Abstract
-
Background
Volar plate avulsion fractures in phalanges are relatively common injuries. While surgical treatment can help reduce limitations in motion after injury, the small size of the fracture fragment can make the procedure challenging. In this study, we used hook plate fixation as a surgical technique for treating volar avulsion fractures in phalanges and evaluated its radiological and clinical outcomes.
-
Methods
The medical records of eight patients (nine digits) with volar plate avulsion fractures of the middle phalanx were retrospectively reviewed. All fractures were treated with a 1.5-mm hook plate after open reduction. Radiologic evaluations were performed using simple radiographs, and clinical outcomes were assessed through range of motion, instability, and pain.
-
Results
The mean follow-up period was 4.9 months (range, 1–9 months). All nine digits achieved bone union at the final follow-up. The mean union time was 2.2 months (range, 1–4 months). In all patients, the range of motion in the proximal interphalangeal joint was 85° (range, 70°–100°) before implant removal and 89.4° (range, 80°–100°) after implant removal. All patients demonstrated no joint instability and no residual pain.
-
Conclusions
Using a hook plate for volar plate avulsion fractures presents a promising alternative to existing fixation methods. Its biomechanical advantages and ease of fabrication make it a valuable tool in hand surgery.
-
Level of evidence
IV.
-
Keywords: Fingers, Fracture fixation, Bone plate, Range of motion, Follow-up study
Introduction
Background
Volar plate avulsion fractures of the proximal interphalangeal (PIP) joint are relatively common injuries caused by hyperextension or axial loading, frequently observed in athletes and younger individuals engaged in contact sports [
1,
2]. Although many of these injuries can be managed conservatively, unstable fractures involving larger fragments or joint subluxation often require surgical fixation to restore joint congruity and prevent long-term stiffness, chronic pain, and functional impairment [
3].
Several surgical techniques have been introduced, including tension band wiring, screw fixation, mini-plates, and suture anchor methods [
4-
6]. However, fixation of small or comminuted fragments remains technically demanding, and inadequate fixation may lead to loss of reduction or limited range of motion (ROM) [
7,
8]. Recently, hook plates have been proposed as an alternative fixation method that can effectively convert tensile forces of the volar plate into compressive forces across the fracture site, ensuring rigid fixation even in small fragment cases [
3,
4]
This study aimed to evaluate the surgical outcomes of volar plate avulsion fractures by retrospectively reviewing the medical records. The findings will provide valuable insights into the surgical management of volar plate avulsion fractures, specifically focusing on the utilization of hook plates. This study can guide clinical decision-making and improve patient outcomes in the treatment of volar plate avulsion fractures.
Methods
Ethics statement
We conducted this study in compliance with the principles of the Declaration of Helsinki. This study was approved by the Institutional Review Board (IRB) Committees of the Medical Research Institute of Kyungpook National University Hospital (IRB No. KNUH 2023-05-035) and Samsung Changwon Hospital, Sungkyunkwan University School of Medicine (IRB No. SCMC 2023-05-016).
Study design and setting
This study is a case series. The medical records of patients in two centers who underwent open reduction and internal fixation using a hook plate at the phalanx from 2013 to 2020 were retrospectively reviewed.
The surgical indication for using the hook plate technique is displaced volar avulsion fracture of the phalangeal bones, which cause instability or extension lag. A large fragment with ROM limitation is also a surgical indication.
The surgical procedure was similar to that described by Kang et al. [
3] and Thirumalai et al. [
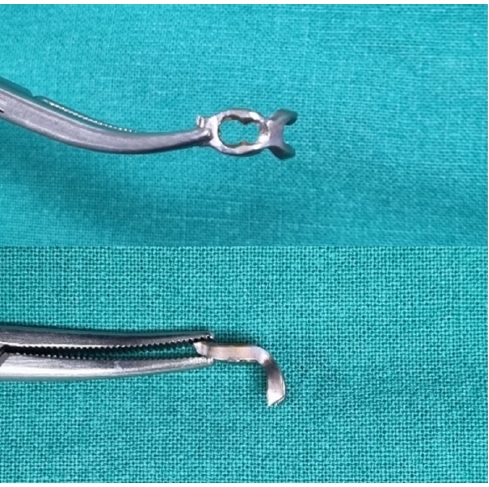
4]. All procedures were performed under general or regional anesthesia. A volar Bruner or zigzag incision was made to expose the PIP joint. The flexor tendon was retracted, and the volar plate was identified between the flexor tendons and the collateral ligament. The fracture fragment was visualized and meticulous dissection was performed to preserve soft-tissue attachments and vascularity. The hook plate was fabricated from a 1.5-mm modular hand system titanium plate (Synthes). A two- or three-hole plate was modified into a hook plate depending on the requirement. The cut ends of the plate were bent into hooks (
Fig. 1). Anatomical reduction of the fracture fragment was successfully achieved using the hook plates (
Fig. 2). Subsequently, the hooks were passed through these slips around the edge of the joint at the distal edge of the fracture fragment. They grabbed onto the lip of the articular surface in an area that does not interfere with joint function. Then, the hooks were used to control and reduce the fracture fragment. A 0.9-mm K-wire could be used to help reduce and hold the fracture fragment temporarily while applying the plate. The plate crossed the fracture line and was fixed with a single screw distal to the fracture (
Fig. 3). Fixation stability was confirmed by passively moving the joint through a full passive ROM under C-arm fluoroscopy. After surgery, the finger was immobilized in a functional position using a dorsal blocking splint for one week. Gradual active and passive ROM exercises were initiated thereafter under protective splinting, and unrestricted use was permitted after radiographic confirmation of bone union.
Once both clinical and radiographic union were confirmed, implant removal was recommended. Implant removal was routinely performed after confirming bone union, and the removal timing was considered equivalent to the time of union. Removal was recommended for all patients, but one patient declined secondary surgery. After bone union was achieved, the plate was removed (
Fig. 4).
Patients with avulsion fracture at the middle phalanx were included. After excluding patients with dorsal and lateral avulsion fractures, nine volar plate avulsion fractures in eight patients were included. Inclusion criteria were displaced volar avulsion fractures of the middle phalanx with clinical instability or motion limitation. Exclusion criteria included dorsal or lateral avulsion fractures, comminuted fractures unsuitable for fixation, and incomplete medical records or follow-up.
Variables
The primary outcomes were radiographic/clinical bone union after hook plate fixation. The secondary clinical outcomes were active ROM of the PIP joint and PIP joint stability.
Data sources and measurement
Demographic and clinical data were abstracted from electronic medical records and operative notes. The clinical results were assessed by evaluating joint instability, residual pain, and changes in ROM before and after plate removal. Radiologic results including fixation failure and achievement of bone union were assessed using simple radiographs.
The criteria for bone union were defined as the disappearance of the fracture line and trabecular bridging across the fracture site on radiographs, accompanied by the absence of tenderness or pain at the fracture site during active motion.
Active ROM of the PIP joint was measured using a standard finger goniometer. Because this was a two-center study, ROM was assessed by two orthopedic surgeons (one at each institution) who followed a standardized measurement protocol and maintained close communication to minimize interobserver variability. ROM was measured twice for each patient—once at the final follow-up before implant removal and again at the follow-up visit after implant removal. As follow-up intervals varied among patients, this variability was acknowledged as a study limitation.
Bias
To minimize selection bias, consecutive patients who met the inclusion criteria were enrolled from both institutions. All surgeries were performed by two senior hand surgeons using a consistent surgical and postoperative rehabilitation protocol. ROM measurements were conducted by each surgeon at their respective institution, following a standardized protocol and maintaining close communication to reduce interobserver variability.
Study size
No a priori sample-size calculation was performed because this was an exploratory retrospective case series of a relatively uncommon surgical indication. All eligible subjects were selected.
Statistical methods
Analyses were primarily descriptive. Continuous variables were summarized as mean (range).
Results
Participants’ characteristics and injury profile
The patients included five men and three women with a mean age of 27.2 years (range, 12–44 years). They had various injury mechanisms, including sports activity, assault, and industrial accident. The average time from the injury to the operation was 16.2 days (range, 1–90 days). The average duration of follow-up was 4.9 months (range, 1–9 months). All patients achieved union at final follow-up without fixation failure. The average time to union was 2.2 months (range, 1–4 months) (
Table 1).
Among the nine digits that achieved union, eight digits underwent implant removal. After implant removal, no complications were observed, and the joints had good stability and showed slightly increased ROM. In all patients, the ROM in the PIP joint was 85° (range, 70°–100°) before implant removal and 89.4° (range, 80°–100°) after implant removal. The mean postoperative interval of ROM measurement was 2.2 months before implant removal, corresponding to the time of bone union, and 4.9 months (range, 1–9 months) at the final follow-up after removal. Because the timing of follow-up visits varied among patients, these measurements may not represent identical postoperative stages for all cases. All patients exhibited no joint instability and no residual pain.
Discussion
Key results
After hook plate fixation for middle phalanx volar plate avulsion fractures, all digits achieved bone union without fixation failure. The mean time to union was 2.2 months (range, 1–4 months). Eight digits underwent implant removal, with no complications related to the removal. The average active ROM of the PIP joint was 85° before removal and 89.4° after. At the final follow-up (mean, 4.9 months), no patients exhibited joint instability or residual pain.
Interpretation and comparison with previous studies
This study demonstrated that hook plate fixation provided consistent bone union and favorable joint stability, even in small avulsion fragments. The surgical management of volar plate avulsion fractures poses significant challenges due to the fixation of small fragments and the restoration of joint stability. For fragments of large size, fixation options such as mini screws and pull-out sutures are available and have been reported to yield good results [
9]. However, for smaller fracture sizes, the options for achieving stability through fixation are limited, leading to a greater consideration of conservative treatment. Additionally, fragment excision has been reported as a method to reduce limited motion following conservative treatment [
10,
11]. This retrospective study aimed to evaluate the surgical outcomes of volar plate avulsion fractures using hook plates as the primary treatment modality.
Hook plates represent an excellent option for overcoming these issues. Since being reported by Teoh and Lee [
12] as a method for fixing bony mallet fragments at the base of the distal phalanx, hook plates have been developed and refined. They offer the advantages of being small in size, minimizing joint invasion, and being easy to manipulate. Although only a single screw was used for distal fixation, the hook component effectively acted as a tension band converting tensile forces into compression across the fracture site, providing sufficient stability even for small fragments. Additionally, it does not directly penetrate the fracture fragments for fixation, thereby reducing the risk of fragment comminution. In addition to avoiding fragment comminution, this technique minimizes soft-tissue disruption and preserves the biological environment around the fracture site, which may facilitate bone healing and reduce postoperative adhesion.
Teoh and Lee [
12] reported successful fixation of distal phalanx mallet fractures without adhesion or joint stiffness, while Kang et al. [
3] later applied the hook plate to proximal phalangeal base fractures and observed occasional tendon adhesion and stiffness. In contrast, our study applied hook plate fixation to middle phalanx volar plate avulsion fractures, achieving complete union and no adhesion, likely due to minimal volar dissection and timely implant removal. Our findings demonstrate that the utilization of hook plates for the fixation of volar avulsion fractures resulted in successful bone union in all patients, with an average union time of 2.2 months. Before and after implant removal, the ROM of the PIP joint increased from 85 degrees to 89.4°, which is consistent with that in previous studies.
There are certainly disadvantages to using hook plates, such as potential irritation or adhesion caused by the implant [
3]. However, in our study, these complications were not observed, possibly prevented by the removal of implants in eight out of nine digits, suggesting that implant removal may have contributed to avoiding such complications.
In our study, implant removal was performed in eight out of nine digits. Following implant removal, good joint stability and a slight increase in the ROM of the PIP joint were observed. No additional manipulation such as brisement was performed at the time of implant removal, and the improvement in ROM occurred gradually during postoperative rehabilitation rather than immediately after removal. This improvement in ROM indicates successful fracture healing and postoperative recovery. Although plate removal after bone union still remains controversial, we experienced limitation of joint motion and restoration of total ROM after removal in all patients. Additionally, plate removal can prevent potential tendon adhesion and joint stiffness that may be caused by the plate. We believe that implant removal should be performed promptly after bone union has been confirmed to prevent adhesion and facilitate early recovery of motion. We proposed that the plate should be removed after bone union to gain complete ROM.
The surgical technique used in this study, which is similar to that of Kang et al. [
3] and Thirumalai et al. [
4], allowed for the anatomical reduction of the fracture fragments and precise placement of the hook plate. The hook plate, which was fabricated from a 1.5-mm modular hand system titanium plate, provided the necessary stability by converting tensile forces into compressive forces across the fracture site.
This study has several limitations to consider. Its retrospective design and small sample size limit the generalizability of the results. The relatively short follow-up duration also precluded assessment of long-term functional outcomes or degenerative changes. In addition, the timing of ROM measurement before and after implant removal was not completely standardized. Although the preremoval measurement was performed at the time of bone union (approximately 2.2 months postoperatively), the post-removal measurement corresponded to the final follow-up period (mean, 4.9 months; range, 1–9 months). Therefore, the observed improvement in ROM may partially reflect natural recovery over time rather than the direct effect of implant removal. Further prospective, comparative studies with larger cohorts are warranted to validate the long-term efficacy and safety of hook plate fixation for volar plate avulsion fractures.
Conclusions
The utilization of hook plates for the surgical treatment of volar plate avulsion fractures resulted in successful bone union and improved joint stability. The use of hook plates offers a viable treatment option for these challenging fractures, allowing for anatomical reduction and restoration of joint function. Further studies are needed to determine the long-term outcomes and compare the effectiveness of different surgical techniques in the management of volar plate avulsion fractures.
Article Information
-
Author contributions
Conceptualization: HJL, DHK. Data curation: KSL, SWS, HJK. Formal analysis: KSL, SWS, HJK. Funding acquisition: HJL. Investigation: KSL, SWS. Methodology: KSL, SWS, DHK. Project administration: DHK. Visualization: KSL, HJK. Writing-original draft: KSL, HJL, DHK. Writing-review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant no. RS-2022-KH130590).
-
Data availability
Contact the corresponding author for data availability.
-
Acknowledgments
None.
-
Supplementary materials
None.
Fig. 1.Fabrication of a hook plate by bending the cut ends of a standard 1.5-mm modular hand system titanium plate into a hook shape.

Fig. 2.Radiographs of a middle phalanx avulsion fracture. (A) Initial fracture. (B) Reduction after open reduction.

Fig. 3.Radiographs after hook plate fixation. (A) Lateral view. (B) Anteroposterior view showing the hook plate crossing the fracture line and secured with a distal screw.

Fig. 4.Radiographs during follow-up. (A) Bone union after treatment with the hook plate. (B) Appearance after implant removal.

Table 1.Baseline demographic and clinical outcomes (patients=8, digits=9)
|
Variable |
Value |
|
Age (yr) |
27.2 (12‒44) |
|
Sex (male:female) |
5:3 |
|
Injury-to-surgery interval (day), |
16.2 (1–90) |
|
Follow-up duration (mo) |
4.9 (1–9) |
|
Time to union (mo) |
2.2 (1–4) |
|
ROM at PIP joint before removal (°) |
85 (70–100) |
|
ROM at PIP joint after removal (°) |
89.4 (80–100) |
References
- 1. Wieschhoff GG, Sheehan SE, Wortman JR, et al. Traumatic finger injuries: what the orthopedic surgeon wants to know. Radiographics 2016;36:1106-28.ArticlePubMed
- 2. Kim YW, Roh SY, Kim JS, Lee DC, Lee KJ. Volar plate avulsion fracture alone or concomitant with collateral ligament rupture of the proximal interphalangeal joint: a comparison of surgical outcomes. Arch Plast Surg 2018;45:458-65.ArticlePDF
- 3. Kang GC, Yam A, Phoon ES, Lee JY, Teoh LC. The hook plate technique for fixation of phalangeal avulsion fractures. J Bone Joint Surg Am 2012;94:e72. ArticlePubMed
- 4. Thirumalai A, Mikalef P, Jose RM. The versatile hook plate in avulsion fractures of the hand. Ann Plast Surg 2017;79:270-4.ArticlePubMed
- 5. Lister G. Intraosseous wiring of the digital skeleton. J Hand Surg Am 1978;3:427-35.ArticlePubMed
- 6. Sakuma M, Nakamura R, Inoue G, Horii E. Avulsion fracture of the metacarpophalangeal joint of the finger. J Hand Surg Br 1997;22:667-71.ArticlePubMedPDF
- 7. Bekler H, Gokce A, Beyzadeoglu T. Avulsion fractures from the base of phalanges of the fingers. Tech Hand Up Extrem Surg 2006;10:157-61.ArticlePubMed
- 8. Lee JY, Teoh LC. Dorsal fracture dislocations of the proximal interphalangeal joint treated by open reduction and interfragmentary screw fixation: indications, approaches and results. J Hand Surg Br 2006;31:138-46.ArticlePubMedPDF
- 9. Lee CH, Kim CU, Cha K. Pullout suture using polyamide monofilaments for volar plate avulsion fractures of the proximal interphalangeal joint. J Hand Surg Eur Vol 2018;43:558-60.ArticlePubMedPDF
- 10. Lee S, Jang SJ, Jeon SH. Factors related to failure of conservative treatment in volar plate avulsion fractures of the proximal interphalangeal joint. Clin Orthop Surg 2020;12:379-85.ArticlePubMedPMCPDF
- 11. Seo I, Lee KS, Chung S, Son SW, Lee HJ. Extension block pinning combined with traction using towel clamps for effective reduction of mallet fracture: a technical tip. Arch Hand Microsurg 2023;28:93-6.ArticlePDF
- 12. Teoh LC, Lee JY. Mallet fractures: a novel approach to internal fixation using a hook plate. J Hand Surg Eur Vol 2007;32:24-30.ArticlePubMedPDF
 , Sang-Woo Son1
, Sang-Woo Son1 , Hee-June Kim1,2,3
, Hee-June Kim1,2,3 , Hyun-Joo Lee1,2,3
, Hyun-Joo Lee1,2,3 , Dong Hee Kim4
, Dong Hee Kim4









 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

