Search
- Page Path
- HOME > Search
Original Articles
- Correlation of bone mineral density with ankle fractures in older adults in Korea: a retrospective cohort study
- Seung Hyun Lee, Chae Hun Lee, Seo Jin Park, Jun Young Lee
- J Musculoskelet Trauma 2025;38(4):186-192. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00150
-
 Abstract
Abstract
 PDF
PDF - Background
Bone mineral density (BMD) is well-documented in relation to fractures of the spine, hip, distal radius, and proximal humerus; however, its correlations with other fracture types are less established. This study aimed to analyze BMD and associated risk factors in older adults (≥65 years of age) with osteoporotic ankle fractures. These fractures involve low-energy trauma, resulting from falls from a standing height or lower, and occur from impacts which typically do not cause fractures in individuals with normal bone.
Methods
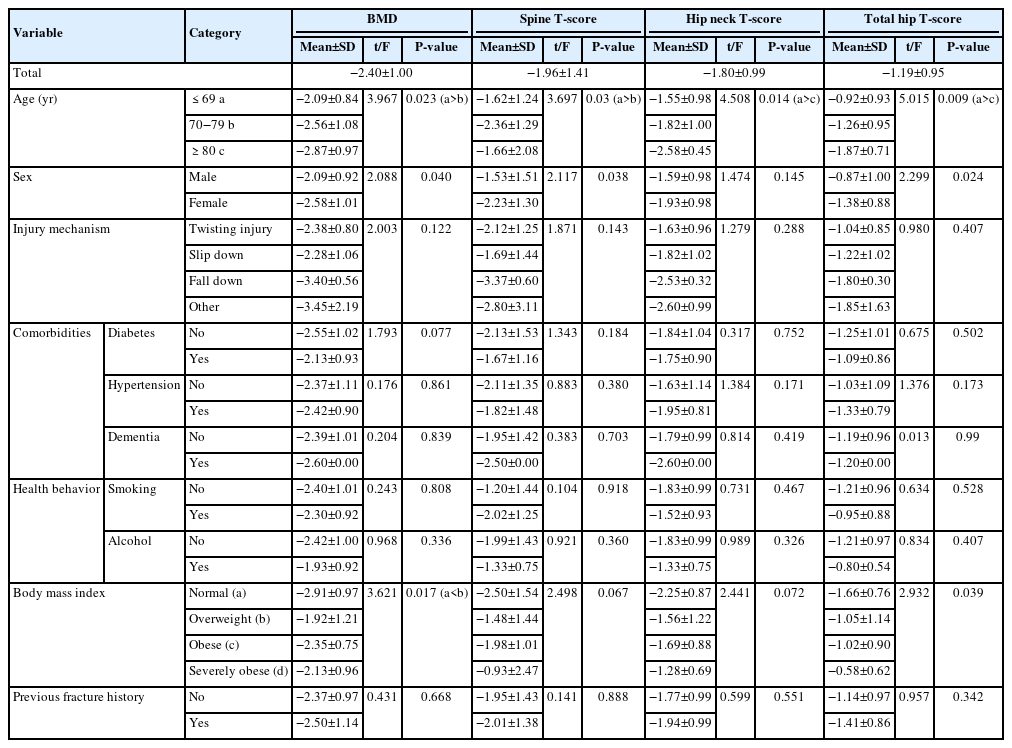
This retrospective study analyzed data from 1,411 patients diagnosed with ankle fractures admitted to Chosun University Hospital between February 2012 and April 2023. After applying inclusion criteria (age ≥65 years; low energy ankle fracture) and exclusion criteria (high energy trauma, open/multiple fractures, missing dual X-ray absorptiometry [DXA]), 73 of 1,411 patients were analyzed. Lumbar spine, femoral neck, and total hip T scores were obtained with a Horizon Wi DXA scanner, and associations with age, sex, mechanism of injury, comorbidities, smoking status, alcohol consumption, body mass index (BMI), and history of fractures were tested by ANOVA with Scheffe post hoc and Fisher exact tests.
Results
Lower BMD correlated significantly with older age, female sex, and lower BMI (P<0.05) in older adults with ankle fractures. No significant associations were observed for comorbidities (diabetes, hypertension, dementia), smoking, alcohol consumption, injury mechanism, or prior fractures.
Conclusion
These results indicate that older age, female, and lower BMI are linked to reduced BMD in ankle fracture patients over 65 years of age. Focused osteoporosis screening and management may therefore be most beneficial for older, low BMI women presenting with ankle fractures. Level of evidence: IV.
- 832 View
- 2,147,483,670 Download

- Comparison of Surgical Outcomes for Lisfranc Joint Injuries: Dorsal Bridge Plating versus Transarticular Screw versus Combination
- Ba Rom Kim, Jun Young Lee, Sung Hun Yang, Seung Hyun Lee
- J Korean Fract Soc 2023;36(1):17-24. Published online January 31, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.1.17
-
 Abstract
Abstract
 PDF
PDF - Purpose
In Lisfranc joint injury, the traditional treatment has been open reduction and internal fixation with a transarticular screw. Despite this, additional complications, such as damage to the articular surface and breakage of the screw, have been reported. Therefore, this study compared the clinical and radiological outcomes of dorsal bridge plating with those of transarticular screws and combination treatment in Lisfranc joint injury.
Materials and Methods
Among the 43 patients who underwent surgical treatment due to Lisfranc joint injury from June 2015 to March 2021, 40 cases followed for more than six months after surgery were analyzed, excluding three patients: one lost to follow-up, one had to amputate, and one expired. The radiological parameters were measured using the Wilppula classification in the last follow-up. The clinical outcomes were evaluated using the American Orthopaedic Foot and Ankle Society (AOFAS) midfoot score.
Results
The AOFAS midfoot score, according to the surgical method, was significantly higher in the dorsal bridge plating (p=0.003). The radiological outcomes showed significantly better anatomical reduction when dorsal bridge plating was used (p=0.040). According to the Wilppula classification, the AOFAS midfoot score improved as the quality of anatomical reduction improved (p=0.018). Finally, the AOFAS midfoot score decreased as the number of column fixations increased (p=0.002). There were two complications: screw breakage in dorsal bridge plating and superficial skin necrosis in the combination treatment. Skin defects caused by necrosis improved after negative pressure wound therapy and split-thickness skin graft.
Conclusion
In treating Lisfranc joint injuries, open reduction and internal fixation by dorsal bridge plating can be an appropriate treatment option. Nevertheless, studies, such as long-term follow-up research, on complications, such as osteoarthritis, will be needed.
- 727 View
- 8 Download

- Analysis of Clinical and Functional Outcomes according to the Blood Sugar Control Status at the Time of Ankle Fractures Resulting from Rotational Injuries
- Jun Young Lee, Dong Seop Lim, Seung Hyun Lee, Seo Jin Park
- J Korean Fract Soc 2022;35(4):135-141. Published online October 31, 2022
- DOI: https://doi.org/10.12671/jkfs.2022.35.4.135
-
 Abstract
Abstract
 PDF
PDF - Purpose
Patients with diabetes are known to have poor clinical outcomes due to the high incidence of complications after ankle joint fracture surgery. This study reports the clinical and functional outcomes based on glycemic control status among patients with ankle joint fractures who underwent surgical treatment.
Materials and Methods
Among patients who underwent surgical treatment due to ankle joint fractures from January 2015 to October 2019, 253 patients with a minimum follow-up of 12 months were identified. We divided them into 3 groups: 195 patients with no diabetes (Group A), 26 patients with well-controlled diabetes (Group B), and 32 patients with uncontrolled diabetes (Group C). In addition, patients with lateral, medial malleolar, bimalleolar, and trimalleolar fractures were identified using radi-ography. The functional outcome measures used for evaluation were the Revised Foot Function Index (FFI), Short Musculoskeletal Function Assessment (SMFA), and the Foot and Ankle Outcome Score (FAOS).
Results
Bone union at 3 months after surgery was high in Group A, showing significant differences compared to the other groups. There was a significant difference between the groups in the incidence of arthropathy and one or more complications. However, the FFI, SMFA, and FAOS did not show significant differences between the groups.
Conclusion
The incidence of complications was high in patients with uncontrolled diabetes compared to the patients with well-controlled diabetes and those with no diabetes. However, functional outcomes showed no significant difference.
- 640 View
- 6 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 First
First Prev
Prev


