Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 26(1); 2013 > Article
-
Original Article
- Clinical Outcomes of the Tibia Segmental Fractures Treated by Intramedullary Nail Using Various Reduction Techniques
- Oog-Jin Shon, M.D., Ji-Hoon Shin, M.D., Chul-Wung Ha, M.D.
-
Journal of the Korean Fracture Society 2013;26(1):50-55.
DOI: https://doi.org/10.12671/jkfs.2013.26.1.50
Published online: January 17, 2013
Department of Orthopaedic Surgery, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu, Korea.
- Address reprint requests to: Oog-Jin Shon, M.D. Department of Orthopaedic Surgery, Yeungnam University Medical Center, 170, Hyeonchung-ro, Nam-gu, Daegu 705-717, Korea. Tel: 82-53-620-3640, Fax: 82-53-628-4020, hhahaha1@naver.com
• Received: June 23, 2012 • Revised: August 6, 2012 • Accepted: October 6, 2012
Copyright © 2013 The Korean Fracture Society
- 445 Views
- 1 Download
Abstract
-
Purpose
- We evaluated the clinical outcomes of tibia segmental fractures treated by intramedullary nailing using various reduction techniques.
-
Materials and Methods
- From January 2003 to June 2009, 18 segmental tibial fracture patients treated by intramedullary nail were enrolled with a minimum 12-month follow-up. The mean follow-up was 38 months (range 15-72). According to the AO classification, the fractures were types 42C2.1, 42C2.2, and 42C2.3 in four, ten, and four patients, respectively. Ten fractures were closed and eight were open. We used various techniques for reduction during operation and investigated bone union time and complication (non-union, malunion etc.).
-
Results
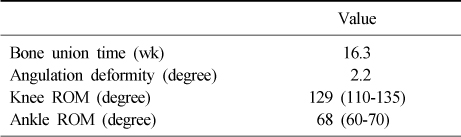
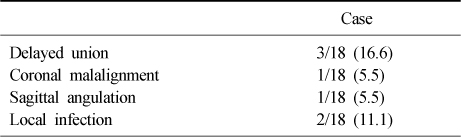
- Bone grafting was performed in three patients. Complete union was achieved in all patients. The mean time for union was 16.3 weeks (range 12-21), except in three delayed union patients. All radiological evaluations showed good alignment (less than 5 degree) except in two patients; and the mean deformity angle was 2.2 degree. Knee range of motion (ROM) was 129 degree, and ankle ROM was 68 degree. Local wound infection occurred in two patients.
-
Conclusion
- Intramedullary nailing is a successful method in the acute management of segmental tibial fractures, if accompanied by appropriate reduction technique.
- 1. Asche G. Results of the treatment of femoral and tibial fractures following interlocking nailing and plate osteosynthesis. A comparative retrospective study. Zentralbl Chir, 1989;114:1146-1154.
- 2. Bone LB, Kassman S, Stegemann P, France J. Prospective study of union rate of open tibial fractures treated with locked, unreamed intramedullary nails. J Orthop Trauma, 1994;8:45-49.
- 3. Bono CM, Levine RG, Rao JP, Behrens FF. Nonarticular proximal tibia fractures: treatment options and decision making. J Am Acad Orthop Surg, 2001;9:176-186.
- 4. Buehler KC, Green J, Woll TS, Duwelius PJ. A technique for intramedullary nailing of proximal third tibia fractures. J Orthop Trauma, 1997;11:218-223.
- 5. Byun YS, Shin DJ. Intramedullary nailing of proximal tibial fractures. J Korean Fract Soc, 2009;22:197-205.
- 6. Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop Relat Res, 1995;(315):25-33.
- 7. Giannoudis PV, Hinsche AF, Cohen A, Macdonald DA, Matthews SJ, Smith RM. Segmental tibial fractures: an assessment of procedures in 27 cases. Injury, 2003;34:756-762.
- 8. Hahn D, Bradbury N, Hartley R, Radford PJ. Intramedullary nail breakage in distal fractures of the tibia. Injury, 1996;27:323-327.
- 9. Kim JR, Lee HS, Choi MK, Lee KB, Park JH, Lee JM. Treatment of distal tibial fractures by interlocking intramedullary nailing. J Korean Soc Fract, 2003;16:348-355.
- 10. Krettek C, Stephan C, Schandelmaier P, Richter M, Pape HC, Miclau T. The use of Poller screws as blocking screws in stabilising tibial fractures treated with small diameter intramedullary nails. J Bone Joint Surg Br, 1999;81:963-968.
- 11. Laflamme GY, Heimlich D, Stephen D, Kreder HJ, Whyne CM. Proximal tibial fracture stability with intramedullary nail fixation using oblique interlocking screws. J Orthop Trauma, 2003;17:496-502.
- 12. Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop Relat Res, 1995;(315):64-74.
- 13. Melis GC, Sotgiu F, Lepori M, Guido P. Intramedullary nailing in segmental tibial fractures. J Bone Joint Surg Am, 1981;63:1310-1318.
- 14. Mosheiff R, Safran O, Segal D, Liebergall M. The unreamed tibial nail in the treatment of distal metaphyseal fractures. Injury, 1999;30:83-90.
- 15. Mueller CA, Eingartner C, Schreitmueller E, et al. Primary stability of various forms of osteosynthesis in the treatment of fractures of the proximal tibia. J Bone Joint Surg Br, 2005;87:426-432.
- 16. Park HB, Kang BJ, Song HR, Koo KH, Jeong ST, Cho SH. Screw breakage in tibial interlocking nailing. J Korean Soc Fract, 2002;15:483-488.
- 17. Robinson CM, McLauchlan GJ, McLean IP, Court-Brown CM. Distal metaphyseal fractures of the tibia with minimal involvement of the ankle. Classification and treatment by locked intramedullary nailing. J Bone Joint Surg Br, 1995;77:781-787.
- 18. Schmidt AH, Finkemeier CG, Tornetta P 3rd. Treatment of closed tibial fractures. Instr Course Lect, 2003;52:607-622.
- 19. Singer RW, Kellam JF. Open tibial diaphyseal fractures. Results of unreamed locked intramedullary nailing. Clin Orthop Relat Res, 1995;(315):114-118.
- 20. Tornetta P 3rd, Collins E. Semiextended position of intramedullary nailing of the proximal tibia. Clin Orthop Relat Res, 1996;(328):185-189.
- 21. Woll TS, Duwelius PJ. The segmental tibial fracture. Clin Orthop Relat Res, 1992;(281):204-207.
REFERENCES
Fig. 1
(A) A 54-year-old male patient, segmental tibial fracture.
(B) Initial stabilization of fibula and reduction technique using Steinmann pin.
(C) Union of the fracture 5 months later.
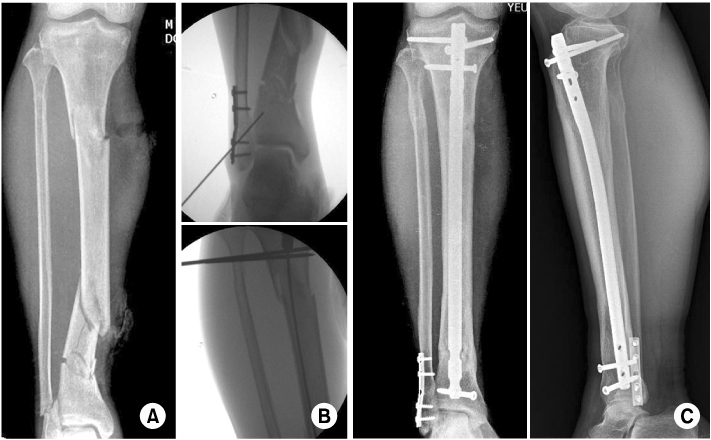
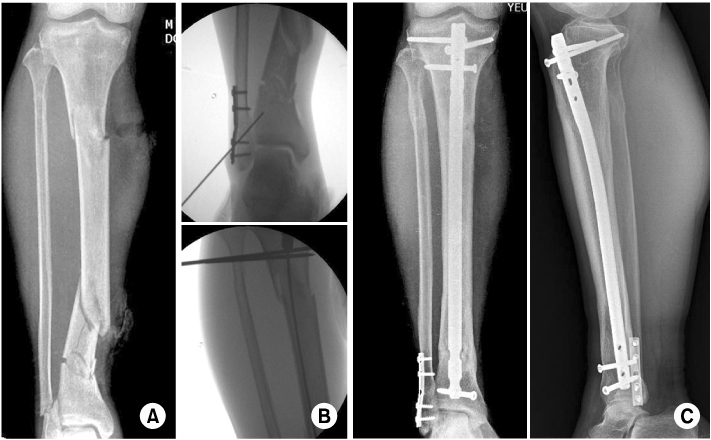
Fig. 2
(A) A 47-year-old male patient, segmental tibial fracture.
(B) Reduction technique using blocking screw.
(C) Union of the fracture 6 months later.


Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

Clinical Outcomes of the Tibia Segmental Fractures Treated by Intramedullary Nail Using Various Reduction Techniques
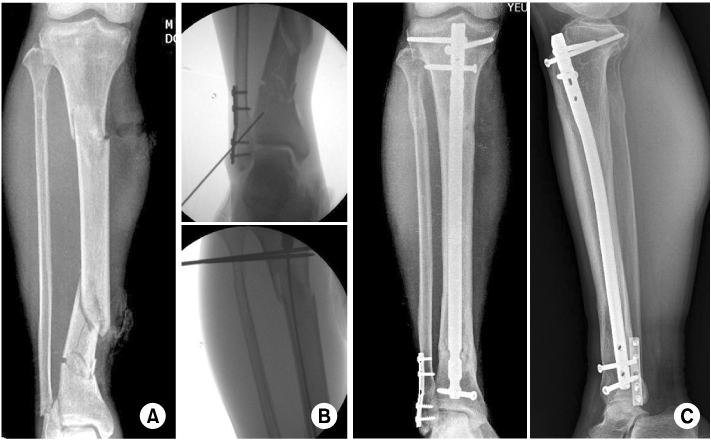


Fig. 1
(A) A 54-year-old male patient, segmental tibial fracture.
(B) Initial stabilization of fibula and reduction technique using Steinmann pin.
(C) Union of the fracture 5 months later.
Fig. 2
(A) A 47-year-old male patient, segmental tibial fracture.
(B) Reduction technique using blocking screw.
(C) Union of the fracture 6 months later.
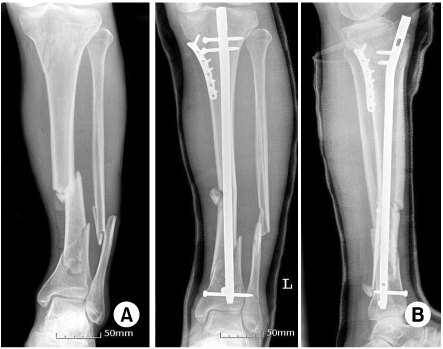
Fig. 3
(A) A 52-year-old male patient, segmental tibial fracture.
(B) Stabilization with a supplemental unicortical plate and expert nail.
Fig. 1
Fig. 2
Fig. 3
Clinical Outcomes of the Tibia Segmental Fractures Treated by Intramedullary Nail Using Various Reduction Techniques
Summary of Clinical Data
Values are presented as mean or mean (range). ROM: Range of motion.
Complications
Values are presented as number (%).
Table 1
Summary of Clinical Data
Values are presented as mean or mean (range). ROM: Range of motion.
Table 2
Complications
Values are presented as number (%).

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

