Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 28(4); 2015 > Article
-
Review Article
- Reconstruction of a Traumatic Soft Tissue Defect
- Jong Woong Park, M.D., Ph.D.
-
Journal of the Korean Fracture Society 2015;28(4):256-265.
DOI: https://doi.org/10.12671/jkfs.2015.28.4.256
Published online: October 19, 2015
Department of Orthopaedic Surgery, Division of Hand Surgery & Reconstructive Microsurgery, Korea University College of Medicine, Seoul, Korea.
- Address reprint requests to: Jong Woong Park, M.D., Ph.D. Department of Orthopaedic Surgery, Korea University Anam Hospital, 73 Inchon-ro, Seongbuk-gu, Seoul 02841, Korea. Tel: 82-2-920-5320, Fax: 82-2-920-5320, ospark@korea.ac.kr
Copyright © 2015 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 763 Views
- 0 Download
- 2 Crossref
Abstract
- Soft tissue defect combined with an open fracture is a very challenging problem to the orthopaedic surgeon. Many complicated open fractures remain with soft tissue defect, chronic osteomyelitis, and sometimes terminate with major limb amputation. Soft tissue defect should be reconstructed as soon as possible, particularly when the bone, tendon, or neurovascular structures are exposed. Exposure for longer than a week significantly increases the risk of secondary infection and tissue necrosis. For the simple soft tissue defect, negative pressure wound closure technology has been introduced and many superficial wounds have been treated successfully using this method. For the more complicated wounds, many kinds of local flaps, pedicled flaps, muscle and fascisocutaneous flaps can be indicated according to the characteristics of the wounds. The free flaps including free vascularized bone graft can be considered as a final choice for the most difficult wound problems. In this article, various reconstruction strategies for soft tissue defect after traumatic open fracture are reviewed.
This review article is enlarged with recently updated knowledges and author's experiences based on the contents of the author's published article (Park JW: Reconstruction of Traumatic Soft Tissue Defect: Local Flap. J Korean Fract Soc. 23(2):251-256, 2010).
None.
None.
- 1. Georgiadis GM, Behrens FF, Joyce MJ, Earle AS, Simmons AL. Open tibial fractures with severe soft-tissue loss Limb salvage compared with below-the-knee amputation. J Bone Joint Surg Am, 1993;75:1431-1441.
- 2. Lange RH. Limb reconstruction versus amputation decision making in massive lower extremity trauma. Clin Orthop Relat Res, 1989;(243):92-99.
- 3. Frykman GK, Leung VC. Free vascularized flaps for lower extremity reconstruction. Orthopedics, 1986;9:841-848.
- 4. Redett RJ, Robertson BC, Chang B, Girotto J, Vaughan T. Limb salvage of lower-extremity wounds using free gracilis muscle reconstruction. Plast Reconstr Surg, 2000;106:1507-1513.
- 5. Levin LS. The reconstructive ladder. An orthoplastic approach. Orthop Clin North Am, 1993;24:393-409.
- 6. Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg, 1986;78:285-292.
- 7. Byrd HS, Cierny G 3rd, Tebbetts JB. The management of open tibial fractures with associated soft-tissue loss: external pin fixation with early flap coverage. Plast Reconstr Surg, 1981;68:73-82.
- 8. Yaremchuk MJ, Brumback RJ, Manson PN, Burgess AR, Poka A, Weiland AJ. Acute and definitive management of traumatic osteocutaneous defects of the lower extremity. Plast Reconstr Surg, 1987;80:1-14.
- 9. Karanas YL, Nigriny J, Chang J. The timing of microsurgical reconstruction in lower extremity trauma. Microsurgery, 2008;28:632-634.
- 10. Wester JL, Pittman AL, Lindau RH, Wax MK. AlloDerm with split-thickness skin graft for coverage of the forearm free flap donor site. Otolaryngol Head Neck Surg, 2014;150:47-52.PDF
- 11. Masquelet AC, Gilbert A. An atlas of flaps of the musculoskeletal system. London: Malden: Martin Dunitz; 2003. p. 275-293.
REFERENCES
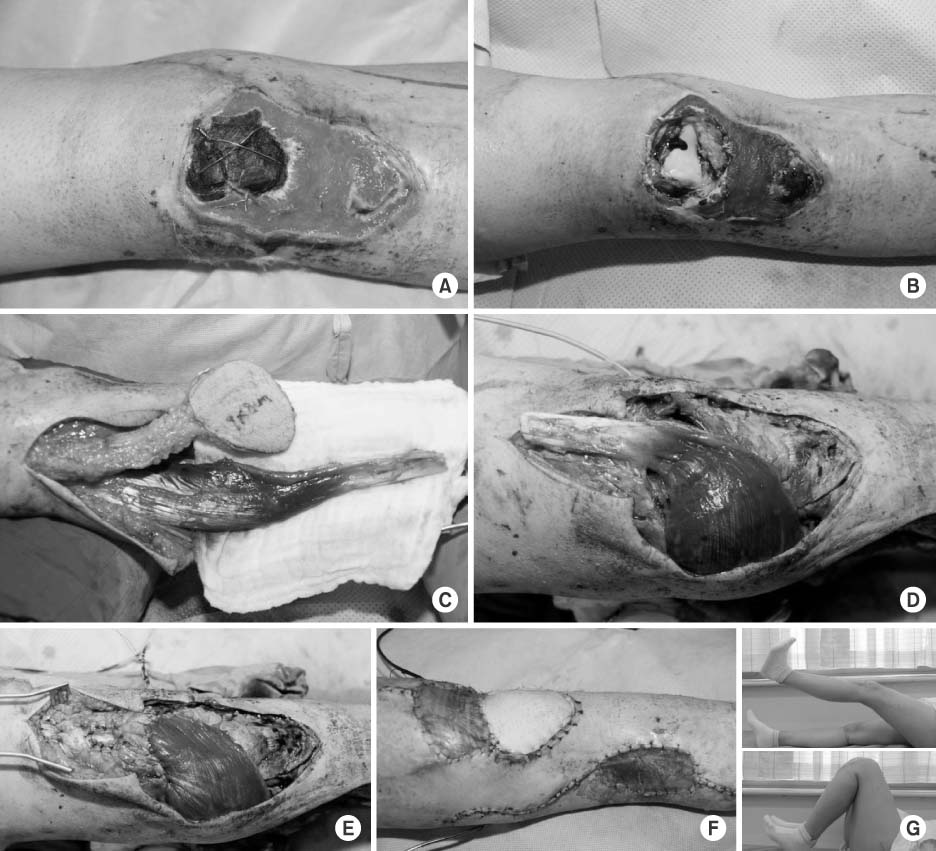
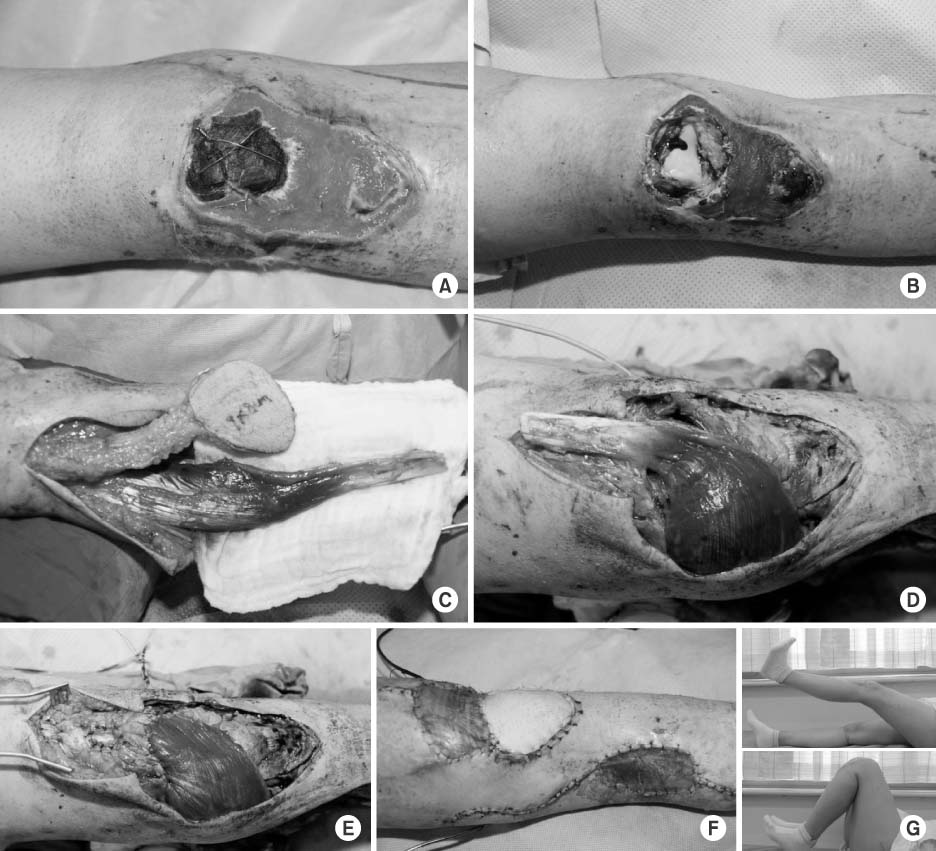
Open fracture around the knee joint. (A) Necrosis of patella and loss of patella tendon. (B) After debridement, the knee joint is opened and reconstruction of quadriceps mechanism is required. (C) Medial gastrocnemius muscle flap and saphenous neurocutaneous island flap are harvested. (D, E) The gastrocnemius muscle is turned to be sutured to the quadriceps muscle. (F) The remaining defect is covered with the saphenous neurocutaneous island flap. (G) Two years later, full range of motion of the knee joint is recovered and the motor grade reaches grade 4.
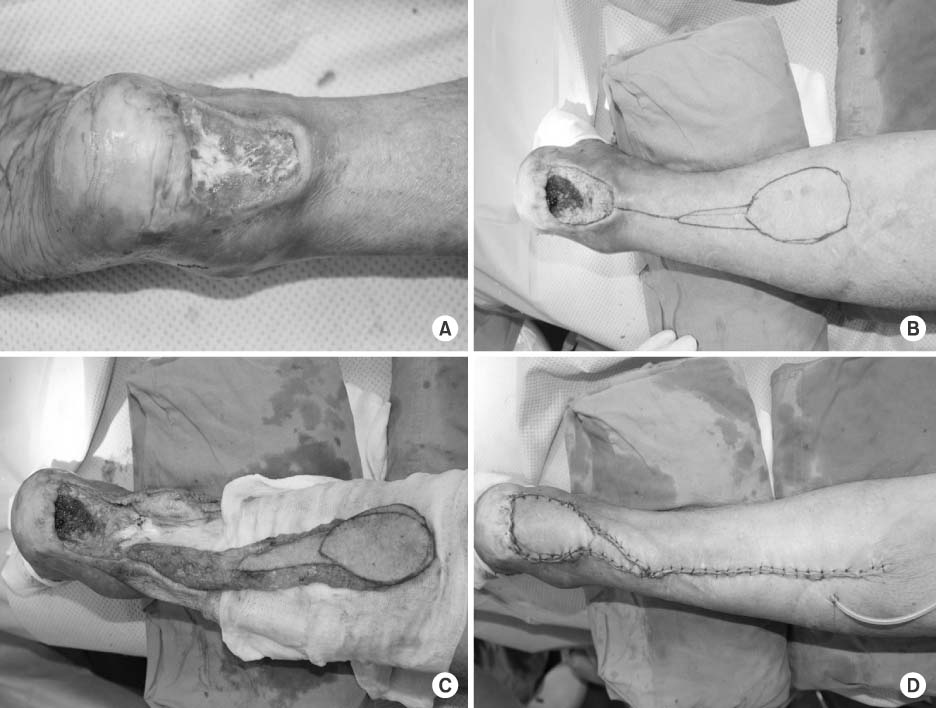
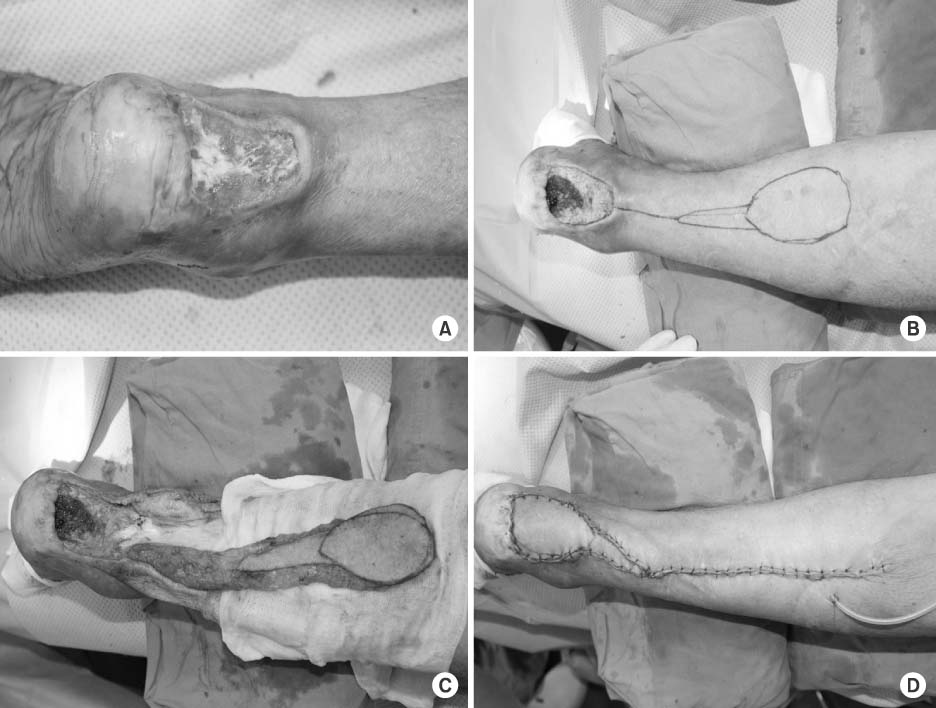
Reverse sural artery flap. (A) Soft tissue defect at the posterior aspect of the ankle. (B) Reverse sural artery flap is designed. (C) Pedicled flap is dissected. (D) After completion of flap insetting.
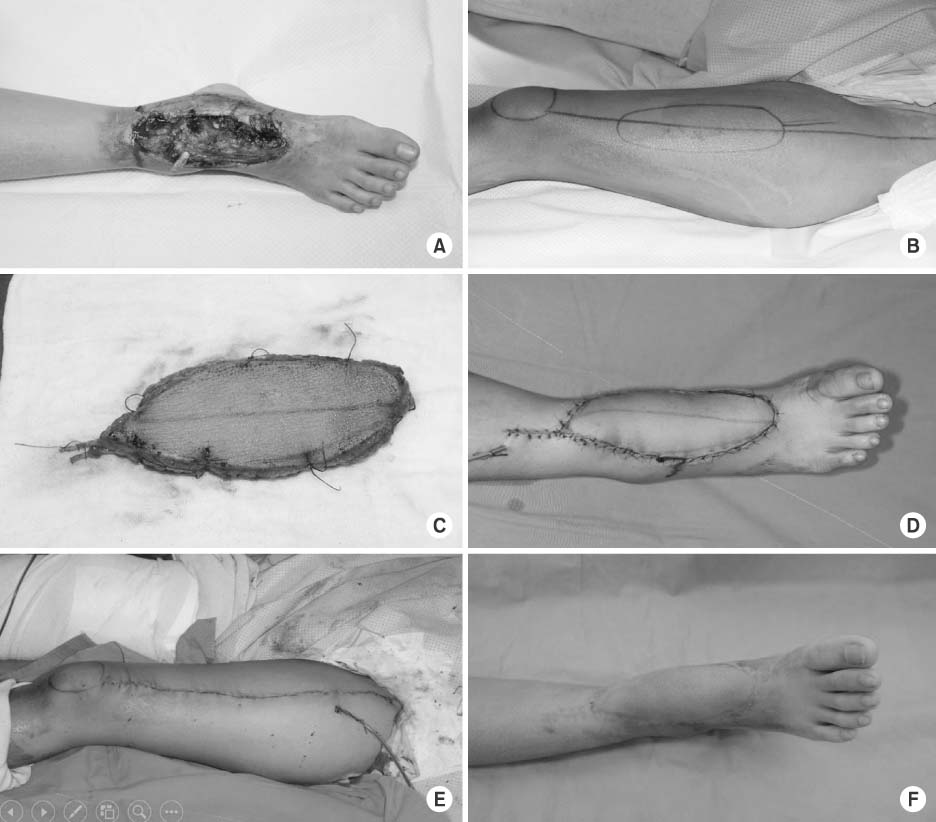
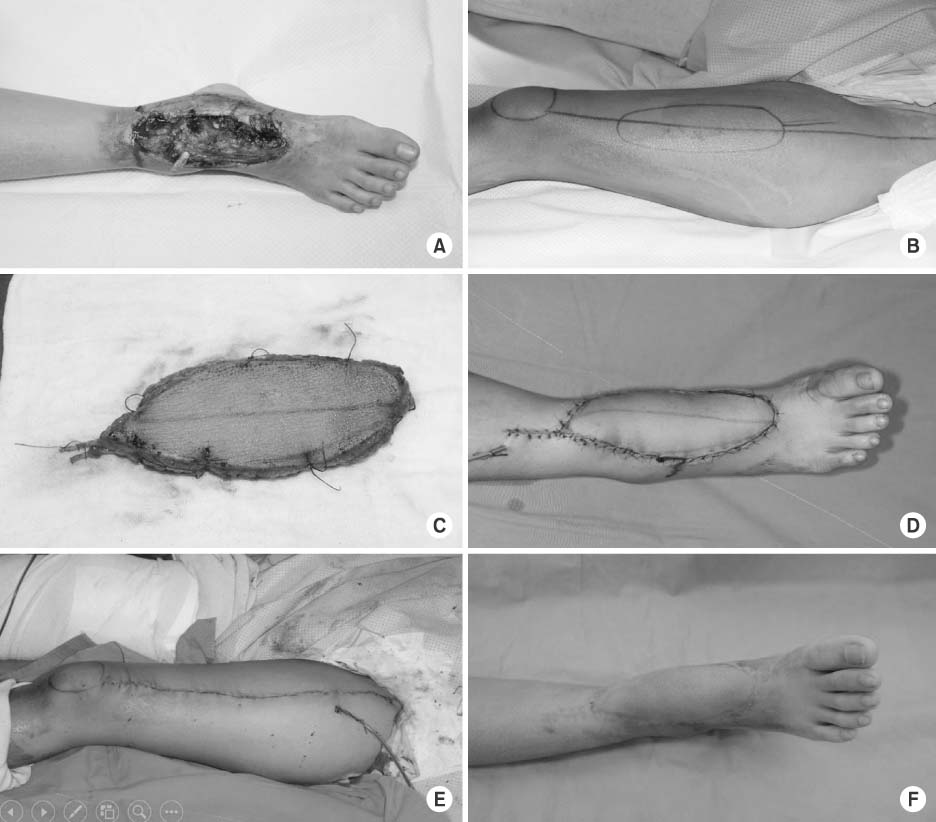
Anterolateral thigh (ALT) flap. (A) Contaminated soft tissue defect on the anterior ankle. (B) ALT flap is designed. (C) Dissected ALT flap. (D) Flap insetting. (E) Donor site is primarily closed. (F) Two months after the operation.
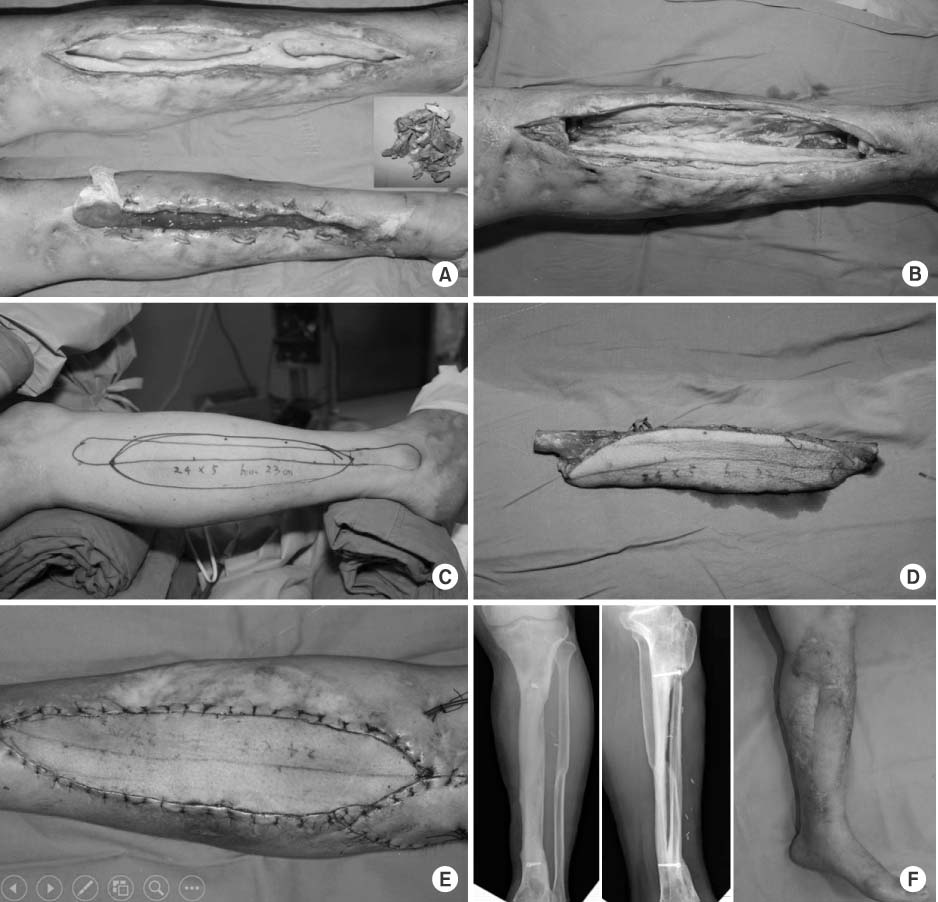
Free vascularized fibular osteocutaneous flap. (A) Large tibia and soft tissue defect after infected open fracture. (B) Sequestrum is removed. (C, D) Free vascularized fibular graft is harvested from the ipsilateral leg. (E) Flap is fixed and repaired. (F) Two years after bone and soft tissue reconstruction.
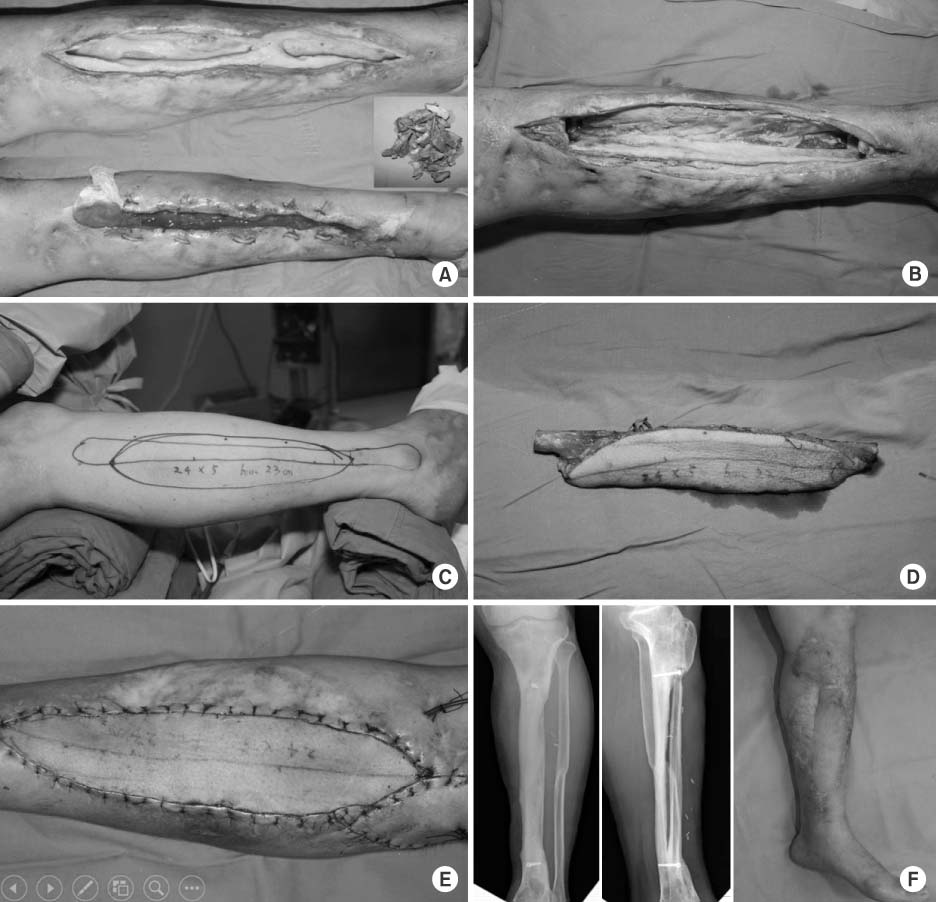
Figure & Data
REFERENCES
Citations


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

