Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(2); 2020 > Article
- Original Article Analysis of the Changes in Femoral Varus Bowing and the Factors Affecting Nonunion for the Treatment of Femoral Shaft Fractures over 60 Years Old Using Piriformis Fossa Insertion Intramedullary Nailing
- Yonghan Cha, Chan Ho Park, Jun-Il Yoo, Jung-Taek Kim, WooSuk Kim, Ha-Yong Kim, Won-Sik Choy
-
Journal of Musculoskeletal Trauma 2020;33(2):65-71.
DOI: https://doi.org/10.12671/jkfs.2020.33.2.65
Published online: April 30, 2020

2Department of Orthopedic Surgery, Yeungnam University Medical Center, Daegu, Korea

3Department of Orthopedic Surgery, Gyeongsang National University Hospital, Jinju, Korea

4Department of Orthopedic Surgery, Ajou University Medical Center, Suwon, Korea

- 886 Views
- 3 Download
- 1 Crossref
- 0 Scopus
Abstract
Purpose
This study examined the bony morphological changes to analyze the factors affecting bony union in the treatment of elderly femoral shaft fractures with varus bowing using piriformis fossa insertion intramedullary nailing.
Materials and Methods
This study included 26 patients over 60 years of age, who were admitted for femoral shaft fractures between January 2005 and December 2014 and treated with piriformis fossa insertion intramedullary nailing. Age, sex, height, weight, bone mineral density, injury mechanism, fracture type, diameter and length of the nail, postoperative lengthening of the femur, postoperative change in varus angle, contact between the lateral and anterior cortex, and the gap between the fracture line and the bony union were checked. The patients were divided into a varus group and nonvarus group, as well as a bone union group and nonunion group. Logistic regression analysis was performed to analyze the factors affecting nonunion.
Results
The patients were classified into 11 in the varus group and 15 in the non-varus group and 24 in the union group and 2 in the nonunion group. The varus group showed a larger increase in leg length and varus angle reduction than the non-varus group (p<0.05). The union group had more contact with the lateral cortical bone than that of the nonunion group (p<0.05). The factor affecting bone union in regression analysis was contact of the lateral cortical bone (p<0.05).
Conclusion
Treatment of a femoral shaft fracture in elderly patients with a varus deformity of the femur using piriformis fossa insertion intramedullary nail increases the length of the femur and decreases the varus deformity. For bony union, the most important thing during surgery is contact of the lateral cortical bone with the fracture site.
Published online Apr 28, 2020.
https://doi.org/10.12671/jkfs.2020.33.2.65
Analysis of the Changes in Femoral Varus Bowing and the Factors Affecting Nonunion for the Treatment of Femoral Shaft Fractures over 60 Years Old Using Piriformis Fossa Insertion Intramedullary Nailing
 , M.D.,
Chan Ho Park
, M.D.,
Chan Ho Park , M.D.,*
Jun-Il Yoo
, M.D.,*
Jun-Il Yoo , M.D.,†
Jung-Taek Kim
, M.D.,†
Jung-Taek Kim , M.D.,‡
WooSuk Kim
, M.D.,‡
WooSuk Kim , M.D.,
Ha-Yong Kim
, M.D.,
Ha-Yong Kim , M.D., Ph.D.
and Won-Sik Choy
, M.D., Ph.D.
and Won-Sik Choy , M.D., Ph.D.
, M.D., Ph.D.
Abstract
Purpose
This study examined the bony morphological changes to analyze the factors affecting bony union in the treatment of elderly femoral shaft fractures with varus bowing using piriformis fossa insertion intramedullary nailing.
Materials and Methods
This study included 26 patients over 60 years of age, who were admitted for femoral shaft fractures between January 2005 and December 2014 and treated with piriformis fossa insertion intramedullary nailing. Age, sex, height, weight, bone mineral density, injury mechanism, fracture type, diameter and length of the nail, postoperative lengthening of the femur, postoperative change in varus angle, contact between the lateral and anterior cortex, and the gap between the fracture line and the bony union were checked. The patients were divided into a varus group and nonvarus group, as well as a bone union group and nonunion group. Logistic regression analysis was performed to analyze the factors affecting nonunion.
Results
The patients were classified into 11 in the varus group and 15 in the non-varus group and 24 in the union group and 2 in the nonunion group. The varus group showed a larger increase in leg length and varus angle reduction than the non-varus group (p<0.05). The union group had more contact with the lateral cortical bone than that of the nonunion group (p<0.05). The factor affecting bone union in regression analysis was contact of the lateral cortical bone (p<0.05).
Conclusion
Treatment of a femoral shaft fracture in elderly patients with a varus deformity of the femur using piriformis fossa insertion intramedullary nail increases the length of the femur and decreases the varus deformity. For bony union, the most important thing during surgery is contact of the lateral cortical bone with the fracture site.
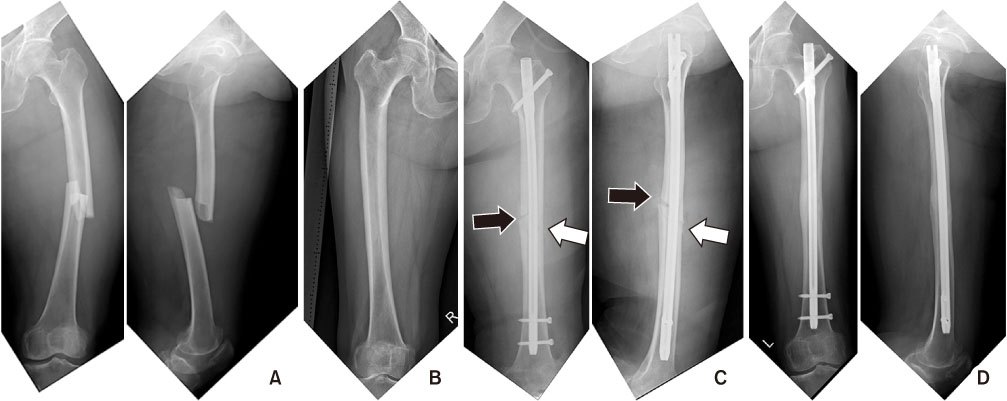
Fig. 1
(A) A 72-year-old female had a femoral diaphyseal fracture. (B) There are more than 5° of femoral bowing on the contralateral radiograph. (C) Radiographs after fracture fixation using an intramedullary nail. Bony contacts are observed at the anterior and lateral cortex of the fracture site (white arrows). On the other hand, fracture gaps are observed at the posterior and medial cortex of fracture sites (black arrows). (D) These are radiographs at postoperative 1-year, and the complete bone union is observed.
Fig. 2
(A) A 65-year-old female had an atypical femoral diaphyseal fracture. (B) There was more than 5° of femoral bowing on the right radiograph. (C) Radiographs after fracture fixation using an intramedullary nail. Bony contacts are observed at the anterior and lateral cortex of the fracture site (white arrows). On the other hand, fracture gaps were observed at the posterior and medial cortex of fracture sites (black arrows). (D) These are radiographs at postoperative 1-year, and the complete bone union was observed.
Fig. 3
Radiograph showing that the medial fracture gap widened after the femoral diaphyseal fracture fixed by an intramedullary nail. The white arrow means the length of the gap at the medial fracture cortex.
Table 1
Comparison between the Varus Bowing Group and the Non-Varus Bowing Group
Table 2
Comparison of the Nonunion Group and Union Bowing Group
Financial support:None.
Conflict of interests:None.
References
-
Karakaş HM, Harma A. Femoral shaft bowing with age: a digital radiological study of Anatolian Caucasian adults. Diagn Interv Radiol 2008;14:29–32.
-
-
Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg. Hong Kong 2007;15:32–36.
-
-
Iagulli ND, Mallory TH, Berend KR, et al. A simple and accurate method for determining leg length in primary total hip arthroplasty. Am J Orthop. Belle Mead NJ 2006;35:455–457.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS





 Cite
Cite

