Abstract
Atypical ulnar fractures (AUFs) are rare complications that are often linked to long-term antiresorptive therapy. Although atypical femoral fractures are well-studied, AUFs lack standardized diagnostic and treatment protocols. This review summarizes current knowledge on AUFs, including their pathophysiology, diagnostic criteria, and management. A case of bilateral AUFs treated with two distinct osteosynthesis methods is presented, emphasizing the principles of biological healing and mechanical stabilization.
-
Keywords: Ulnar fracture, Bisphosphonates, Internal fracture fixation, Bone graft, Teriparatide
Introduction
The use of antiresorptive agents, primarily bisphosphonates, in the management of osteoporosis has led to emerging complications that require attention from medical professionals. One such complication is atypical fractures resulting from decreased bone formation and suppressed bone remodeling.
While early recognition of these fractures has predominantly focused on femoral shaft or subtrochanteric fractures, orthopedic surgeons have increasingly recognized atypical ulnar fractures (AUFs) occurring in the proximal ulna since the first report in 2011 [
1], albeit with a limited number of case reports and literature reviews available to date [
2,
3]. Although much rarer, bilateral AUFs have also been reported [
4,
5].
Unlike typical ulnar fractures, which often respond well to open reduction and plate fixation, the same treatment approach as typical ulnar fractures may result in failure when applied to AUFs [
4,
6,
7]. Nonetheless, a definitive therapeutic strategy has yet to be established due to the rarity of their occurrence. Recent clinical reports advocate for osteosynthesis techniques involving bone grafting for better outcomes [
2,
7].
This study aims to comprehensively review the clinical characteristics, diagnostic approaches, and therapeutic strategies for AUFs based on the existing literature, and to introduce cases of bilateral AUFs and describe our surgical treatment for osteosynthesis, which included the use of autologous iliac bone grafts. Importantly, we note that the specifics of our surgical techniques differed between the right cortical and left cancellous bone graft. This article provides a narrative review of current concepts in AUFs and illustrates them through a representative bilateral case.
Pathophysiology
Several studies have demonstrated an association between bisphosphonate therapy and the occurrence of atypical femoral fractures (AFFs) involving the femoral shaft or subtrochanteric region [
8-
10]. Prolonged suppression of bone turnover and remodeling due to long-term bisphosphonate exposure has been shown to result in the accumulation of microdamage within the bone [
8,
11]. Oversuppression of bone turnover resulting from prolonged bisphosphonate therapy has been reported to reduce bone elasticity, increase resistance to plastic deformation, and decrease resistance to crack propagation, thereby contributing to the development of atypical fractures [
12,
13]. Tensile stress generated by axial loading has been identified as a biomechanical factor contributing to the development of fractures [
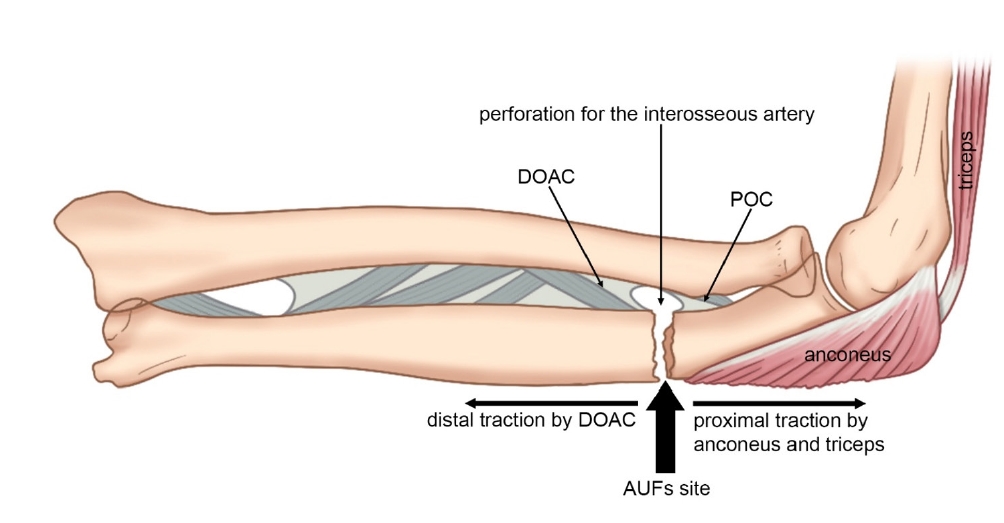
14]. The AUFs have been understood to occur through mechanisms similar to those proposed for AFFs. The interosseous membrane of the forearm serves as a critical longitudinal stabilizer, preserving forearm function and facilitating load transmission between the radius and ulna [
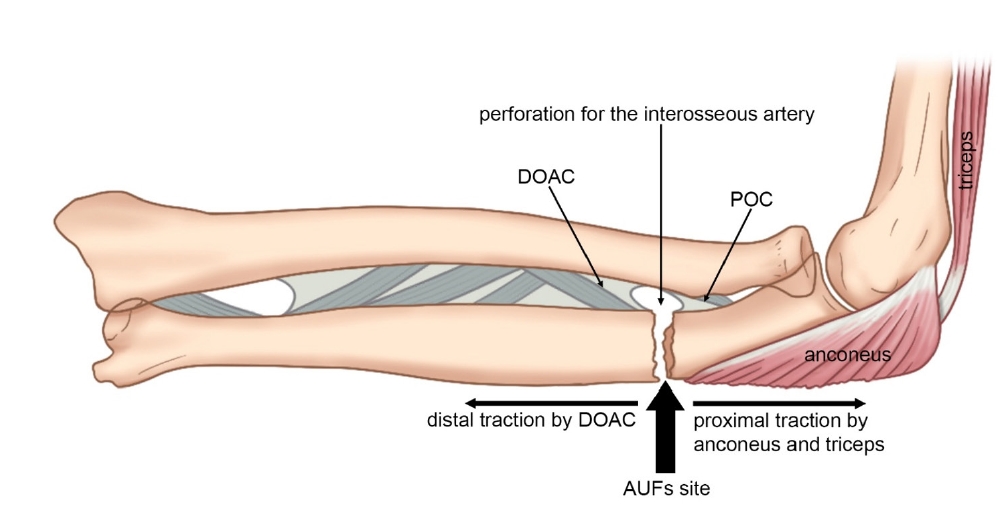
15]. A finite element analysis study demonstrated that the maximum tensile stress, measured at 7.769 MPa at 64.6% of the total ulnar length (153.4 mm of 237.5 mm from the ulnar head), was generated by a combination of axial loading on the ulna, proximal traction by the triceps brachii and anconeus muscles, and distal traction by the interosseous membrane of the forearm [
16]. Tensile stress, generated and transmitted by the interosseous membrane—a ligamentous complex in the forearm—plays a key role in the development of fractures [
17]. The dorsal oblique accessory cord (DOAC) is a robust fibrous structure, whereas the proximal oblique cord (POC) has minimal functional significance in humans [
18]. the DOAC is thought to prevent distal displacement of the radius while exerting a distal traction force on the ulna, with cadaveric studies reporting that the insertion points of the DOAC and POC are located at 61.8%–64.0% of the total ulnar length from the ulnar head, and the maximal tensile stress has been observed to occur between these two structures [
15,
16,
19]. The maximal tensile stress occurs between the DOAC and the POC, generated by the opposing forces of the triceps brachii and anconeus muscles pulling the ulna proximally and the DOAC exerting a distal traction on the ulna, and this stress concentration may be further augmented by the anatomical feature wherein the proximal part of the middle portion of the interosseous membrane consists of a transparent membranous tissue with a perforation for the interosseous artery, leaving the ulna at that level partially unsupported (
Fig. 1) [
16].
Diagnosis
In their 2013 report, the American Society for Bone and Mineral Research (ASBMR) Task Force revised the case definition of AFFs based on accumulated clinical and radiographic evidence [
20]. The revised definition refined the major features by specifying radiographic characteristics, including fracture location along the femoral diaphysis, a transverse or short oblique fracture orientation, minimal or absent comminution, and localized periosteal or endosteal thickening of the lateral cortex [
20].
The diagnostic criteria for AUFs were derived from those established for AFFs. Heo et al. [
21] subsequently modified the 2013 case definition proposed by the ASBMR Task Force to create a case definition for AUFs by incorporating the aforementioned differences (
Table 1).
The diagnostic criteria for AUFs were adapted from those for AFFs by modifying the fracture location to correspond to the ulnar diaphysis. It was proposed that at least four of the five major features must be present for diagnosis, while minor features are not required but may be associated findings. In addition, "previous history or present symptom of atypical femoral fractures" was added as a new minor feature (m5), reflecting the frequent coexistence of AFFs in patients with AUFs [
21].
Treatment Strategies
Medical Strategy
To prevent atypical fractures, it has been suggested that the risk of AFFs decreases by more than 50% within the first year after discontinuation of oral bisphosphonate therapy and by over 80% after 3 years, supporting the practice of implementing drug holidays approximately every 5 years during long-term bisphosphonate treatment [
22].
Several studies have reported favorable outcomes with the use of teriparatide for the healing of atypical fractures. Carvalho et al. [
23] demonstrated that in three postmenopausal women with osteoporosis who sustained atypical subtrochanteric or femoral shaft fractures without major trauma during long-term bisphosphonate therapy, treatment with teriparatide resulted in significant increases in bone turnover markers and radiographic evidence of fracture healing within a few months.
Preclinical studies have also reported favorable effects of teriparatide treatment for AFFs. In five women with AFFs, 6 months of teriparatide therapy significantly increased the expression of mesenchymal stromal cell markers (CD73, CD90, and CD105), upregulated pluripotency-related genes (notably
NANOG), enhanced cellular proliferation, reduced cellular senescence, and improved both osteogenic and adipogenic differentiation. These findings suggest that teriparatide may rejuvenate bone marrow mononuclear cells, thereby promoting bone regeneration and indicating broader therapeutic potential [
24].
For the management of incomplete AFFs, Feron and Cambon-Binder [
25] proposed a treatment algorithm. When cortical radiolucency is present, conservative management including limited weight-bearing, calcium and vitamin D supplementation, and teriparatide therapy is recommended. Healing should be reassessed after 3 months; if clinical symptoms have resolved, radiographic healing is evident, and magnetic resonance imaging (MRI) demonstrates no bone edema, continued observation. However, if a radiolucent line persists or if there is no clinical or MRI improvement, prophylactic intramedullary nailing should be considered to prevent progression to complete fracture. Although a standardized treatment protocol for AUFs has not yet been established, it is reasonable to speculate that a management algorithm similar to that for AFFs may be applicable.
Although the evidence regarding the efficacy of vitamin D and calcium supplementation in promoting the healing of atypical fractures remains inconclusive and somewhat controversial, multiple studies recommend their administration as part of the overall management strategy during conservative treatment [
20,
21,
25-
27]. In the management of patients with AUFs, vitamin D and calcium supplementation should not be used as standalone therapies but rather as adjunctive measures in conjunction with other treatment modalities.
Although rarely reported, other antiresorptive agents such as denosumab can also lead to AUFs by inhibiting bone resorption, altering bone turnover, and increasing bone mineral density [
3,
28,
29]. While further research is needed, clinicians are advised to maintain a high index of suspicion for AUFs in patients receiving denosumab who present with relevant clinical symptoms and radiographic features.
Case
An 81-year-old female patient sustained injuries to both of her forearms while leaning forward near the tap and subsequently visited the emergency room. She required a cane for outdoor ambulation and had a medical history of cardiac valvular disease. Additionally, she had been prescribed ibandronate by her local hospital for the past 15 years to manage osteoporosis.
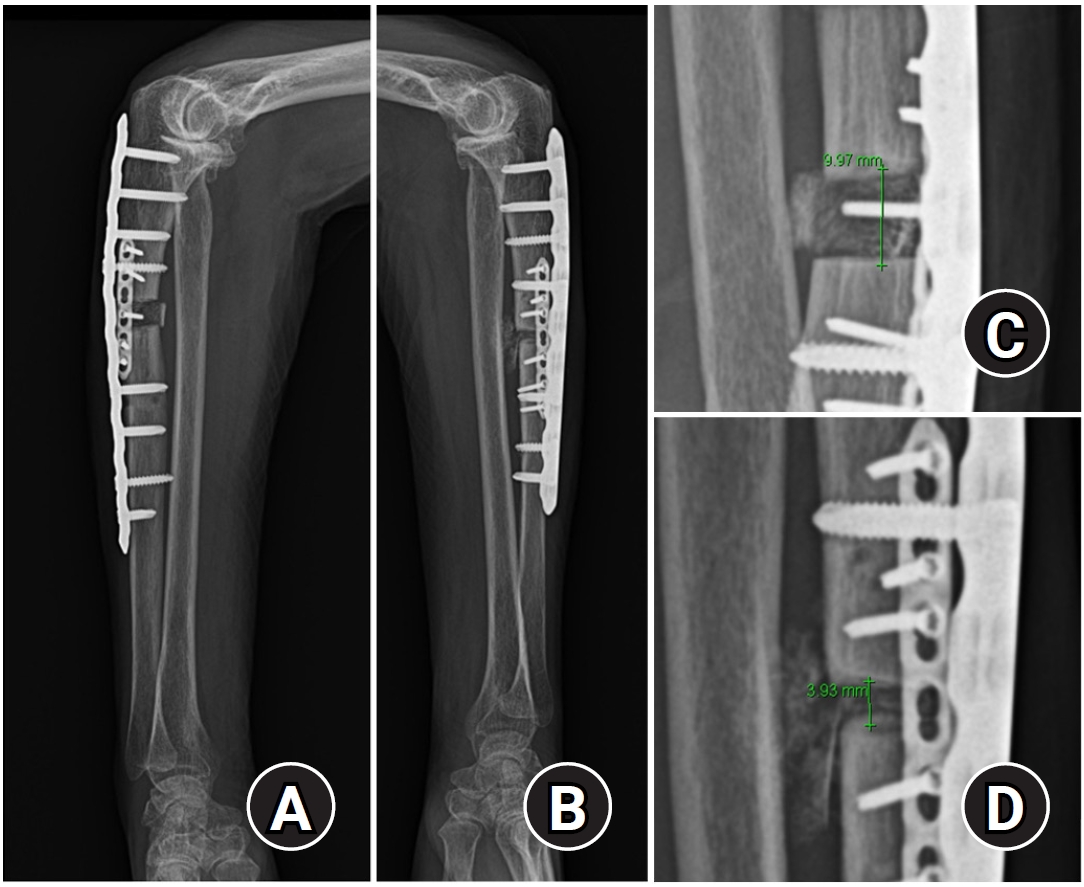
Upon initial X-ray examination, minimal displaced transverse and short oblique fractures were observed in both proximal 1/3 ulna (
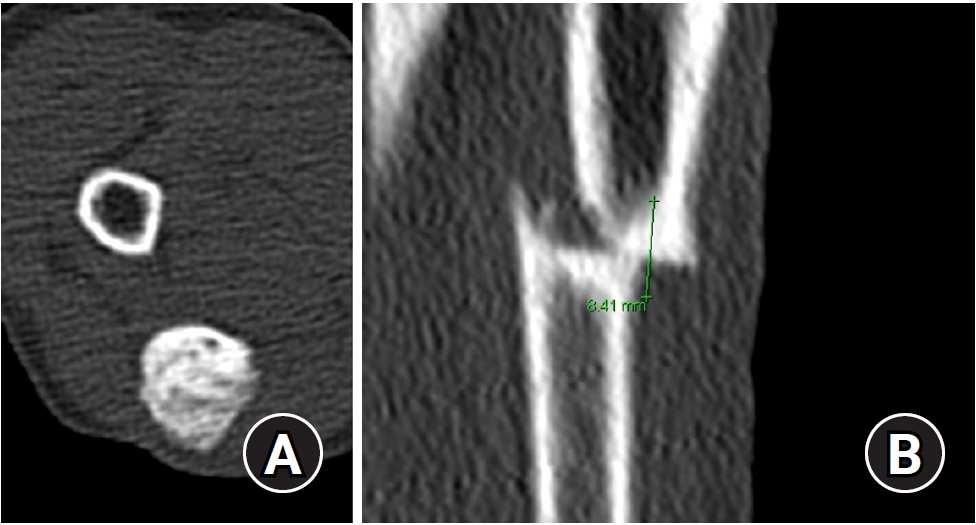
Fig. 2). Additionally, both fracture margins exhibited sclerotic changes with approximately 5 mm thickness at both fracture ends, which were consistent in both forearms. Computed tomographs revealed cortical bone thickness at the fracture site, with a loss of cancellous bone filling in the medullary canal, and cortical thickness on both sides of the fracture section measuring 4 to 5 mm (
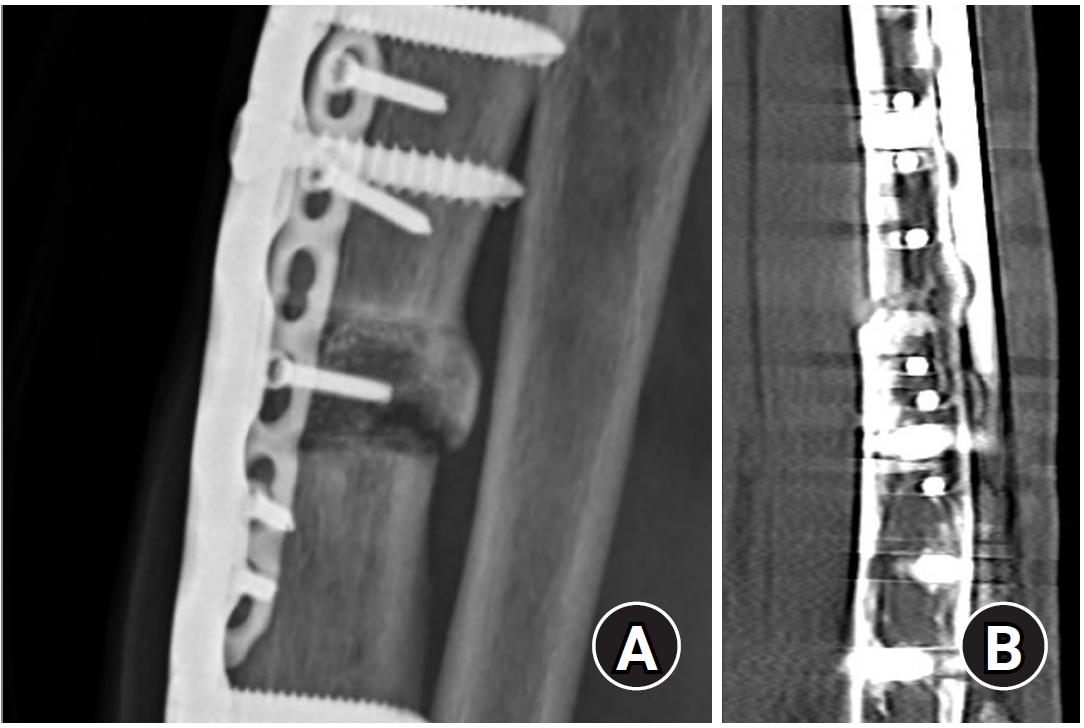
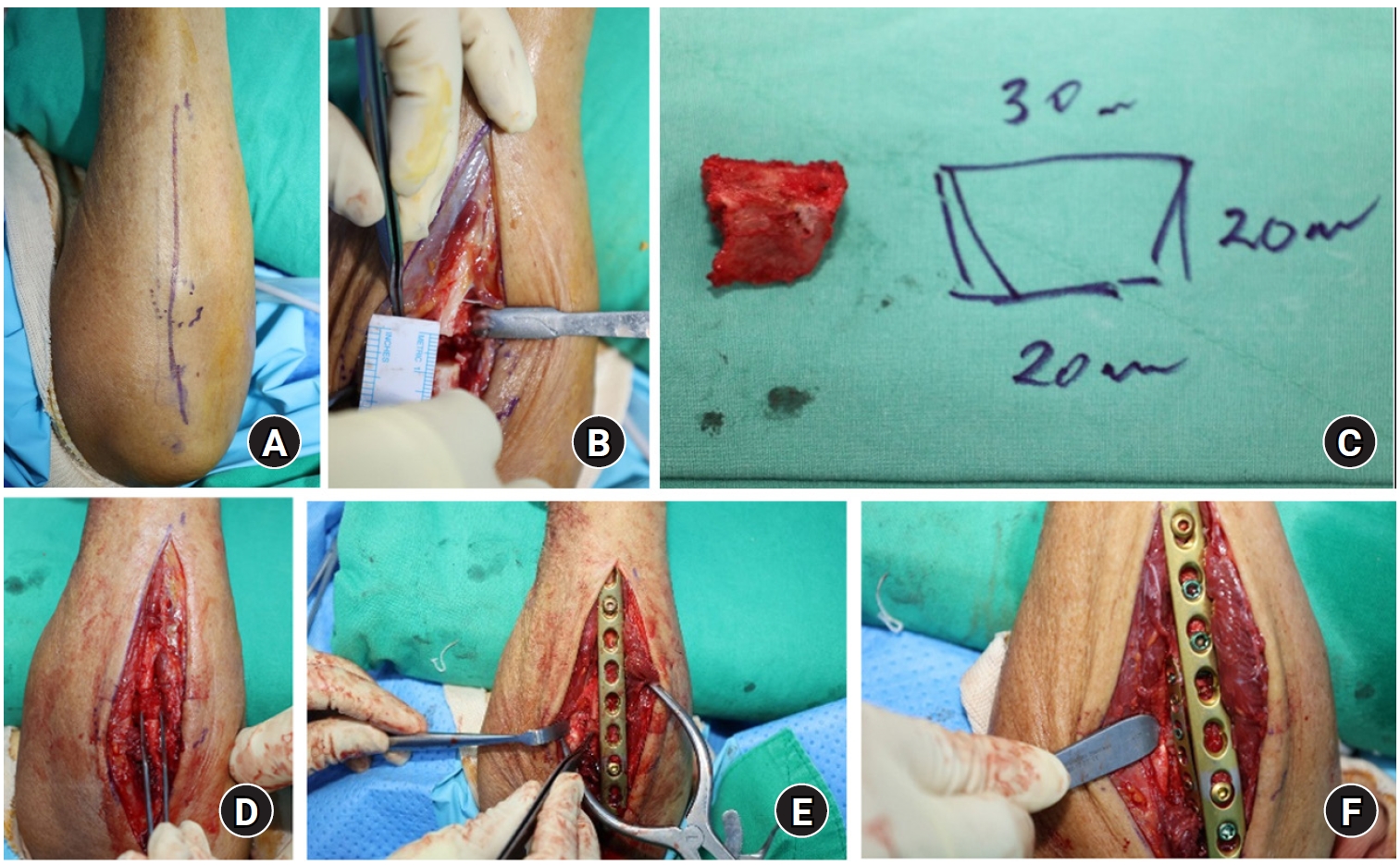
Fig. 3). Under general anesthesia, we attempted osteosynthesis using a bone graft harvested from the patient's right iliac bone, following complete resection of pathologic nonviable cortical bone.
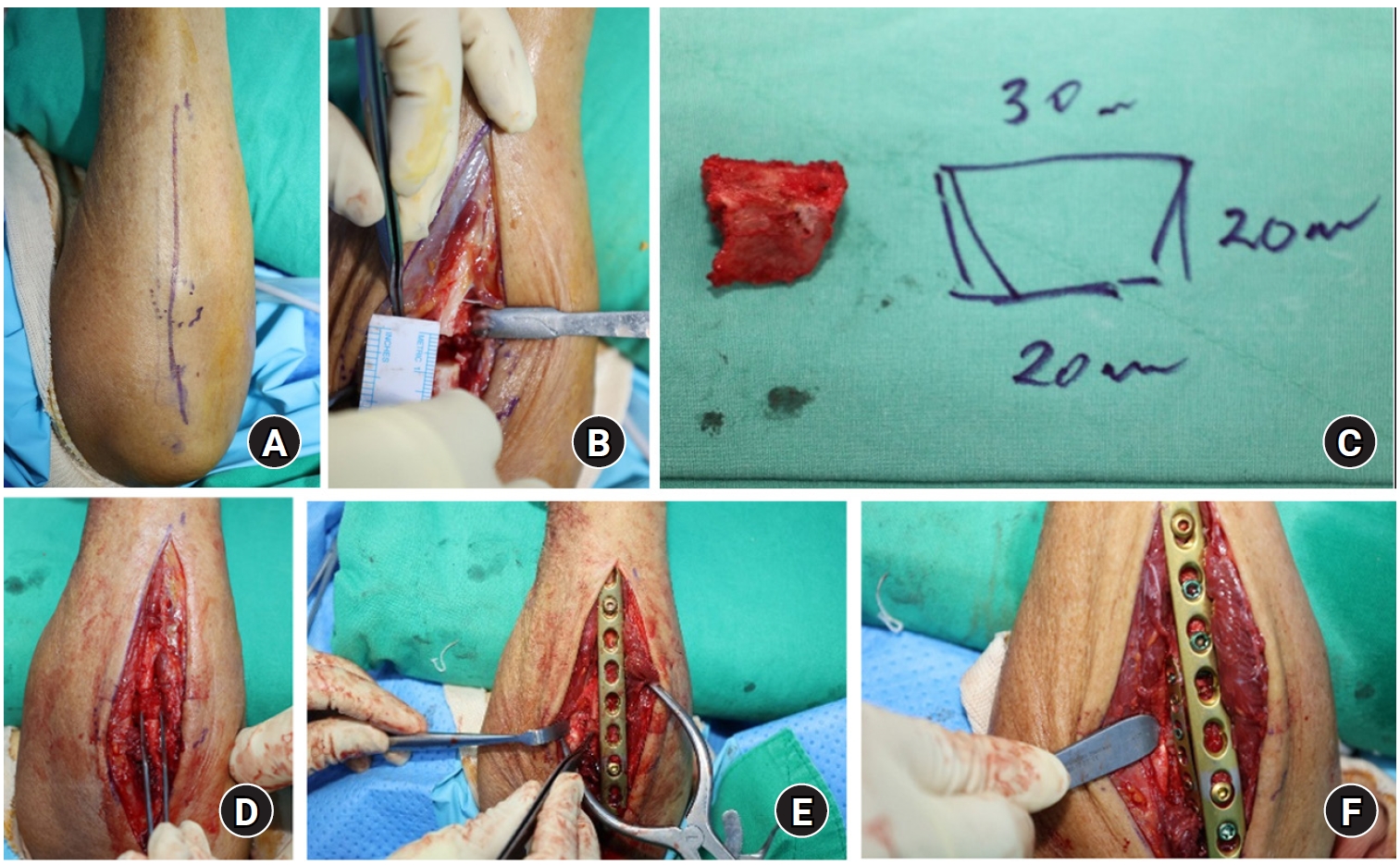
Right forearm
The fracture site was easily identified on the surface due to skin protrusion (
Fig. 4A). We performed a direct ulnar approach between the extensor carpi ulnaris and flexor carpi ulnaris muscles. Using an oscillating saw, we resected a 4 mm thickness of cortical bone in each, resulting in an 8‒10 mm gap between the proximal and distal segments (
Fig. 4B). We harvested a tricortical bone graft over 20 mm in size from the right iliac crest, intending to use 10 mm of harvested bone in each forearm (
Fig. 4C). The graft was halved, and a 10 mm tricortical bone segment was inserted into the resected ulnar gap. The fracture site was then tapped to push it into the defect site (
Fig. 4D). Subsequently, we applied a 10-hole 3.5 mm limited contact locking compression plate (LC-LCP), securing four screws in each segment (
Fig. 4E). Additionally, a 2.0 mm small fragment plate was attached to hold the harvested bone at a 90° angle to the main plate (
Fig. 4F).
Left forearm
Initially, we attempted to apply the same procedures to the left forearm. However, the remaining 10 mm length hard tricortical bone broke during tapping into the gap created by the same 4‒5 mm resection in each fracture segment. Consequently, we modified our original plan, reducing the fracture site until the defect was closed, leaving a 4 mm gap before plate fixation. We applied a 3.5 mm LC-LCP and fixed proximal four screws and distal three screws above and below gap remaining. Additionally, we harvested cancellous bone from the initial iliac crest and inserted it into the defect site. The original cortical bone was further chopped and inserted into the defect area also. To provide further strength, we also applied a 2.0 mm small fragment plate, similar to the approach used for the right arm.
Postoperative and follow-up management
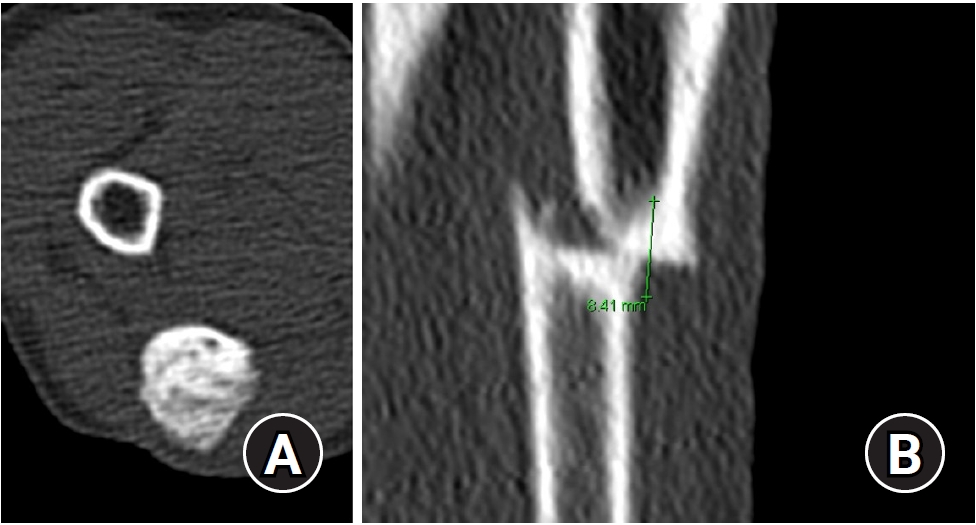
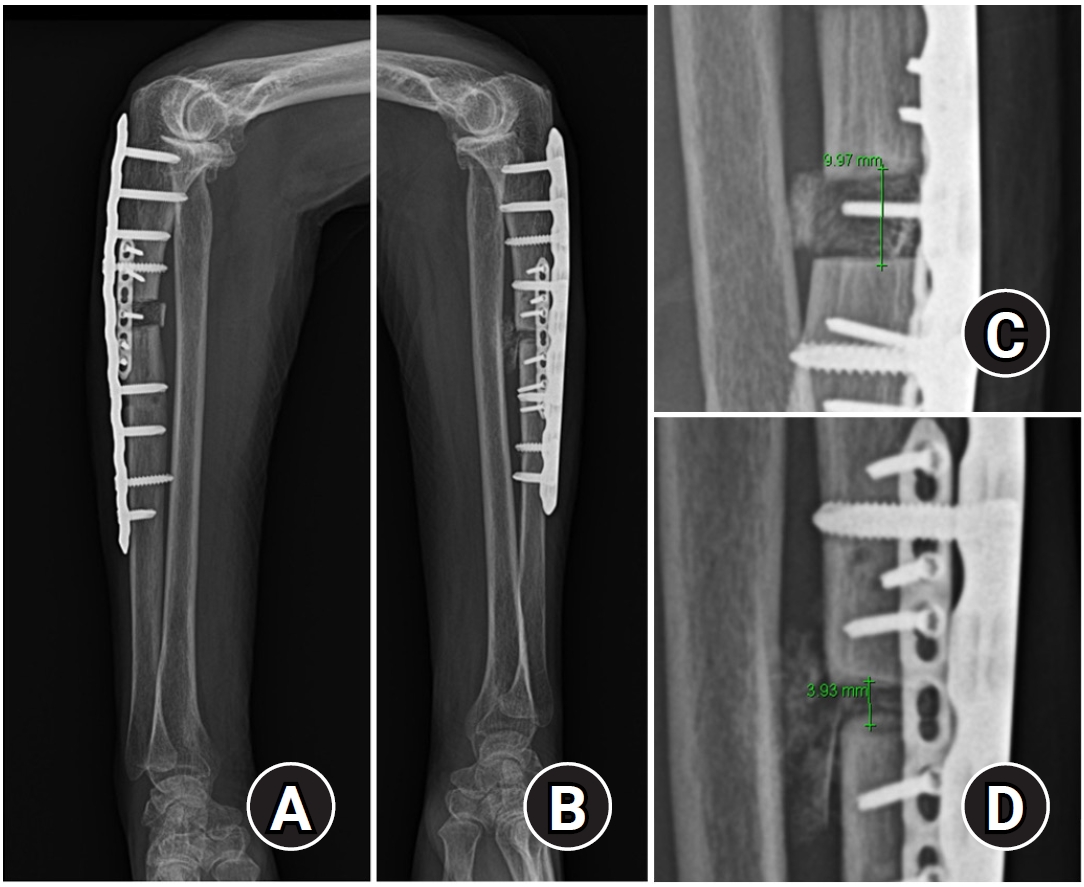
Postoperatively, the bone-grafted gaps measured 9.5 mm and 3.8 mm in the right and left forearms, respectively (
Fig. 5). Additionally, we conducted elbow and wrist X-rays, which revealed a positive ulnar variance of 3 mm in the right wrist and a negative variance of 2 mm in the left wrist (
Fig. 6). Both wrists exhibited ulnocarpal impaction lesion in both lunates.
We discontinued ibandronate medication and initiated treatment with bone-forming and parathyroid hormone agents. Both femurs were examined to check for atypical femur lesions, yielding negative results. Bone mineral density evaluation showed T-scores of ‒3.8 and ‒2.3 in the average lumbar spine and femur neck areas, respectively.
A short arm splint, long enough to cover the fracture site yet allowing for elbow motion, was applied for 2 weeks postoperatively. Given sustained fixation stability with the implant, we permitted elbow and wrist range of motion with intermittent removable brace protection.
Serial X-ray follow-ups were conducted at postoperative intervals of 1 week, 2 weeks, 4 weeks, 8 weeks, and 20 weeks, and thereafter. At the 20-week outpatient follow-up, the patient reported being free of pain at both forearm fracture sites, and both forearms showed complete union without any visible fracture lines (
Fig. 7). For long-term follow-up, we contacted the patient's daughter by phone. She stated that the patient did not return to the outpatient clinic primarily because she had no symptoms and was able to maintain a full range of motion. Furthermore, the patient resides a considerable distance from the hospital, and she was recently diagnosed with lymphadenitis, which may be associated with cancer metastasis.
The patient and the patient’s daughter provided consent for the publication of this case report, including all clinical images.
Case discussion
AUFs represent a distinct subset of ulnar fractures characterized by their unique presentation and etiology. Unlike typical ulnar fractures, AUFs occur spontaneously or with minimal trauma. Prolonged bisphosphonate use can induce microstructural changes in bone tissue, predisposing it to atypical fracture patterns under minimal or spontaneous loading.
To date, only a limited number of case—around 40—have reported on AUFs, and treatment principles have not been firmly established [
2,
6]. Though it is inconclusive in terms of operative treatment strategy, the classic approach of open reduction and internal fixation used in typical ulnar fractures carries a risk of treatment failure [
7]. Nonsurgical treatment of AUFs had a high risk of nonunion. Incomplete or nondisplaced complete fractures that were treated non-surgically eventually progressed to complete displaced fractures and nonunion [
14,
27,
30].
In terms of fracture healing through osteosynthesis, two main principles must be considered: biology and fixation stiffness. Addressing the biology aspect, the sclerotic bone margins at the fracture ends were deemed nonviable lesions, prompting us to resect them completely until normal cancellous bone canal appeared. After sufficient resection, the resulting gap necessitates bone grafting to facilitate the formation of new healthy bone in the gap area. Autologous bone grafts are generally considered to have higher osteogenic potential compared to allografts. However, no comparison was made regarding the superiority between cortical bone graft [
7,
31], which offers structural stability advantages as in the right forearm, and cancellous bone graft [
2], which offers advantages for osteogenesis as in the left forearm. Nonetheless, bone union was confirmed in both groups simultaneously.
The second consideration was fixation stability. We utilized a 3.5 mm LC-LCP straight plate in both forearms, applying a 10-hole plate in the right forearm and a 9-hole plate in the left. Additional 2.0 mm small fragment plates of 6 and 7 holes were added to the right and left forearms, respectively. Notably, the right small plate secured the grafted cortical bone. Although the optimal number of cortices and the length of the plate were not definitively determined, prior studies have suggested that greater stability is advisable compared to primary ulnar fractures. Some authors reported the usefulness of the dual plate for more rigid internal fixation [
2,
32].
Lastly, while not related to fracture healing, consideration must be given to the elbow and wrist joints in forearm fractures. Despite the absence of ulnar-sided wrist pain before or after the operation, ulnocarpal impaction was evident in the wrist radiogram, attributed to a lunate bone lesion. By reducing the resected bone margin in the left forearm, we could decrease the required amount of harvested cancellous bone graft while also unintentionally performing ulnar shortening osteotomy—a classic treatment for ulnocarpal impaction syndrome.
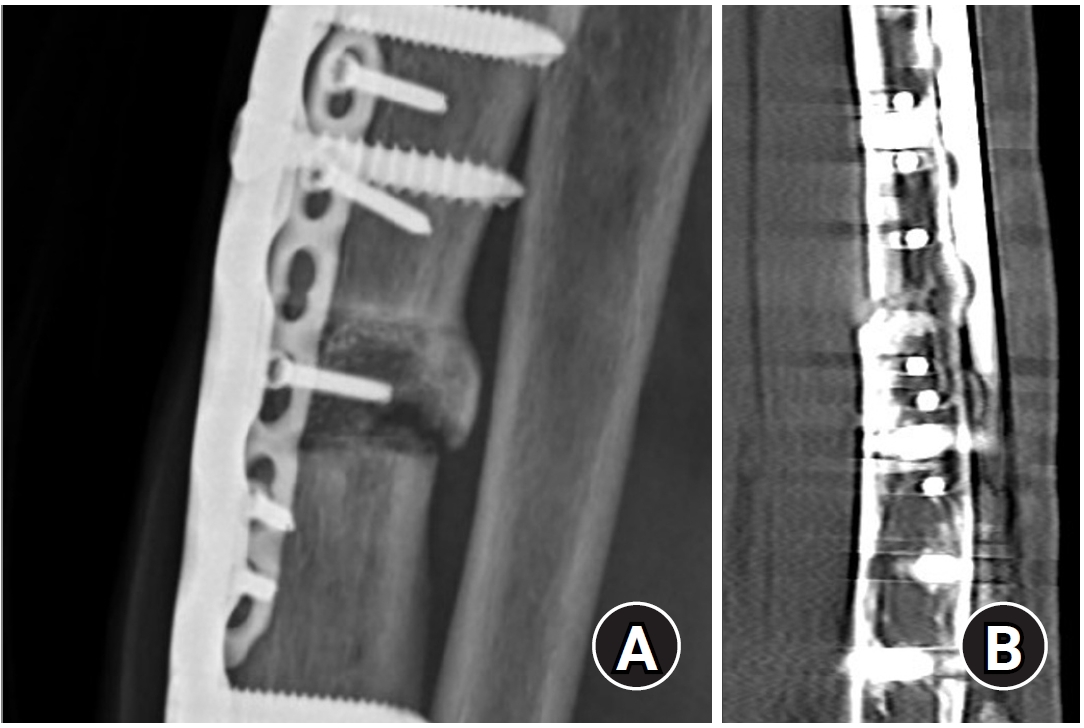
This study has several limitations. Despite our attempts to contact the patient by phone, we were unable to obtain long-term follow-up radiographs to provide further insight for the readership. Instead,
Fig. 8 presents a lateral radiograph from a different 85-year-old female patient who underwent a similar procedure using an iliac cortico-cancellous structural bone graft. The radiograph, taken 20 months postoperatively, demonstrates a similarly favorable outcome.
Although osteosynthesis resulted in favorable clinical outcomes, it remains unclear which type of bone graft—cortical or cancellous—offers superior results, as well as optimizing fixation plate application for sufficient stability, remains uncertain. These limitations underscore the need for further clinical experience and research in the future.
In
Table 2, we summarize the treatment guidelines for AUFs based on previously published literature and our own limited clinical experience.
Conclusions
AUFs represent a rare but clinically significant complication of long-term antiresorptive therapy. Given their distinct pathophysiology and mechanical environment compared to typical ulnar fractures, successful management requires both biological and mechanical optimization. Surgical strategies emphasizing complete resection of unhealthy sclerotic margins, autologous bone grafting either cortical or cancellous depending on the defect characteristics and rigid plate fixation with long and double plating yielded favorable outcomes in our bilateral AUF case. Further accumulation of clinical cases and prospective research are necessary to refine diagnostic criteria and optimize therapeutic approaches for AUFs.
Article Information
-
Author contributions
Conceptualization: CHO, HTK, JKL. Data curation: CHO, HTK. Methodology: JKL. Investigation: CHO, HTK. Resources: HTK. Validation: HTK. Visualization: CHO, JKL. Writing-original draft: CHO. Writing-review & editing: HTK, JKL. All authors read and approved the final manuscript.
-
Conflicts of interest
None.
-
Funding
None.
-
Data availability
Not applicable.
Fig. 1.Anatomical structures related to tensile stress distribution in the proximal ulna. The dorsal oblique accessory cord (DOAC), a robust fibrous structure, inserts at 61.8%–64.0% of the total ulnar length and exerts a distal traction force on the ulna, opposing the proximal pulling forces of the triceps brachii and anconeus muscles. Maximal tensile stress is concentrated between the DOAC and the proximal oblique cord (POC), where a perforation in the proximal portion of the interosseous membrane leaves the underlying ulna partially unsupported. AUF, atypical ulnar fracture.
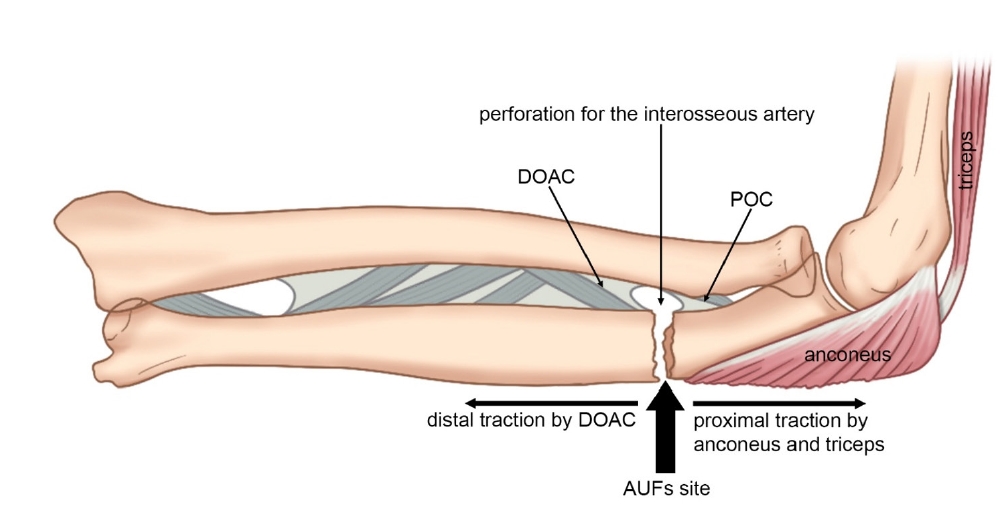
Fig. 2.Initial X-ray images of both forearms. Right forearm (A). Left forearm (B).

Fig. 3.Axial computed tomography image at the level of sclerotic bone lesion without medullary canal (A). The length of both sclerotic margin ends was over 8 mm (B).
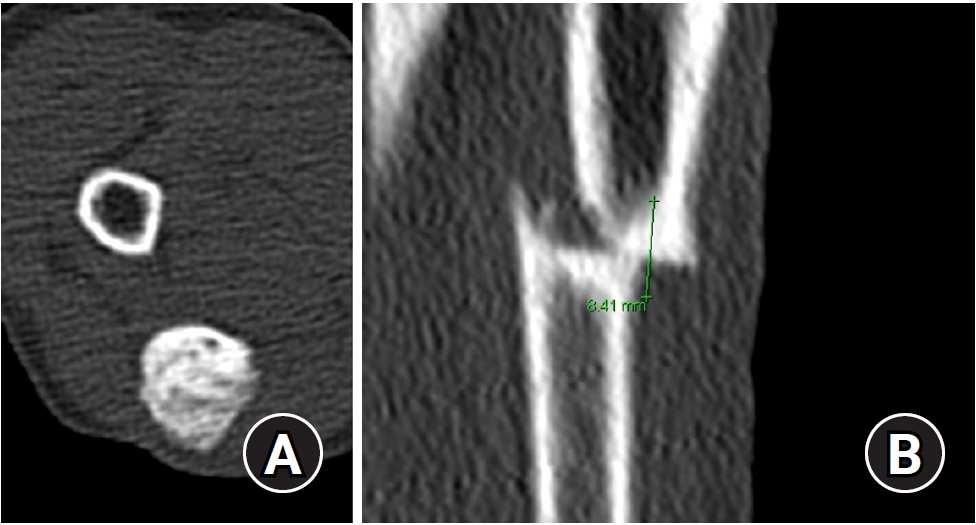
Fig. 4.The protruding atypical ulnar fracture was visible overlying skin (A). The overall gap created by resecting the sclerotic margins of both bone segments measured approximately 9 mm (B). Tricortical bone exceeding 20 mm in length was harvested from the right iliac crest (C). Half of the cortical bone was inset into the defect site (D). The 3.5 mm limited contact locking compression plate fixation (E). Additional 2.0 mm small plate augmentation at the lateral aspect of ulna (F).
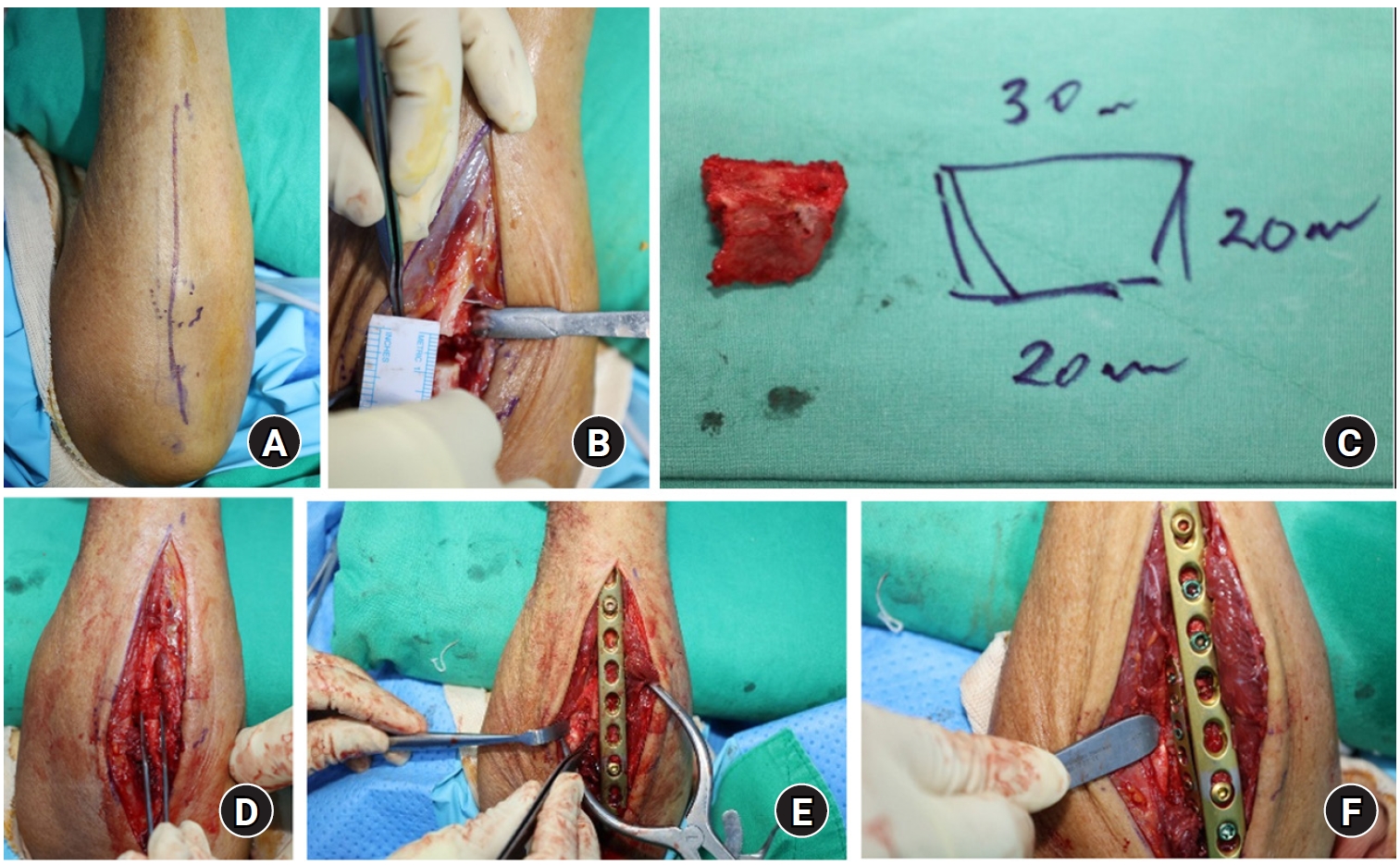
Fig. 5.Postoperative lateral plain X-rays of the right (A) and left (B) forearms. The gaps were measured as 9.9 mm on the right (C) and 3.9 mm on the left (D).
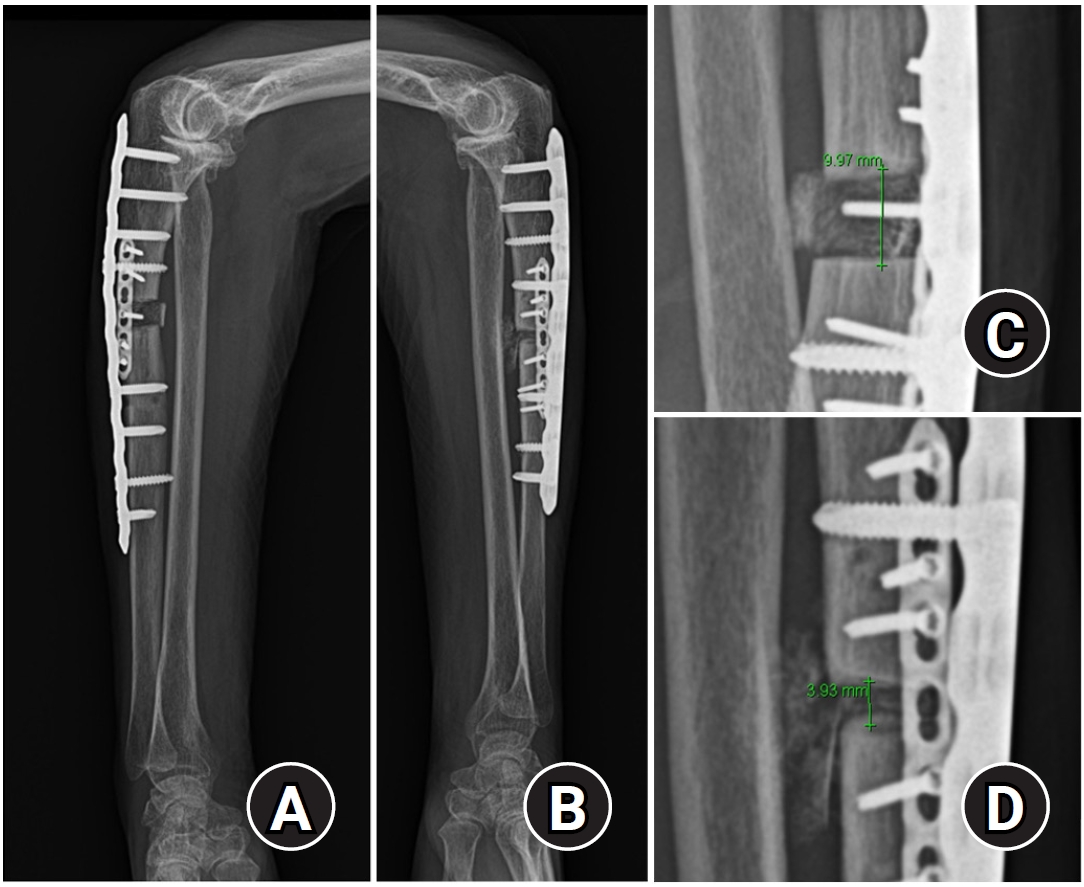
Fig. 6.Postoperative anteroposterior wrist X-ray showing positive and negative ulnar variance. (A) Right wrist. (B) Left wrist.

Fig. 7.At 20 weeks after the operation, the grafted bone was coaptated in the right arm (A) and united in the left arm (B).
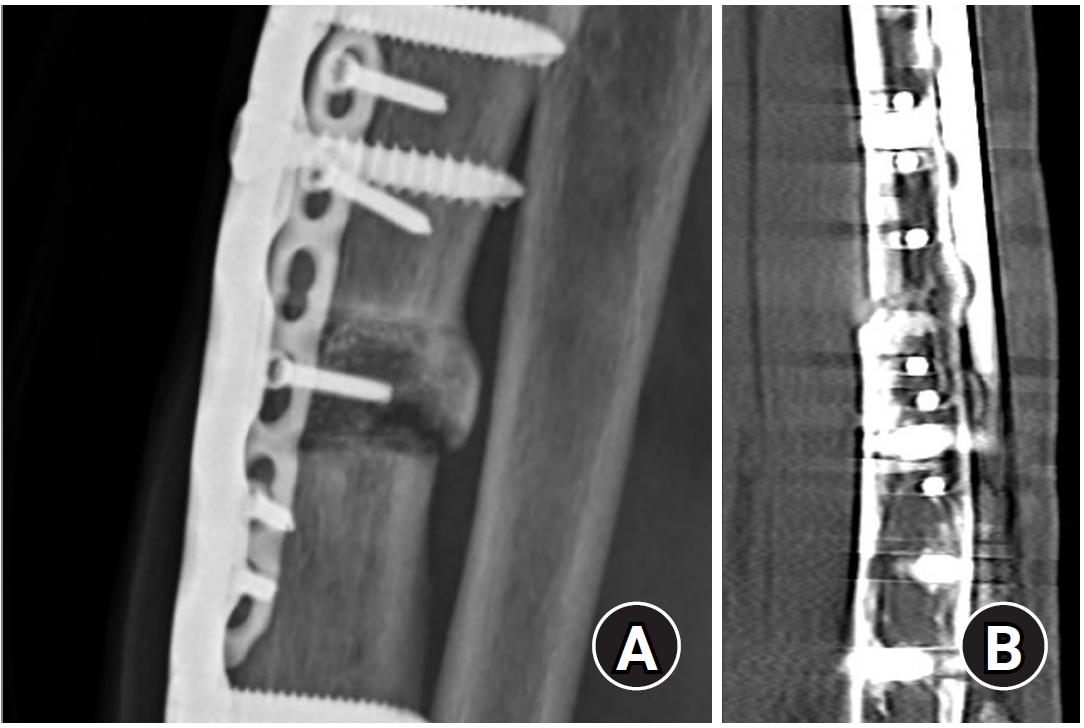
Fig. 8.Lateral radiograph of a different 85-year-old female patient taken 20 months postoperatively. The patient was treated with an iliac cortico-cancellous structural bone graft and showed favorable outcomes. The grafted cortical bone was soundly coaptated (circle) to both the proximal and distal segments of the ulna, as demonstrated in the image.

Table 1.Modified case definition for atypical ulnar fractures
|
Variable |
Revised definition |
|
Fracture location |
The fracture must be located on the ulnar diaphysis between 20% and 45% distal to the olecranon tip. |
|
In addition |
At least 4 of 5 major features must be present. None of the minor features are required but they have sometimes been associated with these fractures. |
|
Major features |
|
|
M1 |
The fracture is associated with minimal or no trauma, as in a fall from a standing height or less. |
|
M2 |
The fracture line originates at the posterior cortex and is substantially transverse in its orientation, although it may become oblique as it progresses anteriorly across the ulna. |
|
M3 |
A complete fracture extends through both cortices and may be associated with an anterior spike; an incomplete fracture involves only the posterior cortex. |
|
M4 |
The fracture is noncomminuted or minimally comminuted. |
|
M5 |
Localized periosteal or endosteal thickening of the posterior cortex is present at the fracture site. |
|
Minor features |
|
|
m1 |
Diffuse cortical thickening of the whole cortex is present at the fracture site. |
|
m2 |
Unilateral or bilateral prodromal symptoms such as dull or aching pain in the forearm. |
|
m3 |
Bilateral incomplete or complete ulnar diaphysis fractures. |
|
m4 |
Delayed fracture healing. |
|
m5 |
Previous history or present symptom of atypical femoral fractures. |
Table 2.Summary of the guideline for atypical ulnar fracture treatment
|
Category |
Key point |
|
Preoperative evaluation |
Review medical history for use of antiresorptive agents |
|
Conduct a laboratory evaluation of bone health profile |
|
Use radiologic studies (X-ray and bone scan) to detect other atypical lesions, including subtrochanteric areas |
|
Discontinue antiresorptive agents preoperatively |
|
Perform a DEXA scan to evaluate current bone density status |
|
Operative principles |
Focus on improving biological healing and fixation stability during osteosynthesis |
|
Debate remains regarding extent of debridement/resection and type of bone graft (cortical vs. cancellous) |
|
Decision algorithm for graft type: use cortical for large segmental defects with mechanical stability; cancellous for enhancing osteogenesis in smaller gaps |
|
Robust fixation recommended: long plate, dual plating, or combined plate and nail techniques |
|
Postoperative management |
Recommend PTH therapy; calcium and vitamin D supplementation (despite inconclusive evidence) |
|
Coordinate with medical team for follow-up medical management |
|
More protection using immobilization and a longer bone union period are required, making close outpatient follow-up imperative |
References
- 1. Stathopoulos KD, Kosmidis C, Lyritis GP. Atypical fractures of the femur and ulna and complications of fracture healing in a 76-year-old woman with Sjögren’s syndrome. J Musculoskelet Neuronal Interact 2011;11:208-11.ArticlePubMed
- 2. Abe K, Kimura H, Yamamoto N, et al. Treatment strategy for atypical ulnar fracture due to severely suppressed bone turnover caused by long-term bisphosphonate therapy: a case report and literature review. BMC Musculoskelet Disord 2020;21:802.ArticlePubMedPMCPDF
- 3. Tan SH, Saseendar S, Tan BH, Pawaskar A, Kumar VP. Ulnar fractures with bisphosphonate therapy: a systematic review of published case reports. Osteoporos Int 2015;26:421-9.ArticlePubMedPDF
- 4. Ohta S, Ikeguchi R, Noguchi T, Kaizawa Y, Matsuda S. Intractable fractures of the bilateral proximal ulnae after 8 years of zoledronate treatment for breast cancer bone metastasis. J Hand Surg Am 2022;47:393.e1-77.ArticlePubMed
- 5. Asano Y, Tajiri K, Yagishita S, Nakanishi H, Ishii T. Bilateral atypical ulnar fractures occurring after long-term treatment with bisphosphonate for 7 years and with teriparatide for 2 years: a case report. Osteoporos Int 2020;31:2473-6.ArticlePubMedPDF
- 6. Hirokawa T, Zukawa M, Makino H, Osada R, Kawaguchi Y. Therapeutic strategy for atypical ulnar fracture in long use of bisphosphonate: a systematic review. J Orthop Sci 2024;29:880-4.ArticlePubMed
- 7. Cha SM, Shin HD, Ahn BK. Revision osteosynthesis after primary treatment of atypical ulnar fractures associated with bisphosphonate usage: nonunion after ordinary open reduction and internal fixation. Arch Orthop Trauma Surg 2021;141:1855-62.ArticlePubMedPDF
- 8. Schilcher J, Koeppen V, Aspenberg P, Michaëlsson K. Risk of atypical femoral fracture during and after bisphosphonate use. Acta Orthop 2015;86:100-7.ArticlePubMedPMC
- 9. Meier RP, Perneger TV, Stern R, Rizzoli R, Peter RE. Increasing occurrence of atypical femoral fractures associated with bisphosphonate use. Arch Intern Med 2012;172:930-6.ArticlePubMed
- 10. Dell RM, Adams AL, Greene DF, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 2012;27:2544-50.ArticlePubMedPDF
- 11. Giusti A, Hamdy NA, Papapoulos SE. Atypical fractures of the femur and bisphosphonate therapy: a systematic review of case/case series studies. Bone 2010;47:169-80.ArticlePubMed
- 12. Tjhia CK, Odvina CV, Rao DS, Stover SM, Wang X, Fyhrie DP. Mechanical property and tissue mineral density differences among severely suppressed bone turnover (SSBT) patients, osteoporotic patients, and normal subjects. Bone 2011;49:1279-89.ArticlePubMedPMC
- 13. Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab 2005;90:1294-301.ArticlePubMed
- 14. Yam MG, Kwek EB. A case of bilateral atypical ulnar fractures with bisphosphonate therapy in a walking aided elderly. Ann Acad Med Singap 2017;46:351-3.ArticlePubMed
- 15. Skahen JR, Palmer AK, Werner FW, Fortino MD. The interosseous membrane of the forearm. anatomy and function. J Hand Surg Am 1997;22:981-5.ArticlePubMed
- 16. Okita S, Saito T, Yamamoto N, et al, Five cases of atypical ulnar fractures associated with long-term bisphosphonate use. an anatomical and mechanical analysis using a finite element model. J Orthop Sci 2024;29:449-53.ArticlePubMed
- 17. Noda K, Goto A, Murase T, Sugamoto K, Yoshikawa H, Moritomo H. Interosseous membrane of the forearm. an anatomical study of ligament attachment locations. J Hand Surg Am 2009;34:415-22.ArticlePubMed
- 18. Tubbs RS, O’Neil JT, Key CD, et al. The oblique cord of the forearm in man. Clin Anat 2007;20:411-5.ArticlePubMed
- 19. Fujita M. An anatomical study on the interosseous membrane of the forearm. Nihon Seikeigeka Gakkai Zasshi 1995;69:938-50.ArticlePubMed
- 20. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014;29:1-23.ArticlePubMed
- 21. Heo YM, Park SE, Cha SM, Shin HD, Choi JK. Diagnostic criteria and treatment of atypical ulnar fractures associated with prolonged bisphosphonate therapy: multicenter case analysis. J Hand Surg Am 2022;47:901.ArticlePubMed
- 22. Reid IR, Billington EO. Drug therapy for osteoporosis in older adults. Lancet 2022;399:1080-92.ArticlePubMed
- 23. Carvalho NN, Voss LA, Almeida MO, Salgado CL, Bandeira F. Atypical femoral fractures during prolonged use of bisphosphonates: short-term responses to strontium ranelate and teriparatide. J Clin Endocrinol Metab 2011;96:2675-80.ArticlePubMed
- 24. Casado-Díaz A, Dorado G, Giner M, et al. Proof of concept on functionality improvement of mesenchymal stem-cells, in postmenopausal osteoporotic women treated with teriparatide (PTH1-34), after suffering atypical fractures. Calcif Tissue Int 2019;104:631-40.ArticlePubMedPDF
- 25. Feron JM, Cambon-Binder A. Medication management after intramedullary nailing of atypical fractures. Injury 2017;48 Suppl 1:S15-7.ArticlePubMed
- 26. Anderson PA, Kates SL, Watts NB. Update on atypical femoral fractures. J Bone Joint Surg Am 2024;106:1819-28.ArticlePubMed
- 27. Yamamoto N, Yamauchi M, Noda T, Matsui Y, Ozaki T.. Atypical ulnar fracture with atypical femoral fracture: a case report and literature review. J Orthop Sci 2022;27:1354-8.ArticlePubMed
- 28. Okubo N, Yoshida T, Ohara M, Takahashi K. Atypical ulnar fracture in an older woman with osteoporosis with a five-year history of denosumab treatment: a case report. J Hand Surg Asian Pac Vol 2022;27:928-32.ArticlePubMed
- 29. Binkley N, Goel H, Shives E, Krueger D, Hare K. A probable atypical ulnar fracture in a man receiving denosumab. Bone 2021;143:115726.ArticlePubMed
- 30. Bjorgul K, Reigstad A. Atypical fracture of the ulna associated with alendronate use. Acta Orthop 2011;82:761-3.ArticlePubMedPMC
- 31. Ito H, Miyakoshi N, Kasukawa Y, et al. Treatment of atypical fracture of the ulnar diaphysis by open reduction and internal fixation with teriparatide. Case Rep Orthop 2019;2019:9103412.ArticlePubMedPMCPDF
- 32. Osada R, Zukawa M, Kimura T. Atypical ulnar fracture associated with long-term bisphosphonate use. J Orthop Sci 2015;20:1132-5.ArticlePubMed
 , Hyun Tak Kang, MD2
, Hyun Tak Kang, MD2 , Jun-Ku Lee, MD2,3
, Jun-Ku Lee, MD2,3







 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 ePub Link
ePub Link Cite
Cite

