Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 25(4); 2012 > Article
-
Original Article
- Comparison of Results of Minimally Invasive Plate Osteosynthesis according to Types of Locking Plate in Distal Femoral Fractures
- Oog Jin Shon, M.D., Ph.D., Moon Soo Kwon, M.D., Chul Hyun Park, M.D., Ph.D.
-
Journal of the Korean Fracture Society 2012;25(4):269-276.
DOI: https://doi.org/10.12671/jkfs.2012.25.4.269
Published online: October 19, 2012
Department of Orthopedic Surgery, Yeungnam University College of Medicine, Daegu, Korea.
- Address reprint requests to: Chul Hyun Park, M.D., Ph.D. Department of Orthopedic Surgery, Yeungnam University Medical Center, 170, Hyeonchung-ro, Nam-gu, Daegu 705-717, Korea. Tel: 82-53-620-3640, Fax: 82-53-628-4240, chpark77@naver.com
• Received: July 28, 2011 • Revised: January 9, 2012 • Accepted: May 20, 2012
Copyright © 2012 The Korean Fracture Society
- 797 Views
- 0 Download
- 2 Crossref
Abstract
-
Purpose
- To compare results of minimally invasive plate osteosynthesis using a locking compression plate and a periarticular locking plate in distal femur fractures.
-
Materials and Methods
- We retrospectively reviewed 31 consecutive femoral fractures who treated by minimally invasive plate osteosynthesis from April 2006 to May 2009. Sixteen patients were treated using a locking compression plate (group A) and 15 patients were treated using a periarticular locking plate (group B).
-
Results
- The mean operation time was 78 minutes and 76 minutes (p=0.273), and the mean radiation exposure time was 1.9 minutes and 2.3 minutes (p=0.001) in the group A and B, respectively. The plate bending during operation was performed in 4 cases of group A. The knee range of motion was 117.5° and 118.2° (p=0.825), and the Lysholm score was 81.3 and 81.8 (p=0.723) in the group A and B, respectively. Schazker criteria showed more than good grade in 93.8% of group A and in 93.3% of group B (p=1.0).
-
Conclusion
- No significant differences in clinical results were observed between the two groups. However, a lower anatomical compliance was showed in the locking compression plate, and a higher risk of radiation exposure was showed in the periarticular locking plate.
- 1. Allen WC, Piotrowski G, Burstein AH, Frankel VH. Biomechanical principles of intramedullary fixation. Clin Orthop Relat Res, 1968;60:13-20.
- 2. Altenberg AR, Shorkey RL. Blade-plate fixation in non-union and in complicated fractures of the supracondylar region of the femur. J Bone Joint Surg Am, 1949;31A:312-316.
- 3. Arneson TJ, Melton LJ 3rd, Lewallen DG, O'Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop Relat Res, 1988;(234):188-194.
- 4. Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur Less Invasive Stabilization System (LISS). Injury, 2001;32:Suppl 3. SC24-SC31.
- 5. Giles JB, DeLee JC, Heckman JD, Keever JE. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. J Bone Joint Surg Am, 1982;64:864-870.
- 6. Guy P, Krettek C, Mannss J, Whittall KP, Schandelmaier P, Tscherne H. CT-based analysis of the geometry of the distal femur. Injury, 1998;29:Suppl 3. C16-C21.
- 7. Henry SL, Trager S, Green S, Seligson D. Management of supracondylar fractures of the femur with the GSH intramedullary nail: preliminary report. Contemp Orthop, 1991;22:631-640.
- 8. Kim SS, Sohn SK, Kim KT, et al. Results of operative treatment of distal femoral fracture. J Korean Fract Soc, 2005;18:232-237.
- 9. Kolb W, Guhlmann H, Windisch C, Marx F, Kolb K, Koller H. Fixation of distal femoral fractures with the Less Invasive Stabilization System: a minimally invasive treatment with locked fixed-angle screws. J Trauma, 2008;65:1425-1434.
- 10. Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (L.I.S.S.): the technique and early results. Injury, 2001;32:Suppl 3. SC32-SC47.
- 11. Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma, 2004;18:509-520.
- 12. Krettek C, Schandelmaier P, Miclau T, Bertram R, Holmes W, Tscherne H. Transarticular joint reconstruction and indirect plate osteosynthesis for complex distal supracondylar femoral fractures. Injury, 1997;28:Suppl 1. A31-A41.
- 13. Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury, 1997;28:Suppl 1. A20-A30.
- 14. Lucas SE, Seligson D, Henry SL. Intramedullary supracondylar nailing of femoral fractures. A preliminary report of the GSH supracondylar nail. Clin Orthop Relat Res, 1993;(296):200-206.
- 15. Martinet O, Cordey J, Harder Y, Maier A, Bühler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury, 2000;31:Suppl 3. c62-c63.
- 16. Oh JK, Oh CW, Park SH, Roh KJ, Jeong CW. Conformity of the LCP-DF (locking compression plate-distal femur) in Korean adult femur: a cadaver study. J Korean Fract Soc, 2005;18:399-404.
- 17. Schütz M, Müller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury, 2001;32:Suppl 3. SC48-SC54.
- 18. Schütz M, Südkamp NP. Revolution in plate osteosynthesis: new internal fixator systems. J Orthop Sci, 2003;8:252-258.
- 19. Shahcheraghi GH, Doroodchi HR. Supracondylar fracture of the femur: closed or open reduction? J Trauma, 1993;34:499-502.
- 20. Shewring DJ, Meggitt BF. Fractures of the distal femur treated with the AO dynamic condylar screw. J Bone Joint Surg Br, 1992;74:122-125.PDF
- 21. Stoffel K, Lorenz KU, Kuster MS. Biomechanical considerations in plate osteosynthesis: the effect of plate-to-bone compression with and without angular screw stability. J Orthop Trauma, 2007;21:362-368.
- 22. Stover M. Distal femoral fractures: current treatment, results and problems. Injury, 2001;32:Suppl 3. SC3-SC13.
- 23. Syed AA, Agarwal M, Giannoudis PV, Matthews SJ, Smith RM. Distal femoral fractures: long-term outcome following stabilisation with the LISS. Injury, 2004;35:599-607.
REFERENCES
Fig. 1
(A) Patients were placed supine and the uninjured leg was in the lowered position for fluoroscopy.
(B) Supracondylar towel bumps made of rolled surgical towels were placed in the area posterior to the supracondylar region.
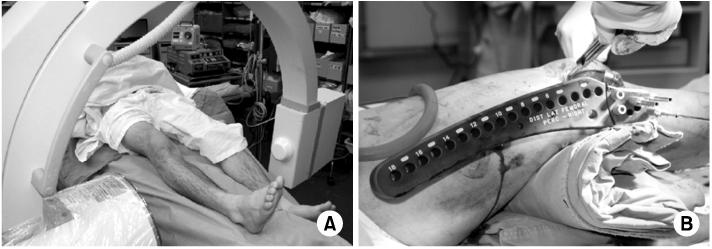
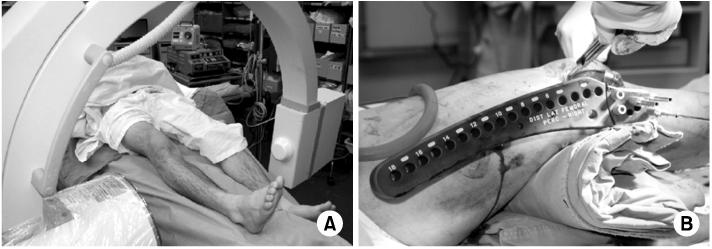
Fig. 2
(A) For the locking compression plate in distal femur procedure, we used a guiding block for distal fixation.
(B) For the Zimmer® periarticular locking plate procedure, a Jig system was used.
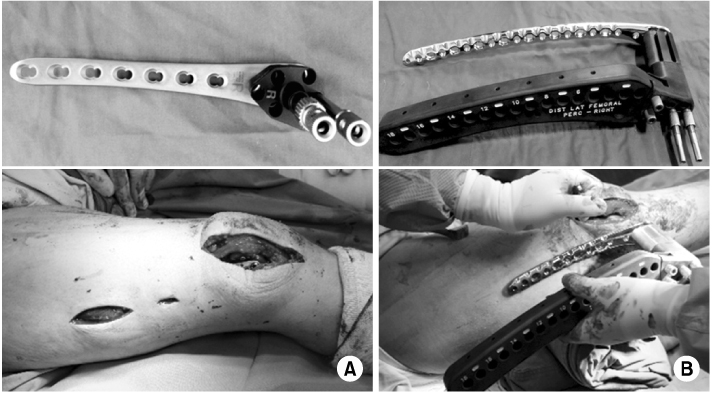
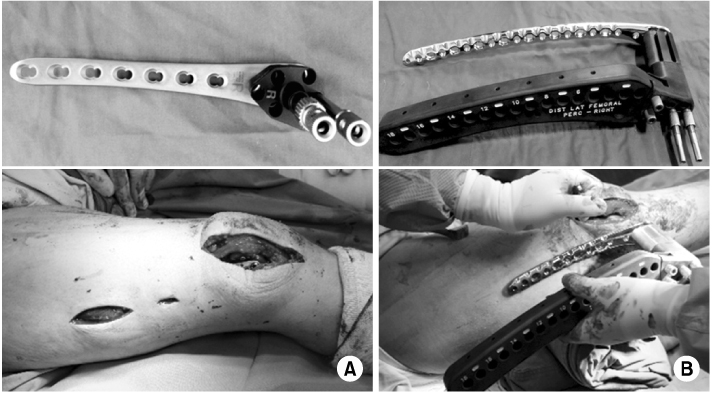
Fig. 3The coronal fracture fragment angle was defined as the angle between the line of the femoral shaft and the distal intercondylar line.
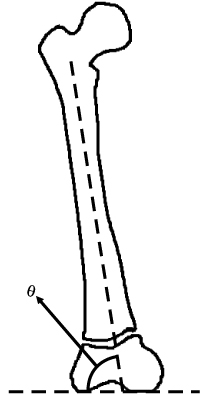
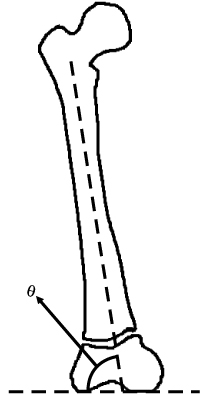
Fig. 4
A 72-year-old woman presented with an AO/OTA type C3 distal femoral fracture on the (A) anterior-posterior and lateral view and (B) 3-dimensional computed tomography.
(C) The fracture was treated with minimally invasive plate osteosynthesis with locking compression plate in distal femur.
(D) The fracture had healed at 19 weeks after the operation.


Fig. 5
A 51-year-old man presented with an AO/OTA type C2 distal femoral fracture on the (A) anterior-posterior and lateral view and (B) 3-dimensional computed tomography.
(C) The fracture was treated with minimally invasive plate osteosynthesis with Zimmer® periarticular locking plate.
(D) The fracture was healed at 18 weeks after the operation.


Fig. 6The distal locking screw penetrated the medial femoral cortex in the (A) locking compression plate in distal femur group and (B) Zimmer® periarticular locking plate (ZPLP) group. However, only the ZPLP group complained of pain by screw irritation.


Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Incidence of nonunion after surgery of distal femoral fractures using contemporary fixation device: a meta‐analysis
Byung-Ho Yoon, In Keun Park, Youngwoo Kim, Hyoung-Keun Oh, Suk Kyu Choo, Yerl-Bo Sung
Archives of Orthopaedic and Trauma Surgery.2021; 141(2): 225. CrossRef - The Mid-Term Result after Osteosynthesis of Intra-Articular Fractures of Distal Femur
Sam Guk Park, Jeong Jae Moon, Oog Jin Shon
Journal of the Korean Fracture Society.2016; 29(4): 242. CrossRef
Comparison of Results of Minimally Invasive Plate Osteosynthesis according to Types of Locking Plate in Distal Femoral Fractures
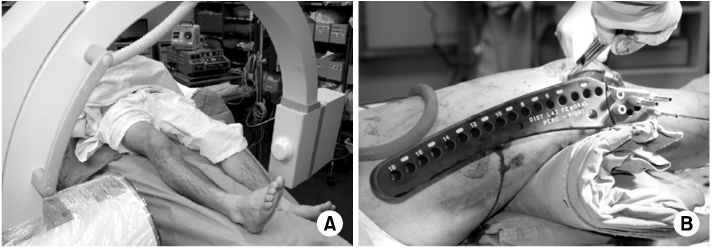
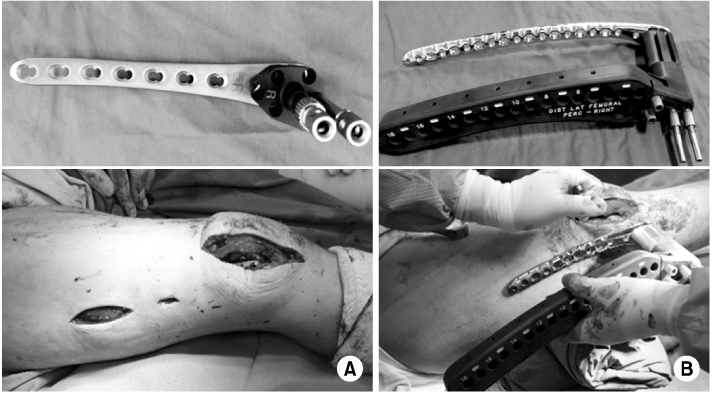
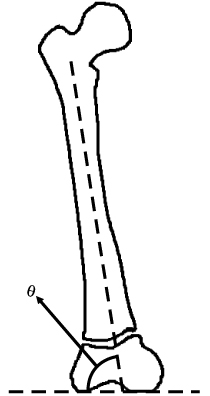


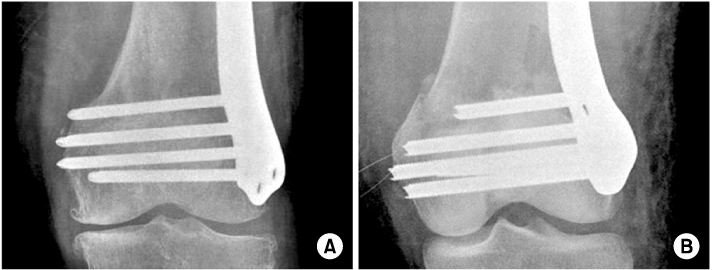
Fig. 1
(A) Patients were placed supine and the uninjured leg was in the lowered position for fluoroscopy.
(B) Supracondylar towel bumps made of rolled surgical towels were placed in the area posterior to the supracondylar region.
Fig. 2
(A) For the locking compression plate in distal femur procedure, we used a guiding block for distal fixation.
(B) For the Zimmer® periarticular locking plate procedure, a Jig system was used.
Fig. 3
The coronal fracture fragment angle was defined as the angle between the line of the femoral shaft and the distal intercondylar line.
Fig. 4
A 72-year-old woman presented with an AO/OTA type C3 distal femoral fracture on the (A) anterior-posterior and lateral view and (B) 3-dimensional computed tomography.
(C) The fracture was treated with minimally invasive plate osteosynthesis with locking compression plate in distal femur.
(D) The fracture had healed at 19 weeks after the operation.
Fig. 5
A 51-year-old man presented with an AO/OTA type C2 distal femoral fracture on the (A) anterior-posterior and lateral view and (B) 3-dimensional computed tomography.
(C) The fracture was treated with minimally invasive plate osteosynthesis with Zimmer® periarticular locking plate.
(D) The fracture was healed at 18 weeks after the operation.
Fig. 6
The distal locking screw penetrated the medial femoral cortex in the (A) locking compression plate in distal femur group and (B) Zimmer® periarticular locking plate (ZPLP) group. However, only the ZPLP group complained of pain by screw irritation.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Comparison of Results of Minimally Invasive Plate Osteosynthesis according to Types of Locking Plate in Distal Femoral Fractures
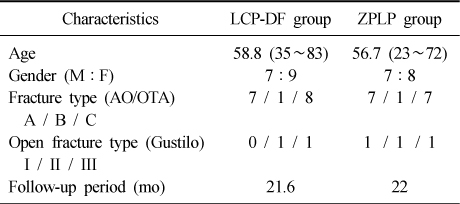
Patient Demographic Data
Values are presented as mean (range) or number. LCP-DF: Locking compression plate in distal femur, ZPLP: Zimmer® periarticular locking plate, M: Male, F: Female.
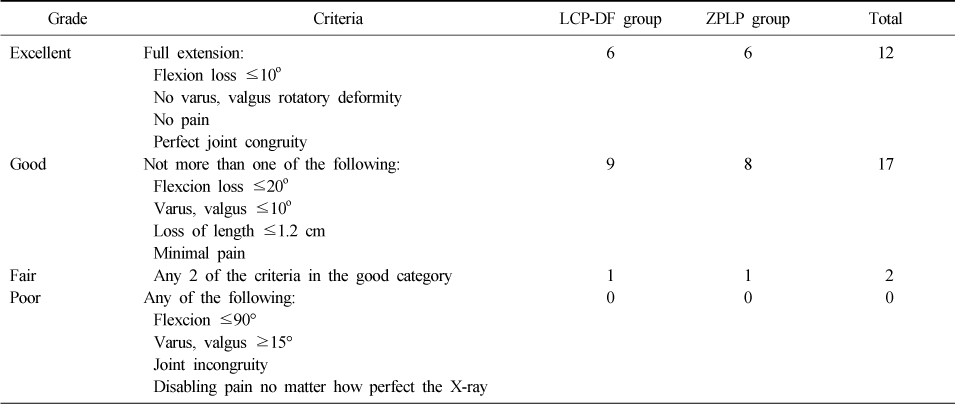
Schatzker Criteria
LCP-DF: Locking compression plate in distal femur, ZPLP: Zimmer® periarticular locking plate.
Table 1
Patient Demographic Data
Values are presented as mean (range) or number. LCP-DF: Locking compression plate in distal femur, ZPLP: Zimmer® periarticular locking plate, M: Male, F: Female.
Table 2
Schatzker Criteria
LCP-DF: Locking compression plate in distal femur, ZPLP: Zimmer® periarticular locking plate.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

