Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 37(4); 2024 > Article
-
Case Report
- Acute on Chronic Stress Fracture of a Varus Deformed Distal Tibia - A Case Report -
-
Seong Kee Shin, M.D.
 , Ki Chun Kim, M.D., Ph.D.
, Ki Chun Kim, M.D., Ph.D. , Eli Schmidt, B.S.*
, Eli Schmidt, B.S.* , Seung Yeon Cho, M.D.
, Seung Yeon Cho, M.D. , Ki Chul Park, M.D., Ph.D.†
, Ki Chul Park, M.D., Ph.D.†
-
Journal of Musculoskeletal Trauma 2024;37(4):184-189.
DOI: https://doi.org/10.12671/jmt.2024.37.4.184
Published online: October 25, 2024
1Department of Orthopedic Surgery, Seoul Medical Center, Seoul, Korea
*Department of Orthopaedics and Rehabilitation, University of Iowa Hospitals & Clinics, Iowa City, IA, USA
†Department of Orthopedic Surgery, Hanyang University Guri Hospital, Guri, Korea
- Correspondence to: Ki Chun Kim, M.D., Ph.D. Department of Orthopedic Surgery, Seoul Medical Center, 156 Sinnae-ro, Jungnang-gu, Seoul 02053, Korea Tel: +82-2-2276-7841 Fax: +82-2-2276-8535 E-mail: 711000e@naver.com
• Received: March 28, 2024 • Revised: June 3, 2024 • Accepted: August 1, 2024
© 2024 The Korean Fracture Society
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,108 Views
- 34 Download
Abstract
- A severe post-traumatic distal tibia vara deformity is an uncommon condition in orthopedics. Typical symptoms include intractable recurrent pain, fragility related to stress fractures over the tensile area, and a limping gait caused by leg length discrepancy. Surgical management should be performed on acute fractures extending from a stress fracture gap. For successful surgical results, deformity correction is important for sustaining axial load bearing for standing and walking. Procedures to manage this condition have been proposed, but there is a high risk of complications, including metal failure, nonunion, and weakness caused by a long period of rehabilitation. In this case, the authors report a successful result using a modified clamshell osteotomy combined with a proximal and distal wedge bone resection in a single stage.
Introduction
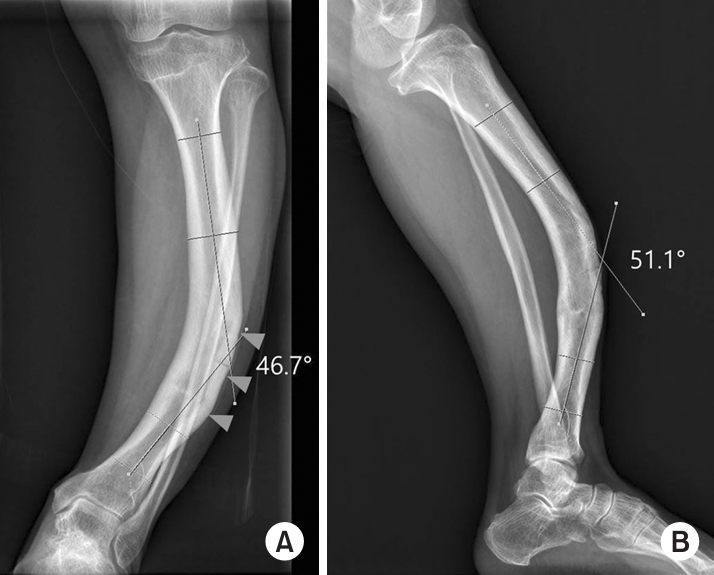
The management of deformity of the tibia has been a challenging issue facing the orthopaedic surgeon. Post-traumatic tibia vara is the condition where there is overloading over the tensile area of the tibia causing the ankle and hindfoot to take on a long term valgus position in order to bear weight. Following a tibia fracture, the incidence of angular deformity reaching greater than 5° after conservative management reportedly reached 3% to 50%.1,2) For successful deformity correction it is imperative to evaluate the range of malalignment and determine the true deformity plane preoperatively. Among some surgical techniques, the clamshell osteotomy was introduced to manage diaphyseal deformity in place of osteotomy or multiplanar plate contouring.3) This technique may be favorable as it is less complicated than an external fixator. However, most cases reported in the literatures are confined to a range from 0° to 32° in angular deformity and 0° to 25° in rotational deformity.3-6) This is a report of patient with severe tibial deformity including an angular deformity of 54.6° in 75° of external rotation view in a three-dimensional (3D) reconstructed computed tomography (CT) image (Fig. 1). This case was further complicated by intractable pain associated with a stress fracture which progressed to an acute fracture following a fall.
Case Report
A 59-year-old female patient presented to a senior surgeon with acute-on-chronic severe pain of the left lower extremity after a mild slip-down fall. The patient had a history of a left distal tibial fracture when she was 12 years old that was managed conservatively. She had been suffering from a limping gait with leg length discrepancy (LLD) and chronic recurrent left lower extremity pain with weight-bearing that was diagnosed at an outside facility as a stress fracture associated with the tibia deformity. Previously, when the pain became aggravated or acutely worsened, treatment included restriction of weight bearing with cast or brace until the pain subsided. Plain radiographs taken at presentation demonstrated a radiolucent gap surrounded by sclerotic cortical thickening over the apex of tibia angulation. In conventional anteroposterior and lateral radiographs, the tibia showed 46.7° of varus and 51.1° of anterior angulation (Fig. 2). In two axial CT images through the proximal tibia just below the knee joint line and distal tibia just above the ankle join line, there was 20.6° of external rotation of the intermalleolar axis with respect to the posterior tibial plateau.7) When measured at the apex of the convex area in the axial plane, the tibia was measured to be 86.6° externally rotated in reference to the posterior tibial plateau and 66.0° externally rotated in reference to the intermalleolar axis. In the sagittal 3D reconstructed image, which was 75° externally rotated in reference to anteroposterior view to set the most definite convex plane, the tibia was angulated 54.6° (Fig. 1). There was a 40.0 mm LLD as measured via scanogram (Fig. 3). The LLD seen was mainly a result of tibia deformity. There was cortical thickening and sclerosis over the convex area (Fig. 2). In bone scan, intensive focal radioactive iodine uptake was observed in the anterior cortex of the distal 1/3 of left tibia suggesting an active state (Fig. 4). Her symptoms were relieved after medication and activity restriction.
Two years later, she had another slip down injury and visited the emergency room for left leg pain. Images taken at presentation showed an oblique distal 1/3 tibia fracture extending from the previous stress fracture gap combined with a distal fibula fracture (Fig. 5). She elected for surgical repair was transferred to the presenting author. On initial physical examination, her skin was intact without vascular compromise despite obvious deformity.
There were two issues to consider for this patient.
First, given the acute fracture of the deformity of the distal tibia, what kind of fixation tool was appropriate to stabilize both the tibia and fibula fracture and also restore alignment and length at the same time? Second, what was the best method to accomplish successful bone union and improve quality of life in relation to both gross leg deformity and tolerable pain?
For deformity correction, a large amount of bone resection could be considered. However, this might lead to limb shortening and nonunion. Progressive correction with external fixation through osteogenesis would be another option. However, this method would take a long time to achieve acceptable alignment and necessitate complex mathematical calculation and delicate management.
For surgical technique, internal and external or hybrid fixation with possible osteotomy would be considered. Fixation with plate and screws only for the fracture itself would lead to be a high risk of nonunion or metal failure if it is not accompanied by sufficient deformity correction. The clamshell osteotomy and fixation with intramedullary nail was developed to correct translational and angular deformity of lower limb long bones, but the angular deformity presented here was too severe for direct application considering the reported range of corrected angular deformity was less than 32°.3,6,8)
In this case, our approach utilized the concept of an intersegmental angular deformity by dividing the tibia into proximal, middle, and distal cylindrical segments. Intersegmental angles were 25.5° between proximal and middle segments and 29.1° between middle and distal segments respectively. Closed wedge osteotomy between the proximal and middle segments was planned within the correctable range which reportedly showed successful results with the clamshell osteotomy. The same procedure was designed between middle and distal segments.
In the supine position under spinal anesthesia, the distal 1/3 of the tibia, centered on middle segment, was approached with an anteromedial incision. The clamshell osteotomy was performed using a 3.5-mm drill to make bicortical holes from anterolateral to posteromedial, perpendicular to the longitudinal axis of the middle segment. Shallow cutting of the anterolateral cortical wall was performed via saw to make a furrow connecting the holes, and then an osteotome was used to fully penetrate the near and far cortices. The intercalary middle segment was made by proximal and distal osteotomies. An additional proximal cut was performed to introduce a 15° wedge block between the proximal and middle segments. For the distal cutting, a 15° wedge block was created with resection of sclerotic bone adjacent to the stress fracture. The soft tissue attached to the triangular fragment in the middle segment was carefully preserved for vascular supply. Then the rotational deformity was corrected by attempting collinear alignment of the patella and second toe. To achieve this, the guidewire was passed from the proximal segment through the middle segment into the distal segment with the aid of fluoroscopic guidance. The length of the guidewire was measured. After draping over the cortex with an elastic bandage to prevent the detachment of the soft tissue and preserve bone fragment deposit in the middle segment, reaming was performed on the proximal and distal segments until cortical chattering. In the middle segment, the reamer was pushed carefully to protect the neurovascular structures. A nail compatible with the length was inserted and two proximal and distal interlocking screws were then inserted. Finally, the fibula was reduced and fixated with plate and screws (Fig. 6).
There was no vascular compromise or heel cord tightening. Postoperatively, the patient was made non–weight-bearing. She was kept in a short leg cast for 5 weeks. On postoperative week 5, she was changed from a short leg cast to a short leg splint, and started half body weight bearing with intermittent ankle movement. She started full weight bearing on postoperative week 8, wearing a brace when outdoors only. She complained of pain in her calf, the dorsomedial side of her midfoot and hindfoot until 6 months, which gradually improved and resolved 17-month postoperatively.
The visual analogue pain score obtained on a prior visit before the acute fracture was 50 on daily life. On 12-month postoperative follow-up, it had improved to 20 with additional improvement to 10 on 24-month postoperative follow-up. At her 4-year follow-up, she reported she could enjoy climbing and do physical work without any complaints of pain. Radiographs at that time demonstrated improved alignment with bridging callus at the osteotomy sites and a LLD of 9 mm (Fig. 7). Cortical thickening and sclerosis as a response to overload of the tensile area had gradually returned to its normal appearance after restoration of alignment (Fig. 8).
Discussion
The clamshell osteotomy was initially developed to realign diaphyseal deformity for the femur and tibia.3) It’s usage has spread to the distal metaphysis as well.4) This technique can correct translational, angular, and rotational deformity and subsequently obtain a leg lengthening effect in the range of 2 cm as a one stage procedure.3) In general, lower limb lengthening along the anatomical axis can often be ignored if it is less than 2 cm, and it is possible if it falls within the range of 2 to 4 cm. When more than 4 cm lengthening is required, neurovascular compromise should be considered.9) The patient in this report could achieve lengthening effect through straightening the varus deformed tibia by closed wedge osteotomy combined with clamshell osteotomy. Unlike axial limb lengthening, neurovascular injury by distraction might not happen in this patient whose neurovascular route was mainly decurved with minor traction.
This technique has also been applied in the treatment of acute fracture in a deformed femur and tibia.8) Utilizing this technique, the patients involved in acute and chronic tibia deformity were able to return to their pre-injury level of activity.
In this case, the degree of angular deformity of the tibia was beyond the reported range of deformity managed with the clamshell osteotomy. The tibia was gradually adapted to the continuous strain over the convex area which caused the thickened cortex to sustain stress and obliterated the intramedullary area.10) However, the accumulation of repeated stress exhausted the compensation capacity and lead to a failure to heal the outer cortex and a fragile condition leading to an acute injury. The authors introduced a 3 segment concept and applied the clamshell osteotomy to each intersegmental area. Considering the successful range of clamshell osteotomy, 15° of wedge segments were resected from each intersegmental area. Following these resections, the 54.6° angular deformity between proximal and distal fragments has decreased into 24.6°, which was in accordance with the range of angular deformity with reportedly successful results.3,6,8) Therefore, the clamshell osteotomy combined with wedge osteotomy could lead to a successful result for angular deformity more than 32°.3)
Russell et al.3) suggested that lengthening of the tibia by >3 cm is one of the relative contraindications. However, this patient’s limb (tibia) length was successfully restored and LLD has improved from 4.0 cm to 9 mm.
In conclusion, it is challenging to visualize that a tibia with such severe angular deformity combined with an acute injury extended from a stress fracture gap could be realigned with a conventional clamshell osteotomy.
When this technique was combined with a wedge osteotomy utilizing the concept of intersegmental angular deformity correction, both the capacity for correction increased and the limitation of a tibia LLD could be overcome in a one stage operation.
Fig. 1.
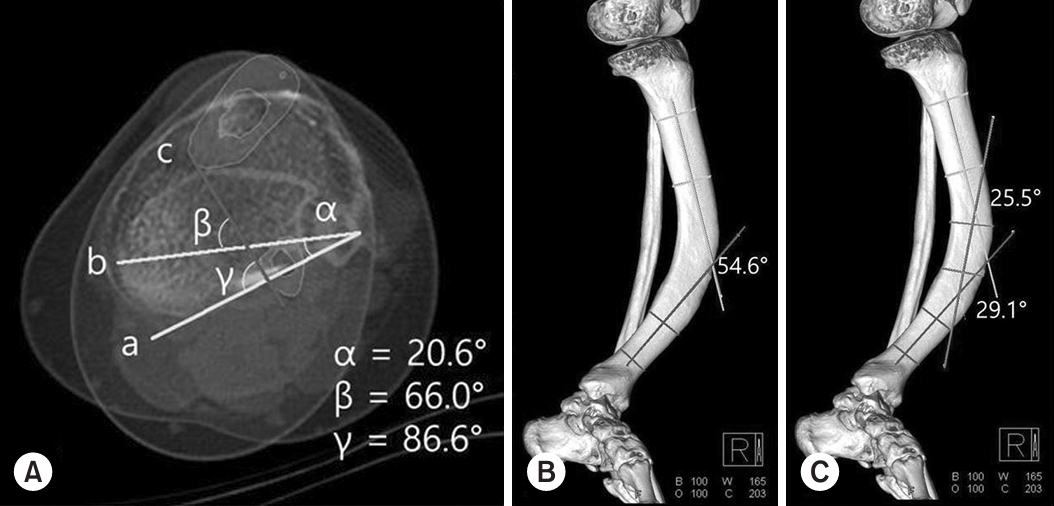
Angular measurements were performed in a three-dimensional (3D) reconstructed computed tomography (CT) image. (A) Three axial CT slices were used: one through the proximal tibia just below the knee joint line (‘a’), one through the distal tibia and fibula (‘b’) just above the ankle joint line, and one through the apex of the convex area (‘c’). The blue color indicates cortical bones of the tibia and fibula in the axial CT slice through the apex of the convex area. On a superimposed image of these three slices, ‘α,’ ‘β,’ and ‘γ’ indicates the rotation angle of the intermalleolar axis (‘b’) in reference to the posterior tibial plateau (‘a’), the rotation angle of the apex of the convex area in reference to the intermalleolar axis (‘b’) and the posterior tibial plateau, respectively. (B) In the 3D reconstructed image showing the most angular deformity in 75° of the external rotation view, the yellow and blue lines represent the longitudinal axes of proximal and distal segments each. The tibia was angulated at 54.6° between the proximal and distal segments. (C) The green lines represent the boundary line and the longitudinal axis of the middle segment. The tibia was angulated 25.5° between the proximal and middle segments and 29.1° between the middle and distal segments.
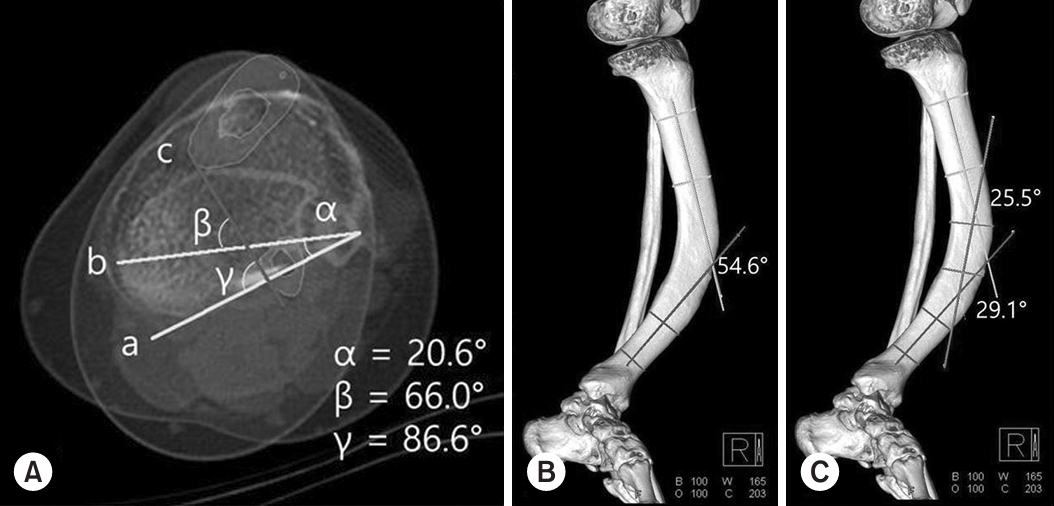
Fig. 2.
Conventional weight-bearing anteroposterior and lateral images from a 59-year-old female with an acute-on-chronic injury to her left lower extremity. (A) Anteroposterior standing radiograph shows a 46.7° varus angulation of the left tibia. The bisecting lines illustrate the anatomic axes of the proximal and distal tibial segments in the coronal plane, indicating the varus deformity. There was an intramedullary narrowing caused by the cortical thickening and sclerosis over the convex area (arrowheads). (B) Lateral radiograph of the tibia showed 51.1° of anterior angulation. The bisecting lines show the anatomic axes of the proximal and distal tibial segments in the sagittal plane, indicating the anterior angular deformity.
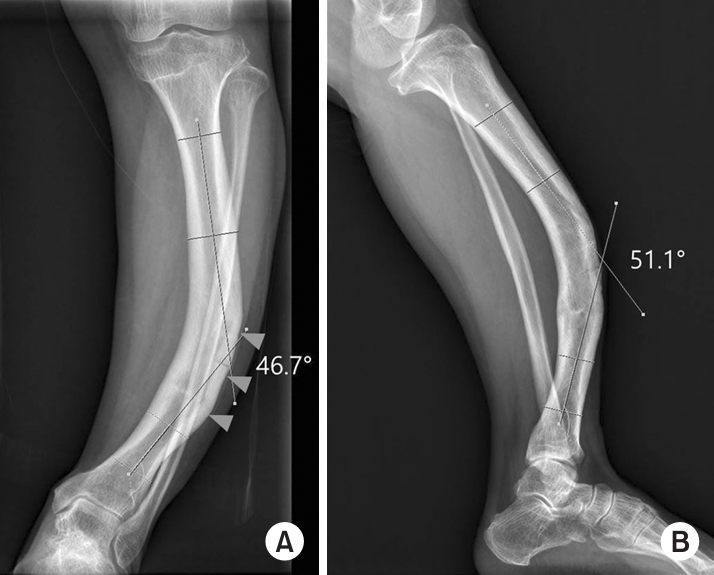
Fig. 3.

Standing anteroposterior radiograph of the lower extremity performed using computed radiography on a case with approximately 40 mm shortening of the tibia related to bowing.

Fig. 4.
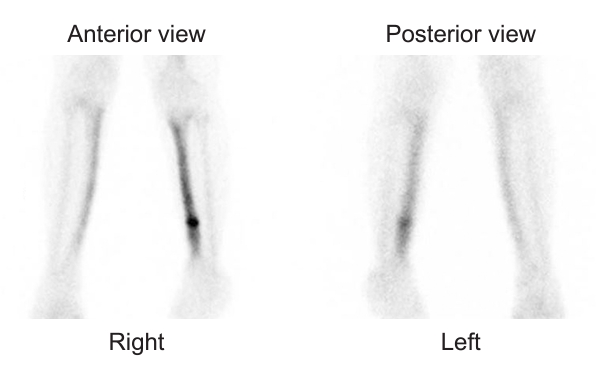
Anterior and posterior bone scan images of both lower extremities showed intensely and focally increased radioactive iodine uptake at the anterior cortex of the distal 1/3 of the left tibial shaft and increased the cortical radioactive iodine uptake in the entire left tibia with bowing deformity. This suggests acute injury surrounded by old post-traumatic change with cortical thickening.
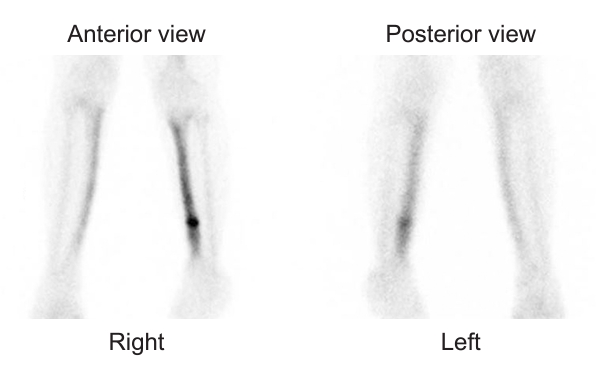
Fig. 5.

Radiographs in the anteroposterior (A) and lateral (B) views and a three-dimensional reconstructed computed tomography scan (C) showing an acute fracture obliquely extending from a previous stress fracture gap combined with a distal fibula fracture.

Fig. 6.
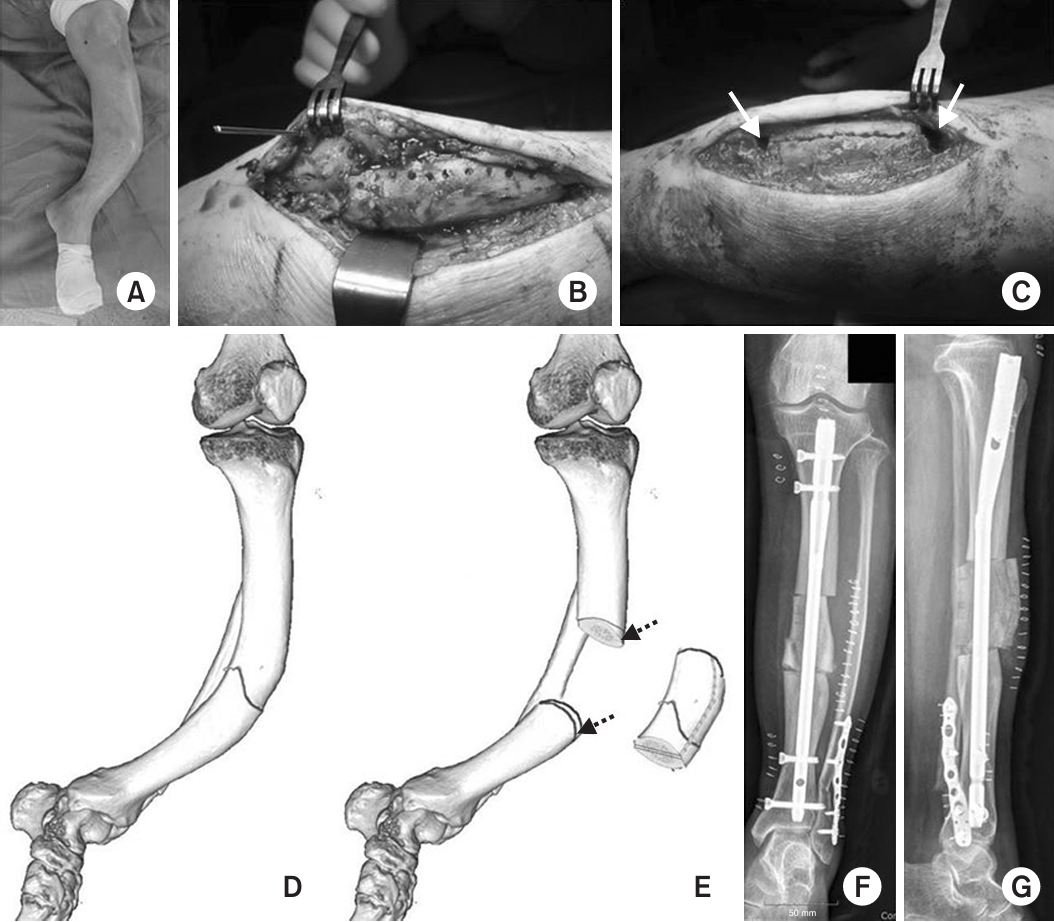
Clinical images of the surgical fields and schematic drawings. (A) Clinical image of left lower leg. (B) A 3.5 mm longitudinal and bicortical hole was made to demarcate the imaginary osteotomy line and ease the clamshell osteotome. (C) The clamshell osteotomy was performed along the pre-made holes. On upper and lower margins, bony defects were observed after 15° wedge shape bone resection (arrows). (D) Drawing of the tibial and fibula fracture. (E) Drawing of the clamshell osteotomy of the middle segment and the lines illustrating the 15° wedge shape bone segment (dotted arrows). (F) Immediate postoperative anteroposterior radiograph. (G) Immediate postoperative lateral radiograph.
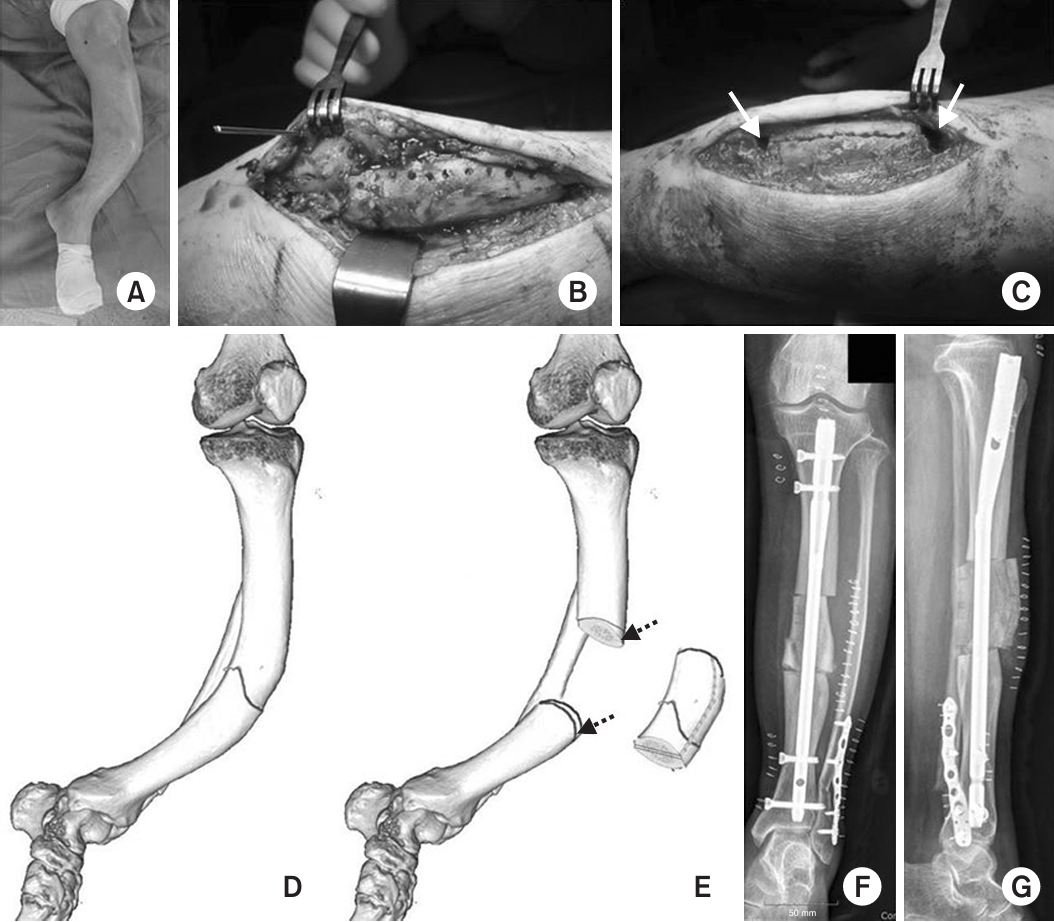
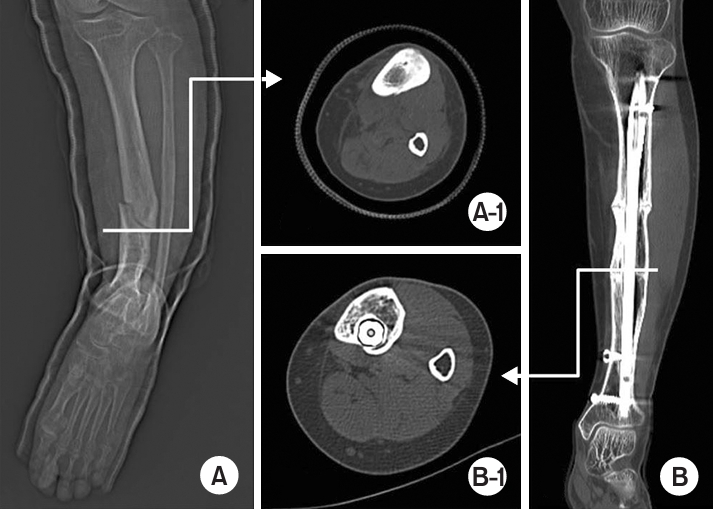
Fig. 7.
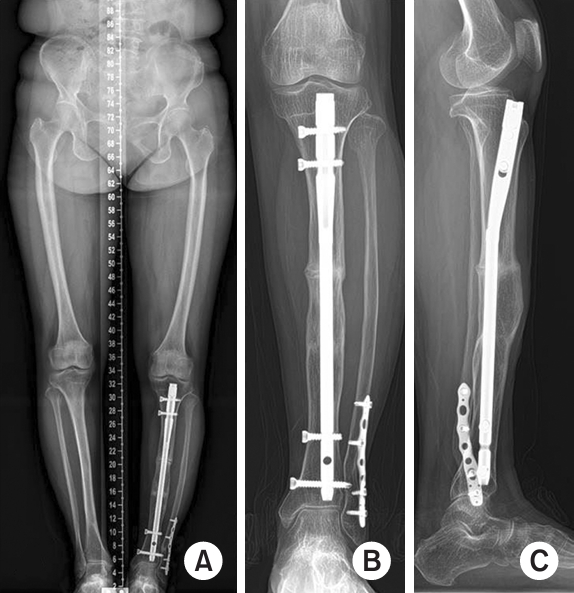
Scanogram (A) and radiographs (B, C) showing the clamshell osteotomy xed with an intramedullary nail. (A) Leg length discrepancy was 9 mm at one-year and two-month postoperatively. (B, C) The bone union of the middle segment with proximal and distal segments and fracture healing was observed at the four-year postoperative conventional radiographs. The cortical thickening and sclerosis had resolved.
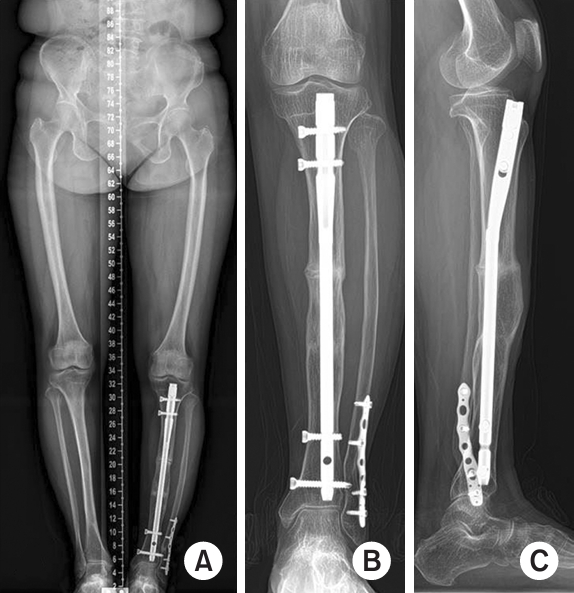
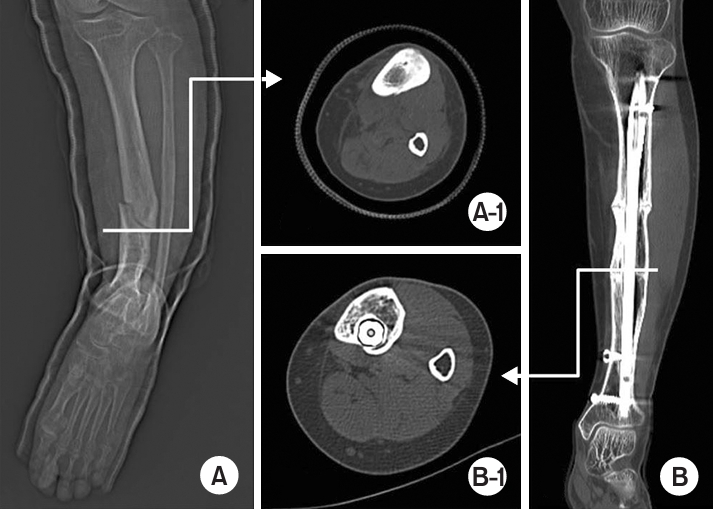
Fig. 8.
Change in the cortical thickness before and after operation. (A) Computed tomography slice of the lower margin in the middle segment showed cortical thickening and obliteration of half of the medullary canal. (A-1). (B) Uniform cortical thickness was observed at the same level of A-1 in one year and 10 months after operation (B-1).
- 1. Keller CS: The principles of the treatment of tibial shaft fractures: a review of 10,146 cases from the literature. Orthopedics, 6: 993-999, 1983.ArticlePubMed
- 2. Sarmiento A, Sobol PA, Sew Hoy AL, Ross SD, Racette WL, Tarr RR: Prefabricated functional braces for the treatment of fractures of the tibial diaphysis. J Bone Joint Surg Am, 66: 1328-1339, 1984.ArticlePubMed
- 3. Russell GV, Graves ML, Archdeacon MT, Barei DP, Brien GA Jr, Porter SE: The clamshell osteotomy: a new technique to correct complex diaphyseal malunions: surgical technique. J Bone Joint Surg Am, 92 Suppl 1 Pt 2: 158-175, 2010.PubMed
- 4. Darden C, Pujari A, Stocchi C, Forsh D: Distal tibial metaphyseal malunion treated with clamshell osteotomy: a case report. JBJS Case Connect, 13: e23.00072. 2023.
- 5. Patel I, Young J, Washington A, Vaidya R: Malunion of the tibia: a systematic review. Medicina (Kaunas), 58: 389, 2022.ArticlePubMedPMC
- 6. Purcell KF, Russell GV, Graves ML: The clamshell osteotomy for diaphyseal malunion in deformity correction and fracture surgery. Medicina (Kaunas), 57: 951, 2021.ArticlePubMedPMC
- 7. Lerch TD, Eichelberger P, Baur H, et al: Prevalence and diagnostic accuracy of in-toeing and out-toeing of the foot for patients with abnormal femoral torsion and femoroacetabular impingement: implications for hip arthroscopy and femoral derotation osteotomy. Bone Joint J, 101-B: 1218-1229, 2019.PubMed
- 8. Pires RE, Gausden EB, Sanchez GT, et al: Clamshell osteotomy for acute fractures in the malunion setting: a technical note. J Orthop Trauma,, 32: e415-e420, 2018.ArticlePubMed
- 9. Hosny GA: Limb lengthening history, evolution, complications and current concepts. J Orthop Traumatol, 21: 3, 2020.ArticlePubMedPMCPDF
- 10. Frost HM: A 2003 update of bone physiology and Wolff ’s Law for clinicians. Angle Orthod, 74: 3-15, 2004.PubMed
References
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

Acute on Chronic Stress Fracture of a Varus Deformed Distal Tibia - A Case Report -
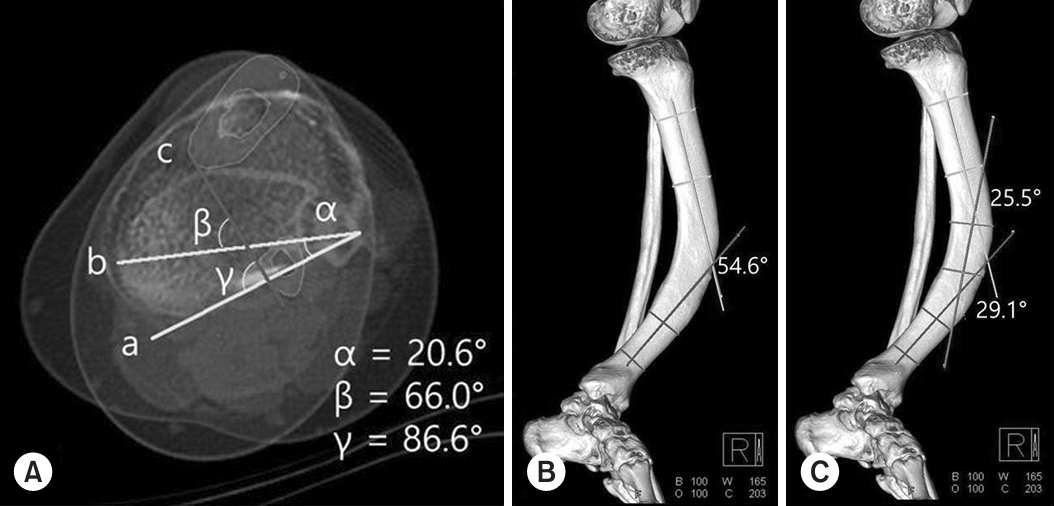







Fig. 1. Angular measurements were performed in a three-dimensional (3D) reconstructed computed tomography (CT) image. (A) Three axial CT slices were used: one through the proximal tibia just below the knee joint line (‘a’), one through the distal tibia and fibula (‘b’) just above the ankle joint line, and one through the apex of the convex area (‘c’). The blue color indicates cortical bones of the tibia and fibula in the axial CT slice through the apex of the convex area. On a superimposed image of these three slices, ‘α,’ ‘β,’ and ‘γ’ indicates the rotation angle of the intermalleolar axis (‘b’) in reference to the posterior tibial plateau (‘a’), the rotation angle of the apex of the convex area in reference to the intermalleolar axis (‘b’) and the posterior tibial plateau, respectively. (B) In the 3D reconstructed image showing the most angular deformity in 75° of the external rotation view, the yellow and blue lines represent the longitudinal axes of proximal and distal segments each. The tibia was angulated at 54.6° between the proximal and distal segments. (C) The green lines represent the boundary line and the longitudinal axis of the middle segment. The tibia was angulated 25.5° between the proximal and middle segments and 29.1° between the middle and distal segments.
Fig. 2. Conventional weight-bearing anteroposterior and lateral images from a 59-year-old female with an acute-on-chronic injury to her left lower extremity. (A) Anteroposterior standing radiograph shows a 46.7° varus angulation of the left tibia. The bisecting lines illustrate the anatomic axes of the proximal and distal tibial segments in the coronal plane, indicating the varus deformity. There was an intramedullary narrowing caused by the cortical thickening and sclerosis over the convex area (arrowheads). (B) Lateral radiograph of the tibia showed 51.1° of anterior angulation. The bisecting lines show the anatomic axes of the proximal and distal tibial segments in the sagittal plane, indicating the anterior angular deformity.
Fig. 3. Standing anteroposterior radiograph of the lower extremity performed using computed radiography on a case with approximately 40 mm shortening of the tibia related to bowing.
Fig. 4. Anterior and posterior bone scan images of both lower extremities showed intensely and focally increased radioactive iodine uptake at the anterior cortex of the distal 1/3 of the left tibial shaft and increased the cortical radioactive iodine uptake in the entire left tibia with bowing deformity. This suggests acute injury surrounded by old post-traumatic change with cortical thickening.
Fig. 5. Radiographs in the anteroposterior (A) and lateral (B) views and a three-dimensional reconstructed computed tomography scan (C) showing an acute fracture obliquely extending from a previous stress fracture gap combined with a distal fibula fracture.
Fig. 6. Clinical images of the surgical fields and schematic drawings. (A) Clinical image of left lower leg. (B) A 3.5 mm longitudinal and bicortical hole was made to demarcate the imaginary osteotomy line and ease the clamshell osteotome. (C) The clamshell osteotomy was performed along the pre-made holes. On upper and lower margins, bony defects were observed after 15° wedge shape bone resection (arrows). (D) Drawing of the tibial and fibula fracture. (E) Drawing of the clamshell osteotomy of the middle segment and the lines illustrating the 15° wedge shape bone segment (dotted arrows). (F) Immediate postoperative anteroposterior radiograph. (G) Immediate postoperative lateral radiograph.
Fig. 7. Scanogram (A) and radiographs (B, C) showing the clamshell osteotomy xed with an intramedullary nail. (A) Leg length discrepancy was 9 mm at one-year and two-month postoperatively. (B, C) The bone union of the middle segment with proximal and distal segments and fracture healing was observed at the four-year postoperative conventional radiographs. The cortical thickening and sclerosis had resolved.
Fig. 8. Change in the cortical thickness before and after operation. (A) Computed tomography slice of the lower margin in the middle segment showed cortical thickening and obliteration of half of the medullary canal. (A-1). (B) Uniform cortical thickness was observed at the same level of A-1 in one year and 10 months after operation (B-1).
Fig. 1.
Fig. 2.
Fig. 3.
Fig. 4.
Fig. 5.
Fig. 6.
Fig. 7.
Fig. 8.
Acute on Chronic Stress Fracture of a Varus Deformed Distal Tibia - A Case Report -

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 ePub Link
ePub Link Cite
Cite

