Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 29(1); 2016 > Article
-
Review Article
- Scaphoid Fractures and Nonunion
- Jin Rok Oh, M.D., Ph.D.
-
Journal of the Korean Fracture Society 2016;29(1):79-92.
DOI: https://doi.org/10.12671/jkfs.2016.29.1.79
Published online: January 19, 2016
Department of Orthopedic Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea.
- Address reprint requests to: Jin Rok Oh, M.D., Ph.D. Department of Orthopedic Surgery, Yonsei University Wonju College of Medicine, 20 Ilsan-ro, Wonju 26426, Korea. Tel: 82-33-741-1356, Fax: 82-33-746-7326, E-mail: jroh@yonsei.ac.kr
Copyright © 2016 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 492 Views
- 2 Download
Abstract
- Fracture of scaphoid is relatively common, and accurate and prompt diagnosis leads to bony union with good clinical outcome. However, it can be easily missed due to vague symptomatic complaints by patients, which in turn leads to negligence of a doctor in making the diagnosis or anatomical shape of scaphoid that causes minute fracture to be ignored while viewing simple radiography. When missed, nonunion of scaphoid gradually progresses to arthritic change in the wrist. Thus when fracture of the scaphoid is suspected, further evaluation should be initiated with care, and if the diagnosis is confirmed, a proper treatment plan must be set with assessment of stability of the fracture fragment. Internal fixation is usually proposed since solid fixation of the fracture provides early return to daily activity. When nonunion of the scaphoid is present, most patients can achieve bony union with avascular bone graft and internal fixation. However, if there is sclerotic change, large bone cyst or avascular necrosis of the fracture fragment, internal fixation with bone graft that includes vascular supply should be introduced in order to achieve bony union.
- 1. Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg, 1999;33:423-426.Article
- 2. Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br, 1984;66:114-123.ArticlePDF
- 3. Compson JP, Waterman JK, Heatley FW. The radiological anatomy of the scaphoid. Part 1: osteology. J Hand Surg Br, 1994;19:183-187.Article
- 4. Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg Am, 1980;5:508-513.Article
- 5. Steinmann SP, Adams JE. Scaphoid fractures and nonunions: diagnosis and treatment. J Orthop Sci, 2006;11:424-431.Article
- 6. Weber ER, Chao EY. An experimental approach to the mechanism of scaphoid waist fractures. J Hand Surg Am, 1978;3:142-148.Article
- 7. Cockshott WP. Distal avulsion fractures of the scaphoid. Br J Radiol, 1980;53:1037-1040.Article
- 8. Horii E, Nakamura R, Watanabe K, Tsunoda K. Scaphoid fracture as a "puncher's fracture". J Orthop Trauma, 1994;8:107-110.Article
- 9. Russe O. Fracture of the carpal navicular. Diagnosis, non-operative treatment, and operative treatment. J Bone Joint Surg Am, 1960;42-A:759-768.Article
- 10. Cooney WP, Dobyns JH, Linscheid RL. Fractures of the scaphoid: a rational approach to management. Clin Orthop Relat Res, 1980;(149):90-97.Article
- 11. Freeland P. Scaphoid tubercle tenderness: a better indicator of scaphoid fractures? Arch Emerg Med, 1989;6:46-50.Article
- 12. Munk B, Bolvig L, Krøner K, Christiansen T, Borris L, Boe S. Ultrasound for diagnosis of scaphoid fractures. J Hand Surg Br, 2000;25:369-371.ArticlePDF
- 13. Chen SC. The scaphoid compression test. J Hand Surg Br, 1989;14:323-325.ArticlePDF
- 14. Parvizi J, Wayman J, Kelly P, Moran CG. Combining the clinical signs improves diagnosis of scaphoid fractures. A prospective study with follow-up. J Hand Surg Br, 1998;23:324-327.Article
- 15. Grover R. Clinical assessment of scaphoid injuries and the detection of fractures. J Hand Surg Br, 1996;21:341-343.ArticlePDF
- 16. Kawamura K, Chung KC. Management of wrist injuries. Plast Reconstr Surg, 2007;120:73e-89e.Article
- 17. Fusetti C, Poletti PA, Pradel PH, et al. Diagnosis of occult scaphoid fracture with high-spatial-resolution sonography: a prospective blind study. J Trauma, 2005;59:677-681.Article
- 18. Senall JA, Failla JM, Bouffard JA, van Holsbeeck M. Ultrasound for the early diagnosis of clinically suspected scaphoid fracture. J Hand Surg Am, 2004;29:400-405.Article
- 19. Fowler C, Sullivan B, Williams LA, McCarthy G, Savage R, Palmer A. A comparison of bone scintigraphy and MRI in the early diagnosis of the occult scaphoid waist fracture. Skeletal Radiol, 1998;27:683-687.ArticlePDF
- 20. Beeres FJ, Rhemrev SJ, den Hollander P, et al. Early magnetic resonance imaging compared with bone scintigraphy in suspected scaphoid fractures. J Bone Joint Surg Br, 2008;90:1205-1209.ArticlePDF
- 21. Adey L, Souer JS, Lozano-Calderon S, Palmer W, Lee SG, Ring D. Computed tomography of suspected scaphoid fractures. J Hand Surg Am, 2007;32:61-66.Article
- 22. Mallee WH, Doornberg JN, Ring D, et al. Computed tomography for suspected scaphoid fractures: comparison of reformations in the plane of the wrist versus the long axis of the scaphoid. Hand (N Y), 2014;9:117-121.ArticlePDF
- 23. Raby N. Magnetic resonance imaging of suspected scaphoid fractures using a low field dedicated extremity MR system. Clin Radiol, 2001;56:316-320.Article
- 24. Kukla C, Gaebler C, Breitenseher MJ, Trattnig S, Vécsei V. Occult fractures of the scaphoid. The diagnostic usefulness and indirect economic repercussions of radiography versus magnetic resonance scanning. J Hand Surg Br, 1997;22:810-813.Article
- 25. McAdams TR, Spisak S, Beaulieu CF, Ladd AL. The effect of pronation and supination on the minimally displaced scaphoid fracture. Clin Orthop Relat Res, 2003;(411):255-259.Article
- 26. Dias JJ, Taylor M, Thompson J, Brenkel IJ, Gregg PJ. Radiographic signs of union of scaphoid fractures. An analysis of inter-observer agreement and reproducibility. J Bone Joint Surg Br, 1988;70:299-301.ArticlePDF
- 27. Yin ZG, Zhang JB, Kan SL, Wang P. Treatment of acute scaphoid fractures: systematic review and meta-analysis. Clin Orthop Relat Res, 2007;460:142-151.Article
- 28. Clay NR, Dias JJ, Costigan PS, Gregg PJ, Barton NJ. Need the thumb be immobilised in scaphoid fractures? A randomised prospective trial. J Bone Joint Surg Br, 1991;73:828-832.ArticlePDF
- 29. McQueen MM, Gelbke MK, Wakefield A, Will EM, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br, 2008;90:66-71.Article
- 30. Lee JI, Lee YS, Cho SB, et al. Modified fluoroscopic imaging technique for the central screw placement in percutaneous screw fixation of scaphoid fracture. J Trauma, 2010;68:616-619.Article
- 31. Haisman JM, Rohde RS, Weiland AJ. American Academy of Orthopaedic Surgeons. Acute fractures of the scaphoid. J Bone Joint Surg Am, 2006;88:2750-2758.Article
- 32. Pao VS, Chang J. Scaphoid nonunion: diagnosis and treatment. Plast Reconstr Surg, 2003;112:1666-1676. quiz 1677discussion 1678-1679. Article
- 33. Dias JJ. Definition of union after acute fracture and surgery for fracture nonunion of the scaphoid. J Hand Surg Br, 2001;26:321-325.ArticlePDF
- 34. Singh AK, Davis TR, Dawson JS, Oni JA, Downing ND. Gadolinium enhanced MR assessment of proximal fragment vascularity in nonunions after scaphoid fracture: does it predict the outcome of reconstructive surgery? J Hand Surg Br, 2004;29:444-448.ArticlePDF
- 35. Oka K, Moritomo H, Murase T, Goto A, Sugamoto K, Yoshikawa H. Patterns of carpal deformity in scaphoid nonunion: a 3-dimensional and quantitative analysis. J Hand Surg Am, 2005;30:1136-1144.Article
- 36. Oka K, Murase T, Moritomo H, Goto A, Sugamoto K, Yoshikawa H. Patterns of bone defect in scaphoid nonunion: a 3-dimensional and quantitative analysis. J Hand Surg Am, 2005;30:359-365.Article
- 37. Mahmoud M, Koptan W. Percutaneous screw fixation without bone grafting for established scaphoid nonunion with substantial bone loss. J Bone Joint Surg Br, 2011;93:932-936.ArticlePDF
- 38. Capo JT, Shamian B, Rizzo M. Percutaneous screw fixation without bone grafting of scaphoid non-union. Isr Med Assoc J, 2012;14:729-732.Article
- 39. Jiranek WA, Ruby LK, Millender LB, Bankoff MS, Newberg AH. Long-term results after Russe bone-grafting: the effect of malunion of the scaphoid. J Bone Joint Surg Am, 1992;74:1217-1228.Article
- 40. Fernandez DL. A technique for anterior wedge-shaped grafts for scaphoid nonunions with carpal instability. J Hand Surg Am, 1984;9:733-737.Article
- 41. Merrell GA, Wolfe SW, Slade JF 3rd. Treatment of scaphoid nonunions: quantitative meta-analysis of the literature. J Hand Surg Am, 2002;27:685-691.Article
- 42. Stark HH, Rickard TA, Zemel NP, Ashworth CR. Treatment of ununited fractures of the scaphoid by iliac bone grafts and Kirschner-wire fixation. J Bone Joint Surg Am, 1988;70:982-991.Article
- 43. Finsen V, Hofstad M, Haugan H. Most scaphoid non-unions heal with bone chip grafting and Kirschner-wire fixation. Thirty-nine patients reviewed 10 years after operation. Injury, 2006;37:854-859.Article
- 44. Tambe AD, Cutler L, Stilwell J, Murali SR, Trail IA, Stanley JK. Scaphoid non-union: the role of vascularized grafting in recalcitrant non-unions of the scaphoid. J Hand Surg Br, 2006;31:185-190.ArticlePDF
- 45. Kawai H, Yamamoto K. Pronator quadratus pedicled bone graft for old scaphoid fractures. J Bone Joint Surg Br, 1988;70:829-831.ArticlePDF
- 46. Fernandez DL, Eggli S. Non-union of the scaphoid. Revascularization of the proximal pole with implantation of a vascular bundle and bone-grafting. J Bone Joint Surg Am, 1995;77:883-893.Article
- 47. Zaidemberg C, Siebert JW, Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg Am, 1991;16:474-478.Article
- 48. Gabl M, Reinhart C, Lutz M, et al. Vascularized bone graft from the iliac crest for the treatment of nonunion of the proximal part of the scaphoid with an avascular fragment. J Bone Joint Surg Am, 1999;81:1414-1428.Article
- 49. Jones DB Jr, Moran SL, Bishop AT, Shin AY. Free-vascularized medial femoral condyle bone transfer in the treatment of scaphoid nonunions. Plast Reconstr Surg, 2010;125:1176-1184.Article
- 50. Steinmann SP, Bishop AT, Berger RA. Use of the 1,2 intercompartmental supraretinacular artery as a vascularized pedicle bone graft for difficult scaphoid nonunion. J Hand Surg Am, 2002;27:391-401.Article
- 51. Straw RG, Davis TR, Dias JJ. Scaphoid nonunion: treatment with a pedicled vascularized bone graft based on the 1,2 intercompartmental supraretinacular branch of the radial artery. J Hand Surg Br, 2002;27:413. ArticlePDF
- 52. Chang MA, Bishop AT, Moran SL, Shin AY. The outcomes and complications of 1,2-intercompartmental supraretinacular artery pedicled vascularized bone grafting of scaphoid nonunions. J Hand Surg Am, 2006;31:387-396.Article
- 53. Waitayawinyu T, McCallister WV, Katolik LI, Schlenker JD, Trumble TE. Outcome after vascularized bone grafting of scaphoid nonunions with avascular necrosis. J Hand Surg Am, 2009;34:387-394.Article
- 54. Braga-Silva J, Peruchi FM, Moschen GM, Gehlen D, Padoin AV. A comparison of the use of distal radius vascularised bone graft and non-vascularised iliac crest bone graft in the treatment of non-union of scaphoid fractures. J Hand Surg Eur Vol, 2008;33:636-640.ArticlePDF
- 55. Cooney WP. Bone-grafting techniques for scaphoid nonunion. Tech Hand Up Extrem Surg, 1997;1:148-167.Article
- 56. Sakai K, Doi K, Kawai S. Free vascularized thin corticoperiosteal graft. Plast Reconstr Surg, 1991;87:290-298.Article
- 57. Jones DB Jr, Bürger H, Bishop AT, Shin AY. Treatment of scaphoid waist nonunions with an avascular proximal pole and carpal collapse. A comparison of two vascularized bone grafts. J Bone Joint Surg Am, 2008;90:2616-2625.Article
REFERENCES
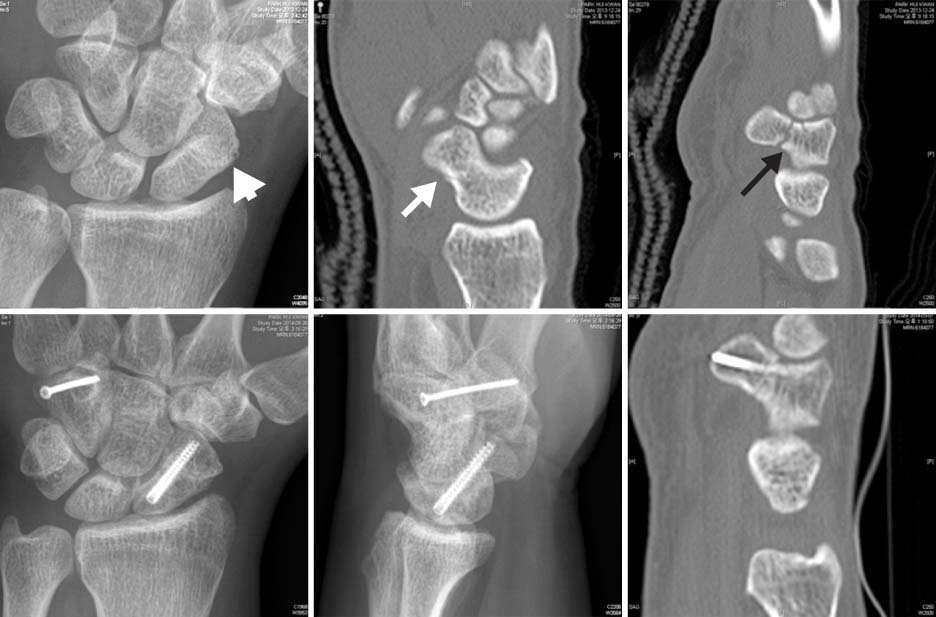
Computed tomography (CT) scan is a very useful diagnostic tool in detection of scaphoid fracture. In a plain X-ray of the wrist, a scaphoid fracture is suspected (white arrow head). CT scan shows cortical breakage in the scaphoid volar aspect (white arrow) and an occult fracture in the hamate hook base (black arrow). In below line photos, the fractures of scaphoid and hamate are fixed with a headless compression screw and a 2 mm screw, respectively, using the dorsal percutaneous technique.
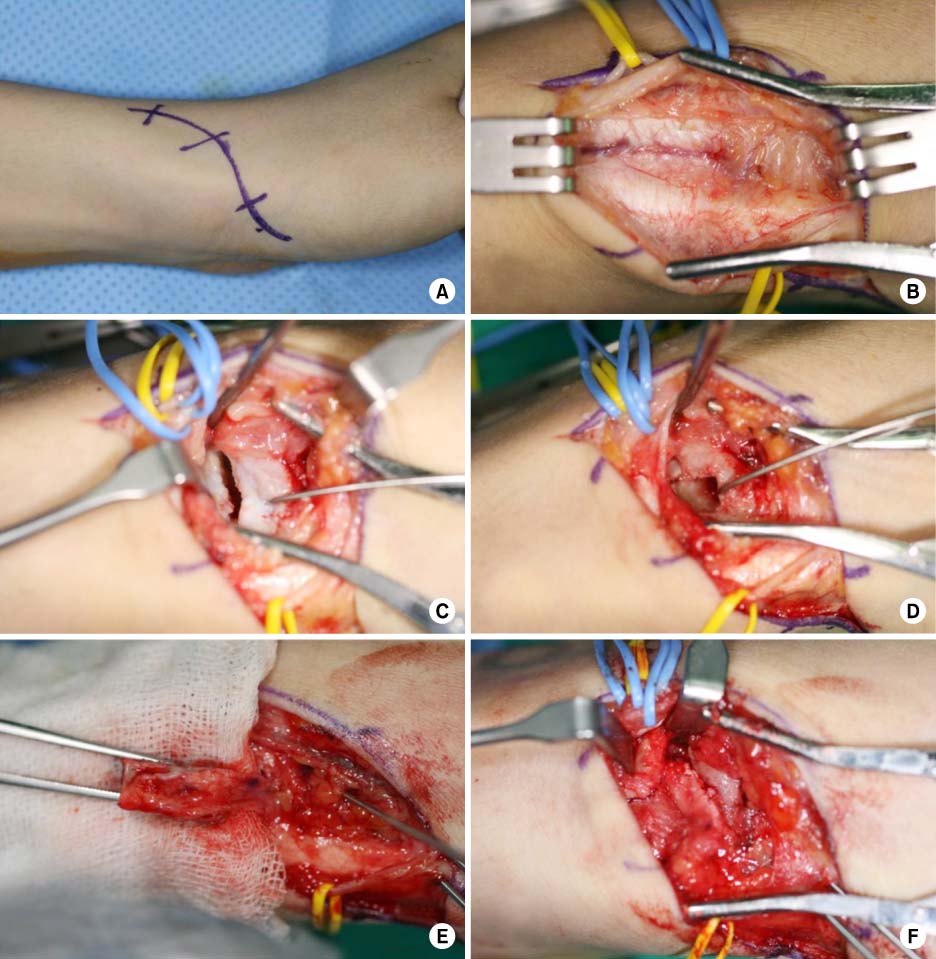
Percutaneous headless compression screw fixation using a palmar approach. There are two techniques in percutaneous headless screw fixation using a volar approach; one is the central method which requires rongeuring the volar side of the trapezium for centralization of distal insertion screw (upper photo line), the other is the oblique method in which screw fixation starts obliquely in order to avoid injury to trapezium (lower photo line).

Surgical procedures for 1,2 intercompartmental supraretinacular artery (1,2-ICSRA) pedicled bone graft (courtesy of Prof. Jong Woong Park). (A) Incision. (B) 1,2-ICSRA identification. (C) Identification of the fracture site. (D) Making a slot for the bone graft. (E) 1,2-ICSRA pedicled bone fragment harvesting. (F) Insertion of bone graft and fixation.
1,2 intercompartmental supraretinacular artery (1,2-ICSRA) pedicled bone graft (courtesy of Prof. Seok Hwan Song). (A) Scaphoid nonunion with atrophic change of the proximal fragment. (B) Postoperative X-ray showing focal radiolucency on the distal radius by donor bone harvesting (arrow). (C) Last follow-up X-ray showing complete union of scaphoid.

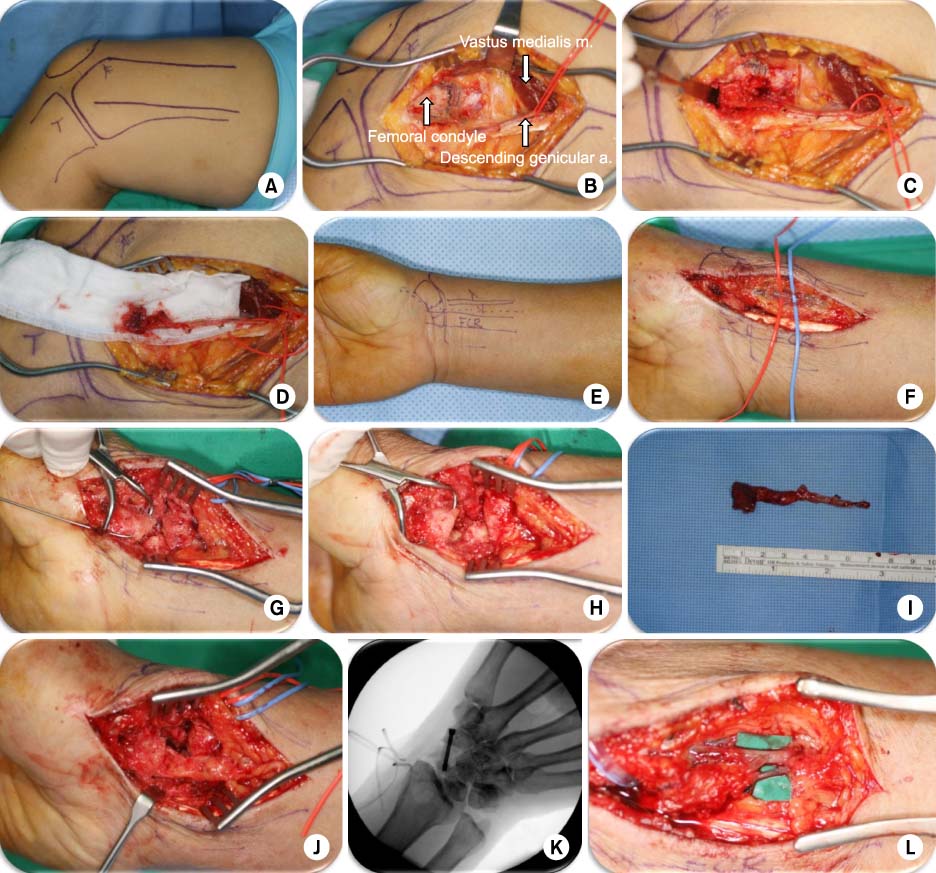
Surgical procedures for medial femoral condyle free vascularized bone graft (courtesy of Prof. Jong Woong Park). (A) Skin incision. (B) Identification of the descending genicular artery (in photo, m: muscle, a: artery). (C, D) Pedicled donor bone harvesting. (E) Recipient incision line. (F) Finding and dissecting radial artery and vein for anastomosis. (G) Finding nonunion site and curettage of fibrotic tissue. (H) Removing cystic and sclerotic portion of both ends with a saw. (I, J) Harvested donor bone trimming according to the defect and inserted into the gap. (K) Graft insetting and fixation with a headless screw. (L) End-to-side anastomosis with radial artery and end-to-end anastomosis with venae comitantes or cephalic vein.
Medial femoral condyle free vascularized bone graft (courtesy of Prof. Jong Woong Park). (A) Scaphoid nonunion with failed 1,2 intercompartmental supraretinacular artery (1,2-ICSRA) vascularized bone graft. (B) Computed tomography (CT) scan showing cystic change, sclerosis and avascular necrosis suspected in the proximal fragment. (C) Wrist lateral view showing dorsal intercalated segmental instability. (D) CT scan showing scaphoid humpback deformity (arrow). (E, F) Postopreative 10 weeks, the X-ray showing successful scaphoid union with scaphoid length restored and humpback deformity corrected.

| Clinical test | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Effusion | 50 | 91 |
| Tenderness on scaphoid tubercle | 87 | 57 |
| Snuff box tenderness | 90 | 40 |
| Scaphoid compression test | 94 | 92 |
| Combined | 100 | 74 |
Next Evaluation in Case of the Highly Suspected Patient with a Negative Simple X-Ray
| Item | Finding | Describing |
|---|---|---|
| Short arm thumb spica splint, after 2 weeks, rechecking simple Xrays16) | Bone resorption or early callus formation adjacent to the fracture site | Low cost, possible time wasting |
| High-resolution ultrasound17,18) | Cortical step-off, cortical interruption, radiocarpal effusion, scaphotrapeziotrapezoidal joint effusion | Sensitivity 78%, specificity 89%, relatively low cost, early detection |
| Bone scan19,20) | Hot uptake | Sensitivity 100%, specificity 90%, useful in multiple fracture-patient and unconsciousness patient |
| Computed tomography21,22) | The better diagnostic performance in reformations along the long axis of the scaphoid than the planes of the wrist | Very effective in detection for nondisplaced scaphoid fractures, useful in evaluation for scaphoid union or eformation or scaphoid nonunion status |
| Magnetic resonance imaging23,24) | Acute fracture, normal or decreased signal in T1 and increased signal in T2; nonunion or avascular necrosis, decreased signal in T1 and T2 | Sensitivity 100%, specificity 90%, useful in detection for ligament injuries or other concomitant injuries |
Criteria for Unstable Scaphoid Fracture (by Cooney)
Data from the article of Haisman et al. (J Bone Joint Surg Am 2006;88:2750-2758).31)
Comparison of Surgical Approach
Figure & Data
REFERENCES
Citations



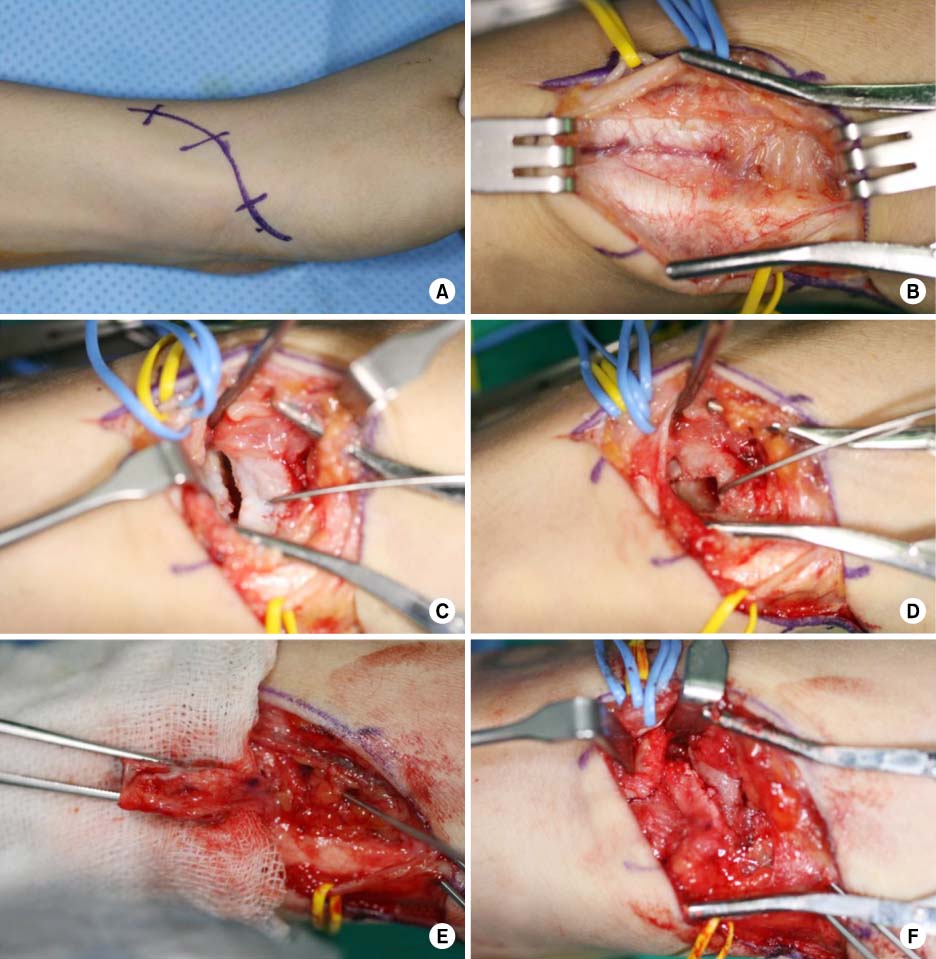

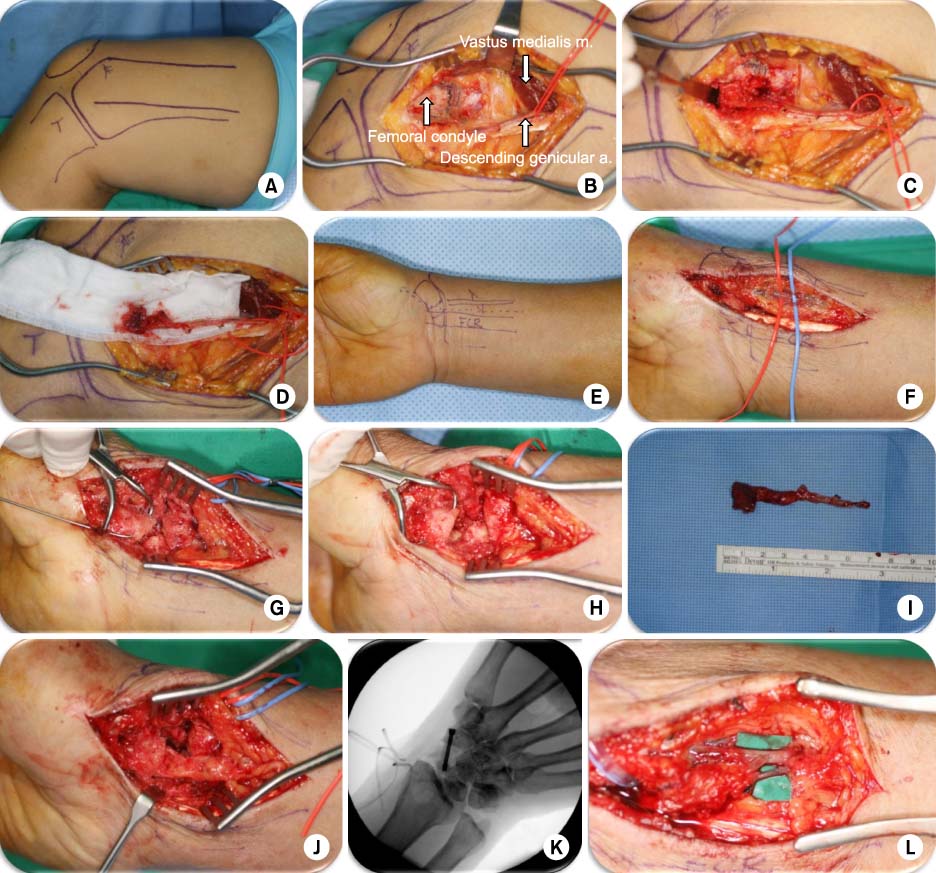

Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
| Clinical test | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Effusion | 50 | 91 |
| Tenderness on scaphoid tubercle | 87 | 57 |
| Snuff box tenderness | 90 | 40 |
| Scaphoid compression test | 94 | 92 |
| Combined | 100 | 74 |
Next Evaluation in Case of the Highly Suspected Patient with a Negative Simple X-Ray
| Item | Finding | Describing |
|---|---|---|
| Short arm thumb spica splint, after 2 weeks, rechecking simple Xrays16) | Bone resorption or early callus formation adjacent to the fracture site | Low cost, possible time wasting |
| High-resolution ultrasound17,18) | Cortical step-off, cortical interruption, radiocarpal effusion, scaphotrapeziotrapezoidal joint effusion | Sensitivity 78%, specificity 89%, relatively low cost, early detection |
| Bone scan19,20) | Hot uptake | Sensitivity 100%, specificity 90%, useful in multiple fracture-patient and unconsciousness patient |
| Computed tomography21,22) | The better diagnostic performance in reformations along the long axis of the scaphoid than the planes of the wrist | Very effective in detection for nondisplaced scaphoid fractures, useful in evaluation for scaphoid union or eformation or scaphoid nonunion status |
| Magnetic resonance imaging23,24) | Acute fracture, normal or decreased signal in T1 and increased signal in T2; nonunion or avascular necrosis, decreased signal in T1 and T2 | Sensitivity 100%, specificity 90%, useful in detection for ligament injuries or other concomitant injuries |
Criteria for Unstable Scaphoid Fracture (by Cooney)
| Item | Criteria |
|---|---|
| Displacement or step-off | >1 mm |
| Angular displacement | >10° |
| Comminuted fracture | |
| Scapholunate angle | >60° |
| Radiolunate angle | >15° |
| Intra-scaphoid angle in wrist postero-anterior view | >40° |
| Intra-scaphoid angle in wrist lateral view | >30° |
Data from the article of Haisman et al. (J Bone Joint Surg Am 2006;88:2750-2758).31)
Comparison of Surgical Approach
| Comparison point | Volar approach | Dorsal approach |
|---|---|---|
| Scaphoid circulation preserving | Superior | Inferior |
| Applicable fracture sites | Fractures in scaphoid waist and distal, humpback deformity correction | Fracture in scaphoid proximal |
| Screw fixation along scaphoid long axis center | Relatively difficult (partial removal of trapezium volar portion) | Easy |
| Radiocarpal ligament injury | Yes | No |
Data from the article of Haisman et al. (J Bone Joint Surg Am 2006;88:2750-2758).

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

