Previous issues
- Page Path
- HOME > Browse articles > Previous issues
Review Articles
- Current concepts and applications of bone graft substitutes in orthopedic surgery
- Jae Ho Cho, Hyung Keun Song
- J Musculoskelet Trauma 2025;38(4):169-177. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00248

-
 Abstract
Abstract
 PDF
PDF - Bone defects, which often arise from high-energy injuries, infections, tumor resections, or nonunions, represent a persistent challenge in orthopedic trauma surgery. Autologous bone grafting remains the gold standard due to its unique combination of osteogenic, osteoinductive, and osteoconductive properties. However, issues such as donor site morbidity, limited graft volume, and increased surgical time have driven the development of bone graft substitutes. These substitutes vary widely in origin, composition, biological activity, and mechanical characteristics, encompassing allografts, xenografts, synthetic materials, and biologically enhanced constructs. This review outlines the fundamental biological principles underlying bone regeneration—including osteogenesis, osteoinduction, and osteoconduction—and addresses additional key factors such as biocompatibility, biodegradability, and mechanical strength. Current bone graft materials are classified by biological origin and functional characteristics, with an emphasis on their use in trauma surgery. Particular attention is given to the clinical applications, indications, and limitations of allograft-based solutions (such as structural allografts and demineralized bone matrix), synthetic ceramics (including calcium phosphate and bioactive glass), and biologically enhanced options, such as recombinant growth factors and stem cell therapies. In trauma settings, graft selection must be tailored to the characteristics of the defect, mechanical demands, the biological environment, and patient-specific factors. Integration with surgical technique and fixation is crucial for optimizing outcomes. Although modern substitutes show promise, none fully replicate the complex biology of autografts. Looking ahead, emerging technologies such as 3D printing, nanotechnology, and smart biomaterials offer exciting possibilities but face translational challenges. This review aims to provide practicing orthopedic surgeons with a concise, evidence-based overview of bone substitute options and their roles in trauma care. By applying core biological principles and clinical judgment, surgeons can better navigate the expanding array of graft materials to improve outcomes for patients with complex skeletal defects.
- 3,863 View
- 82 Download

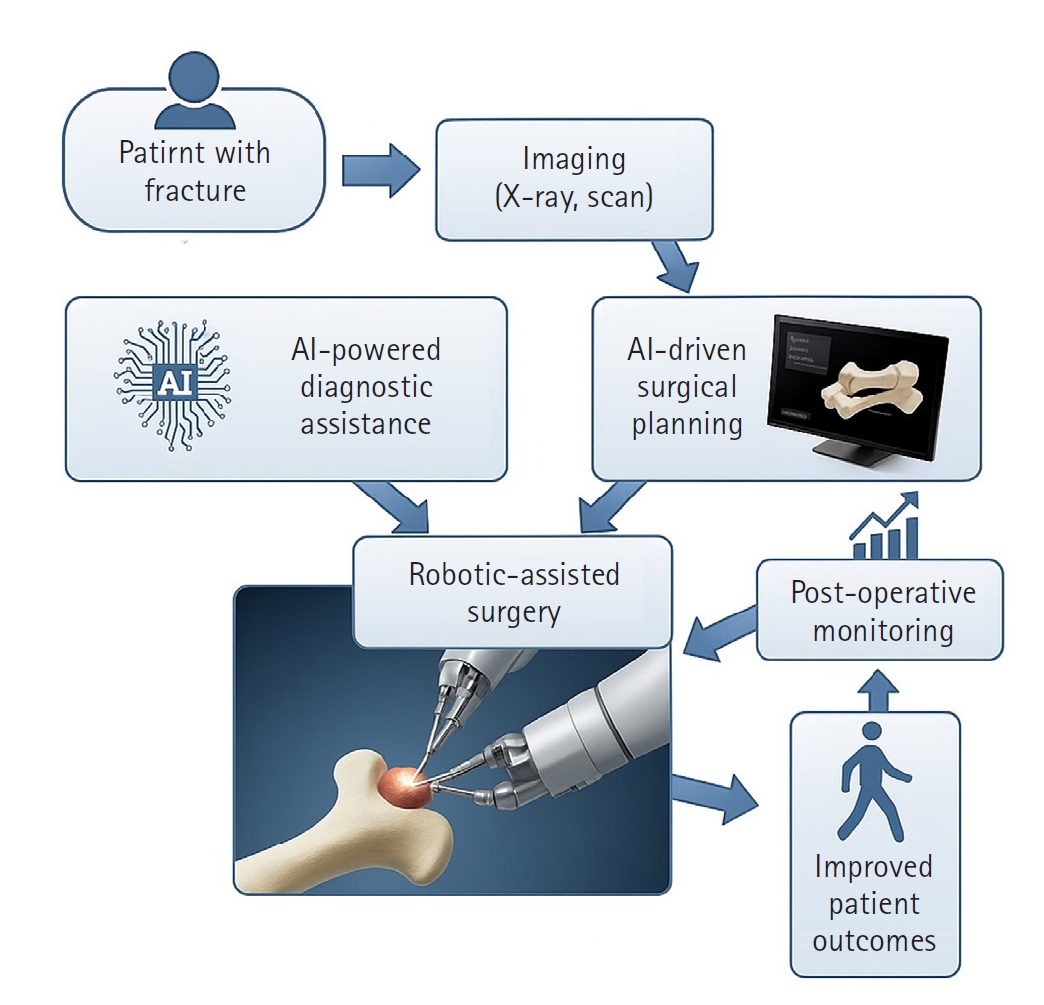
- Innovative applications of artificial intelligence in orthopedics focusing on fracture and trauma treatment: a narrative review
- Chul-Ho Kim, Ji Wan Kim
- J Musculoskelet Trauma 2025;38(4):178-185. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00283
-
 Abstract
Abstract
 PDF
PDF - Artificial intelligence (AI) is bringing about transformative changes in orthopedic surgery, with its potential being particularly prominent in the field of fracture and trauma treatment. This review explores the current applications and future prospects of AI-driven surgical planning and simulation, robot and image-based navigation surgery, and image-assisted diagnostic technologies. Robotic assistance in orthopedic surgery, which was initially applied to improve accuracy in component implantation for knee and hip arthroplasty and to achieve high precision in spinal screw placement, has recently expanded its use to include accurate, minimally invasive reduction of pelvic fractures. In diagnostics, AI aids in the early prediction and classification of ambiguous fractures in various anatomical regions—for example, detecting shoulder or hip fractures, identifying incomplete atypical femur fractures, and classifying femoral neck fractures—through X-ray image analysis. This improves diagnostic accuracy and reduces medical costs. However, significant challenges remain, including high initial costs, steep learning curves, a lack of long-term studies, data bias, and ethical concerns. Continued research, interdisciplinary collaboration, and policy support are crucial for the widespread adoption of these technologies.
- 916 View
- 2,147,483,661 Download

Original Articles
- Correlation of bone mineral density with ankle fractures in older adults in Korea: a retrospective cohort study
- Seung Hyun Lee, Chae Hun Lee, Seo Jin Park, Jun Young Lee
- J Musculoskelet Trauma 2025;38(4):186-192. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00150
-
 Abstract
Abstract
 PDF
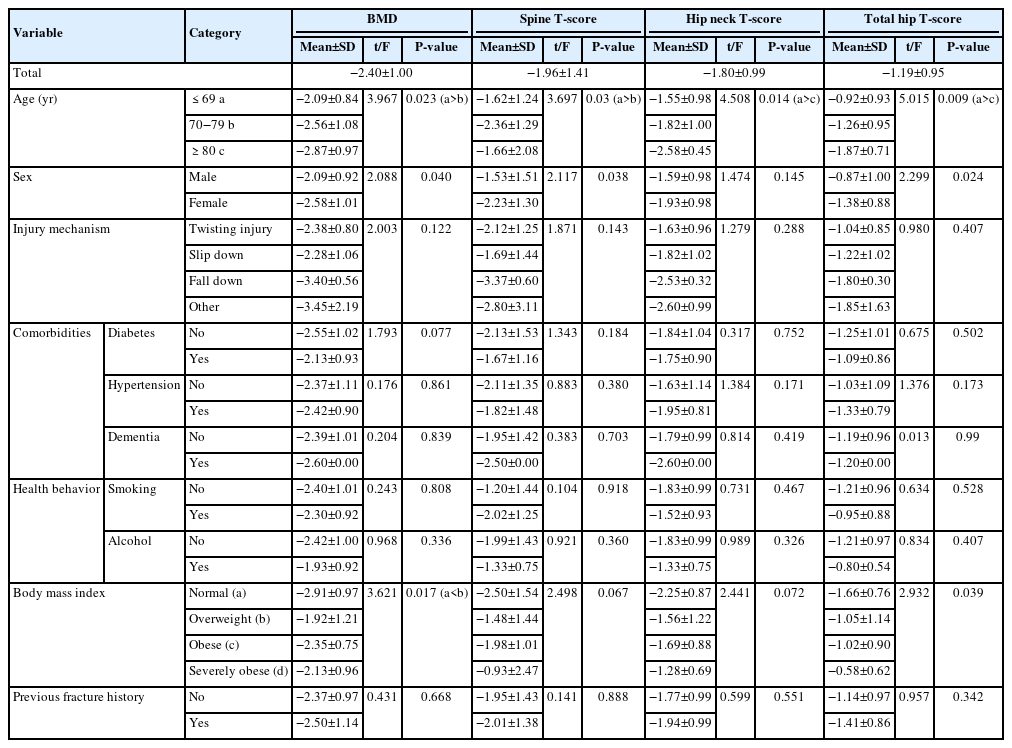
PDF - Background
Bone mineral density (BMD) is well-documented in relation to fractures of the spine, hip, distal radius, and proximal humerus; however, its correlations with other fracture types are less established. This study aimed to analyze BMD and associated risk factors in older adults (≥65 years of age) with osteoporotic ankle fractures. These fractures involve low-energy trauma, resulting from falls from a standing height or lower, and occur from impacts which typically do not cause fractures in individuals with normal bone.
Methods
This retrospective study analyzed data from 1,411 patients diagnosed with ankle fractures admitted to Chosun University Hospital between February 2012 and April 2023. After applying inclusion criteria (age ≥65 years; low energy ankle fracture) and exclusion criteria (high energy trauma, open/multiple fractures, missing dual X-ray absorptiometry [DXA]), 73 of 1,411 patients were analyzed. Lumbar spine, femoral neck, and total hip T scores were obtained with a Horizon Wi DXA scanner, and associations with age, sex, mechanism of injury, comorbidities, smoking status, alcohol consumption, body mass index (BMI), and history of fractures were tested by ANOVA with Scheffe post hoc and Fisher exact tests.
Results
Lower BMD correlated significantly with older age, female sex, and lower BMI (P<0.05) in older adults with ankle fractures. No significant associations were observed for comorbidities (diabetes, hypertension, dementia), smoking, alcohol consumption, injury mechanism, or prior fractures.
Conclusion
These results indicate that older age, female, and lower BMI are linked to reduced BMD in ankle fracture patients over 65 years of age. Focused osteoporosis screening and management may therefore be most beneficial for older, low BMI women presenting with ankle fractures. Level of evidence: IV.
- 831 View
- 2,147,483,670 Download

- Risk factors for ankle fractures in older adults based on clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities in Korea: a retrospective case-control study
- Myeong Jun Song, Se Woong Jang, Jun Young Lee, Seojin Park
- J Musculoskelet Trauma 2025;38(4):193-202. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00143
-
 Abstract
Abstract
 PDF
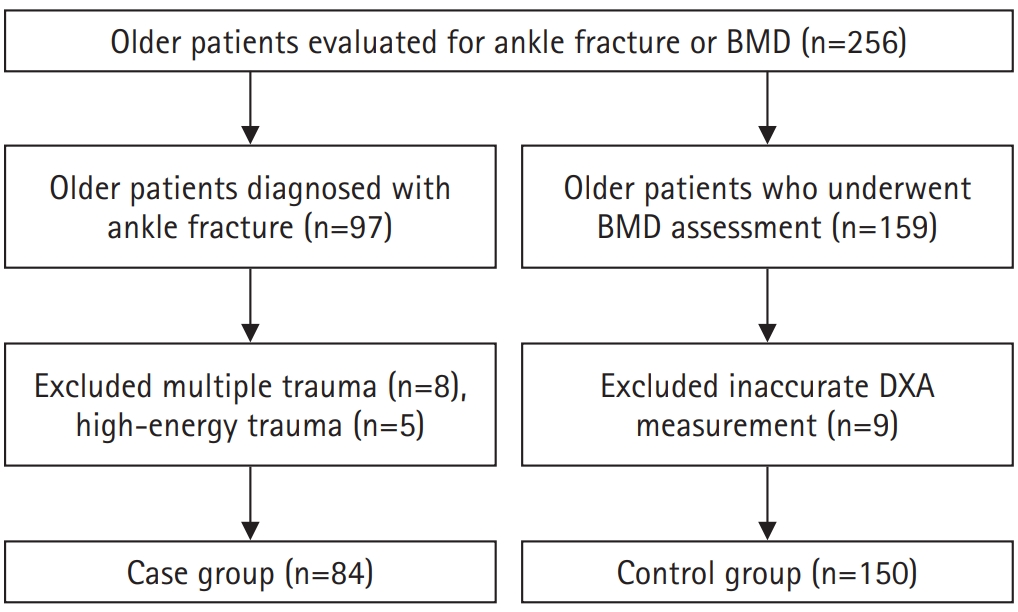
PDF - Background
Ankle fractures are common in older adults; however, their relationship with osteoporotic fractures remains unclear. This study aimed to evaluate potential risk factors for ankle fractures in older adults by analyzing individual clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities.
Methods
We conducted a retrospective case-control study including 84 patients aged ≥65 years with ankle fractures and 150 controls who underwent bone mineral density (BMD) testing without prior ankle fractures. The variables analyzed included age, sex, body mass index, smoking, alcohol consumption, prior fracture history, and comorbidities such as hypertension, diabetes mellitus, and dementia. BMD was measured at the spine, total hip, and femoral neck.
Results
Univariate analysis showed that alcohol consumption, diabetes mellitus, and total hip T-score categories were significantly associated with ankle fractures. In binary logistic regression, alcohol consumption remained significantly associated with higher ankle fracture risk (odds ratio [OR], 5.302; 95% confidence interval [CI], 1.778–15.811; P=0.003), and both osteopenia and osteoporosis at the total hip were also associated with increased risk (OR, 3.260, P=0.049; OR, 3.561, P=0.031, respectively). Diabetes mellitus did not reach statistical significance in the adjusted model (P=0.074). Model fit was adequate (Hosmer-Lemeshow P=0.377), and post hoc power analysis confirmed sufficient sample size.
Conclusions
These findings suggest that lower total hip BMD and alcohol-related factors may be associated with ankle fracture risk in older adults. The FRAX score itself was not calculated; instead, this study focused on analyzing selected clinical components. Limitations include the retrospective design, lack of fall and medication data, and cross-sectional BMD assessment. Level of evidence: III.
- 1,044 View
- 21 Download

- Comparative results of the femoral neck system versus the dynamic hip screw for stable femoral neck fractures in older adults in Korea: a retrospective cohort study
- Byung-Chan Choi, Byung-Woo Min, Kyung-Jae Lee, Jun-Sik Hong
- J Musculoskelet Trauma 2025;38(4):203-211. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00276
-
 Abstract
Abstract
 PDF
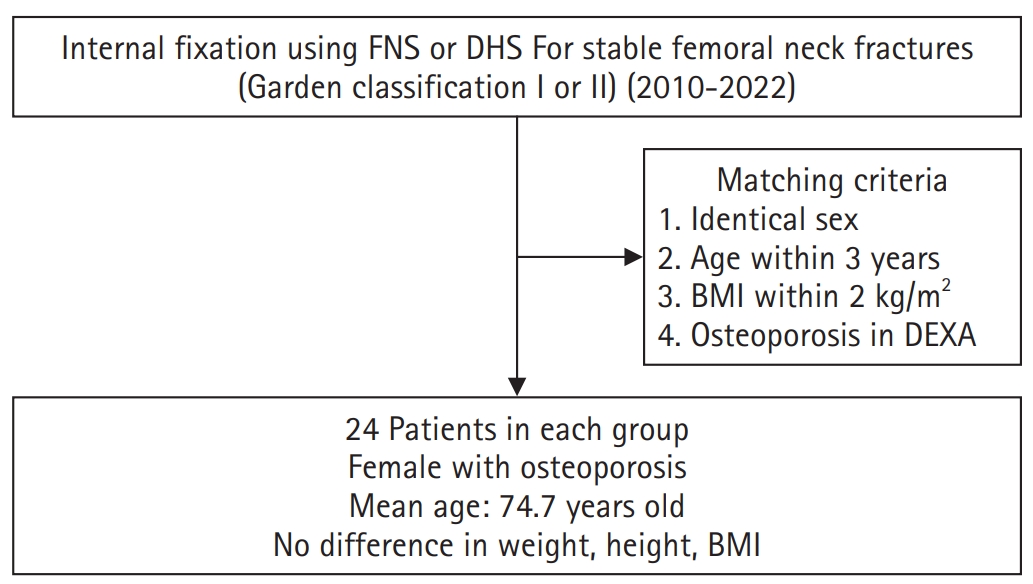
PDF - Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
Methods
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results. Level of evidence: IV.
- 1,494 View
- 20 Download

- Relationship of lateral malleolar fracture patterns to posterior malleolar fracture morphology in supination-external rotation ankle fractures in Korea: a retrospective cohort stduy
- Jong-Eun Kim, Chan-Jin Park, Jun-Young Lee, Keun-Bae Lee, Gun-Woo Lee
- J Musculoskelet Trauma 2025;38(4):212-220. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00234
-
 Abstract
Abstract
 PDF
PDF - Background
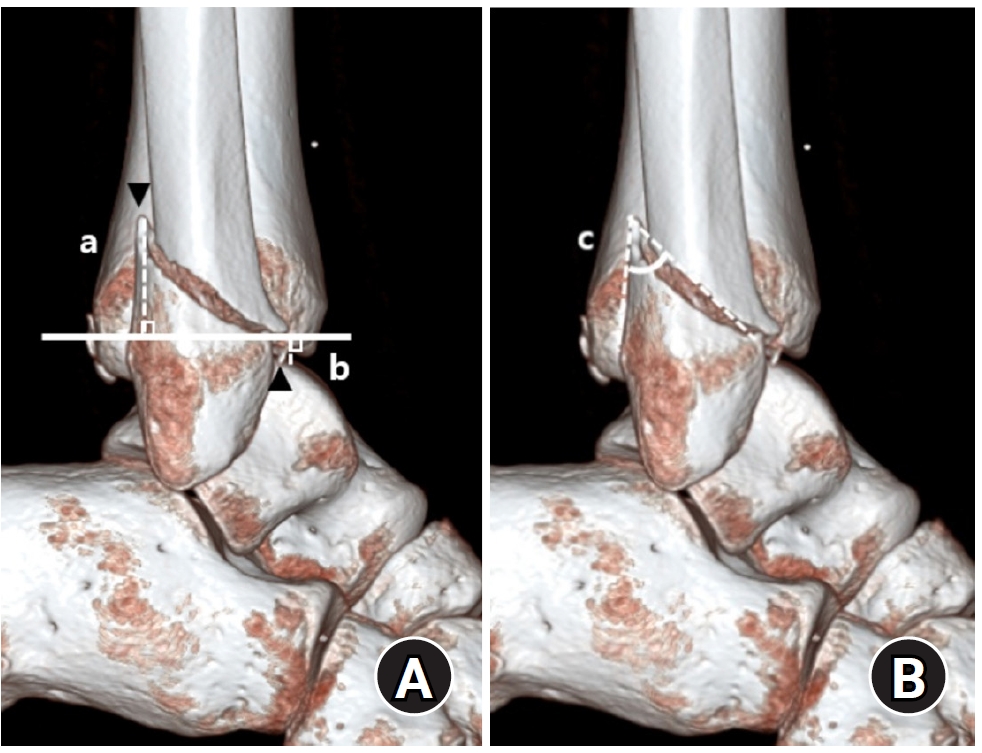
Posterior malleolar fractures frequently accompany rotational ankle fractures. However, the morphological relationship between lateral and posterior malleolar fractures in supination-external rotation (SER) ankle fractures remains unclear. This study aimed to classify lateral malleolar fracture patterns in SER type 3 and 4 ankle fractures and investigated their associations with posterior malleolar fracture morphology.
Methods
We retrospectively reviewed 132 patients with SER type 3 or 4 ankle fractures and concurrent posterior malleolar fractures between January 2016 and December 2021. Lateral malleolar fractures were categorized as fibular fractures extending <4.5 cm proximal to the ankle joint (102 ankles) or fibular fractures extending ≥4.5 cm proximal to the ankle joint (30 ankles) based on posterior cortex height measured using three-dimensional computed tomography (3D-CT). Posterior malleolar fracture morphology was assessed using the Haraguchi and Bartonicek classifications. Quantitative parameters—including fracture height, angle, and articular involvement—were analyzed using 3D-CT imaging.
Results
Fibular fractures extending ≥4.5 cm proximal to the ankle joint were associated with a significantly higher frequency of Haraguchi type II and Bartonicek types 3 and 4 posterior malleolar fractures. This group also exhibited greater articular involvement (19.2% vs. 12.0%) and posterior cortical height (55.4 mm vs. 24.8 mm) compared to the <4.5 cm group (all P<0.001).
Conclusions
In SER type 3 and 4 ankle fractures, a fibular fracture extending ≥4.5 cm proximal to the ankle joint may be associated with posterior malleolar fractures exhibiting greater articular involvement and medial extension. Preoperative evaluation of the lateral malleolar fracture pattern may provide useful insights into posterior malleolar morphology and assist in surgical planning. However, these findings should be interpreted with caution due to inherent study limitations. Level of evidence: IV
- 892 View
- 19 Download

- Hook plate versus periarticular-type volar locking plate for distal radius fractures involving the volar lunate facet in Korea: a retrospective cohort study
- Hyun-Jae Park, Joo-Hak Kim
- J Musculoskelet Trauma 2025;38(4):221-228. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00241
-
 Abstract
Abstract
 PDF
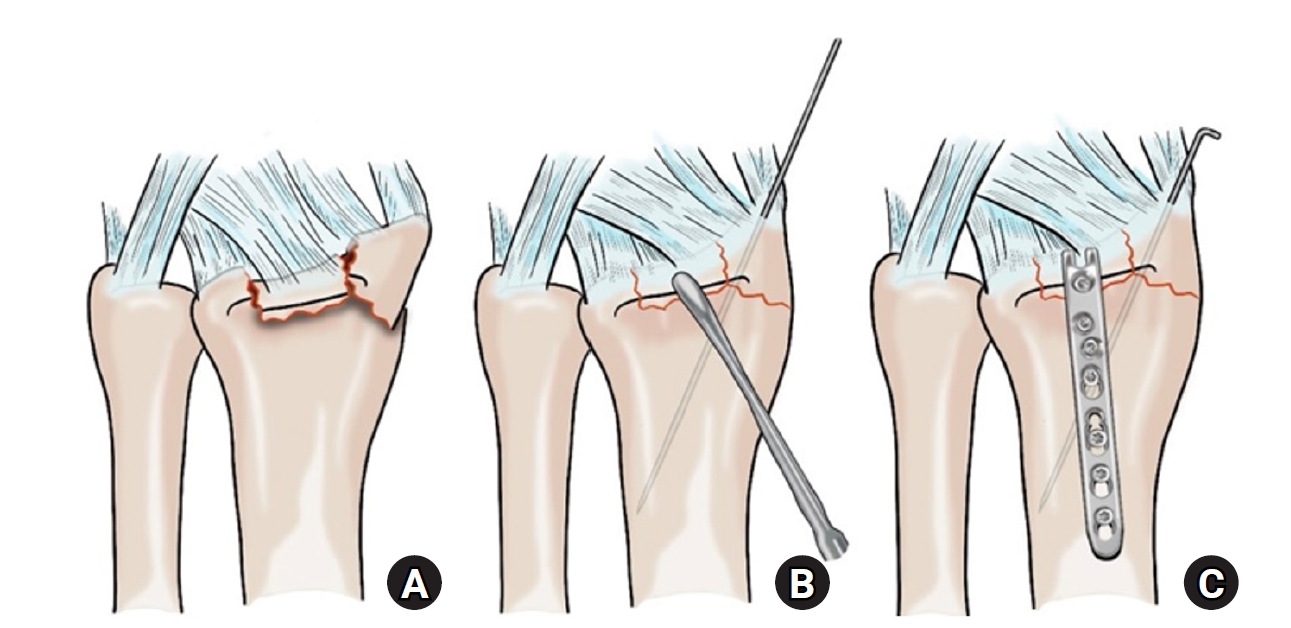
PDF - Background
This study investigated the clinical and radiographic outcomes of hook plate (HP) fixation for volar lunate facet fractures, comparing them with periarticular-type volar locking plates (PVLPs).
Methods
A retrospective review was conducted on 24 patients with distal radius fractures involving volar lunate facet fragments who underwent surgery between January 2016 and April 2021. Patients were divided into two groups: HP (n=12) and PVLP (n=12). Radiographic union, wrist range of motion, Disabilities of the Arm, Shoulder and Hand (DASH) scores, and implant-related complications were compared. Statistical analyses included the Mann-Whitney U test and Fisher exact test.
Results
Radiographic union was achieved in all patients (100%), without secondary displacement or hardware failure. No significant differences were observed between the two groups in wrist flexion (P=0.152), extension (P=0.832), pronation (P=0.792), or supination (P=0.328). The mean DASH scores were 12.8±5.5 in the HP group and 14.6±6.0 in the volar plate group (P=0.449). One patient in the HP group experienced mild flexor tendinopathy that resolved with conservative management. No cases of tendon rupture or early reoperation were reported.
Conclusions
Fixation of volar lunate facet fractures using a HP yielded clinical and radiographic outcomes comparable to those of PVLPs, with a low rate of complications and reliable bony union. Due to its mechanical stability, compatibility with standard surgical approaches, and low risk of flexor tendon irritation, the HP may serve as a valuable alternative for managing volar lunate facet fractures. Level of evidence: IV.
- 319 View
- 10 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 First
First Prev
Prev


