Current issue
- Page Path
- HOME > Browse articles > Current issue
Review Article
- Complications of hand fractures: strategies for prevention and management
- Jong Woo Kang
- J Musculoskelet Trauma 2026;39(1):1-11. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00304
-
 Abstract
Abstract
 PDF
PDF - Various complications can occur after hand fractures. Among them, joint stiffness and malunion are the most common and significant complications, which are often accompanied by tendon adhesions and joint contracture. Careful evaluations of injury characteristics, such as fracture patterns, alignment, and soft tissue injury, are the first step to select appropriate management strategies and prevent complications of hand fractures. Close observation of its clinical prognosis is also essential for early detection and preemptive management of complications. Management of complications includes immobilization, rehabilitation, and various surgical techniques such as tenolysis or capsular release for joint stiffness, corrective osteotomy for malunion, and revisional fixation with bone graft for nonunion. The authors discuss prevention, early recognition, and management strategies for complications of hand fractures in this review.
- 212 View
- 9 Download

Original Articles
- Epidemiological changes and surgical trends of distal radius fractures in adults over 50 years during the COVID-19 pandemic in Korea: a nationwide repeated cross-sectional study
- Han-Kook Yoon, So Ra Yoon, Kee-Bum Hong, Youngsu Jung, SeongJu Choi, Jun-Ku Lee
- J Musculoskelet Trauma 2026;39(1):12-19. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00297
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
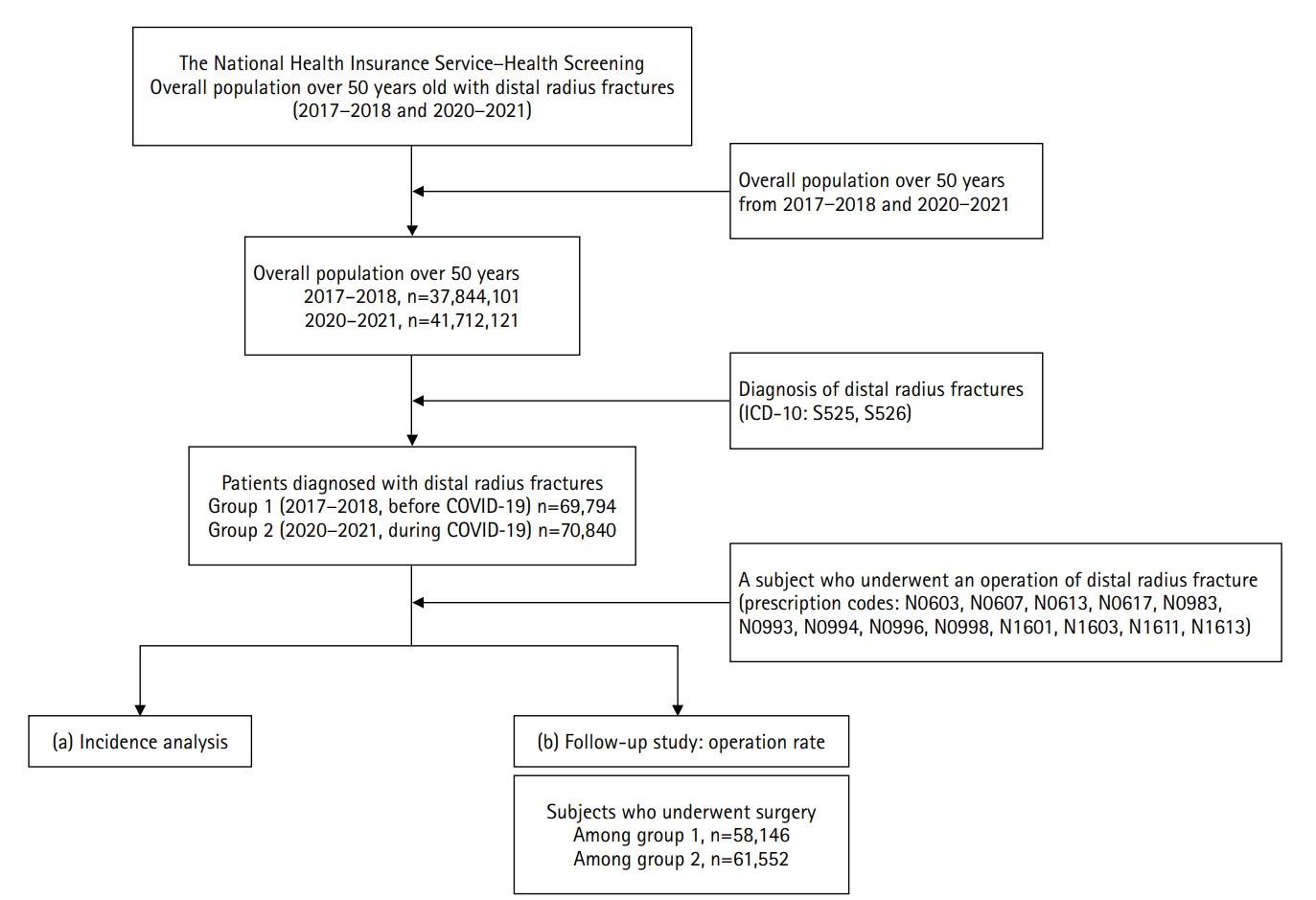
Supplementary Material - Background
The COVID-19 pandemic is likely to have affected bone health in older adults in Korea. This study aimed to analyze changes in the epidemiology and management of distal radius fractures (DRFs) in older adults before and during the COVID-19 pandemic.
Methods
Patients with DRF aged over 50 years in 2017, 2018, 2020, and 2021 were included in this study. Patients were classified into a group with DRF occurring between 2017 and 2018 (before COVID-19) and a group with DRF occurring between 2020 and 2021 (during COVID-19). We calculated the incidence rates of DRF and compared them between the two groups. We also analyzed and compared demographic data (age, sex, income, residence) and the operation rate for DRF between the two groups. Patient selection and treatment were based on International Classification of Diseases, 10th revision codes.
Results
A total of 140,634 patients with DRF (before COVID-19, 69,794; during COVID-19, 70,840) were included. The incidence of DRF before COVID-19 (184.4/100,000 person-years) was higher than during COVID-19 (169.8/100,000 person-years). The operation rate was higher during COVID-19 (86.9%) than before COVID-19 (83.3%).
Conclusion
During the COVID-19 pandemic, the incidence of DRF decreased in South Korea. However, the rate of surgical treatment increased and exceeded the global surgical rate. Level of evidence: III.
- 176 View
- 4 Download

- Association between decreased bone mineral density and Pauwels angle in femoral neck fractures: a cross-sectional study
- Soo-Hwan Jung, Yong-Uk Kwon, Ji-Hun Park
- J Musculoskelet Trauma 2026;39(1):20-29. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00269
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
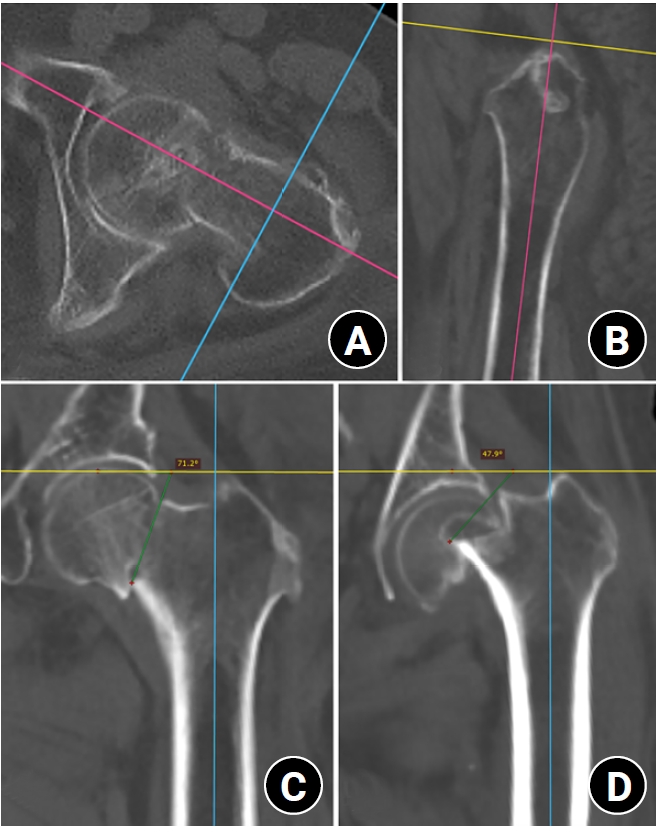
Supplementary Material - Background
Progressive osteoporosis reduces the trabecular structures of the proximal femur, whereas the primary compression trabeculae (PCTs) are relatively preserved. We hypothesize that the loss of the vertically oriented PCTs in osteoporosis, which act as a mechanical barrier, affects fracture line propagation and influences the Pauwels angle. This study investigated the association between bone mineral density (BMD) and Pauwels angles in low-energy femoral neck fractures (FNFs).
Methods
This cross-sectional study included 150 patients (mean age, 75.3 years; range, 50–94 years) diagnosed with intracapsular FNFs between May 2019 and May 2023. BMD was measured within 1 month of the injury date using dual-energy X-ray absorptiometry, and modified Pauwels angles were assessed using a computed tomography-based multiplanar reconstruction program. Multiple linear regression analysis was performed to evaluate the factors influencing the Pauwels angles. The dependent variable was the Pauwels angle, while the independent variables included sex, age, height, body weight, body mass index, American Society of Anesthesiologists score, Charlson comorbidity index score, smoking status, alcohol use, preinjury walking ability, and femoral neck BMD T-scores.
Results
Higher femoral neck BMD T-scores were significantly associated with increased Pauwels angles (β=3.449, P<0.001). Greater body weight was independently associated with increased Pauwels angles (β=0.213, P=0.007).
Conclusions
The Pauwels angle demonstrated a significant association with BMD, with lower BMD associated with less steep Pauwels angles. In the absence of BMD measurement, the Pauwels angle may indicate osteoporosis severity in patients with low-energy FNFs. Level of evidence: III.
- 115 View
- 3 Download

- Three-dimensional computed tomography-based differentiation of engaged versus displaced intertrochanteric fractures using the anterior fracture line: a cross-sectional study from Korea
- Jae-Suk Chang, Jin Yeob Park, Sang-Ok Chun, Chul-Ho Kim
- J Musculoskelet Trauma 2026;39(1):30-37. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00318
-
 Abstract
Abstract
 PDF
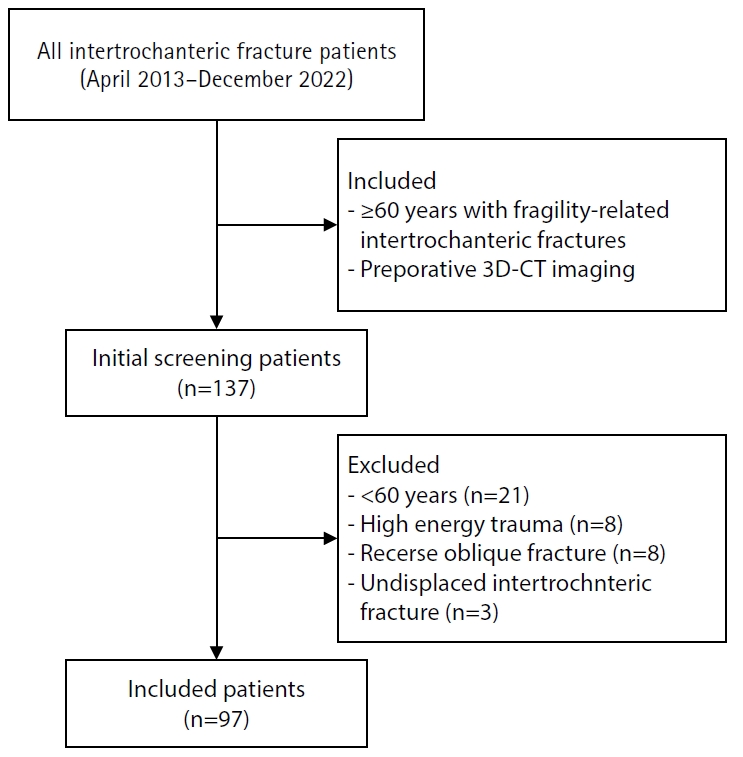
PDF - Background
With the advent of an aging society, osteoporotic fractures—particularly hip fractures—are increasing, with a 1-year mortality rate of 17%. Achieving stable fixation that enables early ambulation is essential but remains challenging because complex intertrochanteric (IT) fracture patterns are often underestimated on plain radiographs. Using three-dimensional computed tomography (3D-CT), this study analyzed whether the anterior fracture line lies medial or lateral to the IT line and examined its relationship with displacement or distal medullary canal engagement, highlighting the potential influence of the joint capsule and capsular ligaments on fracture morphology and fixation stability.
Methods
A retrospective review was conducted on 96 osteoporotic IT fractures in patients aged ≥60 years treated between April 2013 and December 2022 at National Police Hospital and Asan Medical Center, Seoul, Korea. Fractures were classified as engaged, completely displaced, and partially displaced based on 3D-CT findings. The anterior fracture-line position (medial or lateral to the IT line) and the status of the lesser trochanter (LT) were evaluated. The chi-square or Fisher exact test was used for statistical comparisons.
Results
In total, 96 patients were analyzed. Of these, 49 cases (51.0%) were classified as engaged type, 27 cases (28.1%) as completely displaced type, and 20 cases (20.8%) as partially displaced type. When comparing fracture pattern with anterior fracture-line position, the completely displaced type showed a significantly higher proportion of lateral anterior fracture lines than the other two types (P<0.001). However, no significant association was identified between fracture pattern and LT displacement. When the anterior fracture-line position and LT displacement were evaluated together, only the engaged type demonstrated a possible association between a lateral anterior fracture line and LT displacement, though the statistical significance was weak (P=0.047).
Conclusions
Fracture lines lateral to the IT line were strongly associated with displacement in IT fractures; however, their relationship with LT involvement, reflecting iliopsoas tendon traction, was not clearly demonstrated. Although the factors contributing to the engaged-type fracture remain uncertain, the statistical association between fracture pattern and anterior fracture-line position suggests that capsular structures may play a stabilizing role in select fracture configurations. Further studies are needed to clarify these anatomical interactions. Level of evidence:
- 117 View
- 4 Download

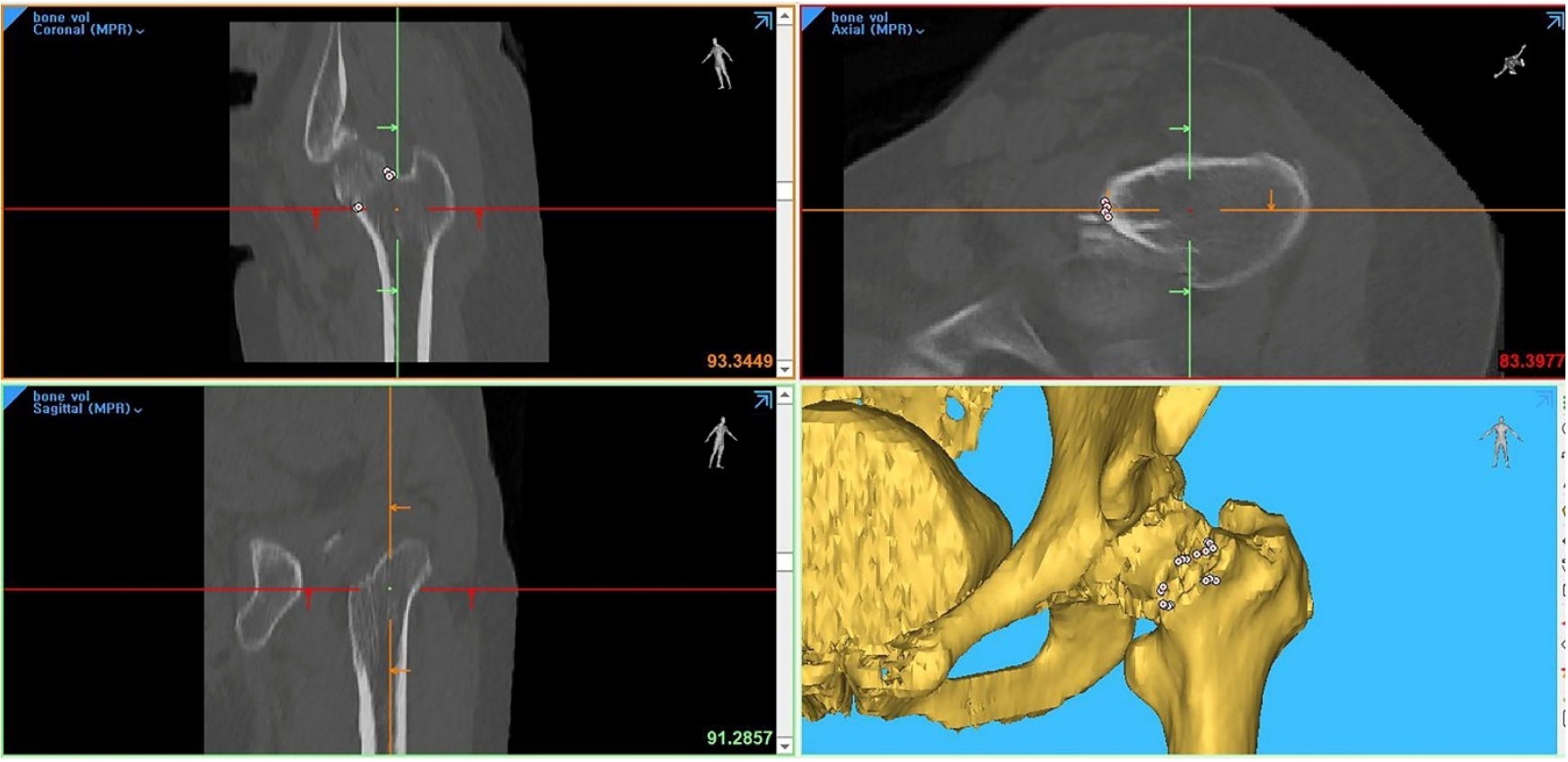
- Computed tomography plane reformatting to reduce projection error in measuring Pauwels angle of femoral neck fractures: a cross-sectional study
- Gyu Min Kong, Jae-Young Lim, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2026;39(1):38-47. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00038
-
 Abstract
Abstract
 PDF
PDF - Objectives
This study aimed to assess fracture verticality in both coronal and axial planes after eliminating projection error in femoral neck fractures among non-older adults, and to demonstrate its clinical utility using computed tomography (CT)-based modeling at actual size.
Methods
This retrospective observational study enrolled 57 patients (30 males and 27 females), aged 20–65 years, with displaced femoral neck fractures. Based on CT images, an actual-size fracture model was constructed. The CT scanning plane was reformatted with the neck-shaft fragment realigned vertically to the ground and parallel to the femoral neck axis. Three consecutive images were used to generate coronal reformats at the centerline and posterior border to measure central and posterior coronal plane verticality as Pauwels’ angle (PA). The central image of the reformatted axial plane was used to assess axial plane verticality. Differences in verticality were analyzed using analysis of variance.
Results
Three coronal morphology types were identified: linear (n=30), concave (n=25), and convex (n=2). Two axial morphology types were observed: cephalad (n=35) and trochanteric (n=22). The mean central PA, posterior PA, and axial verticality were 55.43°±13.79°, 51.44°±11.13°, and 85.74°±18.41°, respectively. Only the central PA showed a significant difference (P<0.001). The PA was significantly higher in the linear coronal type between images (P<0.05) and in the trochanteric axial type (P<0.05).
Conclusions
After reformatting the scanning plane, the central PA showed significant variation between images. Femoral neck fractures of the linear type in the coronal plane and the trochanteric type in the axial plane demonstrated greater verticality than other morphological types. Level of evidence:
- 117 View
- 4 Download

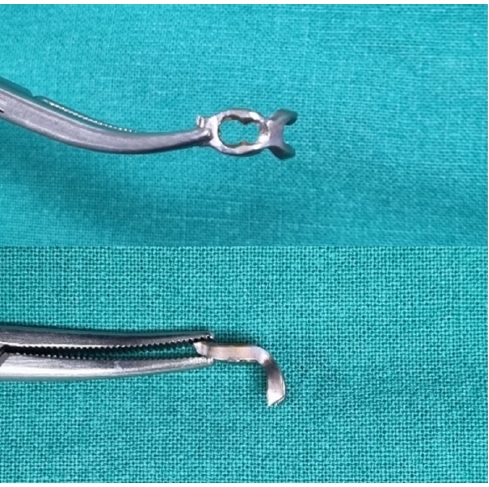
- Hook plate fixation for volar plate avulsion fractures of the middle phalanges in Korea: a case series
- Kang-San Lee, Sang-Woo Son, Hee-June Kim, Hyun-Joo Lee, Dong Hee Kim
- J Musculoskelet Trauma 2026;39(1):48-53. Published online January 25, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00339
-
 Abstract
Abstract
 PDF
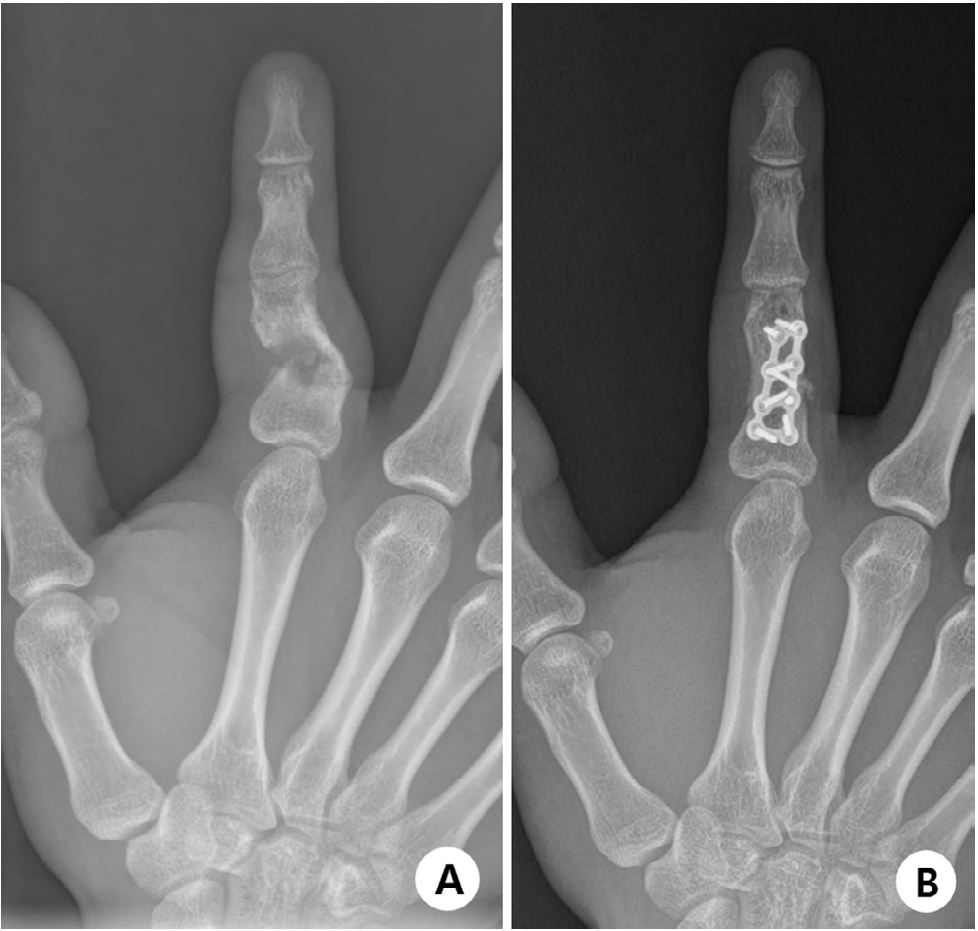
PDF - Background
Volar plate avulsion fractures in phalanges are relatively common injuries. While surgical treatment can help reduce limitations in motion after injury, the small size of the fracture fragment can make the procedure challenging. In this study, we used hook plate fixation as a surgical technique for treating volar avulsion fractures in phalanges and evaluated its radiological and clinical outcomes.
Methods
The medical records of eight patients (nine digits) with volar plate avulsion fractures of the middle phalanx were retrospectively reviewed. All fractures were treated with a 1.5-mm hook plate after open reduction. Radiologic evaluations were performed using simple radiographs, and clinical outcomes were assessed through range of motion, instability, and pain.
Results
The mean follow-up period was 4.89 months (range, 1–9 months). All nine digits achieved bone union at the final follow-up. The mean union time was 2.2 months (range, 1–4 months). In all patients, the range of motion in the proximal interphalangeal joint was 85° (range, 70°–100°) before implant removal and 89.4° (range, 80°–100°) after implant removal. All patients demonstrated no joint instability and no residual pain.
Conclusion
Using a hook plate for volar plate avulsion fractures presents a promising alternative to existing fixation methods. Its biomechanical advantages and ease of fabrication make it a valuable tool in hand surgery. Level of evidence: IV.
- 157 View
- 7 Download

- Surgical outcomes of the coracoid process fracture associated with the acromioclavicular joint injury in Korea: a case series
- Dongju Shin, Sung Choi, Sangwoo Kim, Byung Hoon Kwack
- J Musculoskelet Trauma 2026;39(1):54-61. Published online January 14, 2026
- DOI: https://doi.org/10.12671/jmt.2025.00346

-
 Abstract
Abstract
 PDF
PDF - Background
Excluding technical reports and isolated case reports, there are no published studies evaluating coracoid process fixation with or without an acromioclavicular joint (ACJ) stabilization procedure for coracoid process fractures associated with ACJ injury. The purpose of this study was to assess the surgical outcomes of coracoid process fractures associated with ACJ injuries and to determine the usefulness of coracoid process fixation with or without an ACJ stabilization procedure.
Methods
From February 2006 to December 2015, patients with coracoid process fractures associated with ACJ injuries were enrolled. Radiological and clinical outcomes were analyzed in 12 patients who underwent coracoid process fixation with or without an ACJ stabilization procedure. A 3.5-mm cannulated screw with a washer or a 3.0-mm headless compression screw was used for coracoid process fixation, and either a clavicle hook plate or Kirschner (K)-wires were used for ACJ injuries when additional fixation was necessary.
Results
Bone union was achieved in 11 patients (91.7%), while one case was determined to be a nonunion at 6 months. Radiological union occurred at an average of 3 months (range, 1.5–4 months) in all patients except the nonunion case. At the final follow-up, the average clinical scores were a visual analogue scale (VAS) pain score of 1.5 (range, 0–4) and a UCLA score of 30.9 (range, 28–35). Clinical outcomes were satisfactory in all patients, including the patient with nonunion.
Conclusion
The clinical and radiological outcomes of treating coracoid process fractures associated with ACJ injuries using coracoid process fixation with or without ACJ stabilization were favorable. A cannulated screw with a washer and clavicle hook plate fixation may provide sufficient stability for both the coracoid process fracture and the ACJ injury when feasible. Level of evidence: IV.
- 158 View
- 5 Download

Technical Note
- Rim plate-assisted intramedullary nail and plate combination technique for complex tibial plateau-to-diaphysis fractures: a technical note and case series
- Whee Sung Son
- J Musculoskelet Trauma 2026;39(1):62-71. Published online December 4, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00290

-
 Abstract
Abstract
 PDF
PDF - Complex tibial plateau-to-diaphysis fractures present a significant surgical challenge due to their intricate fracture patterns and frequent association with severe soft tissue damage and concomitant injuries. This technical note introduces a novel fixation strategy: the rim plate-assisted intramedullary nail-plate combination (NPC) technique. In this approach, a rim plate simplifies the conventional NPC procedure by unifying the tibial plateau fracture into a single structural segment. This modification eliminates the need to address the articular and diaphyseal components simultaneously while enhancing articular stability. Furthermore, the technique preserves soft tissue integrity and promotes early rehabilitation. Clinical case examples demonstrate its successful application in managing complex tibial plateau-to-diaphysis injuries. Level of evidence: V.
- 484 View
- 21 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 First
First Prev
Prev


