Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 26(2); 2013 > Article
-
Original Article
- Analysis of the Result Treated with Locking Compression Plate-Distal Tibia and Zimmer Periarticular Locking Plate in Distal Tibia Fracture
- Jun-Young Lee, M.D., Sang-Ho Ha, M.D., Sung-Won Cho, M.D., Sung-Hae Park, M.D.
-
Journal of the Korean Fracture Society 2013;26(2):118-125.
DOI: https://doi.org/10.12671/jkfs.2013.26.2.118
Published online: April 22, 2013
Department of Orthopaedic Surgery, College of Medicine, Chosun University, Gwangju, Korea.
- Address reprint requests to: Jun-Young Lee, M.D. Department of Orthopaedic Surgery, Chosun University Hospital, 365 Pilmun-daero, Dong-gu, Gwangju 501-717, Korea. Tel: 82-62-220-3147, Fax: 2-62-226-3379, leejy88@chosun.ac.kr
Copyright © 2013 The Korean Fracture Society
- 586 Views
- 0 Download
- 1 Crossref
Abstract
-
Purpose
- To evaluate the clinical and radiological results of minimally invasive plate, osteosynthesis, using either a locking compression plate-distal tibia (LCP-DT) or Zimmer periarticular locking plate (ZPLP) for distal tibia fractures.
-
Materials and Methods
- Fifty one patients (51 cases), who underwent minimally invasive osteosynthesis using locking compression plate for distal tibia fractures between October 2008 and August 2011, were followed for more than six months. Eighteen patients were treated with LCP-DT and 33 patients with ZPLP. Time to bony union and anatomic alignment were evaluated radiologically. Clinically, American Orthopedic Foot & Ankle Society ankle-hindfoot scales (AOFAS score) and range of ankle motion were assessed and compared between two groups.
-
Results
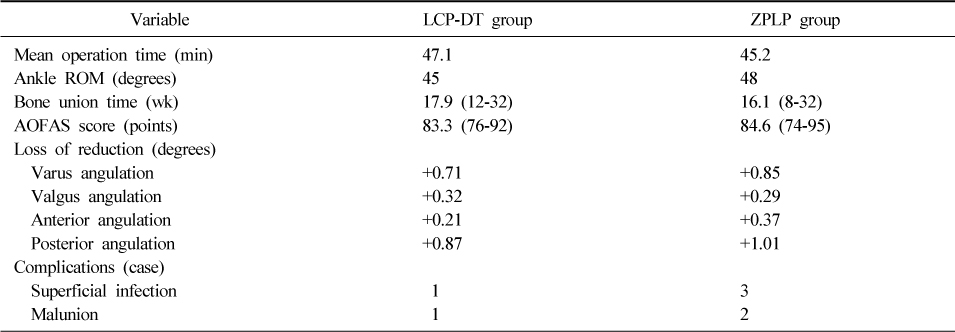
- All patients achieved bony union at an average of 18 weeks on LCP-DT group and 16weeks on ZPLP group. The average American Orthopedic Foot & Ankle Society ankle-hindfoot scales was 83.3 points on the LCP-DT group, 84.6 points on the ZPLP group, and range of ankle motion averaged at 45 degrees, 48 degrees, respectively.
-
Conclusion
- Both types of locking compression plates were effective when performing minimally invasive osteosynthesis for distal tibia fractures.
- 1. Anderson LD, Hutchins WC, Wright PE, Disney JM. Fractures of the tibia and fibula treated by casts and transfixing pins. Clin Orthop Relat Res, 1974;(105):179-191.Article
- 2. Asche G. Results of the treatment of femoral and tibial fractures following interlocking nailing and plate osteosynthesis. A comparative retrospective study. Zentralbl Chir, 1989;114:1146-1154.
- 3. Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma, 2001;15:153-160.Article
- 4. Bone LB, Johnson KD. Treatment of tibial fractures by reaming and intramedullary nailing. J Bone Joint Surg Am, 1986;68:877-887.
- 5. Borrelli J Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma, 2002;16:691-695.
- 6. Collinge C, Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma, 2010;24:24-29.
- 7. Dickson KF, Montgomery S, Field J. High energy plafond fractures treated by a spanning external fixator initially and followed by a second stage open reduction internal fixation of the articular surface--preliminary report. Injury, 2001;32:Suppl 4. SD92-SD98.PubMed
- 8. Edge AJ, Denham RA. External fixation for complicated tibial fractures. J Bone Joint Surg Br, 1981;63:92-97.PDF
- 9. Fisher WD, Hamblen DL. Problems and pitfalls of compression fixation of long bone fractures: a review of results and complications. Injury, 1978;10:99-107.
- 10. Hahn D, Bradbury N, Hartley R, Radford PJ. Intramedullary nail breakage in distal fractures of the tibia. Injury, 1996;27:323-327.PubMed
- 11. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury, 2007;38:365-370.PubMed
- 12. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia--results in 20 patients. Injury, 2006;37:877-887.PubMed
- 13. Helfet DL, Shonnard PY, Levine D, Borrelli J Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury, 1997;28:Suppl 1. A42-A47.PubMed
- 14. Karlström G, Olerud S. Fractures of the tibial shaft; a critical evaluation of treatment alternatives. Clin Orthop Relat Res, 1974;(105):82-115.
- 15. Khoury A, Liebergall M, London E, Mosheiff R. Percutaneous plating of distal tibial fractures. Foot Ankle Int, 2002;23:818-824.PubMedPDF
- 16. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int, 1994;15:349-353.PubMedPDF
- 17. Krackhardt T, Dilger J, Flesch I, Höntzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg, 2005;125:87-94.PDF
- 18. Lee KB, Song SY, Kwon DJ, Lee YB, Rhee NK, Choi JH. A comparison between minimally invasive plate osteosynthesis & interlocking intramedullary nailing in distal tibia fractures. J Korean Fract Soc, 2008;21:286-291.
- 19. Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop, 2004;28:159-162.PubMedPMCPDF
- 20. Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res, 2003;(408):286-291.
- 21. Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg, 1984;103:190-194.PubMedPDF
- 22. Park KC, Park YS. Minimally invasive plate osteosynthesis for distal tibial metaphyseal fracture. J Korean Fract Soc, 2005;18:264-268.
- 23. Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD. Tibial pilon fractures: a comparison of treatment methods. J Trauma, 1999;47:937-941.PubMed
- 24. Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury, 2004;35:615-620.
- 25. Ristiniemi J, Flinkkilä T, Hyvönen P, et al. Two-ring hybrid external fixation of distal tibial fractures: a review of 47 cases. J Trauma, 2007;62:174-183.PubMed
- 26. Ronga M, Longo UG, Maffulli N. Minimally invasive locked plating of distal tibia fractures is safe and effective. Clin Orthop Relat Res, 2010;468:975-982.
- 27. Streicher G, Reilmann H. Distal tibial fractures. Unfallchirurg, 2008;111:905-918.PDF
- 28. Trafton PG. Closed unstable fractures of the tibia. Clin Orthop Relat Res, 1988;(230):58-67.PubMed
REFERENCES


Figure & Data
REFERENCES
Citations

- Biomechanical analysis and clinical effects of bridge combined fixation system for femoral fractures
Da-xing Wang, Ying Xiong, Hong Deng, Fu Jia, Shao Gu, Bai-lian Liu, Qun-hui Li, Qi Pu, Zhong-zi Zhang
Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine.2014; 228(9): 899. CrossRef


Fig. 1
Fig. 2
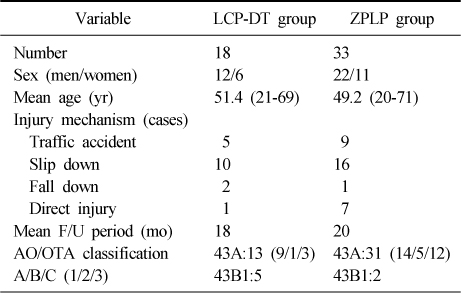
Demographic Data of the Patients
LCP-DT: Locking compression plate-distal tibia, ZPLP: Zimmer periarticular locking plate, F/U: Follow up, AO/OTA: Arbeitsgemeinschaft fur Osteosynthesefragen/Orthopaedic Trauma Association.
Results of LCP-DT and ZPLP Groups
LCP-DT: Locking compression plate-distal tibia, ZPLP: Zimmer periarticular locking plate, ROM: Range of motion, AOFAS: American Orthopedic Foot & Ankle Society ankle-hindfoot scales.
LCP-DT: Locking compression plate-distal tibia, ZPLP: Zimmer periarticular locking plate, F/U: Follow up, AO/OTA: Arbeitsgemeinschaft fur Osteosynthesefragen/Orthopaedic Trauma Association.
LCP-DT: Locking compression plate-distal tibia, ZPLP: Zimmer periarticular locking plate, ROM: Range of motion, AOFAS: American Orthopedic Foot & Ankle Society ankle-hindfoot scales.

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

