Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 33(4); 2020 > Article
- Review Article Tendon Healing: A Review of Basic Science and Current Progress
- Young Woo Kwon, Pei Wei Wang, Jun-Ku Lee
-
Journal of Musculoskeletal Trauma 2020;33(4):227-237.
DOI: https://doi.org/10.12671/jkfs.2020.33.4.227
Published online: October 31, 2020
2Department of Orthopedic Surgery, Inje University Seoul Paik Hospital, Seoul, Korea
- 2,645 Views
- 80 Download
- 0 Crossref
- 0 Scopus
Abstract
The tendon connects the muscles to the bones and transmits the loads generated by the muscles to the bones to move the joints, support the joints, and provide stability to the joints. Approximately 30% of patients complaining of musculoskeletal pain are associated with tendon disease, and approximately 50% of musculoskeletal injuries are caused by a tendon injury. Despite this frequent treatment of tendon damage, studies on the basic biology that provide scientific evidence for treatment, such as development, tendon injury, and healing, are still very limited. This review first summarizes the classification and composition of the tendon identified so far, the surrounding tissue, and the blood supply to the tendon. The limitations of the tendon recovery process after a tendon injury are also discussed. Finally, this review examines ways to improve tendon recovery and the biological approaches and tissue engineering that have been currently studied. In conclusion, innovative progress in promoting tendon healing has not been achieved despite the many advances in the basic structure of the tendon, and the cell and regulatory molecular factors involved in tendon recovery. Biological approaches and tissue engineering, which have become a recent issue, have shown many possibilities for the recovery of damaged cases, but further research will be needed until clinical application.
Published online Oct 22, 2020.
https://doi.org/10.12671/jkfs.2020.33.4.227
Tendon Healing: A Review of Basic Science and Current Progress
Abstract
The tendon connects the muscles to the bones and transmits the loads generated by the muscles to the bones to move the joints, support the joints, and provide stability to the joints. Approximately 30% of patients complaining of musculoskeletal pain are associated with tendon disease, and approximately 50% of musculoskeletal injuries are caused by a tendon injury. Despite this frequent treatment of tendon damage, studies on the basic biology that provide scientific evidence for treatment, such as development, tendon injury, and healing, are still very limited. This review first summarizes the classification and composition of the tendon identified so far, the surrounding tissue, and the blood supply to the tendon. The limitations of the tendon recovery process after a tendon injury are also discussed. Finally, this review examines ways to improve tendon recovery and the biological approaches and tissue engineering that have been currently studied. In conclusion, innovative progress in promoting tendon healing has not been achieved despite the many advances in the basic structure of the tendon, and the cell and regulatory molecular factors involved in tendon recovery. Biological approaches and tissue engineering, which have become a recent issue, have shown many possibilities for the recovery of damaged cases, but further research will be needed until clinical application.
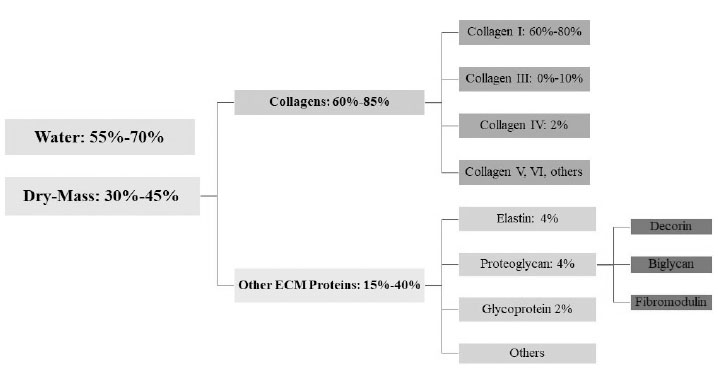
Fig. 1
Tendon composition. ECM: extracellular matrix.
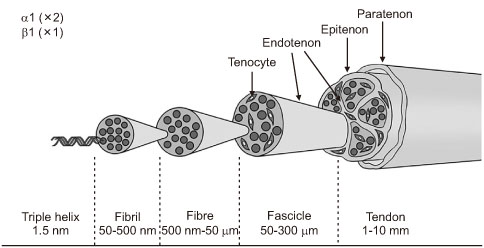
Fig. 2
Tendon structure.
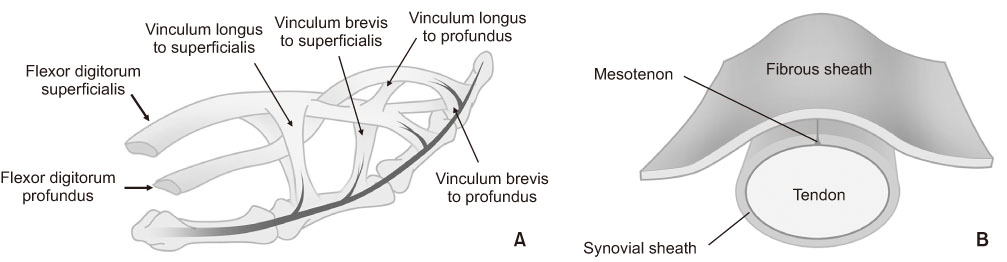
Fig. 3
Extrinsic direct blood supply through the Vincular system (A) and Mesotenon (B).
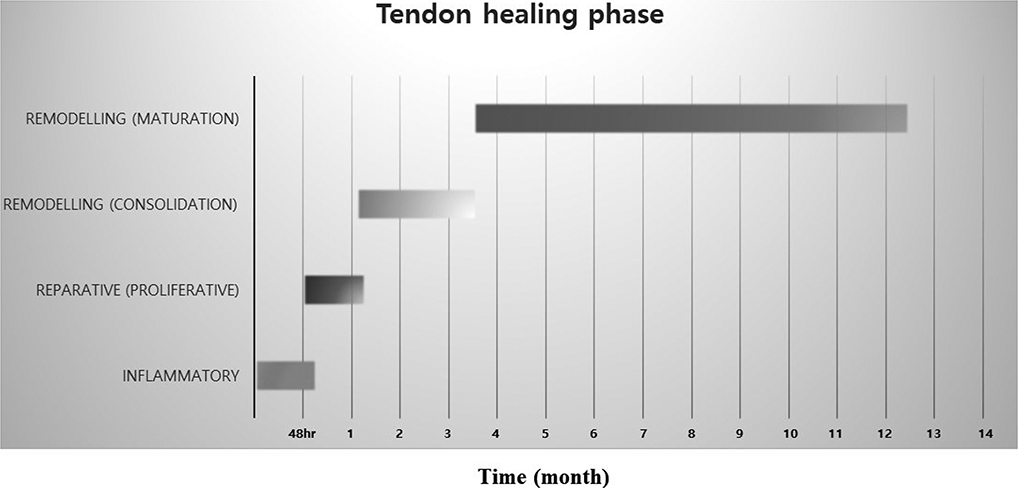
Fig. 4
Tendon repair process in humans. The healing of ruptured tendons passes through three main phases, inflammatory, proliferative, and remodeling phase, which contains the distinctive cell and molecular cascades. These phases overlap, and their duration depends upon the location and severity of the tendon injury.
Financial support:None.
Conflict of interests:None.
References
-
Bordoni B, Varacallo M. Anatomy, tendons. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan; [updated 2020 Jul 31]. [cited 2020 Jun 1].Available from: https://www.ncbi.nlm.nih.gov/books/NBK513237/.
-
-
Frank CB, Shrive NG, Lo IKY, Hart DA. Form and function of tendon and ligament. In: Einhorn TA, O'Keefe RJ, Buckwalter JA, editors. Orthopaedic basic science: foundations of clinical practice. 3rd ed. Rosemont: American Academy of Orthopaedic Surgeons; 2007. pp. 191-222.
-
-
Singer G, Ebramzadeh E, Jones NF, Meals R. Use of the Taguchi method for biomechanical comparison of flexor-tendon-repair techniques to allow immediate active flexion. A new method of analysis and optimization of technique to improve the quality of the repair. J Bone Joint Surg Am 1998;80:1498–1506.
-

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS


 Cite
Cite

