Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 25(4); 2012 > Article
-
Original Article
- Treatment for Bone Defect of Open Tibial Fractures by Using Intramedullary Nail Fixation with Autogenous Iliac Bone Graft
- Hyub Sakong, M.D., Ki Cheor Bae, M.D., Chul Hyun Cho, M.D., Kyung Jae Lee, M.D., Eun Seok Son, M.D., Du Han Kim, M.D.
-
Journal of the Korean Fracture Society 2012;25(4):288-294.
DOI: https://doi.org/10.12671/jkfs.2012.25.4.288
Published online: October 19, 2012
Department of Orthopedic Surgery, Keimyung University School of Medicine, Daegu, Korea.
- Address reprint requests to: Ki Cheor Bae, M.D. Department of Orthopedic Surgery, Keimyung University School of Medicine, 56, Dalseong-ro, Jung-gu, Daegu 700-712, Korea. Tel: 82-53-250-7729, Fax: 82-53-250-7205, bkc@dsmc.or.kr
• Received: April 18, 2012 • Revised: May 22, 2012 • Accepted: July 10, 2012
Copyright © 2012 The Korean Fracture Society
- 389 Views
- 4 Download
Abstract
-
Purpose
- This study was conducted to evaluate the results of intramedullary nail fixation with autogenous iliac bone graft for defects of bone after tibial fractures.
-
Materials and Methods
- Ten patients with bone defects in tibial fractures who had been treated with intramedullary nail fixation with autogenous iliac bone graft between May 2005 and September 2008 with more than 12 month follow-up were subject to study. Of the 10 patients, 8 were male and 2 were female, and the mean age was 50.2 years (29~76 years). By cause of accident, motor vehicle accidents caused 9 cases, a crush caused 1 case, and the average follow-up period was 21.9 months (12~42 months). Radiologically, we analyzed the union of the bone defect on simple x-ray and clinical evaluation was performed using the estimate method of Mekhali.
-
Results
- This study reveals that there was radiological union in all 10 cases and the mean time to union was 8.4 months (5~18 months). By clinical evaluation according to Mekhali's estimate method, 9 patients had excellent outcomes and 1 patient had limitation of motion in the ankle joint rated as a fair clinical result. None of patients developed complications post-operatively.
-
Conclusion
- Our study demonstrated that the intramedullary nail fixation with autogenous iliac bone graft can be a useful operative method because it can remove external fixators early and reduce complications, and autogenous bones have exceptional osteoconduction, osteoinduction, and bone-forming ability resulting in excellent union of bones.
- 1. Aaron AD, Wiedel JD. Allograft use in orthopedic surgery. Orthopedics, 1994;17:41-48.Article
- 2. Aronson J, Johnson E, Harp JH. Local bone transportation for treatment of intercalary defects by the Ilizarov technique. Biomechanical and clinical considerations. Clin Orthop Relat Res, 1989;(243):71-79.
- 3. Awe SI, Rhyu KH, Lee TH. Short term result of bone marrow and morselized allograft without autogenous bone graft in bone defect. J Korean Musculoskelet Transplant Soc, 2004;4:1-8.
- 4. Blokhuis TJ, Termaat MF, den Boer FC, Patka P, Bakker FC, Haarman HJ. Properties of calcium phosphate ceramics in relation to their in vivo behavior. J Trauma, 2000;48:179-186.Article
- 5. Cattaneo R, Catagni M, Johnson EE. The treatment of infected nonunions and segmental defects of the tibia by the methods of Ilizarov. Clin Orthop Relat Res, 1992;(280):143-152.Article
- 6. Cierny G 3rd, Zorn KE. Segmental tibial defects. Comparing conventional and Ilizarov methodologies. Clin Orthop Relat Res, 1994;(301):118-123.
- 7. Dagher F, Roukoz S. Compound tibial fractures with bone loss treated by the Ilizarov technique. J Bone Joint Surg Br, 1991;73:316-321.ArticlePDF
- 8. Greenwald AS, Boden SD, Goldberg VM, Khan Y, Laurencin CT, Rosier RN. American Academy of Orthopaedic Surgeons. The Committee on Biological Implants. Bone-graft substitutes: facts, fictions, and applications. J Bone Joint Surg Am, 2001;83-A:Suppl 2 Pt 2. 98-103.Article
- 9. Hwang C, Bae JY, Koo KH, et al. A comparative experimental study of allograft and porous hydroxyapatite as bone substitutes. J Korean Orthop Assoc, 2007;42:545-552.Article
- 10. Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res, 1990;(250):8-26.Article
- 11. Jung GH, Jung SH, Kim JD, Cho Y. Allograft transplantation in the treatment of bone defect after bone tumor surgery. J Korean Musculoskelet Transplant Soc, 2006;6:79-87.
- 12. Kang HJ, Kim TK, Kweon SH, Shim DM, Lee SI. The usefulness of hydroxyapatite bone transplantation in treatment of metaphyseal fracture with bone defect. J Korean Musculoskelet Transplant Soc, 2011;11:36-41.
- 13. Karlström G, Olerud S. Percutaneous pin fixation of open tibial fractures. Double-frame anchorage using the Vidal-Adrey method. J Bone Joint Surg Am, 1975;57:915-924.Article
- 14. Keating JF, Simpson AH, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg Br, 2005;87:142-150.ArticlePDF
- 15. Kim HT, Yun PJ, Kim IB, Lee DH, Ahn MY, Chang HK. Osteogenic induction of periosteum-derived stem cells transplanted into rabbit long-bone defects. J Korean Orthop Assoc, 2006;41:353-360.ArticlePDF
- 16. Lee SK, Kim SJ, Chang CH, Jang JD, Park HS, Park JS. Treatment of long tubular bone defect of rabbit using autologous cultured osteoblasts mixed with fibrin. J Korean Orthop Res Soc, 2006;9:29-39.
- 17. Lord CF, Gebhardt MC, Tomford WW, Mankin HJ. Infection in bone allografts. Incidence, nature, and treatment. J Bone Joint Surg Am, 1988;70:369-376.Article
- 18. Marsh JL, Prokuski L, Biermann JS. Chronic infected tibial nonunions with bone loss. Conventional techniques versus bone transport. Clin Orthop Relat Res, 1994;(301):139-146.
- 19. Mekhail AO, Abraham E, Gruber B, Gonzalez M. Bone transport in the management of posttraumatic bone defects in the lower extremity. J Trauma, 2004;56:368-378.Article
- 20. Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am, 1997;79:1464-1480.Article
- 21. Paley D, Maar DC. Ilizarov bone transport treatment for tibial defects. J Orthop Trauma, 2000;14:76-85.Article
- 22. Ring D, Jupiter JB, Gan BS, Israeli R, Yaremchuk MJ. Infected nonunion of the tibia. Clin Orthop Relat Res, 1999;(369):302-311.Article
- 23. Roh JY, Oh CW, Oh JK, et al. Bone transport over the intramedullary nail for defects of long bone. J Korean Fract Soc, 2008;21:37-44.Article
- 24. Song HR, Kale A, Park HB, et al. Comparison of internal bone transport and vascularized fibular grafting for femoral bone defects. J Orthop Trauma, 2003;17:203-211.Article
- 25. Webb LX. New techniques in wound management: vacuum-assisted wound closure. J Am Acad Orthop Surg, 2002;10:303-311.Article
- 26. Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma, 1989;3:192-195.Article
REFERENCES
Fig. 1
A 31-year-old male with Gustilo-Anderson type II open fracture on his right tibia.
(A) Radiograph shows comminuted fracture at distal 1/3 of right tibiofibular shaft.
(B) Immediate postoperative radiography shows defect of boneon the distal tibial shaft.
(C) Two months later, the external fixator was removed and intramedullary nail fixation was done.
(D) A bone defect was detected, so a bone graft was done on the bone defect site.
(E) Five months after the bone graft, a radiograph shows that bony union was achieved.
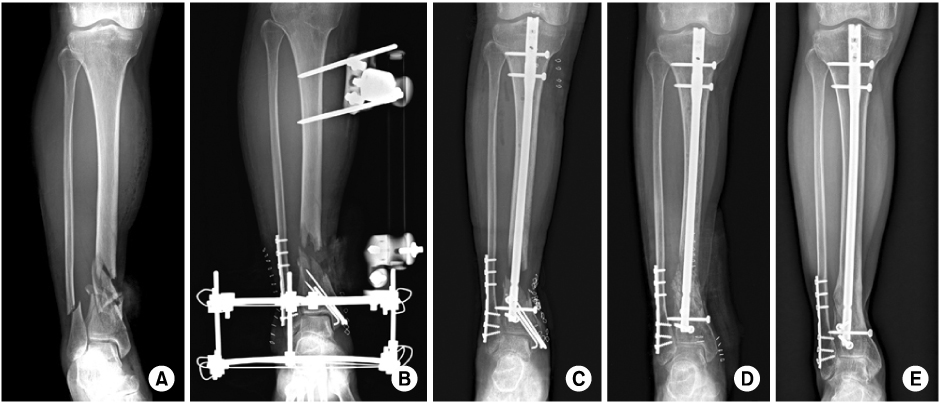
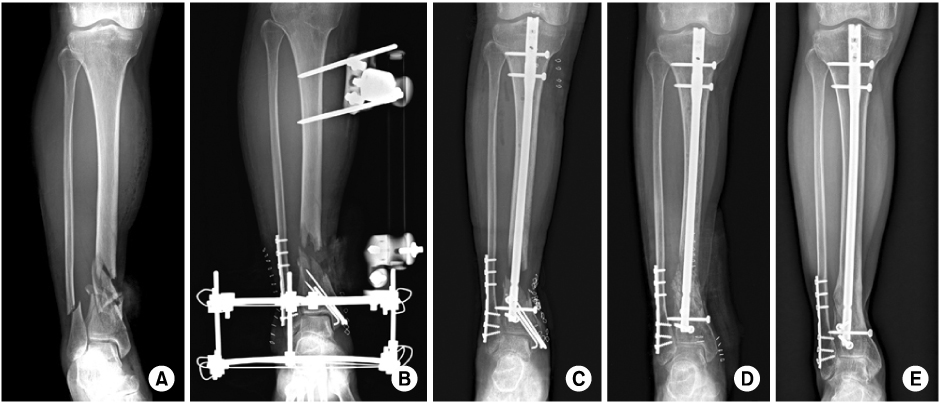
Fig. 2
A 56-year-old female with Gustilo-Anderson type IIIB open fracture on his left tibia.
(A) Radiograph shows comminuted fractures at distal 1/3 of left tibia shaft and lateral malleolus.
(B) Immediate postoperative radiography shows defect of bone on the distal tibial shaft.
(C) Multiple drilling was done for bleeding at the fracture site.
(D) Four months later, the external fixator was removed and intramedullary nail fixation was performed.
(E) A bone defect was detected, so a bone graft was performed on the bone defect site.
(F) Seven months after the bone graft, a radiograph shows that bony union was achieved.
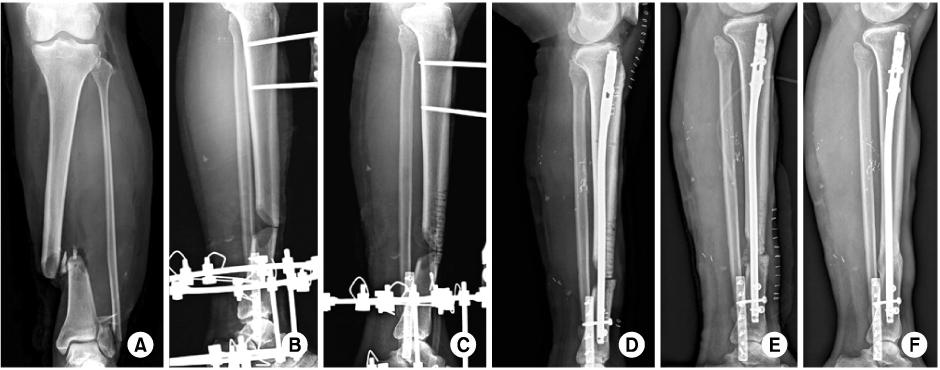
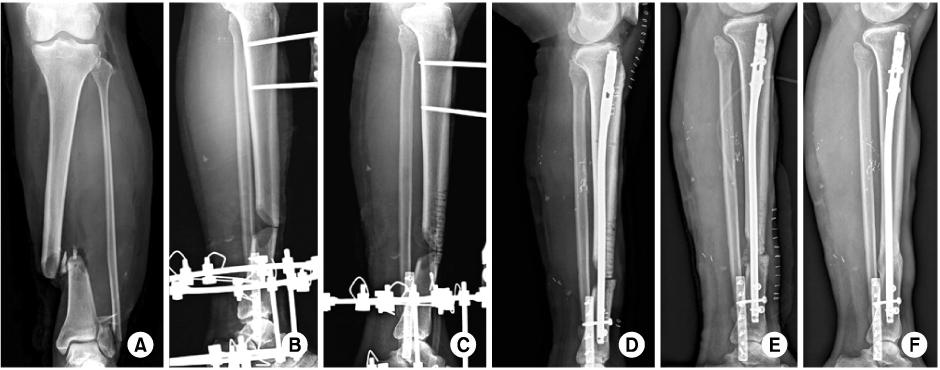
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

Treatment for Bone Defect of Open Tibial Fractures by Using Intramedullary Nail Fixation with Autogenous Iliac Bone Graft
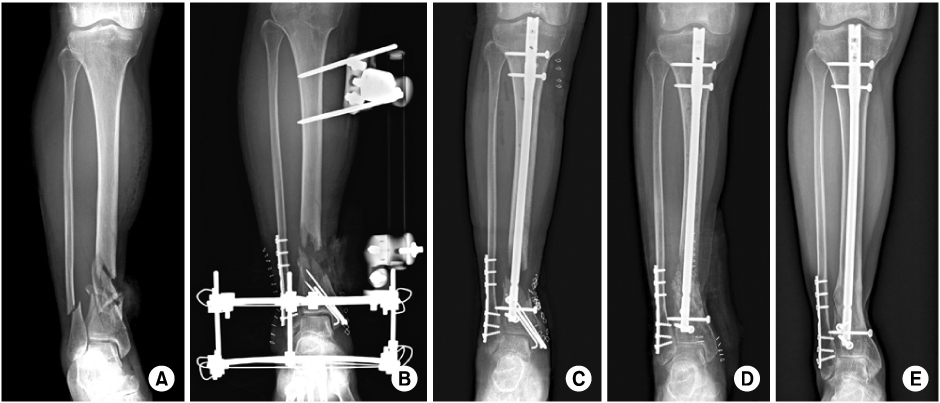
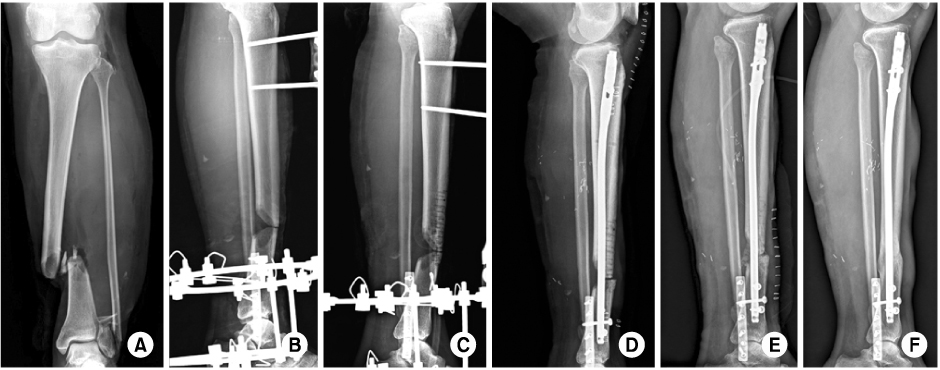
Fig. 1
A 31-year-old male with Gustilo-Anderson type II open fracture on his right tibia.
(A) Radiograph shows comminuted fracture at distal 1/3 of right tibiofibular shaft.
(B) Immediate postoperative radiography shows defect of boneon the distal tibial shaft.
(C) Two months later, the external fixator was removed and intramedullary nail fixation was done.
(D) A bone defect was detected, so a bone graft was done on the bone defect site.
(E) Five months after the bone graft, a radiograph shows that bony union was achieved.
Fig. 2
A 56-year-old female with Gustilo-Anderson type IIIB open fracture on his left tibia.
(A) Radiograph shows comminuted fractures at distal 1/3 of left tibia shaft and lateral malleolus.
(B) Immediate postoperative radiography shows defect of bone on the distal tibial shaft.
(C) Multiple drilling was done for bleeding at the fracture site.
(D) Four months later, the external fixator was removed and intramedullary nail fixation was performed.
(E) A bone defect was detected, so a bone graft was performed on the bone defect site.
(F) Seven months after the bone graft, a radiograph shows that bony union was achieved.
Fig. 1
Fig. 2
Treatment for Bone Defect of Open Tibial Fractures by Using Intramedullary Nail Fixation with Autogenous Iliac Bone Graft
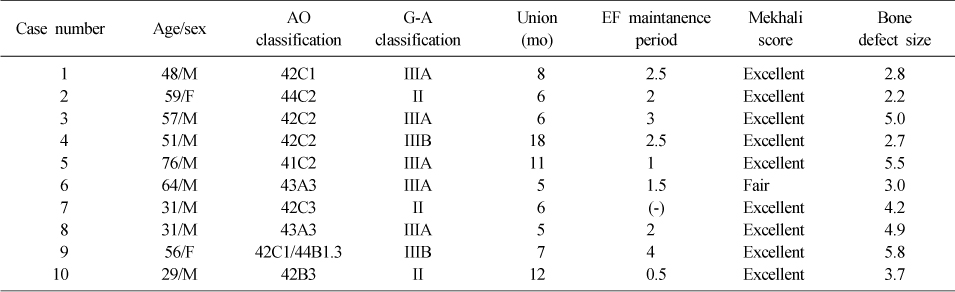
Summary of Cases
G-A classification: Gustilo and Anderson classification, EF: External fixator, M: Male, F: Female.
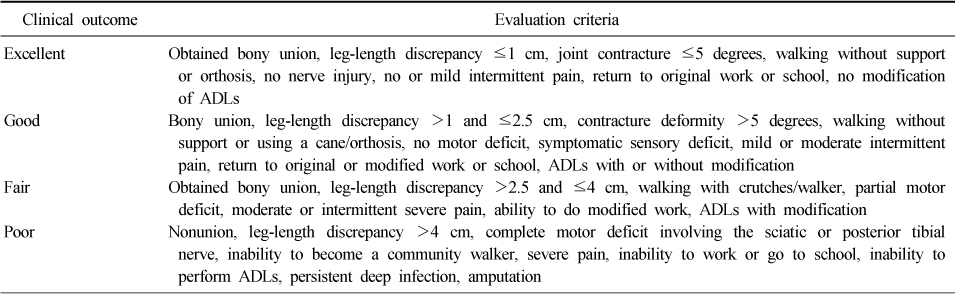
Clinical Outcome Evaluation Criteria
ADLs: Activities of daily living.
Table 1
Summary of Cases
G-A classification: Gustilo and Anderson classification, EF: External fixator, M: Male, F: Female.
Table 2
Clinical Outcome Evaluation Criteria
ADLs: Activities of daily living.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

