosteal entrapment was observed in 14 cases open reduction cases. In all three closed reduction cases, the physeal gap estimated on preoperative ankle CT was under 3 mm with a mean gap of 2.4±0.2 mm (range, 2.1-2.5 mm). In the remaining 14 open reduction cases, the measured physeal gap was over 3 mm, averaging 5.0±2.7 mm (range, 3.1-12.2 mm). There was a significant difference in the preoperative physeal gap between the two groups (p<0.01). Overall, good reduction was achieved in all 17 cases; the postoperative physeal gap was under 2 mm with a mean of 1.0±0.5 mm (closed reduction group, 0.5±0.2 mm; open reduction group, 1.1±0.5 mm).
Conclusion
Open reduction is strongly recommended for triplane fractures with a physeal fracture gap of 3 mm or more in preoperative ankle CT, suggesting the possibility of an entrapped periosteum in the fracture gap.
초록
목적
본 연구의 목적은 원위 경골 삼면 골절에서 수술 전 족관절 컴퓨터 단층촬영에서의 골단판 골절 간격을 측정하여 관혈적 정복이 필요한 골막 포착 유무를 예측하기 위함이다.
대상 및 방법
2004년 4월부터 2022년 9월까지 원위 경골 삼면 골절에 대해 내고정술을 시행 받은 환자를 후향적으로 조사하였다. 인구학적 자료로는 나이, 체질량지수, 과거력 등이 포함되었다. 방사선학적으로는 수술 전 족관절 전후방, 격자상(mortise view), 측방 단순 방사선 촬영 및 족관절 컴퓨터 단층촬영을 분석하였다. 수술 전 족관절 컴퓨터 단층촬영에서 관상면, 시상면에서의 골단판 골절 간격 중 더 큰 간격을 측정하였다. 수술 후 족관절 전후방, 격자상, 측방 단순 방사선 촬영에서 수술 후 골단판 골절 간격을 측정하였으며, 골단판 간격이 2 mm 미만으로 측정될 때 적절한 정복으로 간주하였다.
결과
총 17예 중 3예에서 도수 정복 및 내고정술로 적절한 정복을 얻었으며, 나머지 14예에서 관혈적 정복이 이루어졌고, 골막 포착이 관찰되었다. 도수 정복을 시행한 3예에서 측정한 골단판 골절 간격의 평균은 2.4±0.2 mm (범위 2.1-2.5 mm)로 3 mm 이하로 측정되었다. 또한, 관혈적 정복을 시행한 14예에서 측정한 골단판 골절 간격의 평균은 5.0±2.7 mm (범위 3.1-12.2 mm)로 3 mm 초과로 측정되었다. 도수 정복을 시행한 군에서의 수술 전 골단판 골절 간격이 관혈적 정복을 시행한 군의 골단판 골절 간격보다 통계적으로 유의하게 짧았다(p<0.01). 총 17예에서 수술 후 골단판 골절 간격은 평균 1.0±0.5 mm로 2 mm 미만의 만족스러운 정복이 확인되었다(도수 정복을 시행한 군: 평균 0.5±0.2 mm; 관혈적 정복을 시행한 군: 평균 1.1±0.5 mm).
결론
원위 경골 삼면 골절에서 수술 전 족관절 컴퓨터 단층촬영에서의 골단판 골절 간격이 3 mm 이상으로 측정될 때, 골절 간격 내 골막 포착이 되어있을 가능성이 높아 관혈적 정복술이 고려되어야 한다.
Introduction
The triplane fracture of distal tibia, exclusive to the pediatric population, presents a distinctive fracture pattern in the growth plate of the distal tibia. The triplane fracture is defined as a triad of fracture lines on different anatomical planes—one intra-articular transverse, one sagittal, and one coronal—creating distinct fracture fragments.1,2,3) This complexity arises from the ongoing skeletal development in children, where the growth plate remains a vulnerable region, closing from central to medial, and finally to lateral direction.4) The distal tibia triplane fracture accounts for approximately 5% to 10% of pediatric intra-articular ankle injuries. And the epiphysis of distal tibia is the second most common area of epiphyseal fracture, following that of distal radius in pediatric patients. The fracture usually presents in pediatric patients aged 12 to 15 years with a relatively higher incidence in boys than in girls.5)
In treatment of distal tibia triplane fracture, extra-articular fracture and nondisplaced fracture (<2 mm displacement) can be indications of conservative treatment with immobilization in long leg cast. However, because the distal tibia triplane fracture is associated with complications including physeal arrest, articular incongruity, and angular deformity,6,7) fracture with >2 mm displacement requires closed or open reduction and internal fixation is need in most cases. Furthermore, in cases of intra-articular fracture (step off >2 mm), fracture with >3 mm displacement, and failure to achieve proper reduction, open reduction and internal fixation technique is needed.8) In considering reduction strategies between closed or open, the presence of periosteal entrapment within the fracture fragments further complicates the reduction process. Unlike adult fractures, pediatric fractures, including triplane fractures, often exhibit unique features such as increased cartilaginous content, greater capacity for remodeling, and a propensity for periosteal involvement.9,10) These characteristics necessitate specialized consideration in fracture management strategies. Residual physeal gap >3 mm following closed reduction represented entrapment of periosteum, leading to a higher incidence of premature physeal closure in Salter-Harris type I and II fractures.11) So, when the periosteum is entrapped, anatomical reduction and removal of entrapped periosteum are crucial. However, there were no studies of establishing the standards that predict the entrapment of periosteum and help deciding the reduction strategies. The aim of this study is to measure the physeal fracture gap on preoperative ankle computed tomography (CT), and to predict the entrapment of periosteum that needs open reduction.
Materials and Methods
This study was approved by the Institutional Review Board (IRB) of Dankook University Hospital (IRB No. 2023-11-010), and the written informed consent was waived by the IRB due to the retrospective nature of the study. We retrospectively reviewed our patients who had undergone internal fixation for triplane fracture from April 2004 to September 2022 in single center. Inclusion criteria are as follows; (1) diagnosed as distal tibia triplane fracture, (2) age under 18, and (3) follow-up at least 12 months after surgery. Exclusion criteria are as follows; (1) previous history of surgery or trauma in the affected side of the ankle, (2) concomitant injury in adjacent lower extremity structure, (3) diagnosed with hormone or genetic diseases related to growth, and (4) history of infection or vascular problems.
Among 20 patients who underwent internal fixation for distal tibia triplane fracture, 3 patients were excluded. A total of 17 patients, patients were divided into two groups; one for closed reduction and internal fixation group (Fig. 1), and the other for open reduction and internal fixation group (Fig. 2). Demographic data including age, body mass index (BMI), and past medical history were analyzed. In radiographic evaluations, ankle simple radiographs including anteroposterior (AP), lateral, mortise views and ankle CT scans were taken preoperatively. Postoperatively, AP, lateral, and mortise view of simple ankle radiographs were periodically obtained. The physeal fracture gap was estimated on ankle CT, and the larger gap between coronal and sagittal view of CT was selected. In postoperative simple radiograph, the largest physeal gap was estimated on ankle simple radiographs, and the gap <2 mm was considered as adequate reduction.12)
Fig. 1
Preoperative ankle X-ray, computed tomography (CT), and postoperative ankle X-ray of the closed reduction case, 14-year-old male. (A) Preoperative ankle X-ray. (B) Preoperative ankle CT, coronal, sagittal, and axial view. Arrows, physeal fracture gap: 1.4 mm. (C) Postoperative ankle X-ray.
Fig. 2
Preoperative ankle X-ray, computed tomography (CT), and postoperative ankle X-ray of the open reduction case, 13-year-old male. (A) Preoperative ankle X-ray. (B) Preoperative ankle CT, coronal, sagittal, and axial view. Arrows, physeal fracture gap: 5.8 mm. (C) Postoperative ankle X-ray.
1. Surgical technique
All procedures were performed under general or spinal anesthesia using a thigh pneumatic tourniquet. When reduction was not acceptable despite trying at least two times of closed reduction, we decided to perform open reduction. A longitudinal incision was made on the anterolateral or anteromedial aspect of ankle according to the fracture patterns. After dissecting soft tissues and retracting tendons, fracture site is exposed. After removal of the periosteum entrapped in the fracture site, fracture site is reduced and fixed using two or three cannulated screws using intraoperative C-arm images. After surgery, immobilization with a short leg cast for four weeks was followed by rehabilitation such as muscle strengthening and joint range of motion exercise for about 8 weeks. More vigorous activities were recommended only after 3 months following surgery.
2. Statistical analysis
For comparisons between groups, the Student’s t-test, and the Mann–Whitney U test were used for continuous variables such as age, BMI, and physeal gap after performing the Shapiro–Wilk normality test. In comparison of sex between two groups, Fisher’s exact test was performed. Radiologic parameters between the preoperative and postoperative images were compared using the paired sample t-test or Wilcoxon signed-rank test. Statistical significance was set at p<0.05. Data were analyzed using SPSS Statistics 26.0 statistical software (IBM Corp.), and Prism 8 (GraphPad Software Inc.).
Results
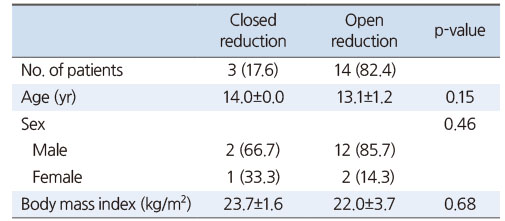
In total 17 cases, three cases demonstrated successful reduction through closed reduction techniques. For the remaining 14 cases, open reduction was necessary to achieve satisfactory reduction. In demographic variables, three cases were female, and 14 cases were male. The mean of age was 13.3±1.2 years (range, 2-16 years). The mean follow-up period was 23.7±16.4 months (range, 12-67 months). There were no significant differences in age, sex, and BMI between closed reduction and open reduction groups (p>0.05) (Table 1). In mechanisms of injury, only one patient was injured by direct injury, and the remaining 16 cases were ankle rotational injuries.
Table 1
Demographic Data of the Patients
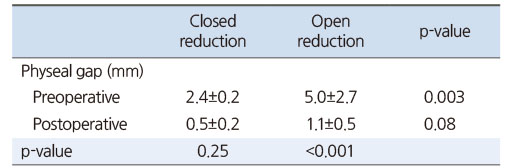
In 14 open reduction cases, periosteal entrapment was observed in all 14 cases (Fig. 3). In all three closed reduction cases, physeal gap on preoperative ankle CT was estimated under 3 mm with a mean gap of 2.4±0.2 mm (range, 2.1-2.5 mm). In the remaining 14 open reduction cases, the physeal fracture gap was measured over 3 mm with a mean of 5.0±2.7 mm (range, 3.1-12.2 mm). There was a significant difference in preoperative physeal fracture gap between two groups (p<0.01). Overall, in all 17 cases, good reduction was achieved that postoperative physeal gap was under 2 mm with a mean of 1.0±0.5 mm (closed reduction group, 0.5±0.2 mm; open reduction group, 1.1±0.5 mm, respectively) (Table 2). At the final follow-up, there were no complaints of symptoms including ankle pain, limitation of ankle range of motion, and feeling of leg length discrepancies.
Fig. 3
Intraoperative photo; Entrapment of the periosteum in the fracture gap.
Table 2
Comparisons of the Physeal Fracture Gap Preoperatively and Postoperatively between Closed Reduction and Open Reduction
Discussion
In pediatric fractures, premature physeal closure after fracture is a considerable problem, resulting in angular deformities or leg length discrepancies.6) Especially, the physis of distal tibia is responsible for half of total tibial growth and grows about 4 to 6 mm in longitudinal direction per year.13,14) Leary et al.15) examined 124 distal tibia physeal fractures for determining the incidence of premature physeal closure. Salter–Harris type II fractures resulted in 67% of the premature physeal closure, followed by Salter–Harris III (13%), Salter–Harris IV (13%), and triplane fracture (7%).
Although triplane fractures are associated with premature physeal closure, severe leg length shortening usually do not occur because triplane fractures present in patients aged 12 to 15 years relatively near skeletal maturity.16,17) Cass and Peterson17) reported 13 triplane fractures that did not result in physeal closure problems.
However, triplane fractures are not always free from premature physeal closure and growth disturbance. Rohmiller et al.18) reported that postreduction residual fracture displacement was the most important factor of premature physeal closure. Rapariz et al.12) analyzed 35 patients that a postreduction residual physeal gap of >2 mm at the articular surface did not result in good long term outcomes and led to degenerative changes. So anatomical or near-anatomic reduction to reduce the fracture gap under 2 mm is important.19)
There were several studies that preoperative ankle magnetic resonance imaging (MRI) provided beneficial information about adjacent ligament injury, and periosteum entrapment.20,21) The widening of physeal fracture gap does not always confirm periosteum entrapment and has a possibility of other soft tissue entrapment. However, Park et al.21) reviewed 50 patients with displaced Salter–Harris type II, III, or IV distal tibial physeal fractures, and investigated the incidence of periosteal entrapment in fracture site. Salter–Harris type II and triplane fractures were revealed to have a high risk of periosteal entrapment. In the present study, although ankle MRI scans were not taken, the periosteal entrapment was observed in all of 14 open reduction cases and the physeal fracture gap was measured over 3 mm in preoperative CT. In CT scans, because it was difficult to distinguish between periosteum and adjacent soft tissues by analyzing the difference of density, measurement of fracture physeal gap was thought to be more objective parameter in this study. Similarly, Barmada et al.11) investigated the predictors of premature physeal closure after pediatric distal tibial fractures and reported that additional open reduction was required in cases of residual physeal gap >3 mm following closed reduction and entrapment of periosteum was observed in all of open reduction cases. So, thinking about the possibility of periosteal entrapment in triplane fractures and importance of periosteum in pediatric fractures, the widened physeal fracture gap should be considered as an important factor that suggests the presence of entrapped periosteum and needs open reduction. In this study, we analyzed the physeal fracture gap on CT scan preoperatively to determine the reduction method, compared with the study of Barmada et al.11) which analyzed the residual physeal gap after closed reduction.
The findings of this study emphasize the critical importance of open reduction in cases of triplane fractures complicated by periosteal entrapment. Non-operative approaches may prove inadequate in such scenarios, as the presence of the periosteum within the fracture site hinders successful reduction. Surgeons must exercise caution and employ meticulous techniques to address this challenge, ensuring optimal outcomes for patients with triplane fractures. Furthermore, based on our results, open reduction is strongly recommended for triplane fractures with a physeal fracture gap of 3 mm or more. Further research and standardized guidelines are warranted to refine the management of this complex fracture pattern and improve overall patient care.
There were several limitations in this study. First, this study was retrospective and used data from a single medical center. Second, the total number of patients was small, especially the closed reduction cases, and the duration of the research was relatively short. Finally, not all patients took follow-up ankle CT or preoperative ankle MRI. If follow-up CT and preoperative MRI were taken, it could have been helpful to measure the more accurate postoperative residual physeal gap and check the periosteal entrapment preoperatively. Further studies are needed to analyze the physeal fracture gap, presence of periosteal entrapment, and outcomes between two reduction techniques.
Conclusion
Open reduction is strongly recommended for triplane fractures with a physeal fracture gap of 3 mm or more in preoperative ankle CT, suggesting that there is a possibility of periosteum entrapped in the fracture gap.
Financial support:None.
Conflict of interests:None.
References
-
Jarvis J. Tibial triplane fractures. In: Mervyn Letts R, Baxter MP, editors. Management of pediatric fractures. Churchill Livingstone; 1994. pp. 735-749.
-
-
Atanelov Z, Bentley TP. Greenstick fracture. In: StatPearls. StatPearls Publishing; 2023.
-
-
Aitken AP. The end results of the fractured distal tibial epiphysis. J Bone Jt Surg 1936;18:685–691.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS





 Cite
Cite

