Search
- Page Path
- HOME > Search
Original Article
- Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
- Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
- J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00157
-
 Abstract
Abstract
 PDF
PDF - Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
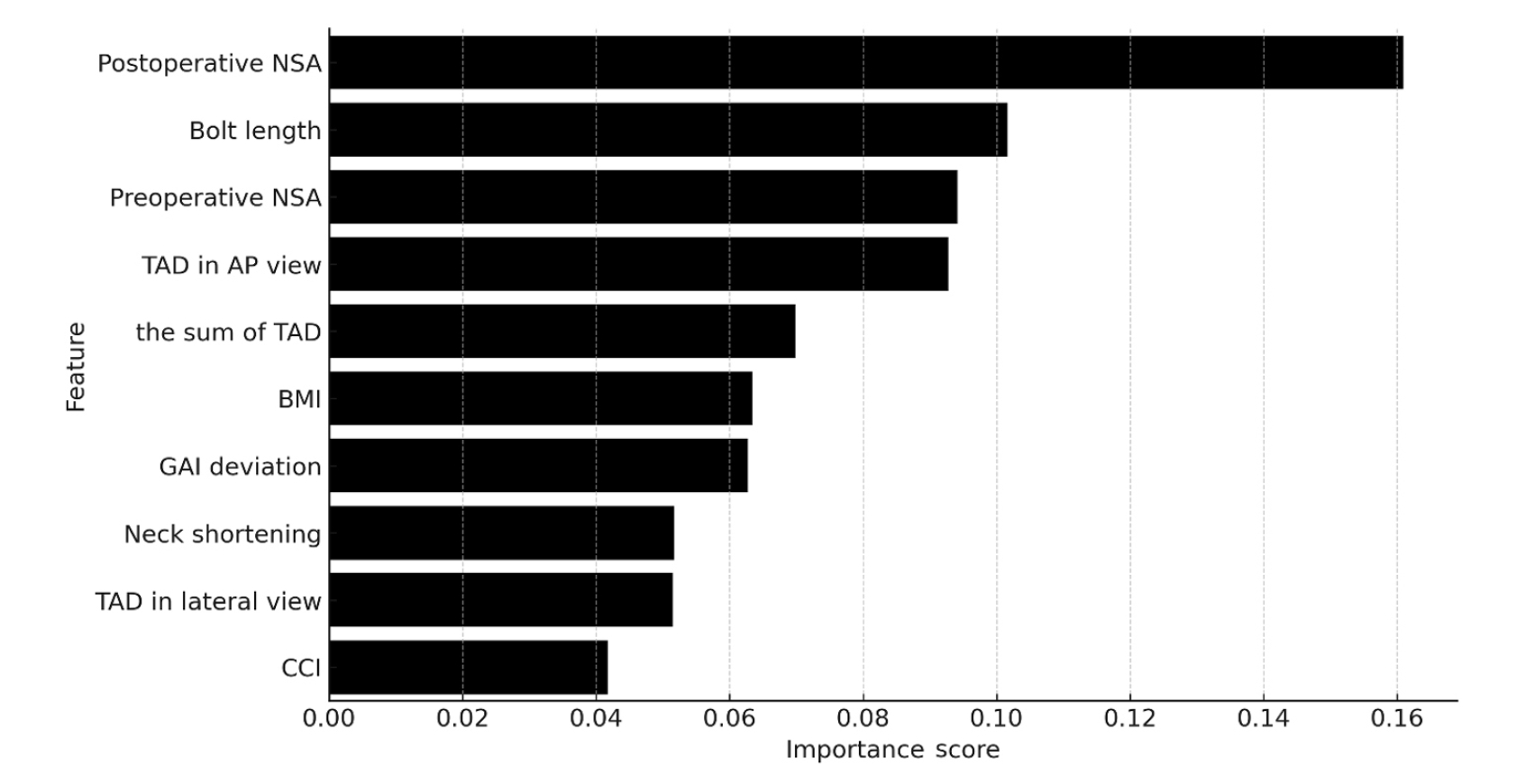
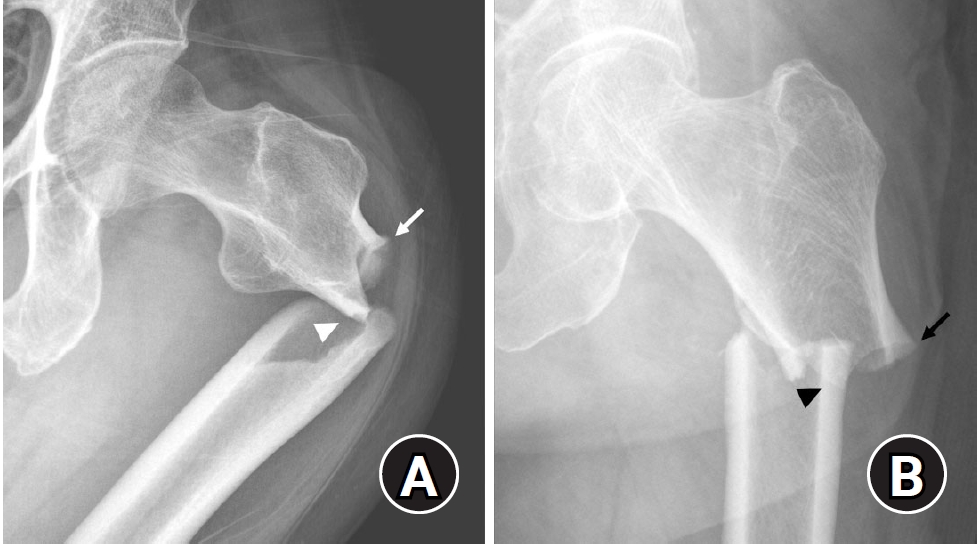
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery. Level of Evidence: III.
- 628 View
- 25 Download

Review Article
- Atypical femoral fractures: an update
- Won-Tae Cho, Jeong-Hyun Koh, Seungyeob Sakong, Jung-Taek Kim
- J Musculoskelet Trauma 2025;38(2):41-52. Published online March 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00031
-
 Abstract
Abstract
 PDF
PDF - This narrative review provides an up-to-date overview of atypical femoral fractures (AFFs), emphasizing diagnostic criteria, epidemiology, pathophysiology, risk factors, and evaluation with screening strategies. AFFs are rare but significant complications associated with prolonged bisphosphonate (BP) therapy for osteoporosis. Although the pathogenesis of AFFs has not been fully elucidated, its primary mechanism is thought to involve impaired bone remodeling, leading to unhealed microfractures that progress to stress fractures under repetitive loading. AFFs can occur in various regions of the femur, influenced by femoral geometry and the lower limb axis. Other risk factors include prolonged steroid use, arthroplasty, genetic predispositions, and metabolic bone disorders. The diagnosis of AFFs is based on criteria established by the American Society for Bone and Mineral Research. Key radiographic features include lateral cortical transverse fracture lines and localized cortical thickening, typically with minimal or no comminution on the medial cortex. Dual-energy X-ray absorptiometry for screening tests and magnetic resonance imaging as an advanced imaging modality enable the early detection of incomplete fractures. This multi-modal approach facilitates the prompt identification of prodromal cortical changes, reducing the risk of complete fractures in high-risk populations, particularly patients undergoing prolonged BP therapy. Level of Evidence: V
- 8,294 View
- 276 Download

Original Articles
- The Results of Intramedullary Nailing with Sliding Restriction and Dynamization Method in Treating Intertrochanteric Fractures
- Hyun Cheol Oh, Sang Hoon Park, Jae Seok Chae, Han Kook Yoon
- J Korean Fract Soc 2024;37(1):8-14. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.8
-
 Abstract
Abstract
 PDF
PDF - Purpose
To evaluate the results of intramedullary nailing with sliding restriction and dynamization methods in treating intertrochanteric fractures.
Materials and Methods
From August 2016 to March 2019, patients aged 65 years and older who underwent intramedullary nailing in treating intertrochanteric fractures were enrolled in this study. The radiological and clinical results were analyzed in 49 patients who had undergone lag screw sliding re-striction and dynamization of the distal interlocking screw method.
Results
Forty-seven patients achieved union without complications (95.9%). The mean union period was 6.5 weeks (range, 6-9 weeks). Complications occurred in two patients (4.1%), including the cut through of the lag screw in one patient and varus deformity of more than 10° in the other. The preinjury mean Koval grade was 2.8 (range, 1-7). The mean was 3.3 (range, 1-7) at the final follow-up, and the mean difference was 0.5 (range, 0-2).
Conclusion
Intramedullary nailing with a sliding restriction and dynamization method for treating in-tertrochanteric fractures achieved union. The reduction achieved during surgery was maintained with good clinical results. This method is a safe and effective treatment technique for femoral intertrochanteric fractures.
- 492 View
- 9 Download

- Effect of Additional Medial Locking Plate Fixation and Autogenous Bone Graft for Distal Femur Nonunion after Lateral Locking Plate Fixation
- Ho Min Lee, Jong Pil Kim, In Hwa Baek, Han Sol Moon, Sun Kyo Nam
- J Korean Fract Soc 2024;37(1):30-38. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.30
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the outcomes of additional medial locking plate fixation and autogenous bone grafting in the treatment of nonunions that occurred after initial fixation for distal femoral fractures using lateral locking plates.
Materials and Methods
The study involved eleven patients who initially underwent minimally invasive lateral locking plate fixation for distal femoral fractures between January 2008 and December 2020. The initial procedure was followed by additional medial locking plate fixation and autogenous bone grafting for clinically and radiographically confirmed nonunions, while leaving the stable lateral locking plate in situ. A clinical evaluation of the bone union time, knee joint range of motion, visual analog scale (VAS) pain scores, presence of postoperative complications, and functional evaluations using the lower extremity functional scale (LEFS) were performed.
Results
In all cases, bone union was achieved in an average of 6.1 months after the secondary surgery. The range of knee joint motion, weight-bearing ability, and VAS and LEFS scores improved at the final follow-up compared to the preoperative conditions. All patients could walk without walking assistive devices and did not experience pain at the fracture site. On the other hand, three patients complained of pain in the lateral knee joint caused by irritation by the lateral locking plate; hence, lateral hardware removal was performed. One patient complained of mild paresthesia at the anteromedial incision site. Severe complications, such as deep infection or metal failure, were not observed.
Conclusion
For nonunion with stable lateral locking plates after minimally invasive lateral locking plate fixation of distal femur fractures, additional medial locking plate fixation and autogenous bone grafting, while leaving the lateral locking plate intact, can achieve successful bone union.
- 264 View
- 4 Download

- Cephalomedullary Nailing with an Additional Cannulated Screw Fixation in Basicervical Femur Fractures
- Keong-Hwan Kim, Woo Dong Nam, Yeon Sik Heo, Gu-Hee Jung
- J Korean Fract Soc 2024;37(1):22-29. Published online January 31, 2024
- DOI: https://doi.org/10.12671/jkfs.2024.37.1.22
-
 Abstract
Abstract
 PDF
PDF - Purpose
The purpose of this study is to analyze the clinical results of patients with basicervical fracture undergoing cephalomedullary nailing (CMN) with an additional cannulated screw fixation compared to only performing CMN. We hypothesized that a difference may exist in the clinical outcomes if an ad-ditional screw is fixed with CMN compared to only performing CMN in basicervical fracture.
Materials and Methods
A total of 28 consecutive patients who underwent CMN for basicervical fracture were included. In 9 cases, only CMN was conducted, and in 19 cases, an additional cannulated screw fixation was performed with CMN. Bone union, sliding distance, reduction status, and fixation failure were evaluated by postoperative radiography, and ambulatory ability was evaluated by functional results. These findings were compared between a group of CMN and a group of CMN with an additional cannulated screw.
Results
There were 4 males and 24 females with a mean age of 84 years (range, 69–100 years). No significant difference was found in postoperative reduction, tip-apex distance, bone union, and walking function recovery after surgery between the two groups, but in the sliding distance of the lag screw, the CMN group demonstrated more sliding (6.2 mm [range, 2.5–13.4 mm] vs 3.5 mm [range, 0.1– 9.2 mm]; p=0.045). Among the two groups, only one case of fixation failure at the postoperative four months was observed in the CMN group (p=0.321), and hemiarthroplasty with nail construct removal was performed.
Conclusion
CMN with additional cannulated screw fixation is a safe and reliable surgical option in basicervical fracture. It provided favorable clinical outcomes and may be a good alternative for treating basicervical fracture.
- 706 View
- 11 Download

- Bone Union Time of Simple Distal Femur Fractures in the Elderly according to Fracture Gap after Treated with Minimally Invasive Plate Osteosynthesis
- Young Ho Cho, Sangwoo Kim, Jaewook Koo
- J Korean Fract Soc 2023;36(4):133-138. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.133
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the difference in bone union time according to the fracture gap after minimally invasive plate osteosynthesis (MIPO) for simple distal femoral fractures in elderly patients.
Materials and Methods
From January 2010 to December 2019, patients aged 60 years or older who underwent surgical treatment for distal femoral fractures due to a low-energy injury were investigated retrospectively. Forty patients were enrolled in the study. The patients were divided into two groups according to the fracture gap after reduction: no more than 2 mm (Group A) and more than 2 mm (Group B) in the anteroposterior and lateral plane. The demographic, operation time, presence or absence of cerclage wiring, plate screw density, plate span ratio, plate length, bone union period, non-union, and complications were evaluated.
Results
No statistical differences in operation time, cerclage wiring, plate screw density, plate span ratio, and plate length were observed between the two groups, and the bone union was achieved in all patients without complication. The bone union period was 17.24±1.48 weeks in Group A and 24.53± 5.20 weeks in Group B, which was statistically significant (p<0.001).
Conclusion
The bone union time in treating geriatric simple distal femur fractures using the MIPO tech-nique was significantly shorter in the 2 mm or less fracture gap than in the greater than 2 mm group.
- 562 View
- 2 Download

- Risk Factors of Fixation Failure in Femoral Neck Fractures
- Sung Hyun Yoon, Kyu Beom Kim, Hyung Jun Lee, Kyung Wook Kim
- J Korean Fract Soc 2023;36(4):118-124. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.118
-
 Abstract
Abstract
 PDF
PDF - Purpose
Internal fixation after a femoral neck fracture (FNF) is one of the conventional treatment options for the young and active elderly patients. However, fixation failure of internal fixation is a probable complication. The treatment of fixation failure after a primary internal fixation of the FNF remains a challenge.
Materials and Methods
Between July 2002 and March 2017, 83 patients who underwent internal fixation after FNF were retrospectively analyzed. Radiological assessments, including Pauwels’ angle, fracture level, reduction quality, and bone union, were measured, preoperatively and postoperatively. Moreover, intraoperative variables such as time to surgery, surgical time, and estimated blood loss were also evaluated.
Results
The patients were divided into the fixation failure and the non-failure groups. Among the 83 patients, 17 cases (20.5%) of fixation failure after the primary internal fixation of the FNF were identi-fied. When comparing the two groups according to the radiographic data, Pauwels’ angle and the reduction quality based on Garden’s angle showed significant differences (p<0.001). Moreover, when comparing the intraoperative variables, unlike the surgical time and estimated blood loss, significant differences were noted in the time interval from injury to surgery and specifically in whether the surgery was performed within 12 hours after injury (p<0.001).
Conclusion
Pauwels’ angle, reduction quality, and time to surgery are the major factors that can predict the possibility of internal fixation failure of the FNF. Early and accurate anatomical reduction is needed to decrease complications after the internal fixation of the FNF.
- 1,589 View
- 19 Download

- Comparison of Clinical Outcomes for Femoral Neck System and Cannulated Compression Screws in the Treatment of Femoral Neck Fracture
- Jae Kwang Hwang, KiWon Lee, Dong-Kyo Seo, Joo-Yul Bae, Myeong-Geun Song, Hansuk Choi
- J Korean Fract Soc 2023;36(3):77-84. Published online July 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.3.77
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the clinical and radiological results of the femoral neck system (FNS) and cannulated compression screws (CCS) for the fixation of femoral neck fractures.
Materials and Methods
Patients who underwent FNS or CCS internal fixation for femoral neck fractures between January 2016 and January 2022 were analyzed retrospectively. The hip joint function using the Harris hip score (HHS) was evaluated three months and one year after surgery. The operation time, fracture healing time, and associated surgical complications in the two groups were compared and analyzed statistically.
Results
Seventy-nine patients were categorized into 38 FNS and 41 CCS groups. The FNS group had a longer operation time and higher postoperative HHS at three months (p<0.01). Femoral neck shortening was lower in the FNS group (p=0.022). There were no significant differences in the fracture healing time and other complications.
Conclusion
There were no differences in most clinical outcomes and complications between the two groups except for the three-month HHS and femoral neck shortening. This study suggests that FNS could be an alternative to CCS for treating femoral neck fractures.
- 595 View
- 14 Download

Technical Note
- Usefulness of Reduction and Internal Fixation Using a 2.4 mm Hand Plating System in Type AO 33-A3 Distal Femur Fracture - Technical Note -
- Bong-Ju Lee, Ja-Yeong Yoon, Seungha Woo
- J Korean Fract Soc 2023;36(1):25-28. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.25
-
 Abstract
Abstract
 PDF
PDF - Open reduction in an AO 33-A3 class distal femur transverse and comminuted fracture is often difficult due to frequent reduction loss during surgery, leading to longer operative time and increased blood loss intra-operation. In this study, the authors report a case in which the use of an offset grid plate (OsteoMed, USA) using 2.4 mm HPS (hand plating system) eased the process of fracture reduction and achieved a stable internal fixation, ultimately leading to successful osteosynthesis. The authors experienced no need for temporary fixation devices such as K-wires or screws, which are otherwise required to stabilize the reduction. The fracture reduction was stable throughout the primary fixation of the fracture using a locking plate and screws. The authors report that the advantage of the HPS plate is fitting into the cortical contour and providing stable maintenance of fracture reduction intra-operation, which would be beneficial in certain distal femoral fracture patterns.
- 393 View
- 7 Download

Original Articles
- Distal Femur Fractures Treated with Distal Femoral Locking Plate Fixation: A Retrospective Study of One Year Mortality and Risk Factors
- Kwang-Hwan Jung, Yoon-Seok Youm, Seung-Hyun Jung, Jae-Min Oh, Ki Bong Park
- J Korean Fract Soc 2023;36(1):10-16. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.10
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the one-year mortality after locking plate fixation for distal femur fractures and the risk factors related to death.
Materials and Methods
From July 2011 to June 2020, 128 patients who underwent locking plate fixation for distal femur fractures were analyzed retrospectively. Epidemiologic information of the patients, characteristics related to fracture and surgery, and death were investigated. The risk factors related to death were investigated using Cox analysis, and a subgroup analysis was also performed based on the age of 65 years.
Results
The one-year mortality rate after locking plate fixation for distal femur fractures was 3.9%, and the mortality rates in patients younger than 65 years and older than 65 years were 0% and 6.7%, respectively. There were no significant risk factors related to death in the total population. On the other hand, in patients aged 65 years or older, however, high-energy fracture and high comorbidity index increased the risk of death after surgery by 6.9-fold and 1.9-fold, respectively.
Conclusion
The one-year mortality rate for the total patients was 3.9%, but the mortality rate for patients over 65 years of age increased to 6.7%. High-energy fractures and high comorbidity index were risk factors related to death after surgery for distal femur fractures in patients aged 65 years or older.
- 364 View
- 1 Download

- Computational Simulation of Femoral Neck System and Additional Cannulated Screws Fixation for Unstable Femoral Neck Fractures and the Biomechanical Features for Clinical Applications
- Ju-Yeong Kim
- J Korean Fract Soc 2023;36(1):1-9. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
To identify the biomechanical features for clinical applications through a computational simulation of the fixation of the Femoral Neck System (FNS) with additional cannulated screws for a Pauwels type III femoral neck fractures.
Materials and Methods
Thirty cadaveric femurs underwent computed tomography, and the images were transferred to the Mimics ® program, resulting in three-dimensional proximal femur models. A three-dimensional scan of the FNS and 6.5 mm and 7.0 mm cannulated screws was performed to enable computerized virtual fixation of FNS with additional cannulated screws for unstable femoral neck fractures. Furthermore, the cannulated screw used for additional fixation was modeled and used as a cylinder within the Ansys program. The biomechanical characteristics of these models were investigated by applying a physiological load virtually.
Results
The maximum von Mises stress value at bone was 380.14 MPa in FNS and 297.87 MPa in FNS+7.0 mm full-thread cannulated screw. The maximum von Mises stress value at FNS was 786.83 MPa in FNS and 435.62 MPa in FNS+7.0 mm full-thread cannulated screw. The FNS group showed the highest maximum von Mises stress values at bone and FNS. For total deformation, the maximum deformation value was 10.0420 mm in FNS and 9.2769 mm in FNS+7.0 mm full-thread cannulated screws. The FNS group represented the highest maximum deformation compared to the other groups.
Conclusion
Considering the anatomical spatiality and biomechanical characteristics of the FNS in unstable femoral neck fractures, when one 7.0 mm full thread cannulated screw was also fixed to the anterosuperior portion of the FNS, significant biomechanical stability was demonstrated.
- 569 View
- 8 Download

- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- Min Sung Kwon, Young Bok Kim, Gyu Min Kong
- J Korean Fract Soc 2022;35(4):162-168. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.162
-
 Abstract
Abstract
 PDF
PDF - Purpose
Trochanteric fixation nail advanced (TFNA) was modified to compensate for the shortcomings of proximal femoral nail antirotation-II (PFNA-II). The clinical and radiological outcomes of surgeries us-ing the PFNA-II and TFNA for femoral intertrochanteric fractures were compared.
Materials and Methods
Eighty-two patients who underwent surgeries using PFNA-II or TFNA were analyzed. Only those who were followed up for more than a year were enrolled. Bone union, shortening of the femoral neck, and the tip–apex distance of the intramedullary nail were compared in the radiological findings. Clinical outcomes, including the frequency of complications and gait ability (Koval score), were also assessed.
Results
The mean follow-up periods were 22 and 19 months for the PFNA-II and TFNA groups, re-spectively. In the PFNA-II group, two cases of femoral head cut-out and one case of varus collapse were observed. In the TFNA group, only one case of femoral head cut-out was observed; however, there was no significant difference in the frequency of complications between the two groups (p=0.37). Ad-ditionally, both the shortening of the femoral neck and the decrease in gait ability after surgery showed relative improvement in the TFNA group compared to the PFNA-II group; however, there was no sig-nificant difference between the two groups.
Conclusion
The use of both TFNA and PFNA-II was associated with satisfactory outcomes. In patients who underwent surgeries using TFNA, the recovery of gait ability, frequency of complications, and short-ening of the femoral neck were not significantly different from PFNA-II, suggesting that both are suitable instrument choices for intertrochanteric fracture treatment. However, the clinical significance must be further assessed using a larger group of patients over a longer follow-up period in future studies. -
Citations
Citations to this article as recorded by- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
Jee Young Lee, Gyu Min Kong
Journal of Orthopaedic Trauma.2025; 39(7): 352. CrossRef - Clinical and Radiological Outcomes of Unstable Intertrochanteric Fractures Treated with Trochanteric Fixation Nail-Advanced and Proximal Femoral Nail Antirotation-II: Correlation between Lateral Sliding of the Helical Blade and Lateral Trochanteric Pain
Sung Yoon Jung, Myoung Jin Lee, Lih Wang, Hyeon Jun Kim, Dong Hoon Sung, Jun Ha Park
Journal of the Korean Orthopaedic Association.2024; 59(3): 208. CrossRef
- Treatment of Incompletely Displaced Femoral Neck Fractures Using Trochanteric Fixation Nail-Advanced in Patients Older Than 50 Years of Age
- 2,187 View
- 30 Download
- 2 Crossref

Case Report
- Insufficiency Fracture of Simultaneously Bilateral Femur Neck in Patient Treated with Long-Term Bisphosphonate Treatment - A Case Report -
- Seong Kee Shin, Hyung Gon Ryu, Dae Won Shin, Beom Su Han
- J Korean Fract Soc 2022;35(3):109-113. Published online July 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.3.109
-
 Abstract
Abstract
 PDF
PDF - Bisphosphonate is used widely for osteoporosis management. On the other hand, some studies have reported that prolonged use of bisphosphonate without a proper resting period can cause insufficiency fracture and, in rare cases, fractures on the femur neck. This paper reports a case of an elderly patient who suffered bilateral femur neck insufficiency fractures induced by non-stopped long-term bisphosphonate therapy. The patient complained of pain in her buttocks at the first visit. During the admission period, inguinal area pain newly developed. Both a femur neck insufficiency fracture was observed on the hip radiographic image. Hip pinning and postoperative parathyroid hormone treatment were performed. The patient was discharged without specific complications and reported improvement in symptoms on the last follow-up. Several authors have reported one-sided femoral neck insufficiency fractures due to bisphosphonate use, but the present case is uncommon in that it occurred simultaneously in both femur necks. In addition, in the case of bilateral femur fractures, the walking ability after surgery is lower than that of one-sided fracture cases, so active rehabilitation is necessary.
- 407 View
- 1 Download

Original Articles
- Mortality-Related Risk Factors in Total Hip Arthroplasty for Femoral Neck Fractures in Elderly Patients
- Jae Sung Suh, Hyung Gon Ryu, Young Ju Roh, Dae Won Shin
- J Korean Fract Soc 2022;35(2):51-56. Published online April 30, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.2.51
-
 Abstract
Abstract
 PDF
PDF - Purpose
Total hip arthroplasty (THA) using dual mobility components (DMC) is a reasonable surgical option for displaced femoral neck fractures in elderly patients, resulting in lower dislocation rates and improved stability. The purpose of this study was to investigate the clinical outcomes and risk factors responsible for mortality in elderly patients who were diagnosed with a displaced femoral neck fracture and had undergone DMC-THA.
Materials and Methods
Out of 147 cases of THA from December 2018 to June 2020, a total of 79 cases were enrolled in this study, with the following characteristics: (1) Garden stage III or IV, (2) over 75 years of age, and (3) over 1 year of follow-up. All the patients received DMC-THA surgery using the anterolateral approach.
Results
The mean follow-up period was 15.0±8.43 months and a total of one dislocation case was observed. The mortality rate was 17.7% (14/79), and it was especially higher in patients with a past medical history of malignancy (odds ratio [OR]=7.18, p=0.03) or a cognitive disorder such as dementia (OR=5.48, p=0.03). Preoperative low initial hemoglobin levels (OR=0.65, p=0.04) and low UCLA (Uni-versity of California at Los Angeles) score (OR=0.47, p=0.02) were also associated with mortality.
Conclusion
When considering THA as a treatment approach in elderly patients with a displaced femoral neck fracture, a high mortality rate is expected in patients with low preoperative hemoglobin levels or a history of malignancy or cognitive disorders. Hence, thorough monitoring and management should be undertaken before and after surgery.
- 288 View
- 24 Download

- Surgical Treatment of AO/OTA 33-C Intra-Articular Distal Femoral Fractures through Parapatellar Approach
- Suk Kyu Choo, Sung Tan Cho, Hyoung Keun Oh
- J Korean Fract Soc 2022;35(1):1-8. Published online January 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose
To report the surgical results of the parapatellar approach for AO/OTA 33-C distal femoral intra-articular fractures.
Materials and Methods
Twenty-one patients with AO/OTA 33-C distal femoral intra-articular fracture were included. There were 11 cases of C2 and 10 cases of C3 fractures. The time of union and the coronal alignment were radiographically investigated. The complications related to surgery were clinically investigated, and a functional evaluation using the range of motion and Oxford knee score was performed to compare the surgical results according to fracture classification.
Results
In all cases, sufficient articular exposure and anatomical reduction were achieved with the parapatellar approach. No cases of coronal malalignment, loss of reduction, and plate failure were noted. On the other hand, in four cases (19.0%), an autogenous bone graft was performed due to delayed union on the meta-diaphyseal fracture site. There were no differences in the radiological and clinical outcomes of the C2 and C3 fractures. The knee joint pain and Oxford knee score were poorer in the delayed union group than the normal union group.
Conclusion
The parapatellar approach is useful for achieving an anatomical reduction of the articular surface of the distal femur and minimally invasive plating technique. Although satisfactory surgical results could be obtained regardless of the degree of articular comminution, a study of the risk factors of delayed metaphyseal fusion may be necessary.
- 362 View
- 2 Download

Case Report
- Helical Blade Locking Sleeve Disassembly Following Failed Femur Intertrochanter Fracture
- Soon Ho Huh, Hong-Man Cho, Ji-Yeon Park
- J Korean Fract Soc 2021;34(3):112-116. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.112
-
 Abstract
Abstract
 PDF
PDF - A helical blade type of hip screw is used widely for the operative management of femoral trochanteric fractures. A 73-year-old female patient was admitted for femoral trochanteric fracture AO/OTA type 31A2.2. A helical blade locking sleeve dissembled 18 weeks after surgery did not achieve accurate reduction. The patient underwent bipolar hip hemiarthroplasty because the fracture reduction was lost, and it was impossible to remove the remaining helical blade without bone loss. The authors report this case of a rare complication of helical blade.
- 399 View
- 3 Download

Original Articles
- Clinical and Radiologic Outcome of Intertrochanteric Fracture Treatment Using TFNA (Trochanteric Fixation Nail-Advanced)
- Hyeon Joon Lee, Hyun Bai Choi, Ba Rom Kim, Seung Hwan Jo, Sang Hong Lee
- J Korean Fract Soc 2021;34(3):105-111. Published online July 31, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.3.105
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the clinical and radiological outcomes of TFNA (Trochanteric Fixation NailAdvanced; Depuy Synthes) for the treatment of proximal femur fractures.
Materials and Methods
This was a retrospective study of 64 patients diagnosed with a proximal femur fracture from January 2019 to November 2019. The patient’s demographic data, preoperatively and postoperatively Koval grade, modified Harris hip score, EQ-5D (Euro-Qol-5 Dimension), sliding and advancement of the blade, radiologic outcome, and complications were investigated.
Results
Fifty patients were available for evaluation at one year postoperatively. The patients reported the following: the Koval grade decreased after surgery; the modified Harris hip score decreased from 78.56±8.88 to 72.74±6.59 (p=0.149); the mean EQ-5D decreased from 0.75±0.09 to 0.72±0.06 (p=0.000). Satisfactory reduction was achieved on a postoperative radiographic examination in 47 patients in six months. Complications occurred in seven cases.
Conclusion
TFNA is considered an appropriate implant for treating intertrochanteric fractures of the femur with a minimum follow-up of one year. -
Citations
Citations to this article as recorded by- GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
Seungcheol Kwon, Minjae Lee, Heeyeon Lee, Jihyo Hwang
Journal of Clinical Medicine.2023; 12(21): 6720. CrossRef - Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
Min Sung Kwon, Young Bok Kim, Gyu Min Kong
Journal of the Korean Fracture Society.2022; 35(4): 162. CrossRef
- GS Hip Nail versus Affixus Hip Fracture Nail for the Intramedullary Nailing of Intertrochanteric Fractures
- 633 View
- 7 Download
- 2 Crossref

- Comparison of Reductions of Left and Right Proximal Portions of Intertrochanteric Fractures Treated by Intramedullary Nailing
- Hyun Cheol Oh, Joong Won Ha, Yung Park, Sang Hoon Park, Han Kook Yoon
- J Korean Fract Soc 2021;34(2):64-70. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.64
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the effect of lag screw insertion on proximal fragments by separating the right and left sides of intertrochanteric fractures in elderly patients that underwent intramedullary nailing.
Materials and Methods
Patients aged ≥65 years that underwent intramedullary nailing after a diag-nosis of intertrochanteric fractures during the period February 2012 to May 2016 were included in the study. The subjects were divided into right and left side groups. The effect of the clockwise rotational force generated when a lag screw was inserted on the proximal fragment was evaluated in both groups.
Results
In the right and left groups, most proximal fragments were located in the intramedullary canal after surgery (45 cases [75.0%] and 67 cases [73.6%], respectively). Clockwise rotation due to lag screw placement in the right group occurred in two cases (3.3%), which both showed internal rotation, and in four cases (4.4%) in the left group, all of which showed external rotation.
Conclusion
After intramedullary nailing of intertrochanteric fractures in elderly patients, proximal fragments were mostly located in the intramedullary cavity. The results obtained confirmed that the clockwise rotational force generated by lag screw insertion did not affect left or right sides. -
Citations
Citations to this article as recorded by- Which side should be taken care of when positioning a lag screw in intertrochanteric femoral fracture: right or left?
Min Uk Do, Kyeong Baek Kim, Sang-Min Lee, Hyun Tae Koo, Won Chul Shin
European Journal of Trauma and Emergency Surgery.2025;[Epub] CrossRef - Midterm Outcomes of Intramedullary Fixation of Intertrochanteric Femoral Fractures Using Compression Hip Nails: Radiologic and Clinical Results
You-Sung Suh, Jae-Hwi Nho, Min Gon Song, Dong Woo Lee, Byung-Woong Jang
Clinics in Orthopedic Surgery.2023; 15(3): 373. CrossRef
- Which side should be taken care of when positioning a lag screw in intertrochanteric femoral fracture: right or left?
- 455 View
- 3 Download
- 2 Crossref

- Comparison of the U-Blade Gamma3 Nail and the Zimmer Natural Nail for the Treatment of Intertrochanteric Fracture
- Jae Sung Suh, Hyung-Gon Ryu, Young Ju Roh, Dae Won Shin, Sang-Min Kim
- J Korean Fract Soc 2021;34(2):57-63. Published online April 30, 2021
- DOI: https://doi.org/10.12671/jkfs.2021.34.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study was performed to compare the clinical results and radiological follow-up differences between intertrochanteric fractures treated with the U-blade Gamma3 nail or the Zimmer natural nail (ZNN).
Materials and Methods
The medical records of 129 cases diagnosed with an intertrochanteric frac-ture (90 cases of U-blade Gamma3 nail, 39 cases of ZNN) from July 2015 to December 2018 were reviewed. Patients were assigned to a U-blade Gamma3 nail (n=39) or a ZNN (n=39) group. To reduce selective bias, groups were subjected to Propensity score matching by age, body mass index, bone mineral density, and fracture type. Patients that met the following criteria were excluded; age <65 years, non-ambulatory, high energy or pathologic fracture, and a follow-up of <6 months. Operation times, estimated blood losses, preoperative and postoperative Koval grades, Harris hip score and radiological lag screw positions in the femoral head, reduction quality, cut-out, tip-apex distance (TAD), lag screw sliding distances, and times to union were compared.
Results
Clinical results were similar in the two groups, but lag screw TAD was significantly greater in Ublade Gamma3 nail group (23.4 mm vs. 21.0 mm) (p=0.042). One case of cut-out occurred in the Ublade Gamma3 nail group, but no other nail-related postoperative complication was noted.
Conclusion
No significant difference was observed between the outcomes of U-blade Gamma3 nail or ZNN treatments of intertrochanteric fractures. We conclude that the U-blade confers no specific advan-tage.
- 627 View
- 8 Download

- Comparison of the Clinical and Radiographic Results between 125° and 130° Caput-Collum-Diaphyseal Angle Proximal Femoral Nail Anti-Rotation II in Patients with Intertrochanteric Fracture
- Soo Jae Yim, Yong Bok Park, Hyun Kwon Kim, Sin Hyung Park
- J Korean Fract Soc 2020;33(4):210-216. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.210
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study compared the clinical and radiographic results of two proximal femoral nail antirotation II (PFNA-II) angled by 125° and 130° in patients with intertrochanteric fractures.
Materials and Methods
From March in 2015 to September in 2016, 65 patients who underwent a closed reduction and internal fixation with PFNA-II for a femoral intertrochanteric fracture were evaluated retrospectively. The minimum follow-up period was two years. Of those, 30 and 35 patients underwent 125° angled PFNA-II and 130° angled PFNA-II, respectively. The clinical performance was evaluated using the Harris hip score, WOMAC (Western Ontario and McMaster Universities Osteoarthrtis Index), and UCLA (University of California Los Angeles) score. Radiographic analyses were performed using standardized anteroposterior and lateral radiographs to assess the implant position and quality of reduction. The blade length, distance between the blade tip and the tip of the greater trochanter, and distance between the blade tip and the most lateral protrusion point of the greater trochanter in the two groups were measured and compared.
Results
The clinical results, including the Harris hip score, WOMAC, and UCLA, were similar in the two groups at the last follow-up postoperatively. In the radiography evaluation, the implant position, quality of reduction, and the blade length were similar in the two groups. The distances between the blade tip and the tip of the greater trochanter were 52.60±3.53 mm and 58.07±5.54 mm in the 125° angled PFNA-II and 130° angled PFNA-II groups, respectively. The distance between the blade tip and the most lateral protrusion point of greater trochanter were 16.48±2.54 mm and 21.19±4.43 mm in the 125° angled PFNA-II and 130° angled PFNA-II groups, respectively. The differences were significant (p=0.031, p=0.012).
Conclusion
The operation with the 125° angled PFNA-II showed a more superior and lateral position of the blade than that with the 130° angled PFNA-II. Nevertheless, lateral thigh pain can occur when the blade is positioned superolaterally.
- 396 View
- 1 Download

- Risk Factors Affecting the Early Complications of Femoral Head Fractures
- HoeJeong Chung, Jin-Woo Lee, Dong Woo Lee, Hoon-Sang Sohn
- J Korean Fract Soc 2020;33(4):204-209. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.204
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study analyzed the prognostic factors in patients with femoral head fractures by comparing two groups with and without complications.
Materials and Methods
A retrospective study was performed on femoral head fracture patients who visited two different level-1 trauma centers from January 1, 2014 to June 30, 2018. Thirty-three patients with a follow-up period of more than one year were included. Early complications were defined as fair or poor in the Thompson–Epstein clinical evaluation criteria and grades 3 or 4 in the Kellgren– Lawrence classification within one year after the fracture. The patients were divided into two groups, with and without early complications. Statistical analysis was performed for the nominal variables with a Fisher’s exact test and continuous variables using a Mann–Whitney U test.
Results
Nine patients (27.3%) had early complications, and there were no significant differences according to age, sex, treatment method, combined fractures, Pipkin classification, and AO/OTA classification between the two groups.
Conclusion
The prognosis in femoral head fractures is difficult to predict. Therefore, the validation of existing classifications or a new classification is necessary.
- 352 View
- 1 Download

- Retrospective Comparative Study of the Intraoperative Fracture Gap Compression in the Treatment of Intertrochanteric Fracture Using Proximal Femoral Nail Antirotation
- Se Jin Kim, Hong Man Cho, Jiyeon Park, Ki Yong An, Young Woo Chung, Woojin Shin
- J Korean Fract Soc 2020;33(4):179-188. Published online October 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.4.179
-
 Abstract
Abstract
 PDF
PDF - Purpose
Intertrochanteric fractures can be treated using proximal femoral nail antirotation (PFNA). This study examined the clinical and radiological results of the intraoperative fracture compression.
Materials and Methods
Ninety-four patients underwent intraoperative compression (Group I), and 88 patients underwent natural sliding only (Group II). The patients were followed-up for more than two years. All patients met the following seven conditions: (1) AO/OTA 31-A1, A2 type intertrochanter fracture, (2) availability of compression of more than one cortical bone in the anterior or medial region of the fracture site under the preoperative imaging test, (3) Singh index grade ≥3, (4) blade position: center-center, center-inferior, (5) tip-apex distance <25 mm, (6) reduction status of good or very good, and (7) positive or neutral medial cortical support position with slightly valgus reduction.
Results
A slight tendency toward significant differences in acute phase pain between the two groups was observed at six weeks postoperatively (p=0.073). Twenty-four months after surgery, lateral extension of the PFNA helical blade between the two groups showed significant differences (p=0.017). Fracture gaps measured immediately after surgery showed significant differences (p=0.001), and a clear tendency for a significant difference in the average fracture union time was found (p=0.065).
Conclusion
Intraoperative fracture compression, intraoperative fracture compression appears beneficial to achieve a successful union of trochanteric fractures provided that all conditions are met to apply the method safely. -
Citations
Citations to this article as recorded by- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
Se Jin Kim, Hong-Man Cho, Myung Cheol Jung
Journal of the Korean Fracture Society.2022; 35(4): 151. CrossRef
- Benefits of a Demineralized Bone Matrix in Osteoporotic Intertrochanteric Femoral Fracture Patients
- 511 View
- 3 Download
- 1 Crossref

Case Reports
- Rendezvous Surgery for Peri-Implant Fractures around Locking Compression Plate on Anterolateral Bowed Femur - A Case Report -
- Hong Man Cho, Jiyeon Park
- J Korean Fract Soc 2020;33(3):159-163. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.159
-
 Abstract
Abstract
 PDF
PDF - An 84-year-old female visited with an intertrochanteric femoral fracture. The patient had undergone an open reduction and internal fixation with a compressive plate and elastic nail in an ipsilateral atypical diaphyseal femoral fracture in the past. Compressive plate and elastic nail remained, and anterolateral bowing was presented. To treat the periprosthetic trochanteric fracture, a proximal femoral nail was used without removing the previously inserted compressive plate. Under the “rendezvous” technique, using a combination of fixating intramedullary nail and compressive plate simultaneously, the distal screw was fixed, and a femoral head lag screw was inserted after reducing the fracture. Complete union of the fracture was achieved 16 months after the operation, and a decrease in mobility function was not found postoperatively. The authors report this case for the “rendezvous” technique as a treatment option for elderly patients with periprosthetic trochanteric fractures, who had previously undergone surgical treatment for ipsilateral atypical diaphyseal femoral fractures with anterolateral bowing.
- 328 View
- 3 Download

- Rare Experience of Bilateral Femoral Neck and Shaft Fractures - A Case Report -
- DaeHyun Choe, Jae-Ho Lee, Ki-Chul Park
- J Korean Fract Soc 2020;33(3):154-158. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.154
-
 Abstract
Abstract
 PDF
PDF - Ipsilateral fractures of the femoral neck and shaft are relatively common injuries and accompany 2% to 9% of all femoral shaft fractures. On the other hand, it is extremely rare for these injuries to occur bilaterally. This paper reports the authors’ experience of a case with bilateral femoral neck and shaft fractures. The patient sustained multiple injuries, including liver laceration with hemoperitoneum, bilateral open fractures of the tibia, and bilateral femoral neck, and shaft fractures caused by a high-speed motor vehicle accident. Under the circumstances, damage-control orthopedic principles were applied, and external fixators were initially placed. After the patient’s general condition showed improvement, both femurs were fixed with a reconstruction nail. Fracture healing was achieved without complications, such as avascular necrosis of the femoral head. Despite the rare occurrence, this paper describes this case because these injuries must be managed with meticulous attention.
- 352 View
- 7 Download

Original Articles
- Clinical and Radiological Outcomes of Polished Cemented Bipolar Hemiarthroplasty for Intertrochanteric Fractures in Elderly Patients
- Suc-Hyun Kweon, Chang-Hyun Shin, Yeong-Chang Lee, Min-Woo Kim, Tae-Ho Kim
- J Korean Fract Soc 2020;33(3):134-141. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.134
-
 Abstract
Abstract
 PDF
PDF - Purpose
To evaluate the clinical and radiological outcomes of bipolar hemiarthroplasty using a polished cemented femoral stem for intertrochanteric fractures in elderly patients.
Materials and Methods
From July 2005 to May 2015, 48 patients diagnosed with intertrochanteric fractures underwent bipolar hemiarthroplasty. The mean age and follow-up period were 80.5 years and 30.5 months, respectively. The postoperative results were evaluated clinically and radiologically.
Results
The mean operation time was 100 minutes (range, 90-120 minutes), and the mean amount of blood loss was 334 ml (range, 170-500 ml). At the last follow-up, the mean Harris hip score (HHS), visual analogue scale (VAS), and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores were 82.2 (range, 76-90), 0.8 (range, 1-3), and 36 (range, 30-40), respectively. Walking was initiated using a walker for partial weight-bearing, and the mean walking time was 5.8 days (range, 3-14 days). Ambulatory ability was restored to a walking state before the injury in 36 cases (75.0%), and wheelchair ambulation was possible in 12 cases (25.0%). The instrumental activities of daily living (IADLs) were 17 patients (35.4%), and the basic activities of daily living (BADLs) were 31 patients (64.6%).
Conclusion
Polished cemented bipolar hemiarthroplasty can achieve secure fixation with no postoperative thigh pain. Restoring the preoperative walking ability will be more helpful for intertrochanteric fractures in elderly patients.
- 388 View
- 2 Download

- Three-Dimensional Analysis of the Morphological Features in the Femur of Atypical Fracture and Practical Implications of Intramedullary Nailing
- Yong Uk Kwon, Kyung-Jae Lee, Joo Young Choi, Gu-Hee Jung
- J Korean Fract Soc 2020;33(2):87-95. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.87
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study analyzed the morphological features of the contralateral femur without an atypical fracture by constructing a three-dimensional model with an actual size medullary canal.
Materials and Methods
Lateral and anterior bowing of the shaft were measured for 21 models, and the shape of the medullary canal was analyzed. To eliminate the projection error, the anteroposterior (AP) femur was rotated internally to the extent that the centerline of the head and neck, which is the ideal position of cephalomedullary nail screw, was neutral, and the lateral femur matched the medial and lateral condyle exactly.
Results
The lateral bowing and anterior bowing was an average of 5.5° (range, 2.8°-10.7°; standard deviation [SD], 2.4°) and 13.1° (range, 6.2°-21.4°; SD, 3.2°), respectively. In the area where lateral bowing increased, the lateral cortex became thicker, and the medullary canal was straightened. On the lateral femur, the anterior angle was increased significantly, and the diameter of curvature averaged 1,370.2 mm (range, 896-1,996 mm; SD, 249.5 mm).
Conclusion
Even if the anterolateral bowing increases in the atypical femur, the medullary canal tends to be straightened in the AP direction. So, it might be considered as a reference to the modification of an intramedullary nail to increase the conformity.
- 347 View
- 4 Download

- Analysis of the Changes in Femoral Varus Bowing and the Factors Affecting Nonunion for the Treatment of Femoral Shaft Fractures over 60 Years Old Using Piriformis Fossa Insertion Intramedullary Nailing
- Yonghan Cha, Chan Ho Park, Jun-Il Yoo, Jung-Taek Kim, WooSuk Kim, Ha-Yong Kim, Won-Sik Choy
- J Korean Fract Soc 2020;33(2):65-71. Published online April 30, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.2.65
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the bony morphological changes to analyze the factors affecting bony union in the treatment of elderly femoral shaft fractures with varus bowing using piriformis fossa insertion intramedullary nailing.
Materials and Methods
This study included 26 patients over 60 years of age, who were admitted for femoral shaft fractures between January 2005 and December 2014 and treated with piriformis fossa insertion intramedullary nailing. Age, sex, height, weight, bone mineral density, injury mechanism, fracture type, diameter and length of the nail, postoperative lengthening of the femur, postoperative change in varus angle, contact between the lateral and anterior cortex, and the gap between the fracture line and the bony union were checked. The patients were divided into a varus group and nonvarus group, as well as a bone union group and nonunion group. Logistic regression analysis was performed to analyze the factors affecting nonunion.
Results
The patients were classified into 11 in the varus group and 15 in the non-varus group and 24 in the union group and 2 in the nonunion group. The varus group showed a larger increase in leg length and varus angle reduction than the non-varus group (p<0.05). The union group had more contact with the lateral cortical bone than that of the nonunion group (p<0.05). The factor affecting bone union in regression analysis was contact of the lateral cortical bone (p<0.05).
Conclusion
Treatment of a femoral shaft fracture in elderly patients with a varus deformity of the femur using piriformis fossa insertion intramedullary nail increases the length of the femur and decreases the varus deformity. For bony union, the most important thing during surgery is contact of the lateral cortical bone with the fracture site. -
Citations
Citations to this article as recorded by- Straight nail insertion through a laterally shifted entry for diaphyseal atypical femoral fractures with bowing: good indications and limitations of this technique
Seong-Eun Byun, Young-Ho Cho, Young-Kyun Lee, Jung-Wee Park, Seonguk Kim, Kyung-Hoi Koo, Young Soo Byun
International Orthopaedics.2021; 45(12): 3223. CrossRef
- Straight nail insertion through a laterally shifted entry for diaphyseal atypical femoral fractures with bowing: good indications and limitations of this technique
- 724 View
- 3 Download
- 1 Crossref

Review Article
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty
- Jung Hoon Choi, Jong Hyuk Jeon, Kyung Jae Lee
- J Korean Fract Soc 2020;33(1):43-51. Published online January 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.1.43
-
 Abstract
Abstract
 PDF
PDF - Although the incidence of postoperative periprosthetic femoral fractures after hip arthroplasty is expected to increase, these complex fractures are still challenging complications. To obtain optimal results for these fractures, thorough clinical and radiographic evaluation, precise classification, and understanding of modern management principles are mandatory. The Vancouver classification system is a simple, effective, and reproducible method for planning proper treatments of these injuries. The fractures associated with a stable femoral stem can be effectively treated with osteosynthesis, though periprosthetic femoral fractures associated with a loose stem require revision arthroplasty. We describe here the principles of proper treatment for the patients with periprosthetic femoral fractures as well as how to avoid complications.
- 991 View
- 6 Download

Original Articles
- Failure of Intramedullary Nailing for Subtrochanteric Atypical Femoral Fractures Caused by Endosteal Cortical Thickening
- Young Ho Roh, Kimoon Kang, Hee Joong Kim, Kwang Woo Nam
- J Korean Fract Soc 2019;32(4):211-221. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.211
- Correction in: J Musculoskelet Trauma 2020;33(1):63
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Recent literature has noted incidences of subtrochanteric atypical femoral fractures (AFFs) in patients who have taken long-term bisphosphonates (BPs). Most cases of subtrochanteric AFFs have been treated with intramedullary nailing and cases of delayed union have been reported. On the other hand, there is no data available on the complications associated with endosteal thickening or cortical thickening. This study evaluated the results of surgical treatment according to the endosteal thickening of the lateral cortex in subtrochanteric AFFs.
MATERIALS AND METHODS
Investigation was performed at the Department of Orthopaedic Surgery, Jeju National University Hospital. The study consisted of patients with subtrochanteric AFFs, defined by the American Society for Bone and Mineral Research (ASBMR) major criteria, who underwent intramedullary nailing from March 2012 to October 2014. The cases were categorized into two groups based on the presence of endosteal thickening. The evaluation included the demographic data, radiographic data of initial reduction state, and duration of BPs.
RESULTS
The demographic data and duration of BPs were similar in the two groups. On the other hand, varus reduction (Group I: 12.5% vs. Group II: 78.9%; p=0.001), delayed union (Group I: 0% vs. Group II: 70.0%; p=0.003), nonunion (Group I: 0% vs. Group II: 47.4%; p=0.017), and union time (Group I: 5.5 months vs. Group II: 8.3 months; p<0.001) were significantly different in the two groups.
CONCLUSION
Endosteal thickening of the lateral cortex in subtrochanteric AFFs was identified as an independent factor that decides the reduction of the fracture and nonunion. The endosteal thickening should be removed to obtain anatomical alignment for successful surgical results. -
Citations
Citations to this article as recorded by- Controlled bending of proximal femoral nails used in fractures of bowed femurs: biomechanical study with clinical application
Hong Moon Sohn, Suenghwan Jo
Medical Biological Science and Engineering.2022; 5(2): 63. CrossRef
- Controlled bending of proximal femoral nails used in fractures of bowed femurs: biomechanical study with clinical application
- 717 View
- 3 Download
- 1 Crossref

- Outcomes following Treatment of Geriatric Distal Femur Fractures with Analyzing Risk Factors for the Nonunion
- Soo young Jeong, Jae Ho Lee, Ki Chul Park
- J Korean Fract Soc 2019;32(4):188-195. Published online October 31, 2019
- DOI: https://doi.org/10.12671/jkfs.2019.32.4.188
- Correction in: J Musculoskelet Trauma 2020;33(1):62
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
Many international journals have published studies on the results of distal femoral fractures in elderly people, but only a few studies have been conducted on the Korean population. The aim of this study was to determine the factors that are associated with the outcomes and prognosis of fixation of distal femur fractures using the minimally invasive plate osteosynthesis (MIPO) technique in elderly patients (age≥60) and to determine the risk factors related witht he occurrence of nonunion.
MATERIALS AND METHODS
This study is a retrospective study. From January 2008 to June 2018, distal femur fracture (AO/OTA 33) patients who underwent surgical treatment (MIPO) were analyzed. A total of 52 patients were included in the study after removing 121 patients that met with the exclusion criteria. Medical records, including surgical records, were reviewed to evaluate the patients' underlying disease, bone mineral density, the number of days delayed from surgery, complications and mortality. In addition, follow-up radiographs were used to determine bone union, delayed union and nonunion.
RESULTS
The average time to achieve bone union was 19.95 weeks, the rate of nonunion was 20.0% (10/50) and the overall mortality was 3.8% (2/52). There were no significant differences in the clinical and radiological results of those patients with or without periprosthetic fracture. On the univariate analysis, which compared the union group vs. the nonunion group, no factors were identified as significant risk factors for nonunion. On the multiple logistic regression analysis, medical history of cancer was identified as a significant risk factor for nonunion (p=0.045).
CONCLUSION
The rate of nonunion is high in the Korean population of elderly people suffering from distal femur fracture, but the mortality rate appears to be low. A medical history of cancer is a significant risk factor for nonunion. Further prospective studies are required to determine other associated factors. -
Citations
Citations to this article as recorded by- Comparison of Clinical Outcomes for Femoral Neck System and Cannulated Compression Screws in the Treatment of Femoral Neck Fracture
Jae Kwang Hwang, KiWon Lee, Dong-Kyo Seo, Joo-Yul Bae, Myeong-Geun Song, Hansuk Choi
Journal of the Korean Fracture Society.2023; 36(3): 77. CrossRef
- Comparison of Clinical Outcomes for Femoral Neck System and Cannulated Compression Screws in the Treatment of Femoral Neck Fracture
- 764 View
- 6 Download
- 1 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


