Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 27(1); 2014 > Article
-
Original Article
- Treatment of Periprosthetic Femoral Fractures Following Total Knee Arthroplasty
- Lih Wang, M.D., Kyu Yeol Lee, M.D., Chul Hong Kim, M.D., Myung Jin Lee, M.D., Min Soo Kang, M.D., Jin Soo Hwang, M.D., Sun Hyo Kim, M.D.
-
Journal of the Korean Fracture Society 2014;27(1):42-49.
DOI: https://doi.org/10.12671/jkfs.2014.27.1.42
Published online: January 17, 2014
Department of Orthopaedic Surgery, College of Medicine, Dong-A University, Busan, Korea.
*Department of Orthopaedic Surgery, Dong-Eui Medical Center, Busan, Korea.
- Address reprint requests to: Lih Wang, M.D. Department of Orthopaedic Surgery, Dong-A University Medical Center, 26 Daesingongwon-ro, Seo-gu, Busan 602-715, Korea. Tel: 82-51-240-2593, Fax: 82-51-254-6757, libi33@dau.ac.kr
Copyright © 2014 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 532 Views
- 2 Download
- 1 Crossref
Abstract
-
Purpose
- The purpose of this study is to compare the treatment results of fracture fixations by using two minimal invasive techniques for patients with periprosthetic femoral fractures following total knee arthroplasty.
-
Materials and Methods
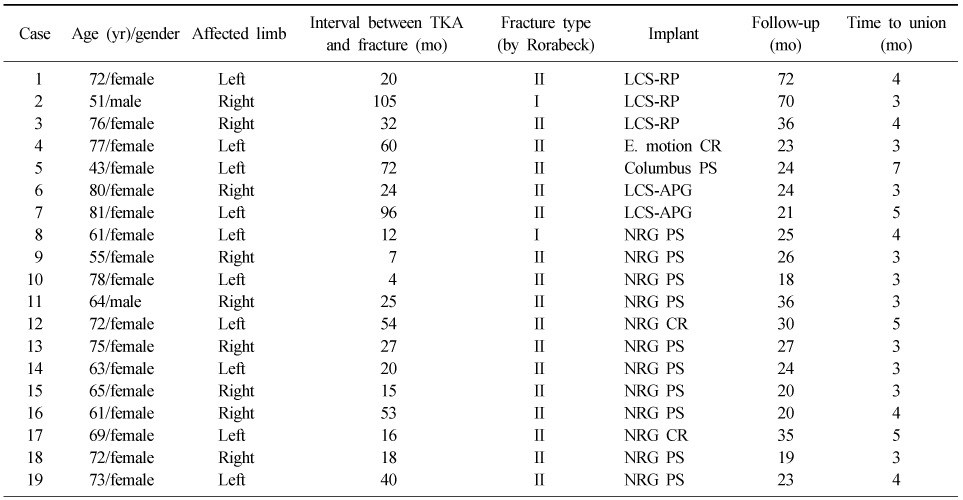
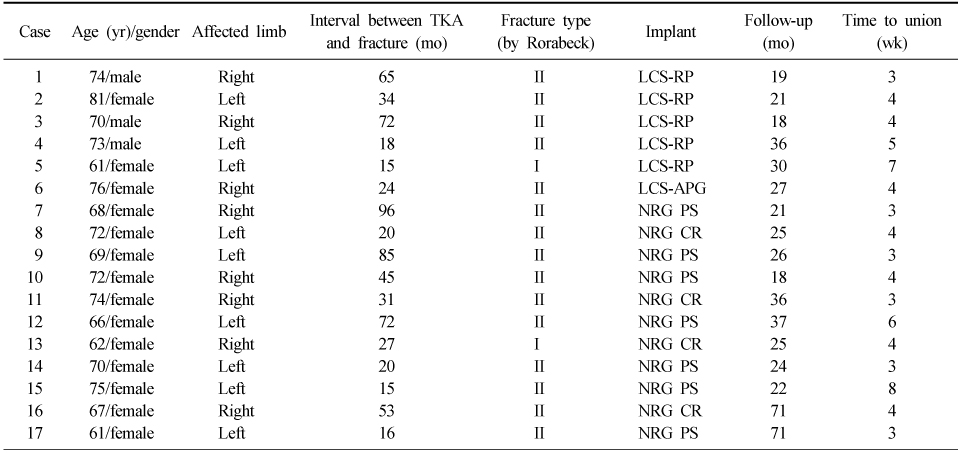
- We reviewed 36 patients (5 males, 31 females) of periprosthetic femoral fractures whom were treated surgically between January 2005 and January 2011. Mean patient age was 68.9 years (range, 43 to 81 years) old and the follow-up period averaged 41 months (range, 18 to 72 months). Nineteen patients were treated with minimal invasive locking plate fixations (group I) and 17 patients with retrograde intramedullary nailing (group II). Clinical and radiological outcomes in each group were comparatively analyzed.
-
Results
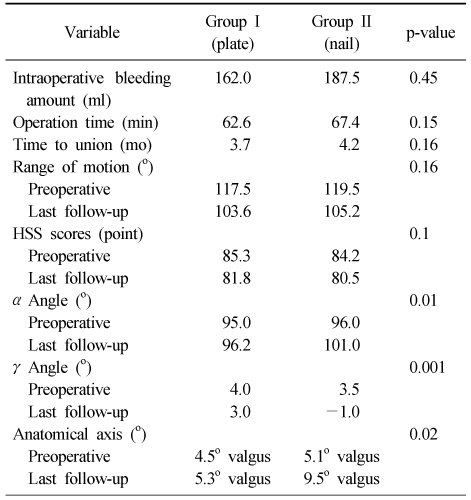
- Successful bone unions occurred in all patients and the mean time to bone union was 3.7 months in group I and 4.2 months in group II. There were no statistical differences between the two groups according to mean operative time and mean intraoperative blood loss. There were also no statistical differences between two groups according to clinical outcomes but the valgus deformity was apparent in group II and radiological outcomes revealed significant differences between the two groups.
-
Conclusion
- For the treatment of periprosthetic femoral fractures after total knee arthroplasty, two minimal invasive techniques have shown good clinical results. However, the minimal invasive plate fixation showed better results in the radiological alignments.
- 1. Bolhofner BR, Carmen B, Clifford P. The results of open reduction and internal fixation of distal femur fractures using a biologic (indirect) reduction technique. J Orthop Trauma, 1996;10:372-377.Article
- 2. Bong MR, Egol KA, Koval KJ, et al. Comparison of the LISS and a retrograde-inserted supracondylar intramedullary nail for fixation of a periprosthetic distal femur fracture proximal to a total knee arthroplasty. J Arthroplasty, 2002;17:876-881.Article
- 3. Bonutti PM, Dethmers D, Ulrich SD, Seyler TM, Mont MA. Computer navigation-assisted versus minimally invasive TKA: benefits and drawbacks. Clin Orthop Relat Res, 2008;466:2756-2762.
- 4. Cain PR, Rubash HE, Wissinger HA, McClain EJ. Periprosthetic femoral fractures following total knee arthroplasty. Clin Orthop Relat Res, 1986;(208):205-214.Article
- 5. Chmell MJ, Moran MC, Scott RD. Periarticular fractures after total knee arthroplasty: principles of management. J Am Acad Orthop Surg, 1996;4:109-116.Article
- 6. DiGioia AM 3rd, Rubash HE. Periprosthetic fractures of the femur after total knee arthroplasty. A literature review and treatment algorithm. Clin Orthop Relat Res, 1991;(271):135-142.
- 7. Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma, 1999;13:401-406.Article
- 8. Hayakawa K, Nakagawa K, Ando K, Ohashi H. Ender nailing for supracondylar fracture of the femur after total knee arthroplasty: five case reports. J Arthroplasty, 2003;18:946-952.
- 9. Herrera DA, Kregor PJ, Cole PA, Levy BA, Jönsson A, Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981-2006). Acta Orthop, 2008;79:22-27.Article
- 10. Kolb W, Guhlmann H, Friedel R, Nestmann H. Fixation of periprosthetic femur fractures with the less invasive stabilization system (LISS)--a new minimally invasive treatment with locked fixed-angle screws. Zentralbl Chir, 2003;128:53-59.
- 11. Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury, 1997;28:Suppl 1. A20-A30.Article
- 12. McLaren AC, Dupont JA, Schroeber DC. Open reduction internal fixation of supracondylar fractures above total knee arthroplasties using the intramedullary supracondylar rod. Clin Orthop Relat Res, 1994;(302):194-198.Article
- 13. Ortiguera CJ, Berry DJ. Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am, 2002;84:532-540.Article
- 14. Ostrum RF, Geel C. Indirect reduction and internal fixation of supracondylar femur fractures without bone graft. J Orthop Trauma, 1995;9:278-284.Article
- 15. Ricci WM, Loftus T, Cox C, Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma, 2006;20:190-196.Article
- 16. Ritter MA, Faris PM, Keating EM. Anterior femoral notching and ipsilateral supracondylar femur fracture in total knee arthroplasty. J Arthroplasty, 1988;3:185-187.Article
- 17. Rolston LR, Christ DJ, Halpern A, O'Connor PL, Ryan TG, Uggen WM. Treatment of supracondylar fractures of the femur proximal to a total knee arthroplasty. A report of four cases. J Bone Joint Surg Am, 1995;77:924-931.Article
- 18. Rorabeck CH, Taylor JW. Periprosthetic fractures of the femur complicating total knee arthroplasty. Orthop Clin North Am, 1999;30:265-277.Article
- 19. Russell GV Jr, Smith DG. Minimally invasive treatment of distal femur fractures: report of a technique. J Trauma, 1999;47:799-801.Article
- 20. Scott RD. Anterior femoral notching and ipsilateral supracondylar femur fracture in total knee arthroplasty. J Arthroplasty, 1988;3:381.
- 21. Wenda K, Runkel M, Degreif J, Rudig L. Minimally invasive plate fixation in femoral shaft fractures. Injury, 1997;28:Suppl 1. A13-A19.Article
- 22. Zlowodzki M, Williamson S, Cole PA, Zardiackas LD, Kregor PJ. Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures. J Orthop Trauma, 2004;18:494-502.Article
REFERENCES
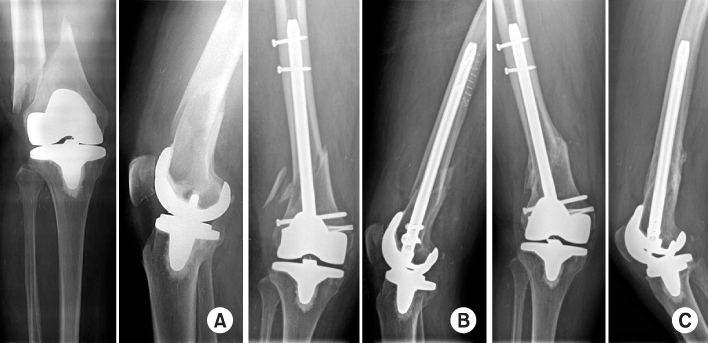

Figure & Data
REFERENCES
Citations

- The Result of Treatment of Femoral Periprosthetic Fractures after Total Knee Arthroplasty
Jun-Beom Kim, In-Soo Song, Dong-Hyuk Sun, Hyun Choi
Journal of the Korean Orthopaedic Association.2014; 49(6): 446. CrossRef
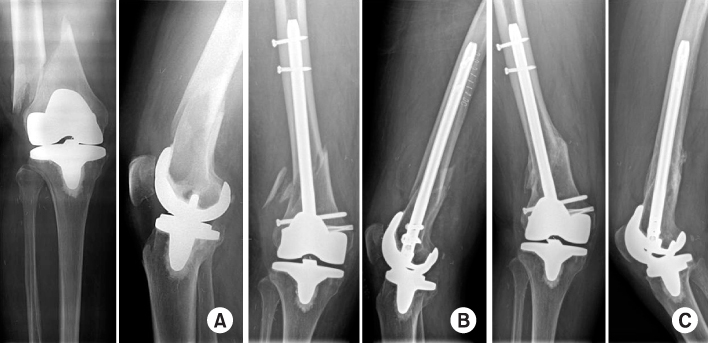
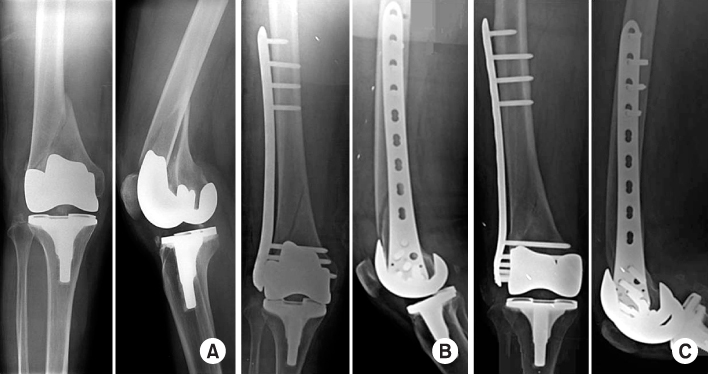
Fig. 1
Fig. 2
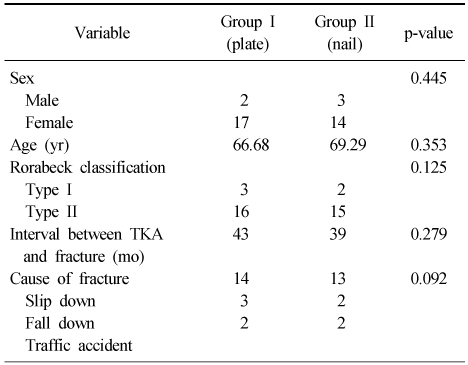
Comparison of Demographics in Group I and II
TKA: Total knee arthroplasty.
Demographics of Nineteen Patients with Periprosthetic Femoral Fractures in Group I
TKA: Total knee arthroplasty, CR: Cruciate retaining, PS: Posterior stabilized.
Demographics of Seventeen Patients with Periprosthetic Femoral Fractures in Group II
TKA: Total knee arthroplasty, CR: Cruciate retaining, PS: Posterior stabilized.
Comparison of Treatment Results in Group I and II
TKA: Total knee arthroplasty.
TKA: Total knee arthroplasty, CR: Cruciate retaining, PS: Posterior stabilized.
TKA: Total knee arthroplasty, CR: Cruciate retaining, PS: Posterior stabilized.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

