Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(3); 2020 > Article
- Case Report Rendezvous Surgery for Peri-Implant Fractures around Locking Compression Plate on Anterolateral Bowed Femur - A Case Report -
- Hong Man Cho, Jiyeon Park
-
Journal of Musculoskeletal Trauma 2020;33(3):159-163.
DOI: https://doi.org/10.12671/jkfs.2020.33.3.159
Published online: July 31, 2020
- 491 Views
- 3 Download
- 0 Crossref
- 0 Scopus
Abstract
An 84-year-old female visited with an intertrochanteric femoral fracture. The patient had undergone an open reduction and internal fixation with a compressive plate and elastic nail in an ipsilateral atypical diaphyseal femoral fracture in the past. Compressive plate and elastic nail remained, and anterolateral bowing was presented. To treat the periprosthetic trochanteric fracture, a proximal femoral nail was used without removing the previously inserted compressive plate. Under the “rendezvous” technique, using a combination of fixating intramedullary nail and compressive plate simultaneously, the distal screw was fixed, and a femoral head lag screw was inserted after reducing the fracture. Complete union of the fracture was achieved 16 months after the operation, and a decrease in mobility function was not found postoperatively. The authors report this case for the “rendezvous” technique as a treatment option for elderly patients with periprosthetic trochanteric fractures, who had previously undergone surgical treatment for ipsilateral atypical diaphyseal femoral fractures with anterolateral bowing.
Published online Jul 24, 2020.
https://doi.org/10.12671/jkfs.2020.33.3.159
Rendezvous Surgery for Peri-Implant Fractures around Locking Compression Plate on Anterolateral Bowed Femur: A Case Report
 , M.D.,
and Jiyeon Park
, M.D.,
and Jiyeon Park , M.D.
, M.D.
Abstract
An 84-year-old female visited with an intertrochanteric femoral fracture. The patient had undergone an open reduction and internal fixation with a compressive plate and elastic nail in an ipsilateral atypical diaphyseal femoral fracture in the past. Compressive plate and elastic nail remained, and anterolateral bowing was presented. To treat the periprosthetic trochanteric fracture, a proximal femoral nail was used without removing the previously inserted compressive plate. Under the “rendezvous” technique, using a combination of fixating intramedullary nail and compressive plate simultaneously, the distal screw was fixed, and a femoral head lag screw was inserted after reducing the fracture. Complete union of the fracture was achieved 16 months after the operation, and a decrease in mobility function was not found postoperatively. The authors report this case for the “rendezvous” technique as a treatment option for elderly patients with periprosthetic trochanteric fractures, who had previously undergone surgical treatment for ipsilateral atypical diaphyseal femoral fractures with anterolateral bowing.
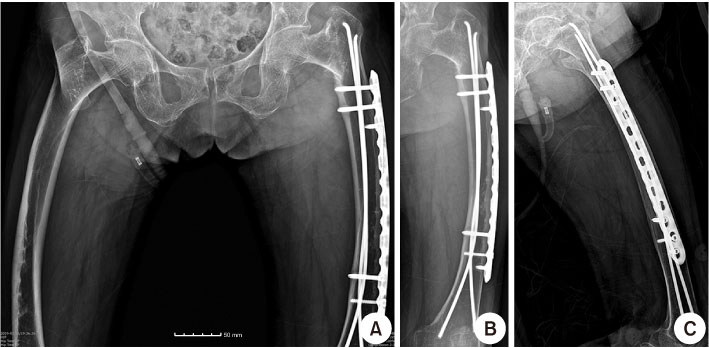
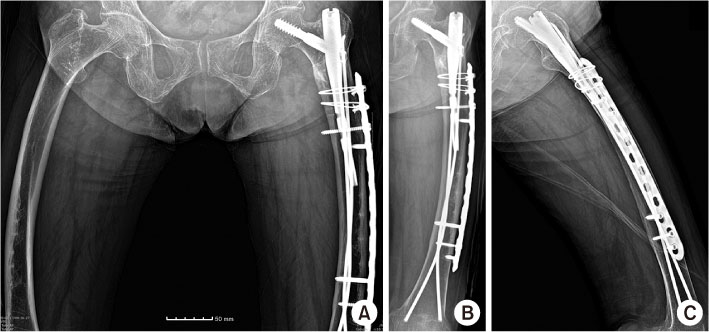
Fig. 1
Simple radiograph of total hip anteroposterior (AP) (A), left femur AP (B), and lateral (C), intertrochanteric femoral fracture AO Foundation/Orthopaedic Trauma Association classification 31-A2 fracture in the left femur with anterolateral bowing and complete union of a previous atypical diaphyseal fracture. A decrease in bone density in the lateral cortex of the femur and pull-out of the distal screw of the compression plate can be found in the left femur AP and lateral (B, C).
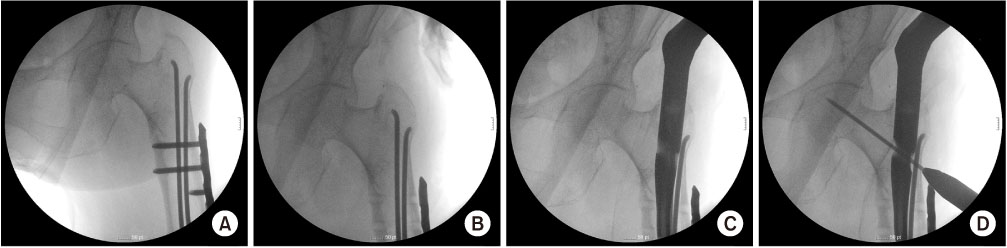
Fig. 2
(A) In the C-arm image intensifier image, stable reduction of a trochanteric fracture was achieved. (B) Three screws inserted in the proximal hole of the compression plate, which can be interrupted for insertion of the proximal femoral nail, were removed. (C) A compression hip nail was inserted successfully without interrupting previously inserted elastic nails. (D) A guidewire for the femoral head lag screw was inserted.
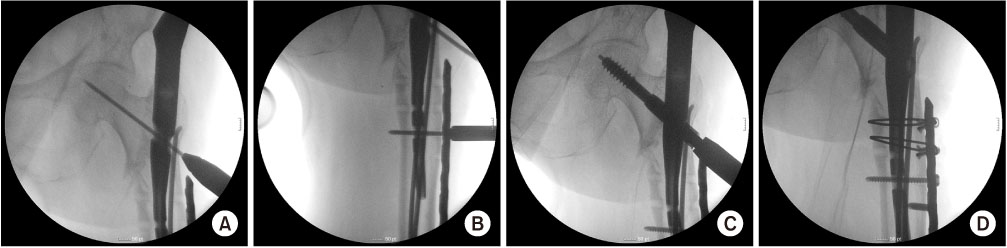
Fig. 3
(A) In the C-arm image intensifier image, a guidewire for the femoral head lag screw was inserted in the center-center position of the femoral head and fixed primarily. (B) A distal screw was inserted, achieving simultaneous fixation of compression plate and compression hip nail. (C) After reaming the femoral head, the lag screw of the femoral head was inserted. (D) For the three screws removed in the proximal compression plate, an additional screw was inserted for the most distal hole, and AO cable wiring was performed for two proximal removed screw holes.
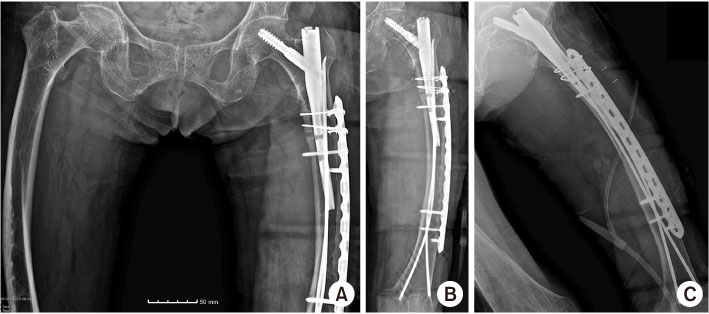
Fig. 4
In the postoperative simple radiograph, successful reduction of the femoral trochanteric fracture can be found in the total hip anteroposterior (AP) (A), left femur AP (B), and lateral (C).
Fig. 5
Sixteen months after the operation, complete union of the femoral trochanteric fracture can be found in the total hip anteroposterior (AP) (A), left femur AP (B), and lateral (C).
Financial support:None.
Conflict of interests:None.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 Cite
Cite

