Abstract
-
Background
The COVID-19 pandemic is likely to have affected bone health in older adults in Korea. This study aimed to analyze changes in the epidemiology and management of distal radius fractures (DRFs) in older adults before and during the COVID-19 pandemic.
-
Methods
Patients with DRF aged over 50 years in 2017, 2018, 2020, and 2021 were included in this study. Patients were classified into a group with DRF occurring between 2017 and 2018 (before COVID-19) and a group with DRF occurring between 2020 and 2021 (during COVID-19). We calculated the incidence rates of DRF and compared them between the two groups. We also analyzed and compared demographic data (age, sex, income, residence) and the operation rate for DRF between the two groups. Patient selection and treatment were based on International Classification of Diseases, 10th revision codes.
-
Results
A total of 140,634 patients with DRF (before COVID-19, 69,794; during COVID-19, 70,840) were included. The incidence of DRF before COVID-19 (184.4/100,000 person-years) was higher than during COVID-19 (169.8/100,000 person-years). The operation rate was higher during COVID-19 (86.9%) than before COVID-19 (83.3%).
-
Conclusions
During the COVID-19 pandemic, the incidence of DRF decreased in South Korea. However, the rate of surgical treatment increased and exceeded the global surgical rate.
-
Level of evidence
III.
-
Keywords: COVID-19, Radius fractures, Wrist fractures, Disease management
Introduction
Background
Distal radius fractures (DRFs) account for approximately 16% of all fractures treated by orthopedic surgeons [
1,
2]. In contrast to high-energy-induced DRFs, which primarily occur in a relatively young population (ages, 5 to 24 years) and predominantly among males, DRFs in the older adults population—predominantly female—often result from low-energy trauma, such as simple falls during daily activities. DRFs in older adults represent a hallmark of fragility fractures in the upper extremity, alongside osteoporotic fractures of the spine and hip. Although DRFs can occur in younger individuals, they are more commonly seen in men over 60 years of age and women after menopause, typically in their 50s [
3].
As life expectancy increases in Korea, DRF in older adults has also been increasing and medical costs rose accordingly [
4,
5]. Before the COVID-19 pandemic, advancements in medical science and the increasing prevalence of physically healthy older adults contributed to a higher proportion of active treatments, including surgical interventions. This shift was further driven by the growing number of patients seeking rapid recovery following DRFs.
Since the outbreak of COVID-19 in late 2019, the global community has faced unprecedented challenges. The pandemic’s rapid spread, coupled with high mortality rates, has significantly increased medical demand. Countries worldwide implemented varying strategies to combat COVID-19, with particular attention to the older adults, who are at heightened risk for severe illness and death. These health risks necessitated greater care and precautionary measures for the older adult populations, including wearing masks, social distancing, and avoiding public places. Consequently, many older adults experienced increased feelings of isolation and loneliness, exacerbated by the closure of public spaces like restaurants, parks, and gyms. These changes forced seniors to adapt to alternative methods for staying active and maintaining their health.
This restricted environment is likely to have affected bone health in the older adult population in Korea, and it is highly likely to have changed the pattern of osteoporotic fractures during this COVID-19 period. Even if an actual osteoporotic fracture occurs, appropriate treatment might not have been provided because of limited medical capacity during the COVID-19 pandemic, and changes in complications and mortality rates can also be expected.
Objectives
Based on these changes, we hypothesized that the incidence of DRFs would decline due to reduced outdoor activity, and that surgical treatment rates would also decrease because of limited access to operative care. Therefore, this study aimed to evaluate nationwide changes in the incidence and management patterns of DRFs before and during the COVID-19 pandemic in Korea.
Methods
Ethics statement
This study was conducted with approval from the Institutional Review Board (IRB) of National Health Insurance Service Ilsan Hospital (IRB No. NHIMC-2023-03-062), which waived the requirement for informed consent as the data were analyzed anonymously.
Study design
It is a repeated cross-sectional study based on data from the National Health Insurance Service (NHIS) of Korea to compare the incidence and operation of DRF before and during COVID-19 pandemic.
Setting
NHIS qualification data were accessed and the data for target population during the periods 2017–2018 and 2020–2021 were retrieved.
Participants
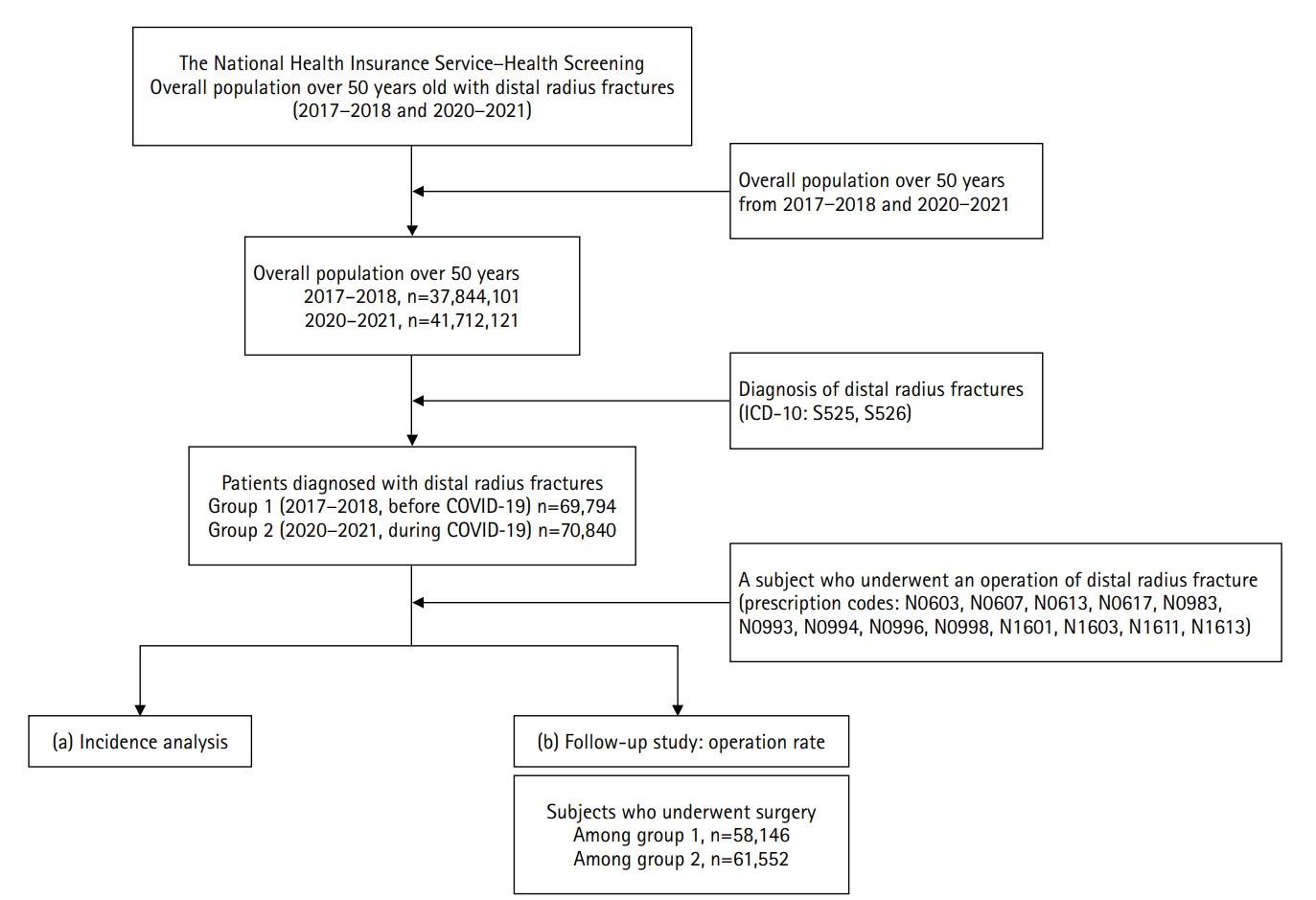
Patient selection for each disease and treatment was based on ICD-10 codes registered with the NHIS. Study participants were identified using NHIS qualification data and included patients aged over 50 years who were diagnosed with DRFs during the periods 2017–2018 and 2020–2021. The ICD-10 codes for DRFs (S52.5 and S52.6) were used for this purpose. To ensure reliable data collection and include only newly diagnosed DRFs within the study periods, a washout period was applied in 2016 and 2019, during which patients identified were excluded from the analysis.
After the initial screening and identification of all patients for the relevant study periods, operation prescription codes (N0603, N0607, N0613, N0617, N0983, N0993, N0994, N0996, N0998, N1601, N1603, N1611, and N1613) were used to identify treatment procedures following the diagnosis. These codes are detailed in
Supplement 1. The flowchart illustrating patient selection and categorization is provided in
Fig. 1.
The primary exposure was calendar period, categorized as pre-COVID-19 (2017–2018) and during COVID-19 (2020–2021). Primary outcome variables for comparison were incidence of DRF. The secondary outcomes included operation rates, surgical technique category, and all-cause mortality within 1 year of the index date. Patient-level covariates included sex, age, income, residence, mortality rate within one year, and the Charlson Comorbidity Index (CCI) score at index date.
Data sources
The study population was drawn from the NHIS, the single largest public insurer in Korea, providing health coverage for all citizens residing in South Korea [
6]. The NHIS maintains comprehensive datasets encompassing 99% of claims data from healthcare providers. These datasets include information on both inpatients and outpatients, covering demographics, diagnoses, and prescriptions. The data fields include sex, age, diagnosis codes based on the International Classification of Diseases (ICD-10) and Korean Classification of Diseases (KCD), as well as treatments covered by the NHIS.
All patients with DRFs from 2017 to 2018 were designated as the reference group 1 (before COVID-19), while patients from 2020 to 2021 were categorized as the comparison group 2 (during COVID-19). The incidence rate of DRF was calculated for each group by dividing the number of cases by the total time at risk for all individuals to develop the condition [
7]. More specifically, we estimated incidence rates by dividing the total number of incident DRF cases in each 2-year period by the sum of the mid-year populations aged 50 years and older in the corresponding two calendar years, which approximates the total person-years at risk. The results are expressed per 100,000 person-years.
Operation rate and type of surgery
We analyzed the number of subjects who underwent operative treatment following a diagnosis of DRF. Operative management was identified using the prescription origin codes of NHIS (
Supplement 1). Additionally, the type of surgery—including open reduction and internal fixation (ORIF), closed reduction and pinning, and external fixation—was categorized based on the corresponding NHIS prescription codes.
Other demographics
We measured and compared gender, age, income, residence, mortality rate within one year, and the CCI score between the two groups [
8]. Income levels were categorized into five groups at 20% intervals, with level 1 representing the lowest income and level 5 the highest. Residential areas were classified into metropolitan and nonmetropolitan regions. The CCI score was calculated to predict mortality based on concurrent conditions such as heart disease, AIDS, or cancer, encompassing a total of 17 categories. A score of zero indicates no comorbidities, while higher scores correspond to an increased predicted mortality rate.
Potential biases include misclassification, as DRFs and surgeries were identified using administrative codes rather than radiographic confirmation. Duplicate counting may occur due to repeated claims; we minimized this by applying washout periods and an episode-based counting rule, which considers only the first qualifying claim per individual within each period. Ascertainment bias is possible during the COVID-19 pandemic if healthcare-seeking behavior or access to care changed, potentially leading to under-recording of fractures.
Study size
A formal sample size calculation was not performed because this was a population-based study using nationwide claims data. We included all eligible NHIS beneficiaries aged ≥50 years within the prespecified calendar periods and captured all incident DRF cases meeting the operational definition.
Statistical methods
For continuous data, the mean, standard deviation, minimum, and maximum values were presented, while categorical data were summarized as frequency and percentage. Pearson chi-squared test was employed to determine statistical significance between the two groups. All statistical analyses were conducted using SAS ver. 9.4 (SAS Institute) and R ver. 4.4.2 (R Foundation for Statistical Computing).
Results
Participants
The details of total population and patients with DRF were summarized in
Table 1.
The total population of the pre-COVID-19 group (group 1, 2017–2018) aged over 50 was 37,844,101. Among them, 69,794 subjects were diagnosed with DRFs. Similarly, the total population of the during-COVID-19 group (group 2, 2020–2021) was 41,712,121, with 70,840 diagnosed cases of DRF. The incidence rate of DRF before COVID-19 was 184.43 per 100,000 population, compared to 169.83 per 100,000 population during COVID-19. The details of incidence rate are shown in
Table 2.
Operation rate and type of surgery
Before COVID-19, 83.3% (58,146 out of 69,794) of patients underwent operative management. During COVID-19, this proportion increased to 86.9% (61,552 out of 70,840). The details of the operative techniques are summarized in
Table 3. Open reduction and internal fixation was the most commonly performed modality, accounting for 70.7% of cases overall, and was more frequently performed during COVID-19 (76.5%, group 2) compared to before COVID-19 (64.8%, group 1).
Other demographics
Table 4 presents and compares the outcomes before and during COVID-19. Although statistical significance was observed for several variables (sex, P<0.0001; age, P<0.0001, income, P<0.0002; surgery rate, P<0.0001; CCI score, P<0.0001), these differences were not considered clinically meaningful due to the large sample size and were therefore not emphasized in the table. Nevertheless, residence (P=0.47) and mortality rate (P=0.15) did not show significant differences between the two groups, even with the large sample size.
Discussion
Key results
Our findings showed that Korea exhibited a distinctive pattern during the pandemic, characterized by a decrease in fracture incidence but a simultaneous increase in surgical management compared with the prepandemic period. This study also provides valuable insight into the national epidemiology and management patterns of DRFs in South Korea. DRFs in the older adult population—predominantly female—often result from low-energy trauma, such as trivial daily activities.
Interpretation
Age and gender have a pronounced effect on the incidence rates of DRFs in the older adults [
9,
10]. The most frequent age group was 60–69 years, and women were significantly more likely than men to experience DRFs both before (2.61 times) and during (2.50 times) COVID-19 (
Table 4). The incidence rate begins to rise after the age of 50 and nearly doubles with each subsequent decade (
Table 2).
Our study had several strengths. First, we analyzed a large dataset containing whole national population provided by the NHIS, which ensures the reliability and generalizability of the findings. The comprehensive scope of the data allowed for an in-depth analysis of epidemiological and management trends in DRFs among the older adults. To our knowledge, there was no nationwide database study comparing the incidence and other demographics of DRF before and during COVID-19 pandemic in South Korea. Second, the data collected were based on a nationwide population, and there was the least chance of selection bias, providing insight to the current management of DRFs in South Korea. Additionally, the study’s focus on a specific and vulnerable age group provides valuable insights into the effects of the COVID-19 pandemic on healthcare access and treatment outcomes.
The reduced numbers of orthopedic fractures, including DRFs, during the COVID-19 pandemic can be explained by lockdown measures, reduced physical activity, and prolonged indoor confinement. The older adults stayed mostly at home due to fears of infection. Some of them did not seek medical attention despite their injury and let it heal without any orthopedic intervention. Poggetti et al. [
11] reported a 28.6% decrease in the number of patients undergoing surgery due to hand and wrist trauma in one of the Italian hospitals during the COVID-19 pandemic. In one of the Turkish hospitals, the total number of fractures recorded during the COVID-19 pandemic was by 61.6% lower than the number of fractures recorded in 2019 [
12].
Consistent with previous Korean data, this study also demonstrated age-related differences in DRF epidemiology. Kwon et al. [
13] reported that the incidence of DRFs steadily increases with advancing age, reflecting their nature as fragility fractures typically caused by low-energy trauma. In our study, the incidence in the 50–59 age group declined during the COVID-19 pandemic compared with the prepandemic years. This may be explained by the fact that relatively younger older adults, who are usually more active, experienced restricted outdoor and leisure activities during the pandemic. In contrast, older adults continued to sustain DRFs at home through trivial falls, which may have contributed to the relatively higher proportion of advanced-age patients during the COVID-19 pandemic.
Since the introduction of volar locking plate fixation in the early 2000s, there has been a notable shift toward more operative treatments [
14-
16]. Despite this ongoing trend, we anticipated a temporary decline in surgical rates during the COVID-19 pandemic because of reduced access to medical care. Contrary to our expectation, however, the surgical proportion of DRFs in Korea actually increased. A US analysis similarly reported a slight rise in surgical management from 2019 to 2020 (50.2% to 52.0%), although the underlying causes remain unclear due to various confounding factors, such as quarantine guidelines, supply chain disruptions, and resource limitations [
17]. This pattern suggests that the rise in surgical proportion may reflect an ongoing nationwide trend toward operative fixation, rather than a direct effect of the COVID-19 pandemic.
In Korea, the surgical rate has consistently exceeded global levels, even during the COVID-19 pandemic [
5,
18]. This resilience reflects the strong accessibility of the healthcare system, supported by universal insurance coverage, relatively low copayments (20%–30%), and widespread private insurance [
19,
20]. The increased proportion of ORIF and relative decline in nonoperative cases suggest that patients with more severe fractures continued to seek hospital care, while minor nondisplaced cases may have been treated at home or miscoded as other injuries. Consequently, the surgical proportion appeared to rise despite an overall reduction in emergency visits.
Regarding operative modalities, previous reports from South Korea have indicated an increasing trend in volar locking plate fixation [
21]. Consistently, this study found that the most common type of surgery for DRFs was ORIF, predominantly using an anatomic volar locking plate. The proportion of plate fixation increased from 77.8% before COVID-19 to 88.1% during COVID-19 (
Table 3). Interestingly, the proportion of plate fixation in Korea is higher than that reported in the United States and other countries [
22]. Although the use of external fixators for DRFs was already low before the COVID-19 pandemic (7.8%), it decreased even further during the pandemic period (3.7%).
Despite analyzing a large dataset from the NHIS-NSC repository, several limitations were unavoidable. First, while this study reported increased rates of surgical intervention before and during the COVID-19 pandemic, the reasons behind these changes remain unclear and cannot be fully explained. Second, bilateral injuries were not addressed in this study, which may have led to an underestimation of the incidence rate and other outcomes. Third, the nationwide nature of the data also meant that patient-reported outcomes or quality-of-life measures were unavailable, limiting the ability to assess the broader clinical impact of the observed management changes. Finally, as a nationwide observational study, this research does not provide specific treatment guidelines.
Clinical implications
Nevertheless, this study is the first attempt to identify changes in the incidence and treatment trends of DRFs before and during the COVID-19 pandemic in South Korea using a national database. The findings highlight the importance of reflecting on our experiences and preparing for unexpected crises, such as future pandemics. By learning from the challenges of the COVID-19 pandemic, we can develop more effective strategies to address the healthcare needs of vulnerable populations during similar crises in the future.
Generalizability
This nationwide claims-based study is likely generalizable to Korean adults aged 50 years and older who are covered by the National Health Insurance system, as the database captures virtually all reimbursed healthcare encounters at the population level. However, extrapolation to other countries should be approached with caution due to differences in population age structure, fracture risk profiles, healthcare access, reimbursement policies, and coding practices.
Conclusions
During the COVID-19 pandemic, the incidence of DRFs has decreased in South Korea. However, the rate of surgical treatment has increased, which is higher than the global surgical rate. While the decrease of incidence seems attributable to pandemic-related behavioral changes, the higher surgical proportion likely reflects preexisting national trends rather than a direct COVID-19 effect.
Article Information
-
Author contributions
Conceptualization: HKY, SC. Data curation: SRY, KBH, YJ, JKL. Funding: SC. Formal analysis: SRY, YJ. Project administration: SC. Supervision: JKL, SC. Writing-original draft: HKY, KBH, SC. Writing-review & editing: HKY, SRY, YJ, JKL, SC. All authors read and approved the final manuscript.
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
This work was supported by National Health Insurance Service Ilsan Hospital (Grant No. NHIMC-2023-CR-024).
-
Data availability
Contact the corresponding author for data availability.
-
Acknowledgments
None.
Supplementary material
Fig. 1.Schematic diagram depicting the study population.

Table 1.Characteristics of the general population by group: before and during COVID-19
|
Variable |
Group 1 (2017–2018) |
Group 2 (2020–2021) |
Total |
|
All |
37,844,101 (47.6) |
41,712,121 (52.4) |
79,556,222 (100) |
|
Sex |
|
|
|
|
Male |
17,821,359 |
19,705,470 |
37,526,829 (47.2) |
|
Female |
20,022,742 |
22,006,651 |
42,029,393 (52.8) |
|
Age (yr) |
|
|
|
|
50‒59 |
16,852,520 |
17,110,074 |
33,962,594 (42.7) |
|
60‒69 |
11,202,543 |
13,436,647 |
24,639,190 (31.0) |
|
70‒79 |
6,625,654 |
7,257,273 |
13,882,927 (17.5) |
|
≥80 |
3,163,384 |
3,908,127 |
7,071,511 (8.9) |
|
Residence |
|
|
|
|
Metropolis |
16,548,301 |
17,843,342 |
34,391,643 (43.2) |
|
Others |
21,295,800 |
23,872,219 |
45,168,019 (56.8) |
Table 2.Incidence rate per 100,000 population a year
|
Variable |
Group 1 (2017–2018) |
Group 2 (2020–2021) |
Total |
|
All |
184.43 |
169.83 |
176.77 |
|
Sex |
|
|
|
|
Male |
64.98 |
62.59 |
63.73 |
|
Female |
290.73 |
265.86 |
277.71 |
|
Age (yr) |
|
|
|
|
50‒59 |
100.55 |
83.94 |
92.19 |
|
60‒69 |
206.20 |
193.53 |
199.29 |
|
70‒79 |
279.04 |
244.51 |
260.99 |
|
≥80 |
355.95 |
325.68 |
339.22 |
|
Residence |
|
|
|
|
Metropolis |
173.96 |
164.50 |
169.05 |
|
Others |
192.56 |
173.79 |
182.64 |
Table 3.Operation rate and details of surgical techniques
|
Variable |
Group 1 (2017–2018) |
Group 2 (2020–2021) |
Total |
|
All |
69,794 (100) |
70,840 (100) |
140,634 (100) |
|
Surgery |
|
|
|
|
No |
11,648 (16.7) |
9,288 (13.1) |
20,936 (14.9) |
|
Yes |
58,146 (83.3) |
61,552 (86.9) |
119,698 (85.1) |
|
Type of surgery |
58,146 (100) |
61,552 (100) |
119,698 (100) |
|
OR + plating |
45,226 (77.8) |
54,209 (88.1) |
99,435 (83.1) |
|
N0603 |
462 (0.8) |
15 (0.0) |
477 (0.3) |
|
N0607 |
5,526 (9.5) |
50 (0.1) |
5,576 (4.7) |
|
N0613 |
431 (0.7) |
12 (0.0) |
443 (0.4) |
|
N0617 |
4,004 (6.9) |
5 (0.0) |
4,009 (3.4) |
|
N1601 |
16,653 (28.6) |
20,825 (33.8) |
37,478 (31.3) |
|
N1603 |
1,247 (2.1) |
1,652 (2.7) |
2,899 (2.4) |
|
N1611 |
15,491 (26.6) |
29,019 (47.2) |
44,510 (37.2) |
|
N1613 |
1,412 (2.4) |
2,631 (4.3) |
4,043 (3.4) |
|
CR + pinning |
8,414 (14.5) |
5,076 (8.3) |
13,490 (11.3) |
|
N0993 |
2,131 (3.7) |
9 (0.0) |
2,140 (1.8) |
|
N0994 |
252 (0.4) |
1 (0.0) |
253 (0.2) |
|
N0996 |
5,518 (9.5) |
4,582 (7.4) |
10,100 (8.4) |
|
N0998 |
513 (0.9) |
484 (0.8) |
997 (0.8) |
|
External fixator |
4,506 (7.8) |
2,267 (3.7) |
6,773 (5.7) |
|
N0983 |
4,506 (7.8) |
2,267 (3.7) |
6,773 (5.7) |
Table 4.Comparison of patients with distal radius fracture between groups
|
Variable |
Group 1 (2017–2018) |
Group 2 (2020–2021) |
Total |
|
All |
69,794 (49.6) |
70,840 (50.4) |
140,634 (100) |
|
Year |
|
|
|
|
2017 |
34,605 (49.6) |
- |
34,605 (24.6) |
|
2018 |
35,189 (50.4) |
- |
35,189 (25.0) |
|
2020 |
- |
33,816 (47.7) |
33,816 (24.0) |
|
2021 |
- |
37,024 (52.3) |
37,024 (26.3) |
|
Sex |
|
|
|
|
Male |
11,581 (16.6) |
12,333 (17.4) |
23,914 (17.0) |
|
Female |
58,213 (83.4) |
58,507 (82.6) |
116,720 (83.0) |
|
Mean age (yr) |
68.1±10.2 |
68.7±10.8 |
68.4±10.2 |
|
Age (yr) |
|
|
|
|
50‒59 |
16,946 (24.3) |
14,363 (20.3) |
31,309 (22.3) |
|
60‒69 |
23,100 (33.1) |
26,004 (36.7) |
49,104 (34.9) |
|
70‒79 |
18,488 (26.5) |
17,745 (25.0) |
36,233 (25.8) |
|
≥80 |
11,260 (16.1) |
12,728 (18.0) |
23,988 (17.1) |
|
Income |
|
|
|
|
1 (lowest) |
4,151 (5.9) |
4,078 (5.8) |
8,229 (5.9) |
|
2 |
13,670 (19.6) |
13,855 (19.6) |
27,525 (19.6) |
|
3 |
14,604 (20.9) |
15,446 (21.8) |
30,050 (21.4) |
|
4 |
21,103 (30.2) |
20,885 (29.5) |
41,988 (29.9) |
|
5 (highest) |
16,266 (23.3) |
16,576 (23.4) |
32,842 (23.4) |
|
Residence |
|
|
|
|
Metropolis |
28,787 (41.2) |
29,353 (41.4) |
58,140 (41.3) |
|
Others |
41,007 (58.8) |
41,487 (58.6) |
82,494 (58.7) |
|
Surgery |
|
|
|
|
Yes |
58,146 (83.3) |
61,552 (86.9) |
119,698 (85.1) |
|
Death within 1 year |
|
|
|
|
Yes |
923 (1.3) |
1,000 (1.4) |
1,923 (1.4) |
|
CCI score |
|
|
|
|
0 |
16,340 (23.4) |
18,242 (25.8) |
34,582 (24.6) |
|
1 |
20,284 (29.1) |
19,798 (27.9) |
40,082 (28.5) |
|
2 |
14,778 (21.2) |
14,366 (20.3) |
29,144 (20.7) |
|
3 |
8,499 (12.2) |
8,524 (12.0) |
17,023 (12.1) |
|
4 |
4,957 (7.1) |
5,033 (7.1) |
9,990 (7.1) |
|
≥5 |
4,936 (7.1) |
4,877 (6.9) |
9,813 (7.0) |
References
- 1. Baek YH, Cho SW, Jeong HE, et al. 10-Year fracture risk in postmenopausal women with osteopenia and osteoporosis in South Korea. Endocrinol Metab (Seoul) 2021;36:1178-88.ArticlePubMedPMCPDF
- 2. Ruch DS, McQueen MM. Distal radius and ulna fractures. In: Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P, McKee MD, editors. Rockwood and Green’s fractures in adults. 8th ed. Lippincott Williams & Wilkins; 2015. p. 1229-86.
- 3. Wolfe SW. Distal radius fractures. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS, editors. Green’s operative hand surgery. 7th ed. Elsevier; 2017. p. 516-87.
- 4. Mallmin H, Ljunghall S. Incidence of Colles’ fracture in Uppsala: a prospective study of a quarter-million population. Acta Orthop Scand 1992;63:213-5.ArticlePubMed
- 5. Viberg B, Tofte S, Rønnegaard AB, Jensen SS, Karimi D, Gundtoft PH. Changes in the incidence and treatment of distal radius fractures in adults: a 22-year nationwide register study of 276,145 fractures. Injury 2023;54:110802.ArticlePubMed
- 6. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan 2009;24:63-71.ArticlePubMed
- 7. Noordzij M, Dekker FW, Zoccali C, Jager KJ. Measures of disease frequency: prevalence and incidence. Nephron Clin Pract 2010;115:c17-20.ArticlePubMedPDF
- 8. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83.ArticlePubMed
- 9. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006;37:691-7.ArticlePubMed
- 10. Sigurdardottir K, Halldorsson S, Robertsson J. Epidemiology and treatment of distal radius fractures in Reykjavik, Iceland, in 2004: comparison with an Icelandic study from 1985. Acta Orthop 2011;82:494-8.ArticlePubMedPMC
- 11. Poggetti A, Del Chiaro A, Nucci AM, Suardi C, Pfanner S. How hand and wrist trauma has changed during COVID-19 emergency in Italy: incidence and distribution of acute injuries. What to learn. J Clin Orthop Trauma 2021;12:22-6.Article
- 12. Turgut A, Arlı H, Altundağ Ü, Hancıoğlu S, Egeli E, Kalenderer Ö. Effect of COVID-19 pandemic on the fracture demographics: data from a tertiary care hospital in Turkey. Acta Orthop Traumatol Turc 2020;54:355-63.ArticlePubMedPMC
- 13. Kwon GD, Jang S, Lee A, et al. Incidence and mortality after distal radius fractures in adults aged 50 years and older in Korea. J Korean Med Sci 2016;31:630-4.ArticlePubMedPMCPDF
- 14. Wilcke MK, Hammarberg H, Adolphson PY. Epidemiology and changed surgical treatment methods for fractures of the distal radius: a registry analysis of 42,583 patients in Stockholm County, Sweden, 2004-2010. Acta Orthop 2013;84:292-6.ArticlePubMedPMC
- 15. Hevonkorpi TP, Launonen AP, Huttunen TT, Kannus P, Niemi S, Mattila VM. Incidence of distal radius fracture surgery in Finns aged 50 years or more between 1998 and 2016: too many patients are yet operated on? BMC Musculoskelet Disord 2018;19:70.ArticlePubMedPMCPDF
- 16. Hong KB, Oh CH, Lim CK, Lee S, Han SH, Lee JK. Does the operator’s experience affect the occurrence of complications after distal radius fracture volar locking plate fixation?: a comparative study of the first four years and thereafter. J Musculoskelet Trauma 2024;37:175-83.ArticlePDF
- 17. He LD, Duggan JL, Lans J, Harper CM, Rozental TD. Trends in orthopedic management of distal radius fractures among Medicare beneficiaries from 2019 to 2020: a claims analysis. J Hand Surg Glob Online 2023;5:717-21.ArticlePubMedPMC
- 18. Azad A, Kang HP, Alluri RK, Vakhshori V, Kay HF, Ghiassi A. Epidemiological and treatment trends of distal radius fractures across multiple age groups. J Wrist Surg 2019;8:305-11.ArticlePubMedPMC
- 19. Lee H, Hwang SH, Park CS, et al. An epidemic of cataract surgery in Korea: the effects of private health insurance on the National Health Insurance Service. Epidemiol Health 2024;46:e2024015. ArticlePubMedPMCPDF
- 20. Park S, Kim K, Callison K. Supplementary private health insurance and household debt, health care utilization, and medical spending following a health Shock. Int J Soc Determinants Health Health Serv 2025;55:187-98.ArticlePubMedPDF
- 21. Lee JH, Lee JK, Park JS, et al. Complications associated with volar locking plate fixation for distal radius fractures in 1955 cases: a multicentre retrospective study. Int Orthop 2020;44:2057-67.ArticlePubMedPDF
- 22. Kakar S, Noureldin M, Van Houten HK, Mwangi R, Sangaralingham LR. Trends in the incidence and treatment of distal radius fractures in the United States in privately insured and Medicare advantage enrollees. Hand (N Y) 2022;17:331-8.ArticlePubMedPDF
 , So Ra Yoon3
, So Ra Yoon3 , Kee-Bum Hong1,2
, Kee-Bum Hong1,2 , Youngsu Jung1,2
, Youngsu Jung1,2 , SeongJu Choi4
, SeongJu Choi4 , Jun-Ku Lee1,2
, Jun-Ku Lee1,2


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 ePub Link
ePub Link Cite
Cite

