Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(2); 2020 > Article
- Review Article Treatment of Periprosthetic Fracture after Total Elbow Replacement Arthroplasty
- Hyunseok Seo, Jin-Hyung Im, Joo-Yup Lee
-
Journal of Musculoskeletal Trauma 2020;33(2):110-117.
DOI: https://doi.org/10.12671/jkfs.2020.33.2.110
Published online: April 30, 2020

2Department of Orthopedic Surgery, Gyeongsang National University Changwon Hospital, Changwon, Korea

- 1,087 Views
- 42 Download
- 1 Crossref
- 0 Scopus
Abstract
The indications for total elbow replacement arthroplasty (TERA) include rheumatoid arthritis, degenerative arthritis, acute fracture, nonunion, malunion, posttraumatic arthritis, tumor, and chronic instability. With the development of designs and the increasing use of TERA, more periprosthetic fractures are occurring. On the other hand, there is less data on periprosthetic fractures after TERA because TERA is a relatively rare procedure. Thus, a careful review of the previous literature and appropriate selection of surgical indications are essential for achieving a satisfactory outcome, which should be accompanied by precise surgery as planned. This article presents the causes, risk factors, classification, and principles of treatment of periprosthetic fractures after TERA.
Published online Apr 28, 2020.
https://doi.org/10.12671/jkfs.2020.33.2.110
Treatment of Periprosthetic Fracture after Total Elbow Replacement Arthroplasty
Abstract
The indications for total elbow replacement arthroplasty (TERA) include rheumatoid arthritis, degenerative arthritis, acute fracture, nonunion, malunion, posttraumatic arthritis, tumor, and chronic instability. With the development of designs and the increasing use of TERA, more periprosthetic fractures are occurring. On the other hand, there is less data on periprosthetic fractures after TERA because TERA is a relatively rare procedure. Thus, a careful review of the previous literature and appropriate selection of surgical indications are essential for achieving a satisfactory outcome, which should be accompanied by precise surgery as planned. This article presents the causes, risk factors, classification, and principles of treatment of periprosthetic fractures after TERA.
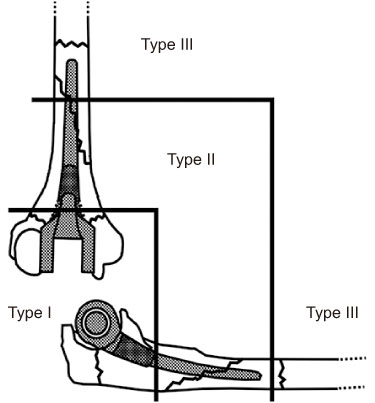
Fig. 1
Mayo classification of periprosthetic fractures after elbow arthroplasty. Type I, fracture of the humeral condyles and olecranon. Type II, humeral and ulnar shaft fracture along the length of the stem. Type III, fracture past the tip of the prosthesis.
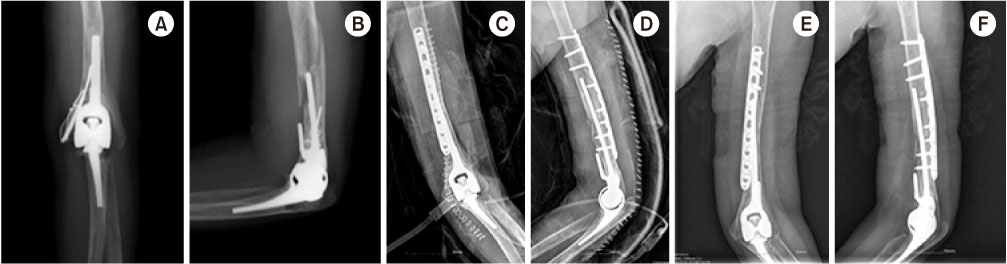
Fig. 2
(A, B) Anteriorposterior (A) and lateral (B) elbow radiographs of a 41-year-old female with rheumatoid arthritis. The comminuted intra-articular fracture of the distal humerus with the displacement of the medial condyle was found. (C) Total elbow replacement arthroplasty was performed, and tension-band wiring was simultaneously applied simultaneously to fix the medial humeral condylar fracture. (D) Anteriorposterior radiographs of 3 months postoperatively, showing bony union.
Fig. 3
(A, B) Anteriorposterior (A) and lateral (B) elbow radiographs of the same patient in Fig. 2 shows the fracture line involved proximal and distal to the tip of the prosthesis with evidence of loosening. The fracture was caused by slip down at 3 years and 7 months after the primary total elbow replacement arthroplasty. (C, D) Revision arthroplasty was done with autologous iliac bone grafting and locking compression plate fixation. (E, F) Anteriorposterior (E) and lateral (F) radiographs of 6 months postoperatively, showing bony union.
Fig. 4
(A) Anteriorposterior and lateral elbow radiographs of a 67-year-old female who had internal fixation for the distal humeral intercondylar and olecranon fracture in the other hospital three-months ago. The radiographs showed no evidence of bony union at the distal humerus. (B) Removal of hardware and total elbow replacement arthroplasty were done. The long arm splint with elbow extension was applied anteriorly after the surgery. (C) Lateral elbow radiographs 1 month postoperatively, showing refracture of the previous olecranon osteotomy site. Conservative treatment with long arm splint was planned. (D) Lateral elbow radiographs of 2 months postoperatively, showing union of the fracture.
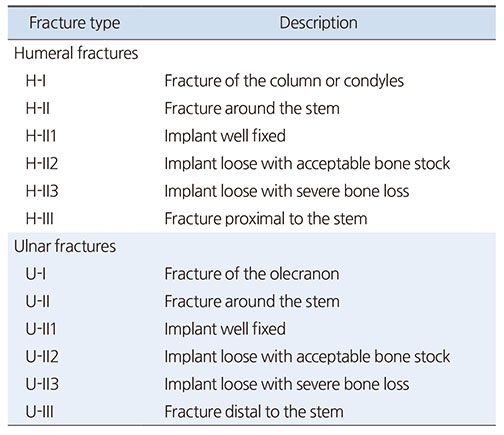
Table 1
Mayo Classification of Periprosthetic Fractures of the Elbow
Table 2
Grading Scale for Humeral Bone Loss
Financial support:None.
Conflict of interests:None.
References
-
Lee SM, Park JC, Song SW, et al. Periprosthetic fractures after total elbow replacement. J Korean Soc Surg Hand 2010;15:107–111.
-
-
O'Driscoll SW, Morrey BF. Periprosthetic fractures about the elbow. Orthop Clin North Am 1999;30:319–325.
-
-
Mavrogenis AF, Angelini A, Guerra E, Rotini R. Humeral fracture between a total elbow and total shoulder arthroplasty. Orthopedics 2011;34:315.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS





 Cite
Cite

