Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 26(4); 2013 > Article
-
Original Article
- Outcomes and Analysis of Factors Affecting Bone Union after Interlocking Intramedullary Nailing in Segmental Tibia Fractures
- Sang Soo Park, M.D., Jun-Young Lee, M.D., Sang-Ho Ha, M.D., Sung-Hae Park, M.D.
-
Journal of the Korean Fracture Society 2013;26(4):275-283.
DOI: https://doi.org/10.12671/jkfs.2013.26.4.275
Published online: October 18, 2013
Department of Orthopaedic Surgery, School of Medicine, Chosun University, Gwangju, Korea.
- Address reprint requests to: Jun-Young Lee, M.D. Department of Orthopaedic Surgery, Chosun University Hospital, 365 Pilmun-daero, Dong-gu, Gwangju 501-717, Korea. Tel: 82-62-220-3147, Fax: 82-62-226-3379, leejy88@chosun.ac.kr
• Received: January 18, 2013 • Revised: July 25, 2013 • Accepted: August 7, 2013
Copyright © 2013 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 641 Views
- 3 Download
- 1 Crossref
Abstract
-
Purpose
- To evaluate the radiological results and complications of interlocking intramedullary nailing for segmental tibia fractures.
-
Materials and Methods
- Twenty-six patients (26 cases) who underwent interlocking intramedullary nailing for segmental tibia fractures between January 2003 and May 2011 were followed for more than one year. We evaluated the complications and statistically analyzed the factors influencing bone union, including open fracture, fracture site, reaming, postoperative angulation, and postoperative fracture gap.
-
Results
- Nineteen cases (73%) achieved bone union with one operation at an average of 7 months (range, 5 to 11). Seven cases had secondary procedures before achieving union. Complications included 7 cases of nonunion, 3 cases of incomplete peroneal nerve injury, 2 cases of superficial infection, 1 case of compartment syndrome. Factors showing statistically significant differences were open fracture, postoperative angulation, and postoperative fracture gap. Factors showing no statistically significant difference were fracture site and reaming.
-
Conclusion
- Nonunion is the most common complication in interlocking intramedullary nailing for segmental tibia fractures. To minimize this complication, comprehension of surgical techniques to reduce anatomically and careful evaluation of the fracture are required.
- 1. Bone LB, Kassman S, Stegemann P, France J. Prospective study of union rate of open tibial fractures treated with locked, unreamed intramedullary nails. J Orthop Trauma, 1994;8:45-49.
- 2. Borrelli J Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma, 2002;16:691-695.
- 3. Canale ST, Beaty JH. Campbell's operative orthopaedics. 11th ed. Philadelphia: Mosby; 2008.vol. 3: p. 3530.
- 4. Catagni MA, Guerreschi F, Holman JA, Cattaneo R. Distraction osteogenesis in the treatment of stiff hypertrophic nonunions using the Ilizarov apparatus. Clin Orthop Relat Res, 1994;301:159-163.
- 5. Chun CH, Lee BC, Hwang GT, Kwon SG, Lee HS. Tibial segmental fracture treated with interlocking intramedullary nail. J Korean Soc Fract, 1997;10:534-540.
- 6. Collinge CA, Sanders RW. Percutaneous plating in the lower extremity. J Am Acad Orthop Surg, 2000;8:211-216.
- 7. Fisher WD, Hamblen DL. Problems and pitfalls of compression fixation of long bone fractures: a review of results and complications. Injury, 1978;10:99-107.
- 8. Huang CK, Chen WM, Chen TH, Lo WH. Segmental tibial fractures treated with interlocking nails. A retrospective study of 33 cases. Acta Orthop Scand, 1997;68:563-566.
- 9. Hupel TM, Weinberg JA, Aksenov SA, Schemitsch EH. Effect of unreamed, limited reamed, and standard reamed intramedullary nailing on cortical bone porosity and new bone formation. J Orthop Trauma, 2001;15:18-27.
- 10. Krettek C, Miclau T, Schandelmaier P, Stephan C, Mohlmann U, Tscherne H. The mechanical effect of blocking screws ("Poller screws") in stabilizing tibia fractures with short proximal or distal fragments after insertion of small-diameter intramedullary nails. J Orthop Trauma, 1999;13:550-553.
- 11. Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop Relat Res, 1995;(315):64-74.
- 12. Langard O, Bo O. Segmental tibial shaft fractures. Acta Orthop Scand, 1976;47:351-357.
- 13. Leunig M, Hertel R. Thermal necrosis after tibial reaming for intramedullary nail fixation. A report of three cases. J Bone Joint Surg Br, 1996;78:584-587.
- 14. Melis GC, Sotgiu F, Lepori M, Guido P. Intramedullary nailing in segmental tibial fractures. J Bone Joint Surg Am, 1981;63:1310-1318.
- 15. Nicoll EA. Fractures of the tibial shaft. A survey of 705 cases. J Bone Joint Surg Br, 1964;46:373-387.
- 16. Olerud S, Karlstrom G. Tibial fractures treated by AO compression osteosynthesis. Experiences from a five year material. Acta Orthop Scand Suppl, 1972;140:1-104.
- 17. Rhee JH, Lee JW, Cho JY, Bae SW, Yoon SH, Lee JY. Nonunion after interlocking intramedullay nailing in tibia segmental fractures. J Korean Soc Fract, 1997;10:309-315.
- 18. Robinson CM, McLauchlan GJ, McLean IP, Court-Brown CM. Distal metaphyseal fractures of the tibia with minimal involvement of the ankle. Classification and treatment by locked intramedullary nailing. J Bone Joint Surg Br, 1995;77:781-787.PDF
- 19. Song GH. Treatment of femoral fractures by bone grafting from trochanter and interlocking intramedullary nail fixation. Zhongguo Gu Shang, 2010;23:950-951.
- 20. Song KJ, Lee KB, Hwang BY. Analysis for the factors influencing bone union in segmental tibial shaft fractures treated with interlocking intramedullary nailing. J Korean Fract Soc, 2004;17:153-159.
- 21. Tarr RR, Resnick CT, Wagner KS, Sarmiento A. Changes in tibiotalar joint contact areas following experimentally induced tibial angular deformities. Clin Orthop Relat Res, 1985;(199):72-80.
- 22. Tornetta P 3rd, Collins E. Semiextended position of intramedullary nailing of the proximal tibia. Clin Orthop Relat Res, 1996;(328):185-189.
- 23. Tucker HL, Kendra JC, Kinnebrew TE. Management of unstable open and closed tibial fractures using the Ilizarov method. Clin Orthop Relat Res, 1992;(280):125-135.
- 24. Wu CC, Shih CH. Segmental tibial shaft fractures treated with interlocking nailing. J Orthop Trauma, 1993;7:468-472.
REFERENCES
Fig. 1
(A, B) Preoperative radiographs of a 56-year-old man show a tibia segmental fracture classified as AO/OTA type 43-C2.
(C, D) The segmental tibia fracture was stabilized with intramedullary interlocking nailing using reaming.
(E, F) Postoperative radiographs show complete bone union with good alignment at 14 months after surgery.


Fig. 2
(A) Intraoperative C-arm image using the blocking screw technique in the proximal portion of segmental tibia fracture.
(B) Intraoperative C-arm image shows good alignment and reduction after intramedullary nailing with a blocking screw on the tibia proximal portion.
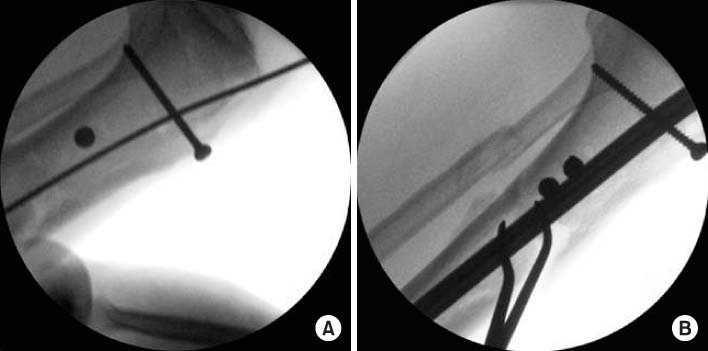
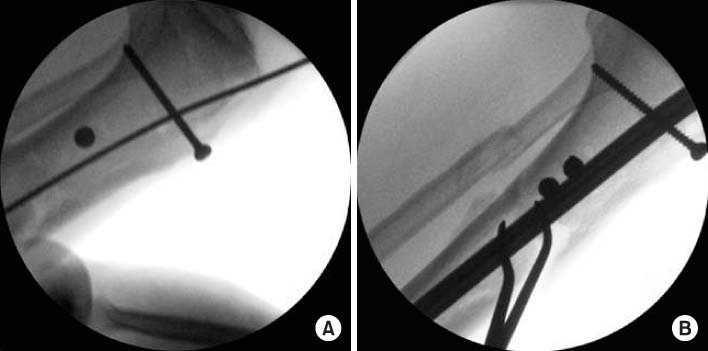
Fig. 3
(A, B) Preoperative radiographs of a 47-year-old man show a tibia segmental fracture classified as AO/OTA type 43-C2.
(C, D) Postoperative radiographs show good alignment and reduction after intramedullary interlocking nailing with additional plating on the tibia proximal portion.


Fig. 4
(A, B) Preoperative radiographs of a 51-year-old man show a tibia segmental open fracture classified as AO/OTA type 43-C2.
(C, D) Initial clinical photo shows Gustilo-Anderson classification IIIA open wound, exposing the bone and muscle.
(E, F) Segmental tibia fracture was stabilized with intramedullary interlocking nailing using unreaming.
(G, H) Follow up x-ray at 16 months after surgery shows nonunion in the proximal and distal sites.
(I) Reoperation has been done with exchange nailing. Postoperative radiographs show complete bone union at 28 months after
primary surgery.


Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Clinical Outcome after Treatment of Tibia Segmental Fracture with Intramedullary Nailing and Minimal Invasive Plate Osteosynthesis
Jun Young Lee, Hyung Seok Park, Dong Hyuk Cha
Journal of the Korean Fracture Society.2020; 33(3): 142. CrossRef
Outcomes and Analysis of Factors Affecting Bone Union after Interlocking Intramedullary Nailing in Segmental Tibia Fractures

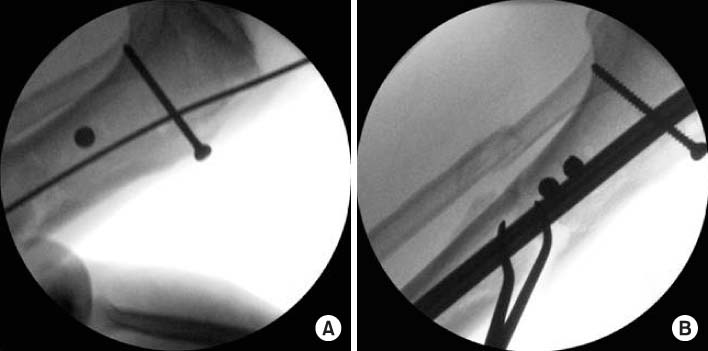


Fig. 1
(A, B) Preoperative radiographs of a 56-year-old man show a tibia segmental fracture classified as AO/OTA type 43-C2.
(C, D) The segmental tibia fracture was stabilized with intramedullary interlocking nailing using reaming.
(E, F) Postoperative radiographs show complete bone union with good alignment at 14 months after surgery.
Fig. 2
(A) Intraoperative C-arm image using the blocking screw technique in the proximal portion of segmental tibia fracture.
(B) Intraoperative C-arm image shows good alignment and reduction after intramedullary nailing with a blocking screw on the tibia proximal portion.
Fig. 3
(A, B) Preoperative radiographs of a 47-year-old man show a tibia segmental fracture classified as AO/OTA type 43-C2.
(C, D) Postoperative radiographs show good alignment and reduction after intramedullary interlocking nailing with additional plating on the tibia proximal portion.
Fig. 4
(A, B) Preoperative radiographs of a 51-year-old man show a tibia segmental open fracture classified as AO/OTA type 43-C2.
(C, D) Initial clinical photo shows Gustilo-Anderson classification IIIA open wound, exposing the bone and muscle.
(E, F) Segmental tibia fracture was stabilized with intramedullary interlocking nailing using unreaming.
(G, H) Follow up x-ray at 16 months after surgery shows nonunion in the proximal and distal sites.
(I) Reoperation has been done with exchange nailing. Postoperative radiographs show complete bone union at 28 months after
primary surgery.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
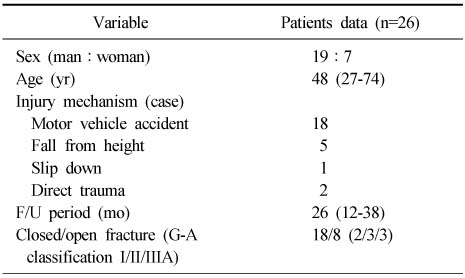
Outcomes and Analysis of Factors Affecting Bone Union after Interlocking Intramedullary Nailing in Segmental Tibia Fractures
Demographic Data of the Patients
Values are presented as number or median (range). F/U: Follow up, G-A: Gutilo-Anderson Classification of Open Fractures.
Table 1
Demographic Data of the Patients
Values are presented as number or median (range). F/U: Follow up, G-A: Gutilo-Anderson Classification of Open Fractures.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

