Abstract
-
Background
Achieving stable fixation that enables early ambulation is essential but remains challenging because complex intertrochanteric (IT) fracture patterns are often underestimated on plain radiographs. Herein, we analyzed whether the anterior fracture line lies medial or lateral to the IT line and examined its relationship with displacement or distal medullary canal engagement.
-
Methods
A retrospective review was conducted on 96 osteoporotic IT fractures in patients aged ≥60 years treated between April 2013 and December 2022 at National Police Hospital and Asan Medical Center, Seoul, Korea. Fractures were classified as engaged, completely displaced, and partially displaced based on three-dimensional computed tomography findings. The anterior fracture-line position (medial or lateral to the IT line) and the status of the lesser trochanter (LT) were evaluated. The chi-square or Fisher exact test was used for statistical comparisons.
-
Results
In total, 96 patients were analyzed. Of these, 49 cases (51.0%) were classified as engaged type, 27 cases (28.1%) as completely displaced type, and 20 cases (20.8%) as partially displaced type. When comparing fracture pattern with anterior fracture-line position, the completely displaced type showed a significantly higher proportion of lateral anterior fracture lines than the other two types (P<0.001). However, no significant association was identified between fracture pattern and LT displacement. When the anterior fracture-line position and LT displacement were evaluated together, only the engaged type demonstrated a possible association between a lateral anterior fracture line and LT displacement (P=0.047).
-
Conclusions
Fracture lines lateral to the IT line were strongly associated with displacement in IT fractures; however, their relationship with LT involvement, reflecting iliopsoas tendon traction, was not clearly demonstrated. Although the factors contributing to the engaged-type fracture remain uncertain, the statistical association between fracture pattern and anterior fracture-line position suggests that capsular structures may play a stabilizing role in select fracture configurations.
-
Level of evidence
III, retrospective study.
-
Keywords: Hip fractures, X-ray computed tomography, Femur, Tendons
Introduction
Background
With the advent of an aging society, the prevalence of osteoporosis and the incidence of osteoporotic hip fractures have imposed a significant socioeconomic burden. According to recent Korean national data, the incidence of osteoporotic hip fractures increased by 138% between 2006 and 2010, and as of 2021, the 1-year mortality rate following hip fracture reached 18.2% [
1], which is the highest among all osteoporotic fractures.
To prevent mortality and frequent postoperative complications associated with osteoporotic hip fractures, early postoperative ambulation is considered crucial [
2]. A prerequisite for early ambulation is stable fracture fixation [
3]. Achieving stable fixation requires an accurate understanding of fracture morphology, including the degree of comminution and displacement, and the selection of an appropriate internal fixation device.
Although the design and performance of internal fixation devices for osteoporotic fractures have improved over time, mechanical complications, such as lag screw cut-out or cut-through of the femoral head [
4], resulting in fixation failure, remain unresolved. One major contributor to these complications is an insufficient understanding of fracture morphology [
5]. In particular, intertrochanteric (IT) fractures are prone to fixation failure when treated without a precise understanding of the fracture pattern. Despite these limitations, many surgeons still rely primarily on plain radiographs for the diagnosis and classification of IT fractures. However, in many cases, additional fracture fragments not visible on X-rays can often be identified only using computed tomography (CT).
Current classification systems for IT fractures are largely based on plain radiographs and, therefore, do not fully capture the complexity of fracture morphology. This limitation may be partly attributable to the influence of the joint capsule and capsular ligaments. In South Korea, although CT scans have become more widely used for the diagnosis of IT fractures compared to the past, supporting evidence for the relationship with the joint capsule and capsular ligaments remains insufficient.
This study focused on two IT fracture patterns that have recently gained attention: the canal engagement and displaced types [
5,
6]. Anatomically, the joint capsule attaches to the mid-portion of the femoral neck posteriorly, whereas anteriorly, the capsular ligaments, such as the iliofemoral ligament, are relatively thick and long, attaching to the IT line. Although IT fractures are considered extra-articular, if the anterior fracture line lies proximal to the IT line, the capsule may remain attached to the distal fragment, rendering the anterior portion of the fracture intra-articular in nature. In such cases, the intact capsule may resist displacement of the proximal fragment, potentially leading to varus deformity and engagement of the inferior beak into the medullary canal of the distal fragment.
This study aimed to assess, using three-dimensional (3D)-CT, whether the anterior part of an IT fracture lies medial (superior) or lateral (inferior) to the IT line, and to investigate the relationship between this anatomical location and the presence of displacement or canal engagement patterns. This analysis was also used to indirectly evaluate the potential role of the joint capsule and capsular ligaments in influencing fracture displacement.
Methods
Ethics statement
This study was approved by the Institutional Review Board (IRB) Ethics Committee of National Police Hospital (IRB No. 11100176-202507-HR-002). The requirement for informed patient consent was waived owing to the retrospective nature of the study, and all analyses were conducted using anonymized clinical data.
Study design and setting
It is a cross-sectional study. This study was conducted at National Police Hospital and Asan Medical Center, Seoul, Korea and included patients who underwent surgery for IT fractures performed by a single surgeon between April 2013 and December 2022.
Participants
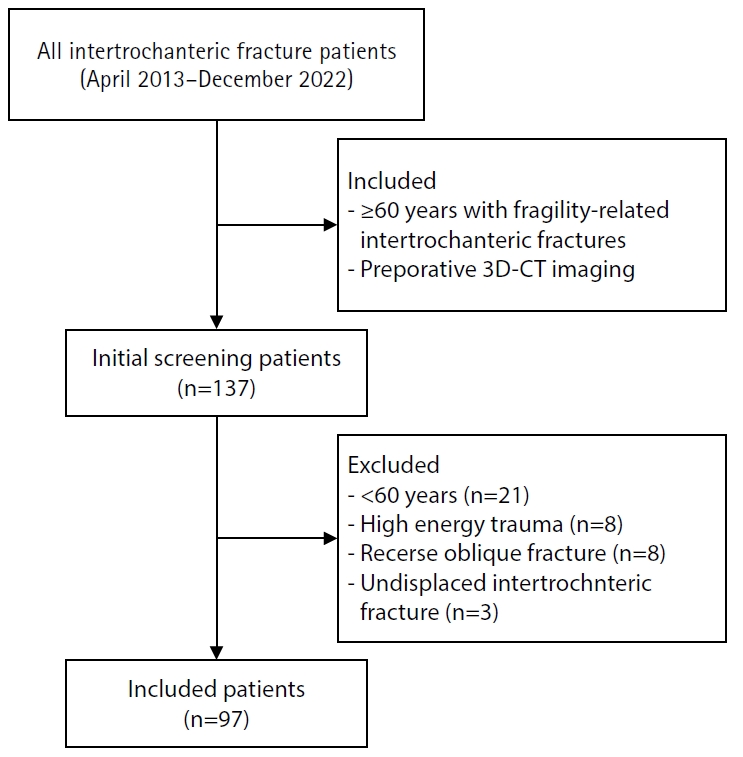
Inclusion criteria were as follows: (1) patients aged ≥60 years with fragility-related IT fractures, and (2) availability of preoperative 3D-CT imaging. The exclusion criteria were as follows: (1) patients aged <60 years (n=21), (2) fractures resulting from high-energy trauma with severe comminution that made definition of the main fracture pattern difficult (n=8), (3) reverse oblique type fractures (n=8), and (4) undisplaced IT fractures (n=3). An initial screening identified 136 patients; applying the exclusion criteria, 96 hips in 96 patients met the inclusion criteria and were included in the analysis. The patient selection process is illustrated in
Fig. 1.
The primary outcome was the CT-based displacement pattern, categorized into three groups: engaged type, completely displaced type, and partially displaced type. The primary exposure was the position of the anterior fracture line relative to the IT line, categorized as medial or lateral according to its location on 3D-CT. The secondary exposure was the displacement status of the lesser trochanter (LT), categorized as intact or displaced on 3D-CT. Baseline covariates included age, sex, body mass index (BMI), and bone mineral density (BMD) T-score at admission, when available from dual-energy X-ray absorptiometry.
Data sources/measurement
Based on 3D-CT scans obtained from all 96 patients, previously established concepts of intramedullary and extramedullary positions of the proximal fracture fragment [
7,
8] were expanded to classify IT fractures into three types according to the location of the proximal head fragment: (1) engaged, (2) completely displaced, and (3) partially displaced.
The engaged type was defined as fractures in which the proximal head fragment was completely embedded into the medullary canal of the distal fracture part. The completely displaced type referred to fractures in which the proximal fragment was entirely outside the medullary canal. The partially displaced type represented an intermediate stage, where the inferomedial part of the fracture line showed minimal displacement, but the proximal portion was visibly displaced. Representative images of these types are presented in
Fig. 2.
Following classification by 3D-CT, each fracture was further subcategorized based on (1) the position of the anterior fracture line and (2) the displacement status of the LT.
The IT line, defined as a bony ridge on the femur that extends anteriorly over the neck of the femur [
9], was identified on 3D-CT imaging in this study. For the anterior fracture line, its position relative to the IT line was used as the criterion: if the fracture line was located medial to the IT line, it was classified as the medial type, and if it was located lateral to the line, it was classified as the lateral type. Representative examples of these types are illustrated in
Fig. 3.
Restricting inclusion to cases with preoperative 3D-CT may select for patients with more complex fractures. This selection bias was mitigated by screening consecutive surgical cases over a defined period and applying exclusion criteria.
Study size
No formal a priori sample size calculation was performed because the study was exploratory and based on available retrospective imaging data.
Statistical analysis
Categorical variables, including the location of the anterior fracture line (medial vs. lateral to the IT line) and the status of the LT (intact vs. displaced), were compared among the three displacement groups (engaged, completely displaced, and partially displaced). The overall (omnibus) comparison across the three groups was conducted using the Pearson chi-square test. When the omnibus test was significant, pairwise 2×2 Fisher exact tests were performed with Bonferroni adjustment for multiple comparisons (adjusted α=0.0167). Effect sizes were reported as odds ratios (95% confidence intervals) and Cramer’s V for the omnibus association. Analyses were conducted using R ver. 4.3.2 (R Foundation for Statistical Computing) with the rcompanion and epitools packages. Statistical significance was defined as two-tailed P<0.05 (or Bonferroni-adjusted threshold for pairwise tests).
Results
Participants’ characteristics
As for the baseline demographics, women were dominant, accounting for 72 of the 96 patients, and the mean age was 84.6 years. A total of 96 patients were analyzed: 49 cases (51.0%) were classified as the engaged type, 27 cases (28.1%) as the completely displaced type, and 20 cases (20.8%) as the partially displaced type. Additional demographic details are presented in
Table 1.
First, in the analysis of whether the position of the anterior fracture line differed significantly among the three fracture types, a significant difference was found in the distribution of anterior fracture-line location across the displacement groups (χ²=14.27, df=2, P<0.001). Subsequent pairwise post-hoc testing revealed that the completely displaced group had a markedly higher proportion of lateral anterior fracture lines (81.5%) compared with the engaged (44.9%, adjusted P=0.010) and partially displaced groups (30.0%, adjusted P=0.002) (
Table 2).
In contrast, neither the overall comparison nor the pairwise comparisons demonstrated any significant association between fracture pattern and LT displacement. Detailed statistical results are presented in
Table 3.
Finally, when the anterior fracture-line position and LT displacement were analyzed together in relation to the fracture pattern (
Table 4), no significant associations were observed in any of the groups except for the engaged type, where a lateral anterior fracture line showed a significant relationship with LT displacement (P=0.047).
Discussion
Key results
The findings revealed that in completely displaced IT fractures, the anterior fracture line was located significantly more lateral to the IT line. This indicates that extracapsular fractures are less likely to become engaged and are more prone to displacement. When both the anterior fracture line position and LT displacement were considered together, cases in which the anterior fracture line was lateral to the IT line and accompanied by LT displacement were significantly more frequent in the engaged type (P=0.047). This suggests that even when the fracture line is located laterally, displacement of the LT may eliminate structural support for the fracture fragment, thereby allowing engagement to occur.
Conversely, the present study failed to demonstrate a statistically significant association between the presence of LT displacement and fracture pattern, failing to support the hypothesis that the iliofemoral ligament plays a decisive role in determining fracture morphology. This represents a limitation of the current study, and further investigations are warranted to clarify these findings.
Interpretation/comparison with previous studies
The proportion of IT fractures in the elderly is increasing globally. For instance, in the United Kingdom, hip fractures increased by 7% between 2020 and 2023 [
10], whereas in Germany, hip fractures accounted for 22% of all fractures among elderly individuals in 2019 [
11]. Mortality associated with these fractures remains high, with 5%–10% of patients dying within 1 month and 33% within 1 year. Furthermore, only approximately one-third of affected individuals regain their preinjury level of activity [
12].
Early ambulation is crucial for achieving a favorable prognosis, with stable fixation serving as the primary determinant of early mobilization. Despite improvements in surgical techniques and implant designs, fixation failure continues to occur in 5%–20% of cases [
13].
Understanding fracture morphology is essential for achieving successful fixation, with increasing emphasis on extramedullary reduction and anteromedial cortical support [
14]. Existing IT fracture classifications are primarily morphology-based and do not account for displacement. These fractures can be further categorized into nondisplaced, engaged, and completely displaced types according to the degree of displacement.
While displaced types are known to result from factors such as iliopsoas muscle and external rotation, the mechanism underlying engaged-type fractures remains unclear until now. This study hypothesized that the joint capsule, pericapsular ligaments—particularly the iliofemoral ligament—and the iliopsoas tendon influence displacement patterns in IT fractures.
According to a previous study by Chandak et al. [
15], it has been suggested that, in irreducible severe IT fractures, the iliopsoas tendon may influence both displacement and reduction. They reported that the distal end of the proximal fragment in an IT fracture can become entrapped by the iliopsoas tendon, thereby preventing closed reduction. This implies that the distal portion of the proximal fragment lies in very close proximity to the iliopsoas tendon. In the current study as well, among progressively displaced fractures, partially displaced cases with an intact lesser trochanter showed a clear predominance of fracture lines located medial to the IT line compared with those located laterally (
Table 4). This finding may suggest a possible role of the capsular ligament and iliopsoas tendon in limiting further displacement of the fracture. It is hypothesized that these soft-tissue structures could help prevent complete separation while varus angulation of the proximal fragment leads to partial displacement into the medullary canal (
Fig. 4). Conversely, in fractures with a similar pattern but with complete displacement, it can be assumed that rupture of the capsular ligament has occurred. Moreover, our results showed that completely displaced types were often located lateral to the IT line, that is, in extracapsular fractures, suggesting that the iliofemoral ligament and anterior capsule may contribute to fracture displacement.
Recently, the cephalomedullary nail has become the most preferred treatment method for IT fractures [
16]. In most cases, cephalomedullary nails are inserted after closed reduction, which offers the advantages of relatively shorter operative time and reduced blood loss. During reduction, intramedullary reduction should be strictly avoided, and slight overcorrection to achieve extramedullary reduction is recommended whenever possible [
7,
8]. However, in engaged-type fractures where the capsular ligament remains attached to the distal fragment, obtaining anatomical reduction using the capsule and capsular ligament is not particularly difficult, but achieving overcorrection for extramedullary reduction can be technically very challenging. In such cases, based on the author’s experience, performing open reduction with capsulotomy can facilitate extramedullary reduction. Therefore, it is important to evaluate the positional relationship between the capsule, capsular ligament, and fracture line preoperatively to plan the surgical approach. Although magnetic resonance imaging (MRI) was not performed in this study, future research on engaged-type fractures should consider preoperative MRI to assess the condition of the capsular ligament.
Our study has several limitations. First, the sample size was relatively small. In addition, because this study was designed to identify specific factors influencing fracture patterns, cases that were excessively unstable or severely comminuted, making it difficult to determine the origin or main fracture line, were excluded from the analysis. Finally, the absence of magnetic resonance imaging limited our ability to more strongly validate the proposed hypothesis. Future studies are planned to address these limitations.
Generalizability
Generalizability is primarily limited to adults aged 60 years and older with fragility IT fractures treated operatively in settings where preoperative 3D-CT and similar classification methods are utilized. External validity may be constrained by the inclusion of only two hospitals and a single-surgeon cohort, as well as by exclusions such as high-energy trauma, reverse oblique, undisplaced, or severely comminuted fractures.
Conclusions
Fracture lines lateral to the IT line were strongly associated with displacement in IT fractures; however, their relationship with LT involvement—representing iliopsoas tendon traction—was not clearly demonstrated. Although the factors influencing the engaged-type fracture remain inconclusive, the statistical association between fracture pattern and anterior fracture-line position suggests that the capsular structures may contribute to stability in select fracture configurations. Further studies are warranted to clarify these anatomical interactions.
Article Information
-
Author contributions
Conceptualization: JSC, CHK. Data curation: SOK, CHK. Formal analysis: JYP, CHK. Investigation: JYP, SOK. Supervision: JSC. Visualization: JYP, SOK. Writing-original draft: JSC, CHK. Writing-review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
None.
-
Data availability
Contact the corresponding author for data availability.
-
Acknowledgments
None.
-
Supplementary materials
None.
Fig. 1.Flowchart of patient selection. 3D-CT, three-dimensional computed tomography.

Fig. 2.Representative three-dimensional computed tomography images of intertrochanteric fractures: (A) engaged type, (B) completely displaced type, and (C) partially displaced type.

Fig. 3.Definition of the anterior fracture line. Based on the intertrochanteric line (yellow dotted line), representative examples are shown of fractures located (A) medial and (B) lateral to the line.

Fig. 4.Schematic illustration of the mechanism through which the iliopsoas tendon contributes to engagement of the proximal fragment.

Table 1.
|
Characteristic |
Value |
|
Patient (hip) |
96 (96 hips) |
|
Sex (male:female) |
24 (25):72 (75) |
|
Age (yr) |
84.6±11.2 |
|
BMI (kg/m2) |
22.5±2.7 |
|
T-score of BMD at admission period |
‒2.8±1.1 |
|
Fracture type |
|
|
Engaged |
49 (51.0) |
|
Partially displaced |
20 (20.8) |
|
Completely displaced |
27 (28.1) |
Table 2.Distribution of anterior fracture-line location (medial vs. lateral) according to the fracture type
|
Fracture type |
Medial |
Lateral |
Row % lateral |
Total |
|
Engaged |
27 |
22 |
44.9 |
49 |
|
Completely displaced |
5 |
22 |
81.5 |
27 |
|
Partially displaced |
14 |
6 |
30.0 |
20 |
|
Total |
46 |
50 |
NA |
96 |
Table 3.Lesser trochanter displacement following fracture type
|
Fracture group |
LT intact |
LT displaced |
Row % displaced |
Total |
|
Engaged |
21 |
28 |
57.1 |
49 |
|
Completely displaced |
13 |
14 |
51.9 |
27 |
|
Partially displaced |
14 |
6 |
30.0 |
20 |
|
Total |
48 |
48 |
NA |
96 |
Table 4.The relationship between the combined anterior fracture line position and lesser trochanter (LT) displacement with the fracture pattern
|
Group |
Medial+intact |
Medial+displaced |
Lateral+intact |
Lateral+displaced |
Total |
|
Engaged |
16 |
11 |
5 |
17 |
49 |
|
Completely displaced |
3 |
2 |
10 |
12 |
27 |
|
Partially displaced |
11 |
3 |
3 |
3 |
20 |
References
- 1. Chung H, Kim TY, Kim J, et al. Long-term trends of osteoporotic hip fractures in South Korea: analysis of National Health Insurance Data from 2006 to 2022. Osteoporos Int 2025;36:1999-2007.ArticlePubMedPDF
- 2. Lee KJ, Um SH, Kim YH. Postoperative rehabilitation after hip fracture: a literature review. Hip Pelvis 2020;32:125-31.ArticlePubMedPMCPDF
- 3. Alito A, Fenga D, Portaro S, et al. Early hip fracture surgery and rehabilitation: how to improve functional quality outcomes: a retrospective study. Folia Med (Plovdiv) 2023;65:879-84.ArticlePubMedPDF
- 4. Esper GW, Fisher ND, Anil U, Ganta A, Konda SR, Egol KA. Cut-through versus cut-out: no easy way to predict how single lag screw design cephalomedullary nails used for intertrochanteric hip fractures will fail. Hip Pelvis 2023;35:175-82.ArticlePubMedPMCPDF
- 5. Ryu HG, Shin DW, Han BS, Kim SM. Risk factors associated with fixation failure in intertrochanteric fracture treated with cephalomedullary nail. Hip Pelvis 2023;35:193-9.ArticlePubMedPMCPDF
- 6. Kim CH, Kim HS, Moon DH. Additional reduction screw fixation technique for pertrochanteric hip fractures: a novel method to prevent excessive sliding in cephalomedullary nail surgery. Hip Pelvis 2021;33:162-6.ArticlePubMedPMCPDF
- 7. Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg 2015;135:811-8.ArticlePubMedPMCPDF
- 8. Lim EJ, Sakong S, Son WS, Cho JW, Oh JK, Kim CH. Comparison of sliding distance of lag screw and nonunion rate according to anteromedial cortical support in intertrochanteric fracture fixation: a systematic review and meta-analysis. Injury 2021;52:2787-94.ArticlePubMed
- 9. Kumar R, Pal AK, Keshkar S. Intertrochanteric fracture: relevant anatomy and classification. Int J Orthop Surg 2022;30:39-44.
- 10. Webster J, Oguzman E, Morris EJ, et al. Trends and variation in the incidence of hip fracture in England before, during, and after the COVID-19 pandemic (2014-2024): a population-based observational study. Lancet Reg Health Eur 2025;57:101427.ArticlePubMedPMC
- 11. Werner M, Macke C, Gogol M, Krettek C, Liodakis E. Differences in hip fracture care in Europe: a systematic review of recent annual reports of hip fracture registries. Eur J Trauma Emerg Surg 2022;48:1625-38.ArticlePubMedPMCPDF
- 12. Graulich T, Omar M, Sehmisch S, Liodakis E. Controversies in the treatment strategies of intertrochanteric fractures: a scoping review and discussion of a literature-based algorithm. J Clin Med 2025;14:2200.ArticlePubMedPMC
- 13. Yoo J, Chang J, Park C, Hwang J. Risk factors associated with failure of cephalomedullary nail fixation in the treatment of trochanteric hip fractures. Clin Orthop Surg 2020;12:29-36.ArticlePubMedPMCPDF
- 14. Mao W, Liu CD, Chang SM, Yang AL, Hong CC. Anteromedial cortical support in reduction of trochanteric hip fractures: from definition to application. J Bone Joint Surg Am 2024;106:1008-18.PubMed
- 15. Chandak R, Malewar N, Jangle A, Agarwal R, Sharma M, Kekatpure A. Description of new “epsilon sign” and its significance in reduction in highly unstable variant of intertrochanteric fracture. Eur J Orthop Surg Traumatol 2019;29:1435-9.ArticlePubMedPDF
- 16. Suh YS, Nho JH, Song MG, Lee DW, Jang BW. Midterm outcomes of intramedullary fixation of intertrochanteric femoral fractures using compression hip nails: radiologic and clinical results. Clin Orthop Surg 2023;15:373-9.ArticlePubMedPMCPDF
 , Jin Yeob Park2
, Jin Yeob Park2 , Sang-Ok Chun1
, Sang-Ok Chun1 , Chul-Ho Kim2
, Chul-Ho Kim2








 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 ePub Link
ePub Link Cite
Cite

