Search
- Page Path
- HOME > Search
Original Article
- Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
- Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
- J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00276
-
 Abstract
Abstract
 PDF
PDF - Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
Methods
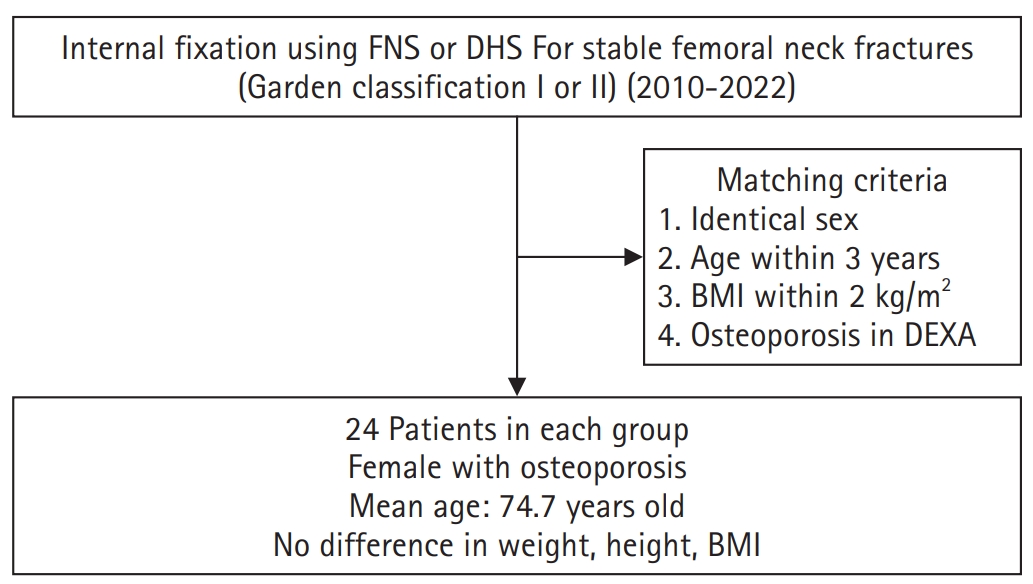
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results. Level of evidence: IV.
- 1,217 View
- 17 Download

Review Article
- Atypical ulnar fractures: a narrative review of current concepts and a case of bilateral surgical management
- Chi-Hoon Oh, Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):124-132. Published online July 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00227
-
 Abstract
Abstract
 PDF
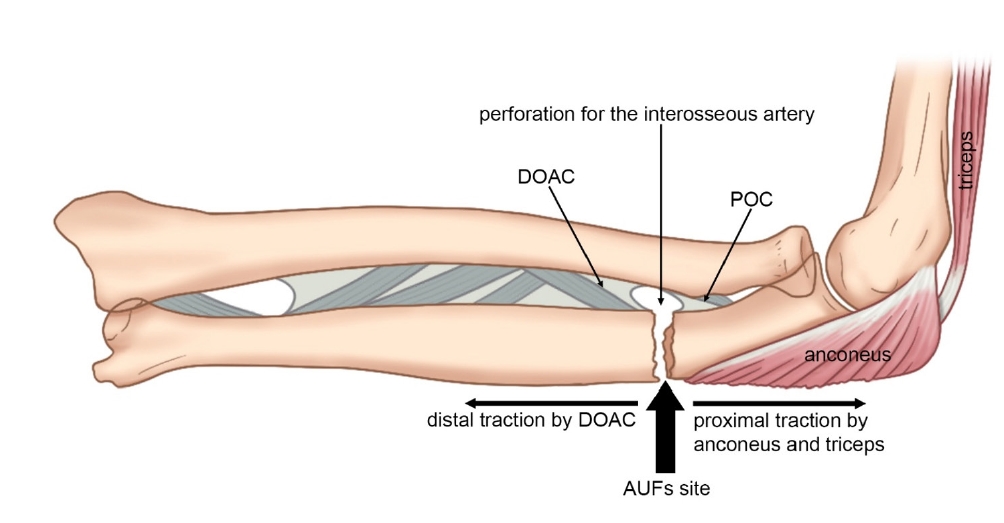
PDF - Atypical ulnar fractures (AUFs) are rare complications that are often linked to long-term antiresorptive therapy. Although atypical femoral fractures are well-studied, AUFs lack standardized diagnostic and treatment protocols. This review summarizes current knowledge on AUFs, including their pathophysiology, diagnostic criteria, and management. A case of bilateral AUFs treated with two distinct osteosynthesis methods is presented, emphasizing the principles of biological healing and mechanical stabilization.
- 1,397 View
- 39 Download

Original Articles
- Comparison of outcomes of reinforced tension band wiring and precontoured plate and screw fixation in the management of Mayo type IIIB olecranon fractures
- Hyun Goo Kang, Tong Joo Lee, Samuel Jaeyoon Won
- J Musculoskelet Trauma 2025;38(2):96-101. Published online February 28, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00059
- Correction in: J Musculoskelet Trauma 2025;38(3):168
-
 Abstract
Abstract
 PDF
PDF - Background
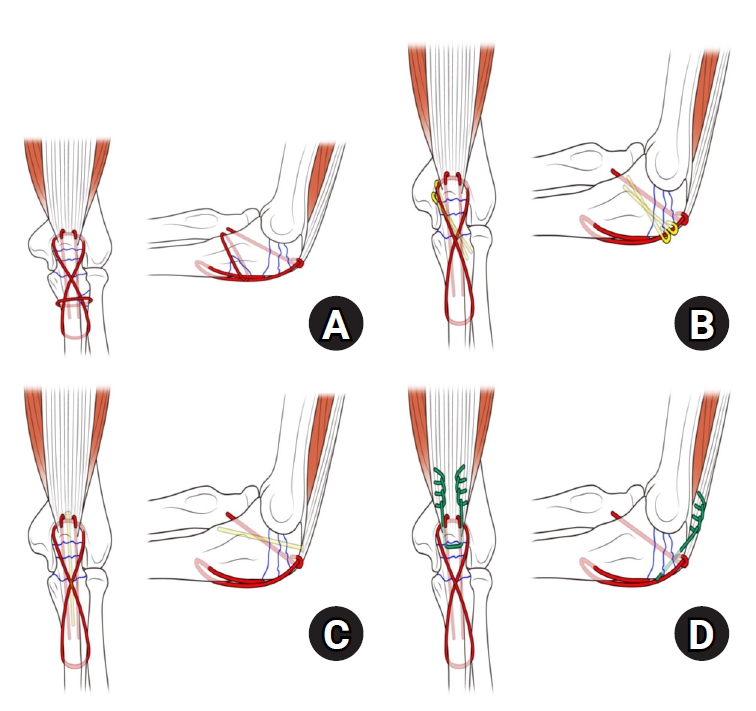
Mayo type IIIB olecranon fractures are characterized by significant displacement and comminution, presenting a challenge in selecting the appropriate fixation technique. This study compared the clinical and radiographic outcomes, complications, and reoperation rates of reinforced tension band wiring (TBW) and precontoured plate and screw fixation (PF) in the surgical treatment of Mayo type IIIB olecranon fractures.
Methods
This retrospective review analyzed 24 patients diagnosed with Mayo type IIIB olecranon fractures, who were treated between 2005 and 2023. Of these, 11 patients underwent reinforced TBW, and 13 received precontoured PF. Clinical outcomes were assessed using Disabilities of the Arm, Shoulder, and Hand (DASH) scores and the Mayo Elbow Performance Score (MEPS). Radiographic outcomes focused on fracture union. Operative times, complication rates, and reoperation rates were compared between the groups.
Results
Both the reinforced TBW and PF groups achieved satisfactory clinical outcomes, with no significant between-group differences in DASH and MEPS scores (P>0.05). Radiographic union was achieved in all patients. The reinforced TBW group demonstrated a significantly shorter operative time than the PF group (93.6±7.4 min vs. 132.3±13.7 min; P<0.001). Complication rates were similar between the two groups (reinforced TBW, 38.4%; PF, 36.3%), but hardware-related irritation occurred more frequently in the reinforced TBW group. Reoperations were required in 15.8% of the reinforced TBW group due to hardware irritation, whereas no reoperations were necessary in the PF group.
Conclusions
Reinforced TBW and PF are both effective surgical options for managing Mayo type IIIB olecranon fractures, yielding comparable clinical and radiographic outcomes. While reinforced TBW offers shorter operative times and lower costs, PF is associated with fewer hardware-related complications. Further prospective studies are needed to optimize treatment strategies for these complex fractures. Level of Evidence: Level III. -
Citations
Citations to this article as recorded by- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
Reva Qiu, Mallika Makkar, Richard Buckley
Injury.2025; 56(11): 112769. CrossRef
- Are posterior olecranon locking plates a problem for patients after fracture healing because of prominence?
- 2,039 View
- 46 Download
- 1 Crossref

- Outcomes of open reduction and internal fixation using 2.0/2.4 mm locking compression plate in isolated greater tuberosity fractures of humerus
- Sung Choi, Dongju Shin, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2025;38(1):32-39. Published online January 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00005

-
 Abstract
Abstract
 PDF
PDF - Background
The purpose of this study was to retrospectively evaluate the radiographic and clinical results of a small single or double low-profile plate fixation of 2.0/2.4 mm locking compression plate (LCP) in treating isolated greater tuberosity (GT) fractures of the humerus. Methods: From June 2015 to October 2022, patients who underwent LCP in treating isolated GT fractures of the humerus were included in this study. The radiological and clinical results were analyzed in 15 patients who underwent open reduction and internal fixation used 2.0/2.4 mm LCP. Results: Bone union was achieved in 14 patients (93.3%) and one failed case was treated with a 2.4 mm single LCP fixation. Radiological union was achieved within 10–20 weeks. Complications occurred in two patients (13.3%), including the reduction failure and shoulder stiffness. At the final follow-up, the average clinical scores were as follows: a visual analog scale for pain of 2.1 (range, 0–5) and a University of California, Los Angeles score of 27.2 (range, 18–31). Regarding range of motion (ROM), the average active ROMs were 142° for forward flexion (range, 120°–150°), 147.1° for abduction (range, 120°– 180°), and 59.3° for external rotation (range, 45°–80°). For internal rotation, the average was observed to reach the 10th thoracic vertebra (range, 1st lumbar vertebra–7th thoracic vertebra). Conclusions: The clinical and radiologic outcomes of treating isolated GT fracture using 2.0/2.4 mm LCP were favorable, and double low-profile plate fixation may be beneficial for sufficient fracture stability if possible. Level of evidence: Level IV, case series.
- 1,725 View
- 54 Download

- Risk Factors of Fixation Failure in Femoral Neck Fractures
- Sung Hyun Yoon, Kyu Beom Kim, Hyung Jun Lee, Kyung Wook Kim
- J Korean Fract Soc 2023;36(4):118-124. Published online October 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.4.118
-
 Abstract
Abstract
 PDF
PDF - Purpose
Internal fixation after a femoral neck fracture (FNF) is one of the conventional treatment options for the young and active elderly patients. However, fixation failure of internal fixation is a probable complication. The treatment of fixation failure after a primary internal fixation of the FNF remains a challenge.
Materials and Methods
Between July 2002 and March 2017, 83 patients who underwent internal fixation after FNF were retrospectively analyzed. Radiological assessments, including Pauwels’ angle, fracture level, reduction quality, and bone union, were measured, preoperatively and postoperatively. Moreover, intraoperative variables such as time to surgery, surgical time, and estimated blood loss were also evaluated.
Results
The patients were divided into the fixation failure and the non-failure groups. Among the 83 patients, 17 cases (20.5%) of fixation failure after the primary internal fixation of the FNF were identi-fied. When comparing the two groups according to the radiographic data, Pauwels’ angle and the reduction quality based on Garden’s angle showed significant differences (p<0.001). Moreover, when comparing the intraoperative variables, unlike the surgical time and estimated blood loss, significant differences were noted in the time interval from injury to surgery and specifically in whether the surgery was performed within 12 hours after injury (p<0.001).
Conclusion
Pauwels’ angle, reduction quality, and time to surgery are the major factors that can predict the possibility of internal fixation failure of the FNF. Early and accurate anatomical reduction is needed to decrease complications after the internal fixation of the FNF.
- 2,390 View
- 27 Download

- Does the Use of a Silicone Ring Tourniquet Help Reduce Bleeding in the Minimally Invasive Internal Fixation with Locking Plate for Distal Femoral Fractures?
- Ki-Bong Park, Hong-Ki Jin, Il-Yeong Hwang, Sung-Who Chang, Sung-Cheon Na
- J Korean Fract Soc 2020;33(3):148-153. Published online July 31, 2020
- DOI: https://doi.org/10.12671/jkfs.2020.33.3.148
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the usefulness of a silicone ring tourniquet by analyzing the changes in the perioperative hemoglobin (Hb) levels or amount of perioperative bleeding compared to those of a pneumatic tourniquet or no usage during minimally invasive plate fixation for distal femoral fractures.
Materials and Methods
From January 2017 to December 2019, 30 patients who underwent minimally invasive plate fixation using a locking compression plate for distal femoral fractures were evaluated and classified as a silicone ring tourniquet (Group 1), a pneumatic tourniquet (Group 2), and no usage (Group 3). The variables for analysis were age, sex, preoperative Hb (preHb), postoperative 72-hour Hb (postHb), differences between preHb and postHb (preHb-postHb), amount of intraoperative and overall transfusion, estimated unit of transfusion corrected by preHb-postHb and total transfusion (Hb-lost), amount of intraoperative and postoperative and total bleeding. One-way ANOVA was used to identify the differences between the groups.
Results
The age, sex, operation time, preHb, preHb-postHb, amount of intraoperative and overall transfusion and Hb-lost were similar in the two groups. The amount of intraoperative bleeding was significantly lower in Group 1 than Group 3 (p=0.004), but there was no difference in the amount of postoperative and total bleeding between the two groups.
Conclusion
The use of a silicone ring tourniquet in the minimally invasive plate fixation for distal femoral fractures decreased the amount of intraoperative bleeding compared to no use of a tourniquet. -
Citations
Citations to this article as recorded by- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
Tae sung Lee, Kwan Kyu Park, Byung Woo Cho, Woo-Suk Lee, Hyuck Min Kwon
BMC Musculoskeletal Disorders.2023;[Epub] CrossRef
- Silicone ring tourniquet could be a substitute for a conventional tourniquet in total knee arthroplasty with a longer surgical field: a prospective comparative study in simultaneous total knee arthroplasty
- 816 View
- 4 Download
- 1 Crossref

- A Retrospective Comparative Study of Internal Fixation with Reconstruction Plate Versus Anatomical Locking Compression Plate in Displaced Intercondylar Fractures of Humerus
- Tong Joo Lee, Young Tae Kim, Dae Gyu Kwon, Ju Yong Park
- J Korean Fract Soc 2014;27(4):294-300. Published online October 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.4.294
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To analyze the clinical result of a conventional reconstruction plate (CRP) fixation and locking compressive plate (LCP) fixation on the surgical treatment of an adult's displaced intercondylar fracture of humerus.
MATERIALS AND METHODS
A total of 40 patients enrolled in the study were treated between August 2002 and May 2012. Fixation with a CRP was performed in 20 patients (group A) and anatomical locking compression plate fixation was performed in 20 patients (group B). The clinical and functional evaluation was performed according to the Mayo elbow performance score and Cassebaum classification of elbow range of motion (ROM), disabilities of the arm, shoulder and hand score.
RESULTS
The Mayo elbow functional evaluation scores, eight cases were excellent, 10 cases were good, and two cases were fair in group A, and 12 cases were excellent, seven cases good, and one case fair in group B; both groups showed satisfactory results. The durations of attaining 90 to 120 degrees of the ROM of joints postoperatively were 8.3 days on average (6 to 15 days) in group A and 5.5 days on average (5 to 9 days) in group B, demonstrating a significant difference between the two groups (p=0.04). Although the correlations of clinical results according to the difference of bone mineral densities (BMDs) were not statistically significant between the two groups (p=0.35), loss of fixation occurred due to loosening of screws in two patients with low BMDs in whose operations reconstruction plates were used.
CONCLUSION
The use of locking compressive plate on the surgical treatment of an diaplaced intercondylar fracture of humerus have a good clinical results because that permits early rehabilitation through good fixation and reduces the complications such as loosening of screws.
- 349 View
- 0 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


