Abstract
-
Background
This study aimed to compare the clinical and radiological outcomes of the femoral neck system (FNS) and the dynamic hip screw (DHS) for the internal fixation of stable femoral neck fractures in older adults.
-
Methods
This retrospective cohort study included 48 matched older adult patients based on sex, age, BMI, and osteoporosis status, who had undergone internal fixation with either FNS or DHS for stable femoral neck fractures between January 2010 and December 2022. To minimize selection bias, a 1:1 case-control matching was performed based on sex, age, body mass index (BMI), and the presence of osteoporosis. A total of 48 patients (24 in each group) were included. We compared perioperative data (operation time, hemoglobin change, transfusion rate), functional outcomes using the Koval score, and radiological outcomes, including union rate, femoral neck shortening, and complication rates.
-
Results
The mean operation time was significantly shorter in the FNS group than in the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). There were no statistically significant differences between the two groups in the union rate (87.5% in FNS vs. 95.8% in DHS), femoral neck shortening, final Koval score distribution, or overall complication rates (12.5% in both groups).
-
Conclusions
For treating stable femoral neck fractures in older adults, the FNS demonstrated comparable clinical and radiological outcomes to the DHS, with the distinct advantage of a shorter operation time. While these findings suggest that the FNS is a promising and safe alternative that may reduce the surgical burden, definitive conclusions are precluded by the small sample size, warranting further research to corroborate these results.
-
Level of evidence
IV.
-
Keywords: Femoral neck fractures, Femoral neck, Bone screws, Internal fracture fixation, Aged
Introduction
Background
With the global trend of an aging society, the incidence of osteoporotic hip fractures, particularly femoral neck fractures, continues to rise steadily [
1]. A femoral neck fracture is considered a severe injury associated with high morbidity and mortality, as it not only causes extreme pain and immediate loss of ambulation, rendering patients unable to maintain an independent daily life, but also leads to fatal systemic complications such as pressure sores, pneumonia, and deep vein thrombosis due to prolonged bed rest. Therefore, a core principle of modern orthopedic treatment is to perform prompt and stable surgical fixation, taking into account the patient's overall medical condition, in order to prevent the vicious cycle of complications and facilitate early functional recovery.
The treatment strategy for femoral neck fractures is determined based on multiple factors, including the patient's age, preinjury activity level, and the degree of fracture displacement and stability, with options ranging from internal fixation to arthroplasty. Among these, internal fixation, or osteosynthesis, is preferentially considered for relatively young or active patients, as well as for non-displaced or stable fractures, as it allows for the preservation of the native joint, thereby maintaining proprioception and physiological function. To date, multiple cannulated screws (CCS) and the dynamic hip screw (DHS) have been widely used as standard methods for the internal fixation of stable femoral neck fractures. The DHS, in particular, is a proven treatment that can provide strong dynamic compression at the fracture site, and its reliability in achieving high union rates in the elderly population with stable fractures has been well-documented, establishing it as a benchmark for osteosynthesis [
2]. However, the DHS has the distinct disadvantage of requiring a relatively large skin incision and extensive soft-tissue dissection, which can increase intraoperative blood loss and consequently impose a significant surgical burden on elderly patients with multiple medical comorbidities [
3,
4].
To overcome these shortcomings and maximize the benefits of minimally invasive surgery, the femoral neck system (FNS; DePuy Synthes) was recently developed. The FNS is a fixation device that combines a locking compression bolt with an angularly stable locking plate, designed to provide excellent rotational and angular stability despite using a single bolt [
5]. This structural feature allows for surgery through a significantly smaller incision compared to the DHS, which is expected to offer the biological advantage of preserving the soft tissues and blood supply to the femoral head. Numerous biomechanical studies have demonstrated that the FNS provides mechanical stability comparable to or superior to existing fixation devices [
6-
8]. Initial clinical studies have reported that the FNS is associated with shorter operation times and less blood loss, while achieving satisfactory union rates [
5,
9,
10].
However, most of the existing research has focused on comparing the FNS with CCS [
11-
13], and there is still a lack of studies directly comparing the clinical outcomes of the FNS with those of the DHS, the traditional gold standard, in elderly patients with osteoporotic fractures [
3,
4].
This study aimed to directly compare the perioperative data, as well as the clinical and radiological outcomes, of internal fixation using the FNS versus the DHS in elderly patients with stable femoral neck fractures, and thereby to investigate the clinical utility and safety of the FNS in a real-world clinical setting.
Methods
Ethics statement
The study’s protocol was reviewed and approved by the Institutional Review Board (IRB) of Keimyung University Dongsan Hospital (IRB No. 2025-08-001), and informed consent was waived due to the study's retrospective nature.
Study design
It is a retrospective cohort study, employing a case-control matching design to compare outcomes of two surgical methods. It was described according to the STROBE statement (
https://www.strobe-statement.org/).
This study was conducted at Keimyung University Dongsan Hospital. The study period extended from January 2010 to December 2022, during which all eligible consecutive patients with stable femoral neck fractures were treated according to institutional protocols. All surgical procedures were performed by a single, experienced orthopedic surgeon with a consistent technique. Patients were positioned supine on a fracture table, and closed reduction of the fracture was performed under C-arm fluoroscopic guidance. For the FNS group, an approximately 3–4 cm skin incision was made over the lateral aspect of the greater trochanter, and the FNS was inserted according to the manufacturer's guidelines. For the DHS group, a standard lateral approach was used with an approximately 8–10 cm incision to insert the DHS. A 1-hole side plate was used for all patients in the FNS group. In the DHS group, a 2-hole plate was utilized in 21 cases and a 3-hole plate in three cases. Furthermore, an additional anti-rotation screw was employed in eight cases within the DHS group to augment rotational stability. Efforts were made to achieve an ideal implant position in the center of the femoral head on both anteroposterior and lateral views. However, in some cases, a slightly inferior position of the bolt in the anteroposterior view was unavoidable due to individual variations in fracture patterns or femoral neck anatomy. According to the manufacturer's guidelines, the tip of the screw or bolt was intended to be positioned within 5–10 mm of the subchondral bone. Postoperatively, all patients received prophylactic antibiotics for 48 hours. Mechanical and pharmacological prophylaxis, including low-molecular-weight heparin and intermittent pneumatic compression devices, was implemented to prevent deep vein thrombosis. A standardized rehabilitation protocol was applied to all patients in both the FNS and DHS groups. The protocol was uniformly structured to promote early mobilization as follows: sitting as tolerated from the day of surgery to mitigate the risks of pulmonary complications. This was followed by mobilization to a wheelchair on postoperative days 1 to 2. Subsequently, the initiation of tolerable standing and toe-touch weight-bearing with a walker was permitted from postoperative day 3 for all patients. Demographic, clinical, and radiological data were collected through a review of electronic medical records and the picture archiving and communication system.
Participants
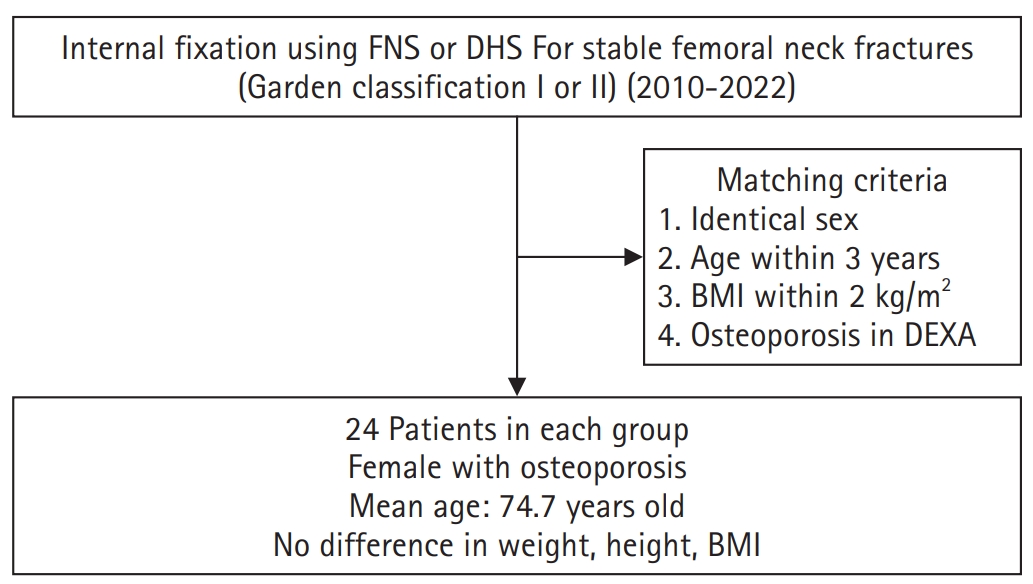
This study included patients aged 65 years or older who were diagnosed with a stable femoral neck fracture and underwent internal fixation with either the FNS or the DHS.
A stable fracture was defined as a Garden type I or II. To ensure comparability between the groups and to minimize selection bias, a 1:1 case-control study design was employed. Patients in the FNS group were matched with patients in the DHS group based on sex, age (within ±3 years), body mass index (BMI; within ±2 kg/m²), and the presence of osteoporosis, as confirmed by a dual-energy X-ray absorptiometry (DEXA) scan (
Fig. 1). Ultimately, a total of 48 patients, with 24 in each group, were included in this study. All patients included in the study were female. The mean age was 74.5 years (range, 66–85 years) in the FNS group and 75.0 years (range, 67–86 years) in the DHS group. The mean BMI was 21.7 kg/m² and 22.4 kg/m², respectively, and the mean T-score on DEXA scan was –3.5 and –3.4, respectively. No statistically significant differences were observed between the two groups in any of the demographic characteristics, including age, BMI, and bone mineral density (
Table 1).
Primary outcomes included radiographic union, femoral neck shortening, and complication rates (fixation failure, avascular necrosis [AVN], and nonunion). Secondary outcomes included perioperative variables (operation time, hemoglobin change, transfusion rate) and functional outcomes assessed with the Koval score.
Data sources/measurement
Clinical assessment
Perioperative variables included the total operation time (from anesthesia induction to skin closure), the change in hemoglobin level between preoperative and postoperative days 2 (
Table 1), and the incidence of allogenic blood transfusion during hospitalization (until postoperative days 3). Functional assessment was performed using the Koval score [
14] to evaluate ambulatory capacity before the injury and at the final follow-up. The Koval score ranges from 1 (independent ambulation) to 5 (bedridden), with higher scores indicating greater functional dependence.
Radiological assessment
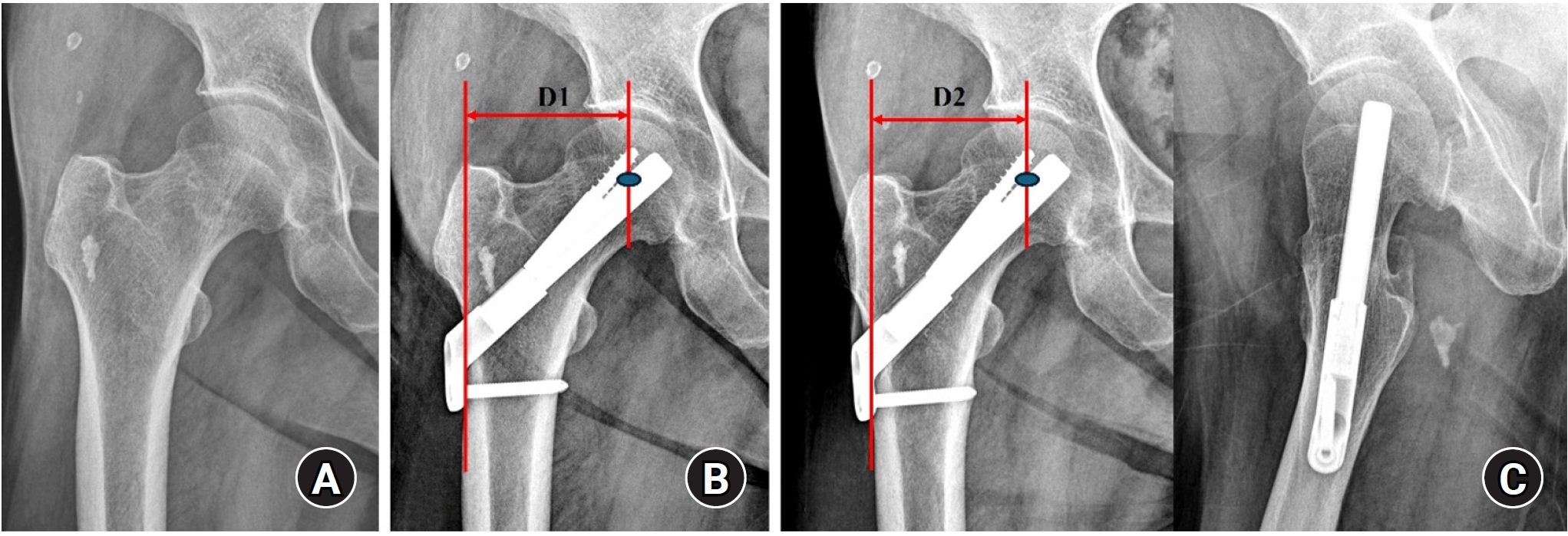
Standardized anteroposterior and lateral radiographs of the hip were obtained immediately postoperation and at each follow-up visit (6 weeks, 3 months, 6 months, 1 year, and annually thereafter). Radiological union was defined as the disappearance of the fracture line, accompanied by the absence of pain on full weight-bearing. Femoral neck shortening was calculated as the difference in the distance from the center of the femoral head to the lateral cortex of the femur between the immediate postoperative and final follow-up radiographs (
Fig. 2). Femoral neck shortening was measured independently by two experienced orthopedic surgeons, and the average of their values was used for the analysis. Complications, including fixation failure (e.g., screw cut-out or excessive sliding), AVN of the femoral head, nonunion, and the need for revision surgery, were investigated.
Measurement bias was reduced by independent, blinded radiographic assessments. All consecutive eligible patients with complete records were included to minimize attrition bias.
Study size
No sample size estimation was performed; all available matched cases during the study period were analyzed.
Statistical methods
All statistical analyses were performed using IBM SPSS ver. 26.0 (IBM Corp.). Continuous variables between the two groups were compared using the Mann-Whitney U test after assessing for normality. In contrast, categorical variables were analyzed using Fisher exact test or the linear-by-linear association test. The Wilcoxon signed-rank test was used to compare preinjury and final follow-up Koval scores. A P-value of less than 0.05 was considered statistically significant for all analyses.
Results
Clinical outcomes
The mean operation time was significantly shorter in the FNS group, at 60.9 minutes, compared to 70.8 minutes in the DHS group (P=0.007). The postoperative decrease in hemoglobin levels (1.0 g/dL in the FNS group vs. 1.2 g/dL in the DHS group; P=0.311) and the transfusion rate (16.7% [4/24] in the FNS group vs. 25.0% [6/24] in the DHS group; P=0.477) showed a tendency to be lower in the FNS group. However, this difference did not reach statistical significance.
There was no difference in the preinjury Koval scores between the two groups. At the final follow-up, the Koval scores in both groups showed a significant decline in function compared to their preinjury status (P<0.001). However, there was no statistically significant difference in the distribution of final follow-up Koval scores between the two groups (P=0.071) (
Table 2).
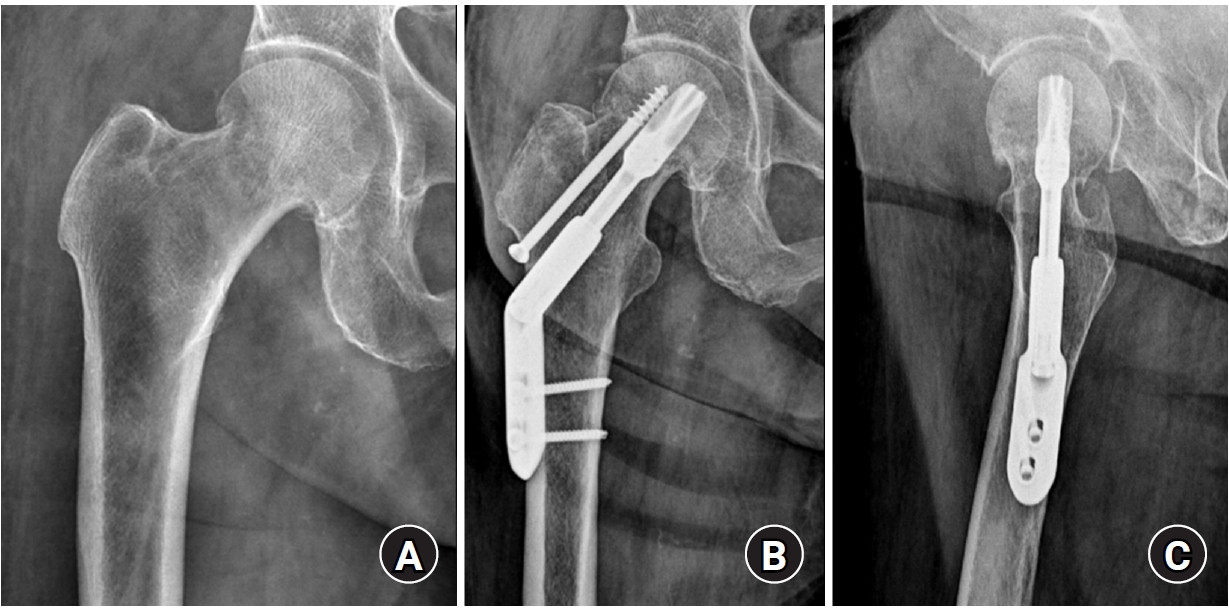
At the final follow-up, the union rate was 87.5% (21/24) in the FNS group and 95.8% (23/24) in the DHS group, with no statistically significant difference between the two groups (P=0.296) (
Figs. 2,
3). The mean femoral neck shortening was measured at 6.1 mm in the FNS group and 5.9 mm in the DHS group, and no significant difference was observed (P=0.427).
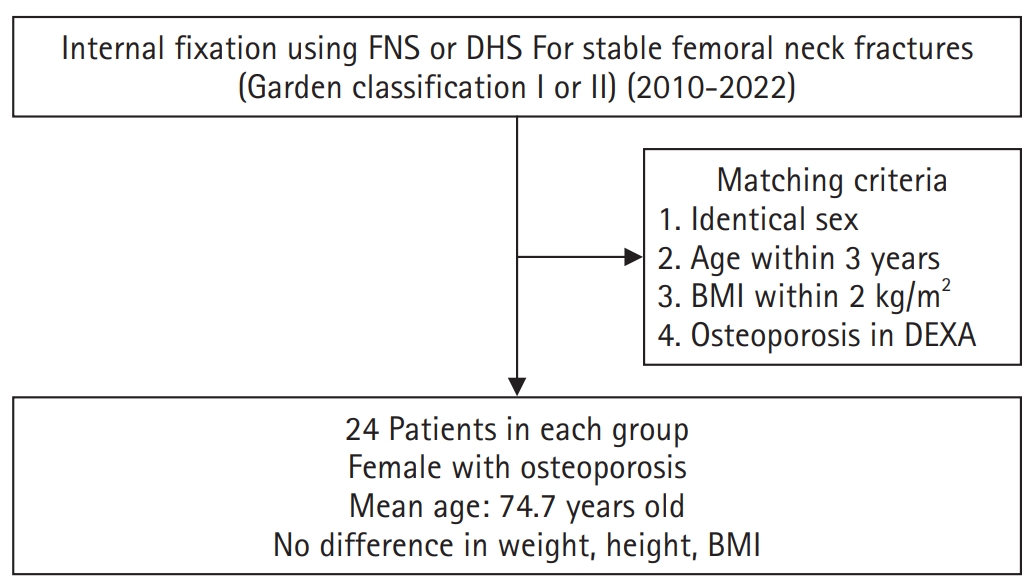
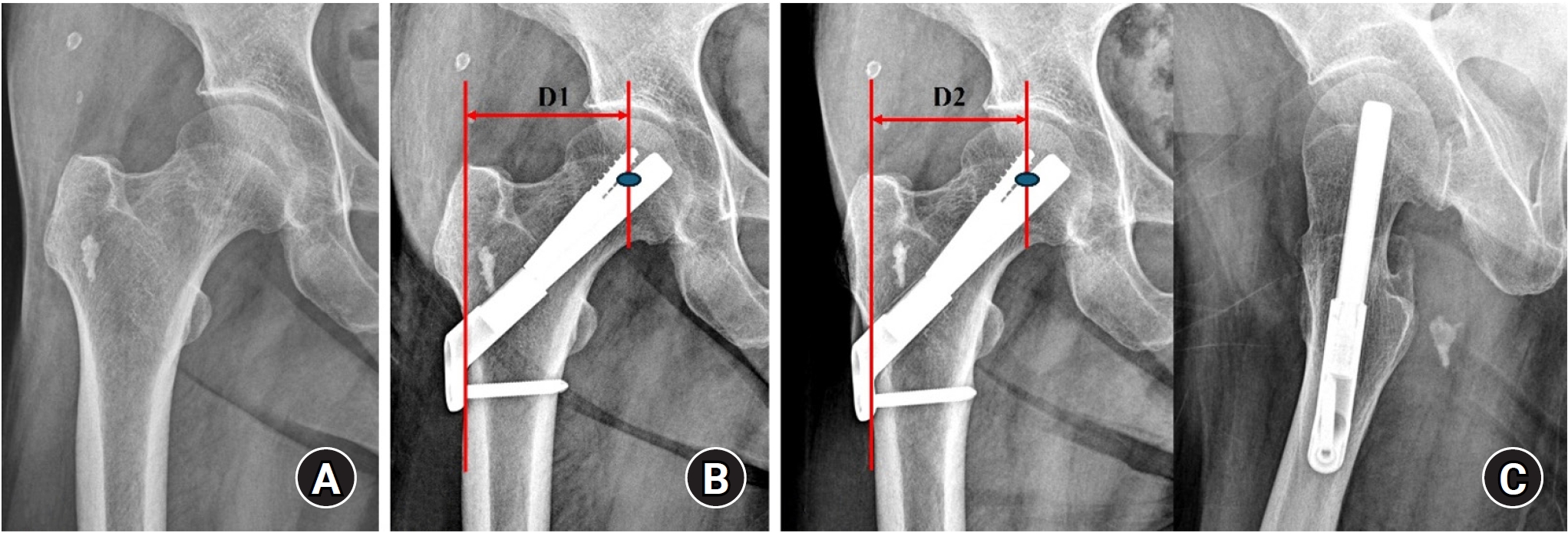
Complications occurred in a total of three cases (12.5%) in the FNS group, which included two cases of fixation failure and one case of AVN. In the DHS group, complications also occurred in three cases (12.5%), consisting of one case of nonunion and two cases of AVN. There was no significant difference in the overall complication rate between the two groups (P=1.000). All patients who experienced complications (six patients) required conversion to arthroplasty (
Table 3,
Fig. 4).
Discussion
Key results
The principal finding of this investigation was a statistically significant reduction in mean operative duration of approximately 10 minutes in the FNS group compared to the DHS group (60.9 minutes vs. 70.8 minutes; P=0.007). This result provides objective evidence of the minimally invasive advantage of the FNS and is congruent with the findings of several antecedent studies.
Interpretation/comparison with previous studies
Niemann et al. [
3] reported that the FNS significantly reduced not only the operation time but also the fluoroscopy time compared to the DHS. Similarly, a study by Zheng et al. [
4] identified that the FNS had the shortest operative duration when compared to both DHS and CCS. For elderly patients, particularly those burdened by multiple medical comorbidities, a reduction in operative duration has significant clinical implications that extend beyond mere surgical efficiency. It is directly correlated with reduced exposure to anesthetic agents, diminished potential for intraoperative hemorrhage, and a lower risk of surgical site infection secondary to abbreviated exposure of the surgical field to the external environment, all of which may positively influence the patient's systemic physiological condition [
15]. In the current study, although not reaching statistical significance, a trend toward a more minor postoperative hemoglobin decrement and a lower transfusion rate was observed in the FNS group, a finding likely attributable to the smaller cutaneous incision and less extensive soft-tissue dissection required for the FNS procedure. It may, therefore, be posited that the FNS constitutes a valid therapeutic alternative capable of mitigating the physiological burden of surgery in this vulnerable patient demographic.
In this study, no significant differences were found between the two groups for most clinical and radiological outcomes, except for the operation time. The union rate, functional outcome at final follow-up (Koval score), and the degree of femoral neck shortening were all comparable. Although the union rate in the DHS group was slightly higher (95.8% vs. 87.5%), this difference was not statistically significant, which may be attributed to the limited sample size of our study. Nevertheless, both fixation methods demonstrated high rates of successful union, suggesting clinical comparability in this regard. This clinical equivalence is supported by experimental evidence demonstrating the sufficient biomechanical stability provided by the FNS. A biomechanical study by Moon et al. [
8] on a basicervical femoral neck fracture model, there were no statistically significant differences in axial stiffness and rotational stability between FNS and DHS. This implies that the combination of a locking compression bolt and an angularly stable plate in the FNS can maintain fracture stability as effectively as the lag screw and side plate construct of the DHS. It is therefore conceivable that, in stable fractures, the combination of 'adequate stability' and the biological advantages of 'soft-tissue and blood-supply preservation' offered by FNS contributed to achieving clinical outcomes comparable to those provided by robust fixation with DHS.
The complication rate was also identical in both groups at 12.5%, which is within an acceptable range compared to other large-scale studies. Davidson et al. [
10] reported a reoperation rate of 15.7% in their analysis of 102 FNS patients, and Stassen et al. [
5] reported a mechanical failure rate of 9.3% in a one-year follow-up study. The two cases of fixation failure in our FNS group may be related to the poor bone quality of the osteoporotic elderly patients or surgical technique, rather than to an inherent problem with the implant itself. Several biomechanical studies have emphasized that the stability of the FNS is highly dependent on the precise central placement of the implant within the femoral neck [
7,
16]. Especially in elderly patients with low bone mineral density, accurate implant positioning is crucial to prevent fixation failure, particularly the 'cut-out' phenomenon. Furthermore, Cha et al. [
17] have pointed out that the 5-mm increments in the FNS bolt length can make fine adjustments of the insertion depth difficult and have proposed a surgical technique to compensate for this. Therefore, a thorough understanding of and attention to these technical aspects are required to achieve successful clinical outcomes with the FNS.
Femoral neck shortening is a primary concern after internal fixation, as it can lead to limb length discrepancy, abductor muscle weakness, and an abnormal gait, ultimately resulting in functional impairment. In our study, the mean femoral neck shortening was minimal and did not differ significantly between the two groups (6.1 mm in the FNS group vs. 5.9 mm in the DHS group). While this suggests both implants effectively control for excessive collapse, it is important to note that even minor shortening can have clinical implications for abductor function and gait. The lack of a statistically significant difference in our cohort should be interpreted with caution, and larger studies are needed to definitively compare the two implants in their ability to prevent clinically relevant shortening. While some studies have reported that FNS is more effective than CCS in preventing femoral neck shortening [
11,
12], the results tend to be similar when compared with DHS, as observed in our study. This may be because both devices operate on a similar mechanism that allows for dynamic compression at the fracture site while controlling for excessive vertical displacement.
First, due to its retrospective design, there is a potential for selection bias. Although we attempted to minimize this by employing a case-control matching design to ensure similar demographic characteristics between the groups, the fundamental limitation of non-randomization and the potential for unmeasured confounding variables remain. Second, the study was conducted at a single institution with a relatively small number of patients. This limited sample size inherently restricts the statistical power of our analyses, making it difficult to detect subtle but potentially clinically meaningful differences between the groups. Consequently, outcomes that did not reach statistical significance, such as the trends observed in union rates and transfusion rates, should be interpreted with caution as they may be susceptible to a type II error. Additionally, the small sample size precluded a sub-group analysis based on the radiographic position of the implant. While the surgical goal was optional center-center placement, minor variations (some inferior placement on anteroposterior position view) due to fracture patterns or patient anatomy were unavoidable. The potential influences of these deviations on fixation stability and clinical results could not be statistically assessed and therefore represent another limitation of our study. Third, the follow-up period was relatively short and different between the two groups, which is insufficient to fully assess long-term complications such as AVN or posttraumatic arthritis. Fourth, our analysis of blood-related outcomes did not account for potential confounding variables such as the time from injury to admission and the time from admission to surgery. These intervals could have influenced preoperative hemoglobin levels and transfusion requirements, potentially confounding the interpretation of perioperative blood loss. While we attempted to standardize our analysis by measuring the change from the immediate preoperative hemoglobin level, the lack of data on these time intervals is a limitation that should be considered when interpreting the results related to hemoglobin drop and transfusion rates. Nevertheless, this study holds academic significance as one of the few studies to directly compare FNS and DHS in a real-world clinical setting for elderly patients with osteoporotic, stable femoral neck fractures.
Conclusions
In conclusion, for the treatment of stable femoral neck fractures in the elderly, internal fixation with FNS provides comparable rates of union, functional recovery, and complications when compared to the traditional DHS, while offering the distinct advantage of a significantly shorter operation time. Therefore, FNS appears to be a promising clinical alternative that is both effective and safe, capable of achieving stable fixation while reducing the surgical burden on the patient. However, given the study's limitations, particularly the sample size, these findings should be considered preliminary. Future large-scale, prospective, randomized controlled trials are warranted to corroborate these findings and provide more definitive conclusions.
Article Information
-
Author contribution
Conceptualization: BWM, KJL. Data curation: BCC, BWM, KJL. Formal analysis: BCC, BWM. Software: BCC, BWM. Investigation: KJL. Methodology: KJL. Supervision: KJL. Validation: BCC, BWM, JSH. Visualization, JSH. Writing-original draft: KJL, JSH. Writing-review & editing: BCC, BWM, KJL. All authors read and approved the final manuscript.
-
Conflict of interests
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Data availability
Contact the corresponding author for data availability.
-
Acknowledgments
None.
-
Supplementary materials
None.
Fig. 1.A flow chart of patient selection. FNS, femoral neck system; DHS, dynamic hip screw; BMI, body mass index; DEXA, dual-energy X-ray absorptiometry.
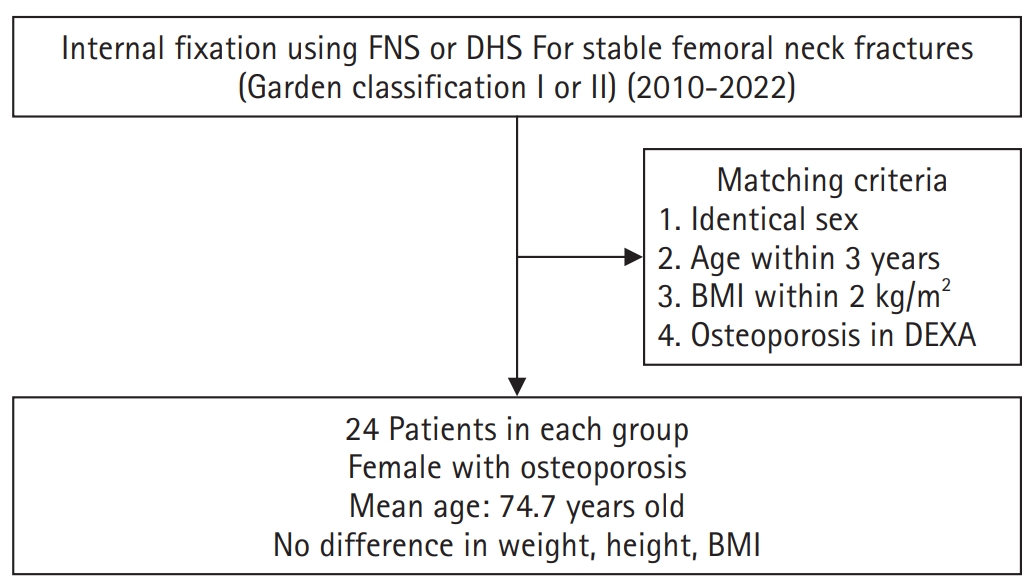
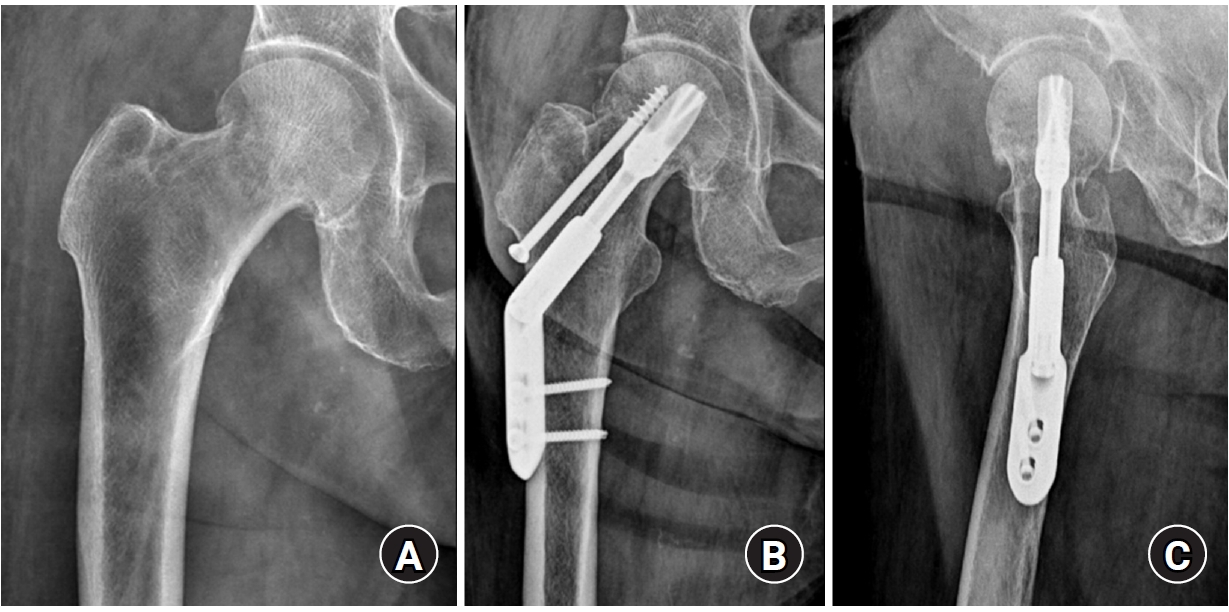
Fig. 2.(A, B) A 67-year-old female patient with a right femoral neck fracture (Garden type 1) treated with the femoral neck system. (C) The postoperative 4-year radiograph shows a well-healed fracture site and no complications related to the implant. Femoral neck shortening (D2‒D1) was calculated as the difference in the distance from the center of the femoral head to the lateral cortex of the femur between the immediate postoperative and final follow-up radiographs.
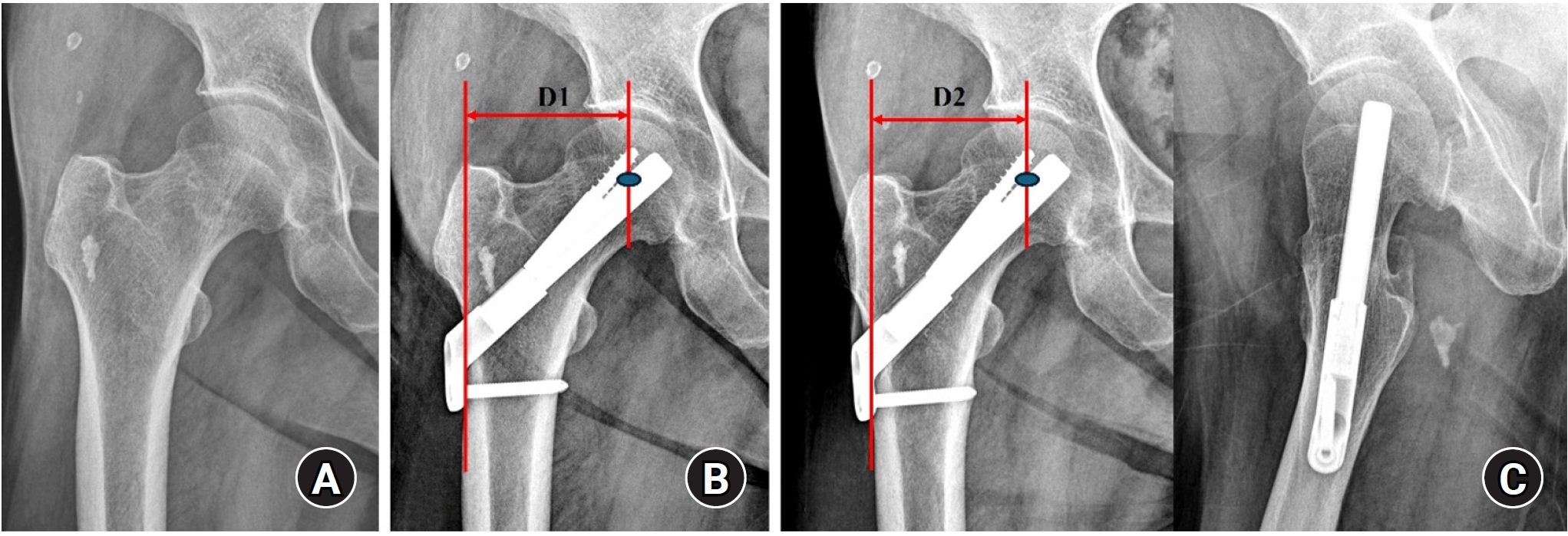
Fig. 3.(A, B) An 86-year-old female patient with a stable right femoral neck fracture treated with a dynamic hip system. (C) Postoperative 1-year anteroposterior and axial radiographs show a well-healed fracture site and no complications related to the implant.
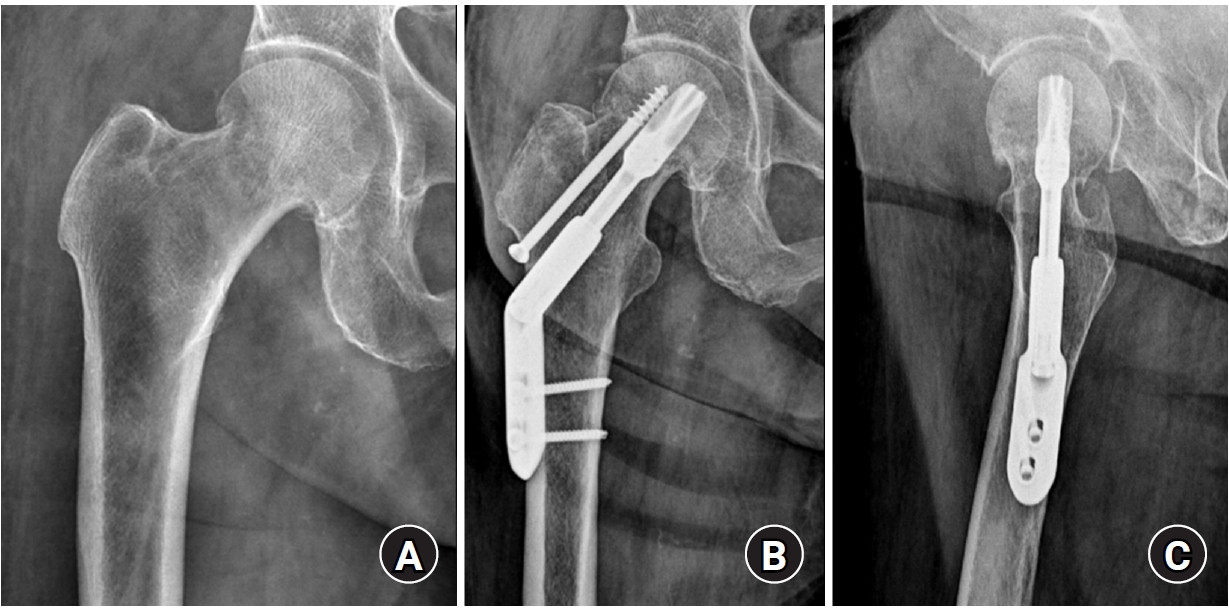
Fig. 4.(A) A 64-year-old female patient sustained a stable femoral neck fracture on the left side. (B) The fracture was treated with the femoral neck system (FNS; anteroposterior and axial view). (C) A postoperative 6-month radiograph shows fixation failure of the FNS.

Table 1.Demographics of the two groups
|
Variable |
FNS group (n=24) |
DHS group (n=24) |
P-value |
|
Sex (male:female) |
0:24 |
0:24 |
1.000 |
|
Mean age (yr) |
74.5 |
75.0 |
0.673 |
|
Average body mass index (kg/m²) |
21.7 |
22.4 |
0.336 |
|
Average preoperative hemoglobin level (g/dL) |
11.7 |
11.2 |
0.302 |
|
Average postoperative days 2 hemoglobin level (g/dL) |
11.1 |
10.6 |
0.243 |
|
Average T-score on DEXA (femoral neck area) |
‒3.5 |
‒3.4 |
0.573 |
|
Fracture classification (Garden classification I:II) |
2:22 |
4:20 |
0.388 |
|
Average follow-up interval (mo) |
14.9 |
30.9 |
0.003 |
Table 2.Clinical results of the two groups
|
Variable |
FNS group (n=24) |
DHS group (n=24) |
P-value |
|
Preinjury Koval scorea) (1/2/3/4/5 grade) |
12/8/3/1/0 |
12/8/3/1/0 |
1.000 |
|
Final follow-up Koval scorea) (1/2/3/4/5 grade) |
6/5/2/10/1 |
6/12/2/4/0 |
0.071 |
|
Average hemoglobin drop (between preoperative and postoperative days 2; g/dL) |
1.0 |
1.2 |
0.311 |
|
Transfusion rate (until postoperative days 3) |
4/24 |
6/24 |
0.477 |
|
Mean operation time (min) |
60.9 |
70.8 |
0.007 |
Table 3.Radiologic results of the two groups
|
Variable |
FNS group (n=24) |
DHS group (n=24) |
P-value |
|
Union rate (%) |
21 (87.5) |
23 (95.8) |
0.296 |
|
Femoral neck shortening (mm) |
6.1 |
5.9 |
0.427 |
|
Complication |
|
|
1.000 |
|
Fixation failure |
2 |
0 |
|
|
Avascular necrosis |
1 |
2 |
|
|
Nonunion |
0 |
1 |
|
References
- 1. Kanis JA, Oden A, McCloskey EV, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 2012;23:2239-56.ArticlePubMedPMCPDF
- 2. Min BW, Lee KJ, Bae KC, Lee SW, Lee SJ, Choi JH. Result of internal fixation for stable femoral neck fractures in elderly patients. Hip Pelvis 2016;28:43-8.ArticlePubMedPMCPDF
- 3. Niemann M, Braun KF, Ahmad SS, Stockle U, Mardian S, Graef F. Comparing perioperative outcome measures of the dynamic hip screw and the femoral neck system. Medicina (Kaunas) 2022;58:352.ArticlePubMedPMC
- 4. Zheng Z, Lim C, Tan CMP, et al. Femoral neck system as a safe alternative to cannulated compression screw and dynamic hip screw in femoral neck fractures: an early comparative study. Singapore Med J 2024;Jan. 8. [Epub]. https://10.4103/singaporemedj.SMJ-2022-024.
- 5. Stassen RC, Jeuken RM, Boonen B, Meesters B, de Loos ER, van Vugt R. First clinical results of 1-year follow-up of the femoral neck system for internal fixation of femoral neck fractures. Arch Orthop Trauma Surg 2022;142:3755-63.ArticlePubMedPDF
- 6. Teng Y, Zhang Y, Guo C. Finite element analysis of femoral neck system in the treatment of Pauwels type III femoral neck fracture. Medicine (Baltimore) 2020;99:e23120. ArticlePubMedPMC
- 7. Nan C, Ma L, Liang Y, Li Y, Ma Z. Mechanical effects of sagittal variations on Pauwels type III femoral neck fractures treated with Femoral Neck System (FNS). BMC Musculoskelet Disord 2022;23:1045.ArticlePubMedPMCPDF
- 8. Moon JK, Lee JI, Hwang KT, Yang JH, Park YS, Park KC. Biomechanical comparison of the femoral neck system and the dynamic hip screw in basicervical femoral neck fractures. Sci Rep 2022;12:7915.ArticlePubMedPMCPDF
- 9. Vazquez O, Gamulin A, Hannouche D, Belaieff W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): short-term clinical and radiological outcomes. J Orthop Surg Res 2021;16:477.ArticlePubMedPMCPDF
- 10. Davidson A, Blum S, Harats E, et al. Neck of femur fractures treated with the femoral neck system: outcomes of one hundred and two patients and literature review. Int Orthop 2022;46:2105-15.ArticlePubMedPMCPDF
- 11. Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res 2021;16:504.ArticlePubMedPMCPDF
- 12. Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res 2021;16:370.ArticlePubMedPMCPDF
- 13. He C, Lu Y, Wang Q, et al. Comparison of the clinical efficacy of a femoral neck system versus cannulated screws in the treatment of femoral neck fracture in young adults. BMC Musculoskelet Disord 2021;22:994.ArticlePubMedPMCPDF
- 14. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture: a retrospective study in geriatric patients. Clin Orthop Relat Res 1995;(310):150-9.PubMed
- 15. Cheng H, Clymer JW, Po-Han Chen B, et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res 2018;229:134-44.Article
- 16. Jung CH, Cha YH, Yoon HS, et al. Mechanical effects of surgical variations in the femoral neck system on Pauwels type III femoral neck fracture: a finite element analysis. Bone Joint Res 2022;11:102-11.PubMed
- 17. Cha Y, Song JU, Yoo JI, et al. Improved control over implant anchorage under the use of the femoral neck system for fixation of femoral neck fractures: a technical note. BMC Musculoskelet Disord 2021;22:621.ArticlePubMedPMCPDF
 , Byung-Woo Min
, Byung-Woo Min , Kyung-Jae Lee
, Kyung-Jae Lee , Jun-Sik Hong
, Jun-Sik Hong




 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

