Abstract
-
Background
This study investigated the clinical and radiographic outcomes of hook plate (HP) fixation for volar lunate facet fractures, comparing them with periarticular-type volar locking plates (PVLPs).
-
Methods
A retrospective review was conducted on 24 patients with distal radius fractures involving volar lunate facet fragments who underwent surgery between January 2016 and April 2021. Patients were divided into two groups: HP (n=12) and PVLP (n=12). Radiographic union, wrist range of motion, Disabilities of the Arm, Shoulder and Hand (DASH) scores, and implant-related complications were compared. Statistical analyses included the Mann-Whitney U test and Fisher exact test.
-
Results
Radiographic union was achieved in all patients (100%), without secondary displacement or hardware failure. No significant differences were observed between the two groups in wrist flexion (P=0.152), extension (P=0.832), pronation (P=0.792), or supination (P=0.328). The mean DASH scores were 12.8±5.5 in the HP group and 14.6±6.0 in the volar plate group (P=0.449). One patient in the HP group experienced mild flexor tendinopathy that resolved with conservative management. No cases of tendon rupture or early reoperation were reported.
-
Conclusions
Fixation of volar lunate facet fractures using a HP yielded clinical and radiographic outcomes comparable to those of PVLPs, with a low rate of complications and reliable bony union. Due to its mechanical stability, compatibility with standard surgical approaches, and low risk of flexor tendon irritation, the HP may serve as a valuable alternative for managing volar lunate facet fractures.
-
Level of evidence
IV.
-
Keywords: Wrist injuries, Internal fracture fixation, Radius fractures, Bone plates, Lunate bone
Introduction
Background
Distal radius fractures are one of the most common fractures seen in elderly patients. However they are known to be particularly challenging to treat when accompanied by a volar lunate facet fragment [
1]. Anatomically, the short radiolunate ligament and the anterior distal radioulnar ligament originate from the edge of the volar lunate facet, and their deforming forces can cause dislocation of the fracture fragment if fixation is insufficient, resulting in wrist joint instability [
2].
The volar lunate facet of the distal radius is a critical structure that contributes to load transmission through both the radiocarpal and distal radioulnar joints and serves as the primary restraint against volar subluxation of the distal articular surface [
2-
4]. Inadequate reduction and fixation of this fragment may result in complications such as secondary displacement, underscoring the need for thorough preoperative planning and evaluation [
1,
5,
6]. Moreover, the anatomical complexity of the distal radius adds to the technical challenge of achieving stable fixation, particularly for surgeons with limited experience in managing intraarticular fractures [
1].
Several prior studies have explored the option of extending or positioning the volar locking plate more proximally to provide enhanced support to the ulnar aspect of the distal radius, particularly the lunate facet [
1]. While this modification can reinforce fixation in that region, placing the plate distal to the watershed line to address very distal fractures may lead to complications such as flexor tendon irritation, tendinitis, or even rupture [
3]. Furthermore, in cases where the fracture fragment is too small, the standard volar locking plate may fail to offer adequate stability.
Numerous surgical techniques have been explored to achieve stable fixation of volar lunate facet fragments in distal radius fractures, yet their outcomes have been inconsistent and often accompanied by complications such as flexor tendon irritation or rupture [
7-
10]. A promising alternative involves the use of a hook plate (HP), a hook-shaped metal implant originally developed for distal ulnar fixation. This device has demonstrated favorable outcomes in securing the lunate facet fragment and promoting bone union, while minimizing the risk of complications [
9,
11]. The HP is well suited in terms of size, contour, and length for supporting the volar ulnar corner of the distal radius. It also offers technical convenience, as it can be implanted through a standard volar approach without the need for additional instruments or dorsal exposure.
The purpose of this study was to evaluate the clinical and radiographic outcomes of internal fixation using a HP in distal radius fractures involving the volar lunate facet fragment. To validate its effectiveness, we compared outcomes with those of periarticular-type volar locking plate (PVLP) fixation. We hypothesized that HP fixation would provide stable fragment control, facilitate reliable union, and achieve comparable functional outcomes, while minimizing implant-related complications such as flexor tendon irritation.
Methods
Ethics statement
This study was approved by the Institutional Review Board (IRB) of at Myongji Hospital (IRB No., 2022-11-026). The requirement for informed consent was waived due to the retrospective nature of the study.
Study design
It is a retrospective cohort study based on chart review from the electronic medical records. It was described according to the STROBE statement (
https://www.strobe-statement.org/).
It was conducted at Myongji Hospital Between January 2016 and April 2021. Surgical procedures were performed under general anesthesia with the patient in the supine position and a pneumatic tourniquet applied to the upper limb. A modified Henry approach was used [
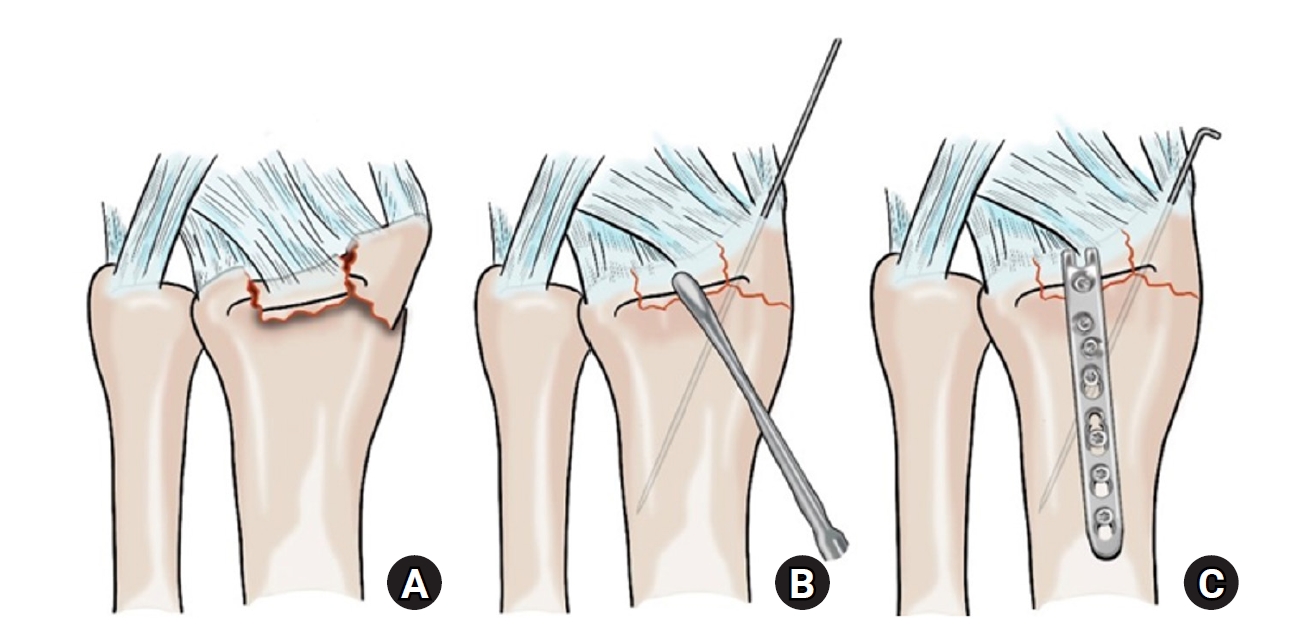
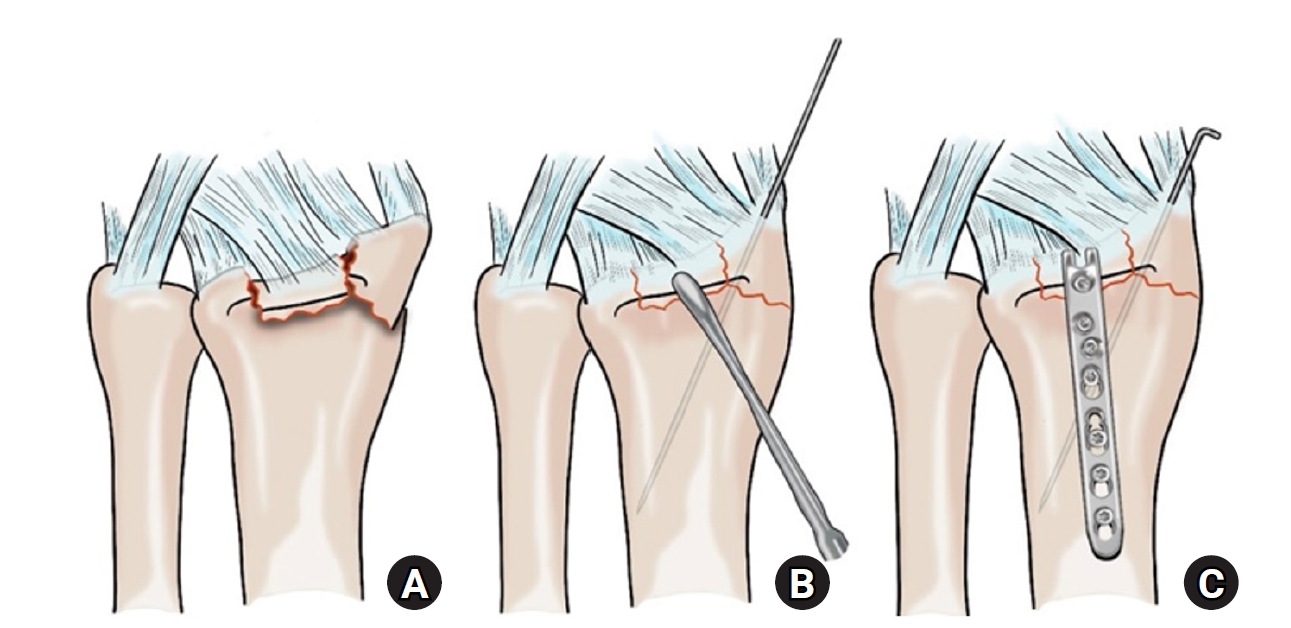
12]. After incising the sheath of the flexor carpi radialis tendon, the tendon was retracted ulnarly to expose the floor of its compartment. The pronator quadratus was then incised along its ulnar border and elevated subperiosteally to expose the fracture site. Following hematoma evacuation and debridement, reduction was achieved using reduction forceps. In the HP group, the volar lunate facet fragment was reduced using reduction forceps and stabilized with a HP applied to the volar-ulnar corner of the distal radius. Screws were inserted for fixation, and if fragment size permitted, additional screws were used to secure the lunate facet directly (
Figs. 1,
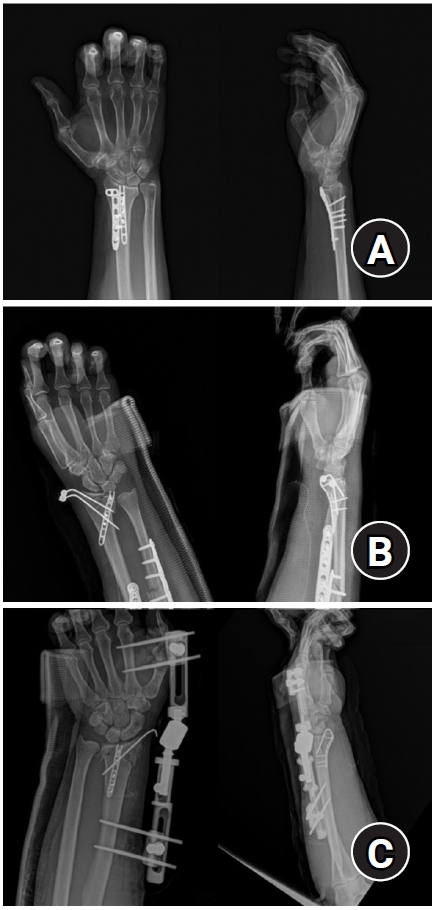
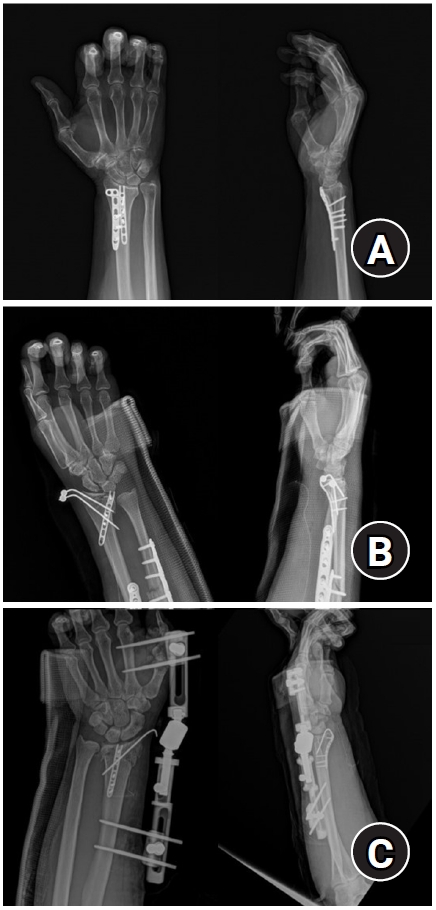
2). Additional fixation, such as a LCP-L distal radius plate (
Fig. 3A), percutaneous pinning (
Fig. 3B), or percutaneous pinning with external fixation (
Fig. 3C), was applied as required based on fracture complexity and the presence of radial styloid or articular comminution. In the PVLP group, fracture reduction and fixation were performed using the PVLPs alone, without HP application (
Fig. 4). In all cases, intraoperative fluoroscopy was used to confirm reduction and implant positioning, followed by irrigation and layered wound closure.
Adult patients aged 18 years or older who underwent surgical treatment for distal radius fractures with volar lunate facet fragments were screened for eligibility.
Fractures were classified according to the AO/OTA classification system, and only those classified as type B3, C2, or C3 were included. Patients were excluded if they had open fractures, a history of previous ipsilateral wrist surgery, or incomplete radiographic or clinical follow-up. Among them, patients who had a minimum follow-up period of 6 months after surgery were included. A total of 24 patients met the inclusion criteria and were divided into two groups based on the fixation method used. The HP group included 12 patients who underwent fixation with a 2.0 mm locking compression plate (LCP) distal ulnar HP (Synthes), with or without adjunctive fixation. Based on the fracture configuration, additional fixation such as a 2.4 mm LCP-L distal radius plate (Synthes), percutaneous pinning, or percutaneous pinning with external fixation was applied as necessary. The PVLP group consisted of 12 patients treated with PVLP alone. In this group, implants included the 2.4 mm variable angle LCP volar rim distal radius plate (Synthes) and the Acu-Loc volar distal radius plate (Acumed).
Variables
The primary outcome was radiographic union of the volar lunate facet fragment. Secondary outcomes included active range of motion, Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire, implant-related complications (including implant failure, infection, tendon rupture, flexor tendinopathy), and the need for reoperation.
Data sources/measurement
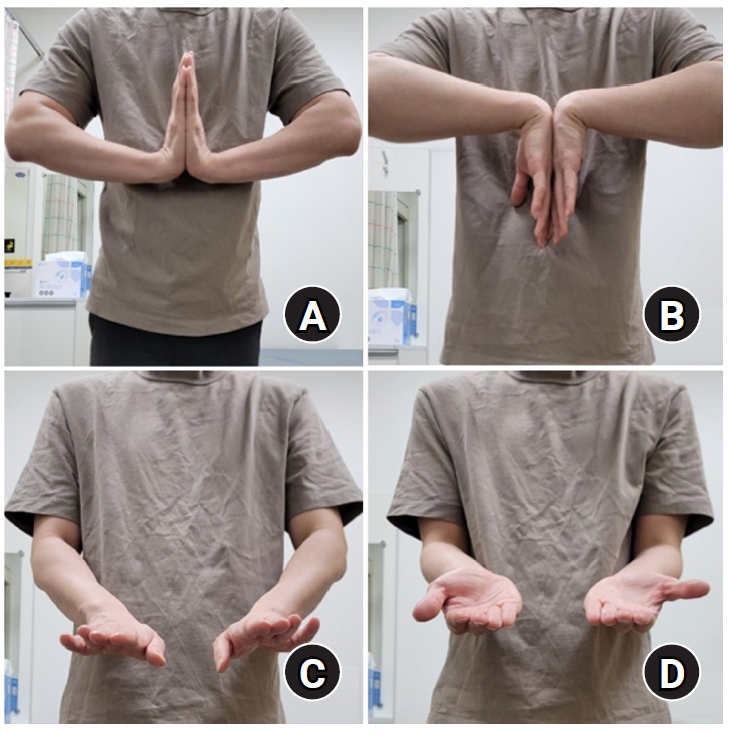
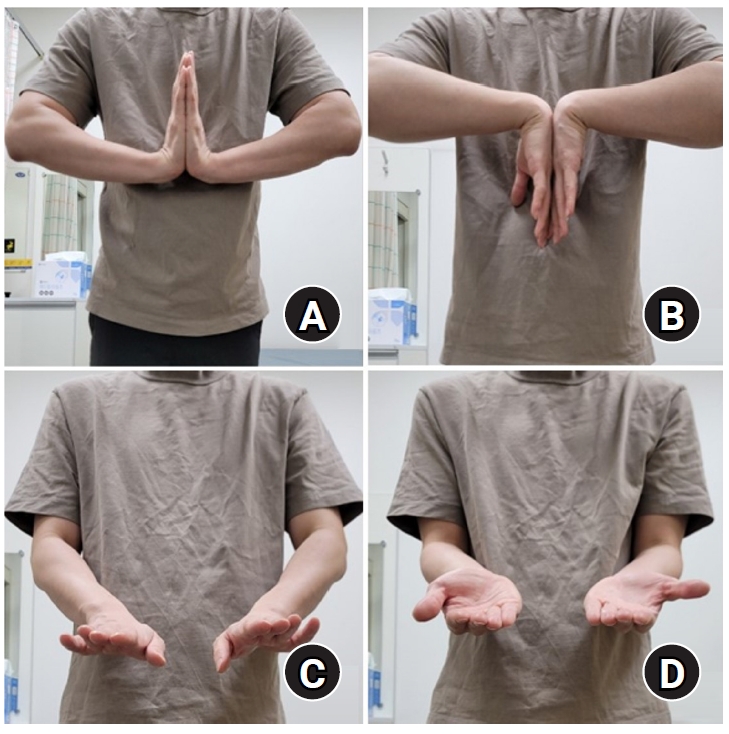
Standard anteroposterior and lateral radiographs were obtained at 2, 4, 6, and 12 weeks postoperatively to evaluate maintenance of reduction and radiographic union. At the final follow-up visit, wrist range of motion—including flexion, extension, pronation, and supination—was measured using a goniometer by an independent evaluator (
Fig. 5).
To minimize measurement bias, range of motion was assessed by an independent evaluator not involved in the surgery. All radiographs were reviewed by two orthopedic surgeons independently.
Study size
No sample size estimation was performed; all eligible patients during the study period were included.
Statistical methods
Demographic variables, fracture classification, fixation method, and clinical outcomes were compared between the HP and PVLP groups. Continuous variables such as range of motion angles and visual analog scale scores were expressed as mean±standard deviation and analyzed using the Mann-Whitney U test. Categorical variables, including union rate and complication incidence, were analyzed using Fisher exact test. A P-value of less than 0.05 was considered statistically significant. All statistical analyses were performed using the IBM SPSS ver. 25.0 (IBM Corp.). There were no missing outcome data; all patients completed clinical and radiographic follow-up.
Results
Participants
A total of 24 patients with distal radius fractures involving volar lunate facet fragments were included in the study, comprising 12 patients in the HP group and 12 patients in the PVLP group. The mean age was 54.9 years (range, 25–77 years) in the HP group and 60.1 years (range, 28–84 years) in the PVLP group. There were eight males and four females in the HP group, and four males and eight females in the PVLP group. According to the AO/OTA classification, eight patients (67%) in the HP group and 11 patients (92%) in the PVLP group had type B3 fractures, one patient (8%) in the HP group and 0 patient in the PVLP group had type C2, while three patients (25%) in the HP and one patient (8%) in the PVLP group had C3 fractures. The mean body mass index (BMI) was 25.1 kg/m² (range, 20.8–30.0) in the HP group and 24.2 kg/m² (range, 21.2–29.1) in the PVLP group (
Table 1).
In the HP group, all patients underwent internal fixation of the lunate facet fragment using a 2.0 mm LCP distal ulna HP. Among them, two patients (17%) were treated with the HP alone, six patients (50%) received an additional volar locking plate, three patients (25%) underwent adjunctive percutaneous pinning, and one patient (8%) received both percutaneous pinning and external fixation. The choice of additional fixation was based on the severity of articular comminution and the presence of radial styloid fractures. No statistically significant differences in union rate were found among the different fixation techniques (P=1.000) (
Table 2).
In the PVLP group, all patients underwent internal fixation using a PVLP without application of a HP. The implants used included the 2.4 mm variable angle LCP volar rim distal radius plate (Synthes) in seven patients and the Acu-Loc volar distal radius plate (Acumed) in five patients. No statistically significant difference in union rate was found among the different plate types (P=1.000) (
Table 3).
Postoperative radiographs obtained at 2, 4, 6, and 12 weeks demonstrated that all patients with available follow-up maintained stable reduction without displacement of the lunate facet fragment. Radiographic union was confirmed in all patients (100%) in both groups. Computed tomography was not routinely performed before implant removal; instead, articular congruency was assessed using plain radiographs obtained prior to hardware removal, including anteroposterior, both oblique, and lateral views. No malunion was found, and articular congruency was intact in both groups. None of the patients in either group demonstrated secondary displacement or hardware loosening during the follow-up period (
Tables 2,
3).
Functional outcomes were evaluated at the final follow-up. The average wrist range of motion at final follow-up was as follows: in the HP group, flexion was 80.0°±0.0°, mean extension was 65.0°±10.0°, mean pronation was 86.7°±8.9°, and mean supination was 80.0°±0.0°; in the PVLP group, flexion was 78.3°±3.9°, extension 64.2°±9.0°, pronation 87.5°±6.2°, and supination 79.2°±2.9°. There were no statistically significant differences in range of motion between the two groups (respectively, P=0.152, P=0.832, P=0.792, P=0.328). The mean DASH scores were 12.8±5.5 in the HP group and 14.6±6.0 in the PVLP group. There were no statistically significant differences in the mean DASH scores between the two groups (P=0.449) (
Table 4).
No patient experienced major complications such as implant failure, infection, or tendon rupture. One individual in the HP group, who had both a HP and a volar locking plate, developed mild flexor tendinopathy. The symptoms were managed with conservative measures until the scheduled implant removal. The early reoperation rate was zero in both groups. After solid bone healing was verified, we removed the hardware in every case—on average, 10.8±3.3 months after the index surgery in the HP group and 10.4±3.3 months in the PVLP group (P=0.805) (
Table 5).
Discussion
Key results
To evaluate the clinical and radiographic outcomes of internal fixation, 24 patients were analyzed, evenly divided between the HP and PVLP groups. Radiographic union was achieved in all patients without displacement, malunion, or hardware failure. Wrist range of motion and DASH scores did not differ significantly between the groups. One HP patient developed mild flexor tendinopathy that resolved conservatively. No infections, tendon ruptures, or early reoperations occurred. Hardware removal was performed in all patients after solid healing.
Interpretation/comparison with previous studies
The volar lunate facet serves as a critical structure for both radiocarpal and distal radioulnar joint stability. Due to the anatomical location and ligamentous attachments, even small displacement can compromise wrist function and lead to treatment failure if not adequately reduced and stabilized [
3]. Moreover, the load on the lunate facet increases during functional forearm postures, and inadequate fixation of the volar margin fracture fragment can lead to displacement due to deformational stress [
3].
Achieving anatomical reduction and stable fixation of the volar lunate facet fragment is technically demanding, particularly for less experienced surgeons. The widely used modified Henry approach may be limited in providing clear visualization of the volar-ulnar aspect of the distal radius [
12]. In particular, excessive retraction of soft tissues to improve access can increase the risk of median nerve injury [
12]. To address this issue, Tordjman et al. [
13] proposed a palmar-radial approach that utilizes the interval between the flexor tendons and neurovascular structures to improve access to the ulnar side of the distal radius while minimizing retraction-related complications.
Despite advancements in volar locking plate design, most implants are constrained to placement proximal to the watershed line due to their size and shape. When placed more distally to support lunate facet fragments, volar plates may cause flexor tendon irritation, tendinosis, or even rupture [
7,
8]. Several alternative techniques have been developed to overcome these limitations. For example, O'Shaughnessy et al. [
9] designed a volar HP specifically for lunate facet support, though some patients required early plate removal due to tendon irritation. Moore et al. [
14] introduced a spring-wire augmentation technique, and Minato et al. [
10] proposed loop-wiring fixation for volar rim fragments; however, these approaches often entail technical complexity or increased risk of tendon injury. Similarly, Jeon et al. [
5] used tension band wiring through the posterior cortex, but reported cases of extensor tendon irritation. Imatani et al. [
11] described the plate buttress and double-tiered subchondral support (PD) technique using an anatomical low-profile volar plate, which showed favorable outcomes but still requires a dedicated implant system.
In contrast, the present study utilized a HP, originally designed for distal ulna. Its hook structure provided direct buttress support to the volar-ulnar corner of the distal radius, especially in cases where the fragment was too small or distal to allow secure fixation with locking screws alone. Importantly, the narrower width and compact shape of the HP make it less likely to impinge on the flexor tendons although it crosses the watershed line; whereas only one patient in our study experienced mild flexor tendinopathy in the HP group, which resolved with conservative treatment and did not necessitate early implant removal. No cases of flexor tendon rupture, hardware failure, or early reoperation were observed.
Furthermore, the HP can be applied using a single volar approach, avoiding the need for dorsal dissection or complex implant setups. Because it is a readily available and commonly stocked implant, it may be a particularly attractive option in cases where specialized fixation systems such as the PD plate is not available. Clinical and radiographic outcomes in the HP group were comparable to those observed in the PVLP group, with similar union rates, range of motion, DASH scores, and complication profiles.
Limitations
First, due to its retrospective design, there is a potential for selection bias. The small number of cases also limits the ability to detect subtle differences in clinical outcomes. Another limitation is that the PVLP group included more complex distal radius fractures, not just isolated volar lunate facet fractures. This mix of cases may have affected the comparison between the two fixation methods. However, such inclusion reflects real clinical practice, where PVLPs are often used for multifragmentary intraarticular fractures involving the lunate facet. Despite these limitations, the findings offer useful insight into the practical strengths and weaknesses of using a HP for volar marginal fragment fixation.
Conclusions
Using a HP to fix distal radius fractures that involve the volar lunate facet showed good clinical and radiographic results, similar to those seen with PVLPs. The HP gave solid buttress support to the lunate facet, led to reliable bone healing, and had few complications. Since this implant is easy to use through a standard volar approach, is commonly available in most operating rooms, and causes little risk of flexor tendon irritation, it can be a useful option—especially when the fracture fragment is small or located very distally. Larger, prospective studies will be helpful to confirm these findings.
Article Information
-
Author contribution
Conceptualization: JHK. Data curation: HJP, JHK. Formal analysis: HJP, JHK. Supervision: JHK. Validation: JHK. Writing-original draft: HJP. Writing-review & editing: HJP, JHK. All authors have read and approved the final version of the manuscript.
-
Conflict of interests
Joo-Hak Kim is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
-
Funding
None.
-
Data availability
Contact the corresponding author for data availability.
-
Acknowledgments
None.
-
Supplementary materials
None.
Fig. 1.Surgical procedure. (A) Volar lunate facet fragment after distal radius fracture. (B) Reduction of the fragment and temporary fixation with a Kirschner wire. (C) Application of a hook plate to the volar aspect of the distal radius; additional percutaneous pinning was performed when plate fixation alone was insufficient.
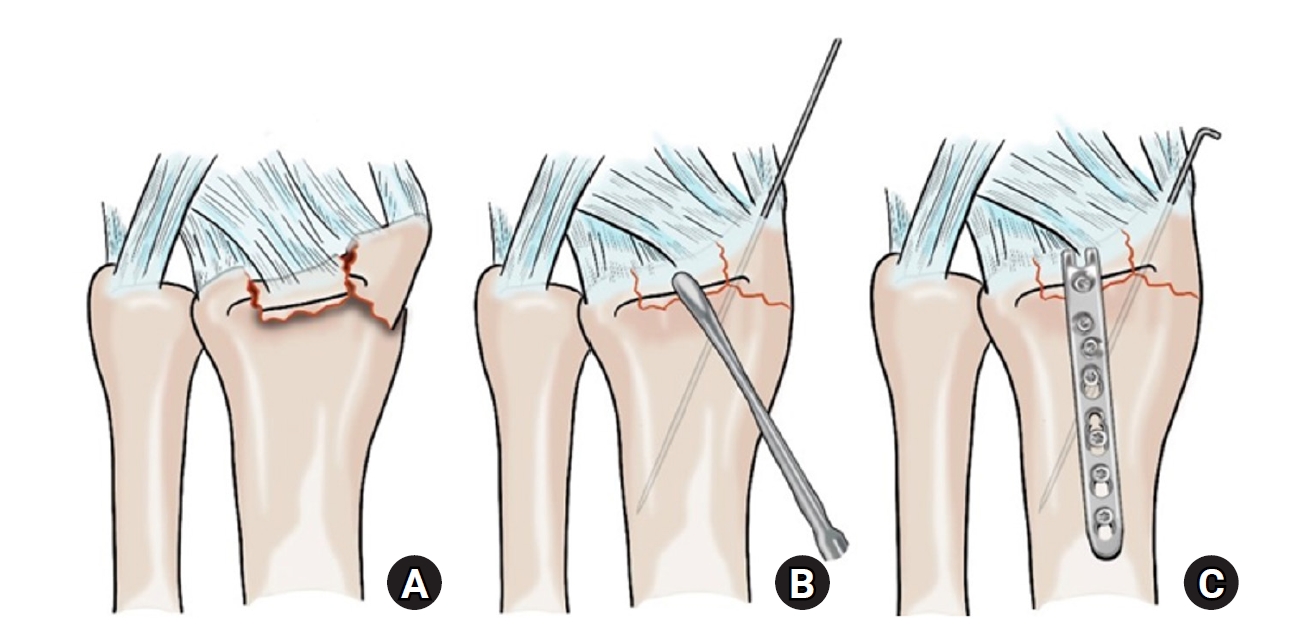
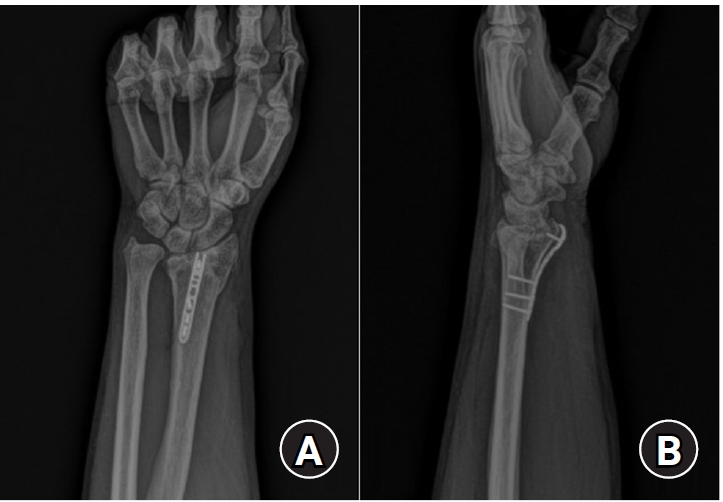
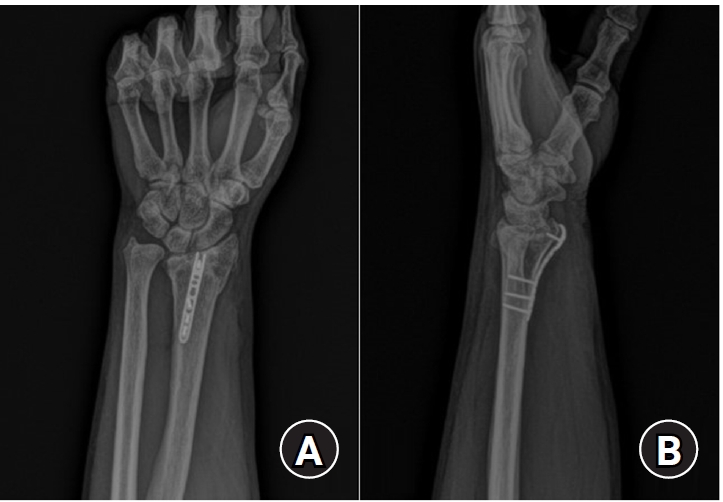
Fig. 2.Postoperative radiographs (A) anteroposterior and (B) lateral: a 2.0 mm locking compression plate distal ulnar hook plate (Synthes) used for fixation in a distal radius fracture with a volar lunate facet fragment.
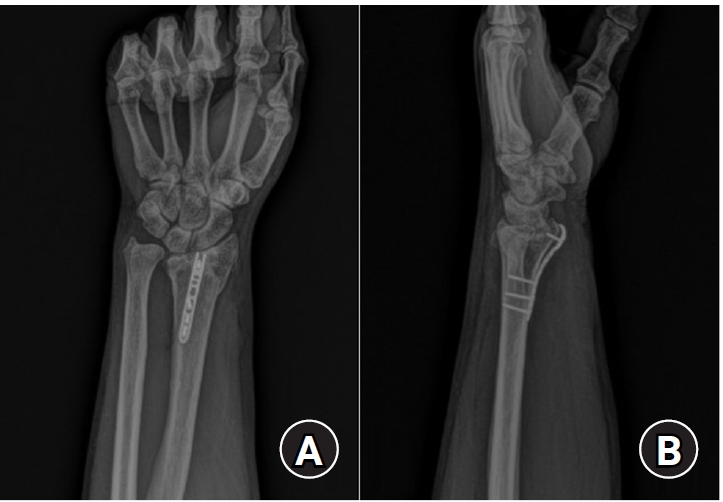
Fig. 3.Postoperative radiographs (anteroposterior and lateral). (A) Volar articular marginal fragment of the distal radius fixed by two plates: a standard 2.4 mm LCP-L distal radius plate (Synthes) and a 2.0 mm locking compression plate distal ulnar hook plate (Synthes). (B) Additional percutaneous pinning after plating. (C) Additional percutaneous pinning and external fixator after plating.
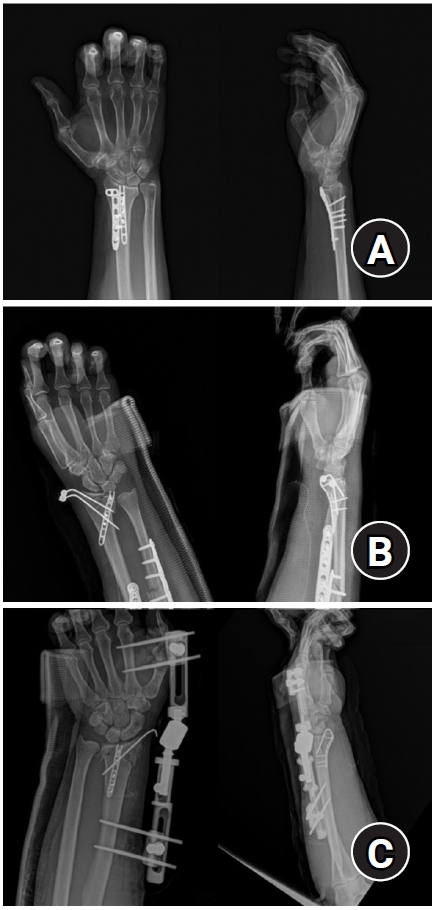
Fig. 4.Postoperative radiographs (anteroposterior and lateral). (A) A 2.4 mm variable angle locking compression plate volar rim distal radius plate (Synthes) used for fixation in a distal radius fracture with a volar lunate facet fragment. (B) Acu-Loc volar distal radius plate (Acumed) used for fixation in a distal radius fracture with a volar lunate facet fragment.

Fig. 5.Wrist range of motion—including (A) flexion, (B) extension, (C) pronation, and (D) supination—was measured at the final follow-up.
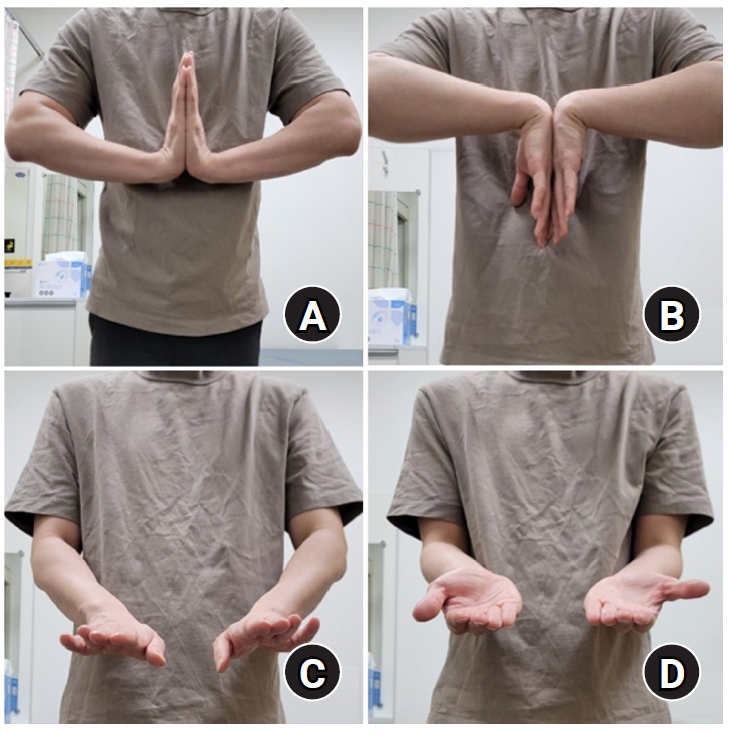
Table 1.Demographic characteristics
|
Variable |
HP group (n=12) |
PVLP group (n=12) |
P-value |
|
Age (yr) |
54.9±13.8 |
60.1±15.1 |
0.392 |
|
BMI (kg/m2) |
25.1±3.0 |
24.2±2.8 |
0.436 |
|
Sex (male:female) |
8 (67):4 (33) |
4 (33):8 (67) |
0.221 |
|
Dominant hand (right:left) |
7 (58):5 (42) |
11 (100):0 (0) |
0.056 |
|
AO type (B3:C2:C3) |
8 (67):1 (8):3 (25) |
11 (92):0 (0):1 (8) |
0.290 |
Table 2.Fixation techniques and radiographic union rate in the hook plate (HP) group
|
Variable |
HP group (n=12) |
|
Hook plate only |
2 |
|
Hook plate+volar locking plate (LDRS) |
6 |
|
Hook plate+percutaneous pinning |
3 |
|
Hook plate+pinning and external fixation |
1 |
|
Radiographic union rate (%) |
100 |
|
Union rate comparison among the techniques |
P=1.000 |
Table 3.Fixation techniques and radiographic union rate in the PVLP group
|
Variable |
PVLP group (n=12) |
|
Synthes (2.4-mm variable angle LCP volar rim distal radius plate) |
7 |
|
Acumed (Acu-Loc volar distal radius plate) |
5 |
|
Radiographic union rate (%) |
100 |
|
Union rate comparison among the techniques |
P=1.000 |
Table 4.Comparison of wrist range of motion and functional outcomes between HP and PVLP groups
|
Variable |
HP group |
PVLP group |
P-value |
|
Flexion (°) |
80.0±0.0 |
78.3±3.9 |
0.152 |
|
Extension (°) |
65.0±10.0 |
64.2±9.0 |
0.832 |
|
Pronation (°) |
86.7±8.9 |
87.5±6.2 |
0.792 |
|
Supination (°) |
80.0±0.0 |
79.2±2.9 |
0.328 |
|
DASH |
12.8±5.5 |
14.6±6.0 |
0.449 |
Table 5.Comparison of complications and reoperation outcomes between HP and PVLP groups
|
Variable |
HP group |
PVLP group |
P-value |
|
Overall |
1 |
0 |
1.0 |
|
Implant failure |
0 |
0 |
- |
|
Infection |
0 |
0 |
- |
|
Tendon rupture |
0 |
0 |
- |
|
Flexor tendinopathy |
1 |
0 |
1.0 |
|
Early reoperation |
0 |
0 |
- |
|
Hardware removal timing (mo), mean±SD |
10.8±3.3 |
10.4±3.3 |
0.805 |
References
- 1. Harness NG, Jupiter JB, Orbay JL, Raskin KB, Fernandez DL. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am 2004;86:1900-8.ArticlePubMed
- 2. Andermahr J, Lozano-Calderon S, Trafton T, Crisco JJ, Ring D. The volar extension of the lunate facet of the distal radius: a quantitative anatomic study. J Hand Surg Am 2006;31:892-5.ArticlePubMed
- 3. Genda E, Horii E. Theoretical stress analysis in wrist joint--neutral position and functional position. J Hand Surg Br 2000;25:292-5.ArticlePubMedPDF
- 4. Rikli DA, Honigmann P, Babst R, Cristalli A, Morlock MM, Mittlmeier T. Intra-articular pressure measurement in the radioulnocarpal joint using a novel sensor: in vitro and in vivo results. J Hand Surg Am 2007;32:67-75.ArticlePubMed
- 5. Jeon N, Oh JK, Cho JW, Kim Y. Tension band wiring technique for distal radius fracture with a volar articular marginal fragment: technical note. J Korean Fract Soc 2020;33:38-42.ArticlePDF
- 6. Obata H, Baba T, Futamura K, et al. Difficulty in fixation of the volar lunate facet fragment in distal radius fracture. Case Rep Orthop 2017;2017:6269081.ArticlePubMedPMCPDF
- 7. Kara A, Celik H, Oc Y, Uzun M, Erdil M, Tetik C. Flexor tendon complications in comminuted distal radius fractures treated with anatomic volar rim locking plates. Acta Orthop Traumatol Turc 2016;50:665-9.ArticlePubMedPMC
- 8. Beck JD, Harness NG, Spencer HT. Volar plate fixation failure for volar shearing distal radius fractures with small lunate facet fragments. J Hand Surg Am 2014;39:670-8.ArticlePubMed
- 9. O'Shaughnessy MA, Shin AY, Kakar S. Volar marginal rim fracture fixation with volar fragment-specific hook plate fixation. J Hand Surg Am 2015;40:1563-70.ArticlePubMed
- 10. Minato K, Yasuda M, Shibata S. A loop-wiring technique for volarly displaced distal radius fractures with small thin volar marginal fragments. J Hand Surg Am 2020;45:261.e1-7.ArticlePubMed
- 11. Imatani J, Kondo H. Volar lunate facet rim fractures: K-I classification and technique. J Wrist Surg 2021;11:230-7.ArticlePubMedPMC
- 12. Conti Mica MA, Bindra R, Moran SL. Anatomic considerations when performing the modified Henry approach for exposure of distal radius fractures. J Orthop 2016;14:104-7.ArticlePubMedPMC
- 13. Tordjman D, Hinds RM, Ayalon O, Yang SS, Capo JT. Volar-ulnar approach for fixation of the volar lunate facet fragment in distal radius fractures: a technical tip. J Hand Surg Am 2016;41:e491-500.ArticlePubMed
- 14. Moore AM, Dennison DG. Distal radius fractures and the volar lunate facet fragment: Kirschner wire fixation in addition to volar-locked plating. Hand (N Y) 2014;9:230-6.ArticlePubMedPDF
 , Joo-Hak Kim
, Joo-Hak Kim




 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

