Search
- Page Path
- HOME > Search
Original Articles
- Risk factors for ankle fractures in older adults based on clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities in Korea: a retrospective case-control study
- Myeong Jun Song, Se Woong Jang, Jun Young Lee, Seojin Park
- J Musculoskelet Trauma 2025;38(4):193-202. Published online October 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00143
-
 Abstract
Abstract
 PDF
PDF - Background
Ankle fractures are common in older adults; however, their relationship with osteoporotic fractures remains unclear. This study aimed to evaluate potential risk factors for ankle fractures in older adults by analyzing individual clinical components of the Fracture Risk Assessment (FRAX) tool and comorbidities.
Methods
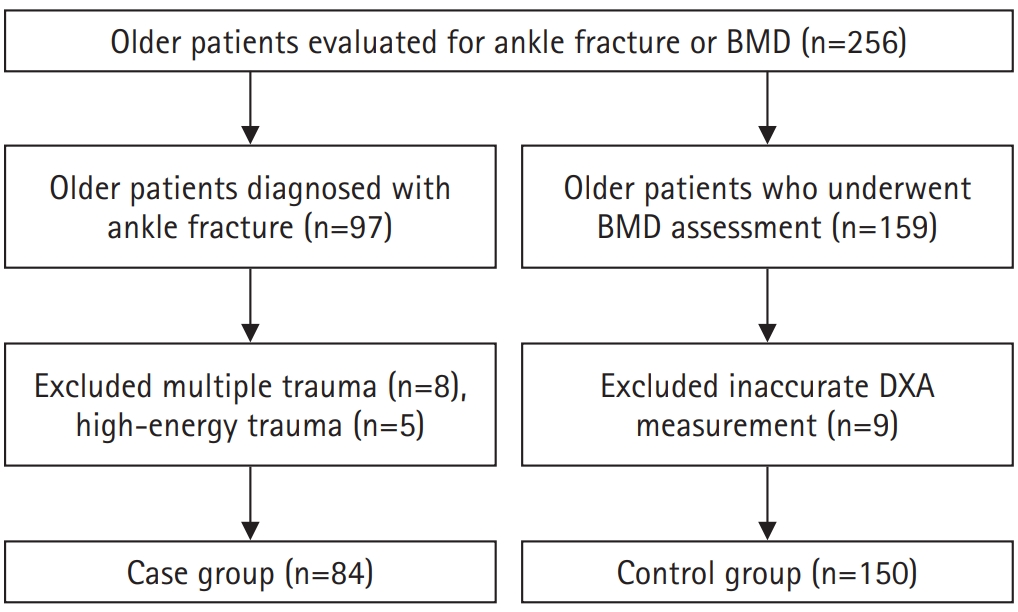
We conducted a retrospective case-control study including 84 patients aged ≥65 years with ankle fractures and 150 controls who underwent bone mineral density (BMD) testing without prior ankle fractures. The variables analyzed included age, sex, body mass index, smoking, alcohol consumption, prior fracture history, and comorbidities such as hypertension, diabetes mellitus, and dementia. BMD was measured at the spine, total hip, and femoral neck.
Results
Univariate analysis showed that alcohol consumption, diabetes mellitus, and total hip T-score categories were significantly associated with ankle fractures. In binary logistic regression, alcohol consumption remained significantly associated with higher ankle fracture risk (odds ratio [OR], 5.302; 95% confidence interval [CI], 1.778–15.811; P=0.003), and both osteopenia and osteoporosis at the total hip were also associated with increased risk (OR, 3.260, P=0.049; OR, 3.561, P=0.031, respectively). Diabetes mellitus did not reach statistical significance in the adjusted model (P=0.074). Model fit was adequate (Hosmer-Lemeshow P=0.377), and post hoc power analysis confirmed sufficient sample size.
Conclusions
These findings suggest that lower total hip BMD and alcohol-related factors may be associated with ankle fracture risk in older adults. The FRAX score itself was not calculated; instead, this study focused on analyzing selected clinical components. Limitations include the retrospective design, lack of fall and medication data, and cross-sectional BMD assessment. Level of evidence: III.
- 286 View
- 12 Download

- Demographic and Radiographic Parameters as Predictors of Reduction Loss after Conservative Treatment of Distal Radius Fractures in Adults
- Kyu Jin Kim, Dae Won Shin, Seong Kee Shin
- J Korean Fract Soc 2023;36(2):45-51. Published online April 30, 2023
- DOI: https://doi.org/10.12671/jkfs.2023.36.2.45
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study examined the demographic and radiological risk factors for later reduction loss of distal radius fractures treated conservatively. Materials and Methods This study enrolled patients treated for distal radius fractures between January 2017 and December 2019. Seventy-eight patients were included in the analysis and divided into two groups. The patients who showed minimal reduction loss within an acceptable radiologic angle after initial manual reduction were classified as Group A. The patients who showed reduction loss out of an acceptable radiologic angle and finally malunited or converted to surgical treatments were classified as Group B. The patient’s age and bone marrow density were used as demographic data. The initial X-ray images were evaluated to determine the fracture type. Various radiological parameters were measured. Results The 78-patient study cohort consisted of nine men and 69 women with a mean age of 67 years. Forty-eight cases were sorted into Group A, and 30 cases into Group B. On logistic regression analysis, the age of 80 or older was a risk factor for later fracture displacement among the demographic factors (p=0.037, odds ratio=4.937). Among the radiographic factors, the presence of distal ulnar fracture and dorsal cortical comminution were disclosed as risk factors of later displacement (p=0.049, 0.003, odds ratio=3.429, 7.196). Conclusion When conservative management for distal radius fracture is decided in patients more than 80 years of age or accompanied by a distal ulnar fracture or with dorsal cortical comminution, the possibility of later displacement of the distal radius should be considered.
- 380 View
- 1 Download

- Perioperative Blood Loss in Intramedullary Hip Screw for Intertrochanteric Fracture: Analysis of Risk Factors
- Jai Hyung Park, Hwa Jae Jung, Hun Kyu Shin, Eugene Kim, Se Jin Park, Taeg Su Ko, Jong Hyon Park
- J Korean Fract Soc 2015;28(1):53-58. Published online January 31, 2015
- DOI: https://doi.org/10.12671/jkfs.2015.28.1.53
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
We compared visible blood loss and calculated blood loss after intramedullary fixation in intertrochanteric fracture, and evaluated correlation between blood loss and its risk factors.
MATERIALS AND METHODS
A total of 256 patients who underwent closed reduction and intramedullary fixation in femoral intertrochanteric fracture between 2004 and 2013 were enrolled in this study. The total blood loss was calculated using the formula reported by Mercuiali and Brecher. We analyzed several factors, including fracture pattern (according to Evans classification), gender, age, body mass index (BMI), anesthesia method, cardiovascular and cerebrovascular disease, preoperative anemia, American Society of Anesthesiologists (ASA) score and use of antithrombotic agents.
RESULTS
Total calculated blood loss (2,100+/-1,632 ml) differed significantly from visible blood loss (564+/-319 ml). In addition, the blood loss of unstable fracture patient was 2,496+/-1,395 ml and multivariate analysis showed a significant relationship between blood loss and fracture pattern (p<0.01). However, other factors showed no statistically significant difference.
CONCLUSION
Total calculated blood loss was much greater than visible blood loss. Patients with unstable intertrochanteric fracture should be treated with care in order to reduce blood loss.
- 318 View
- 0 Download

- Neurologic Injury within Pelvic Ring Injuries
- Ji Wan Kim, Dong Hoon Baek, Jae Hyun Kim, Young Chang Kim
- J Korean Fract Soc 2014;27(1):17-22. Published online January 31, 2014
- DOI: https://doi.org/10.12671/jkfs.2014.27.1.17
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the incidence of neurologic injury in pelvic ring injuries and to assess the risk factors for neurologic injury related to pelvic fractures.
MATERIALS AND METHODS
Sixty-two patients with the pelvic ring injury were enrolled in the study from March 2010 to May 2013. When the neurologic injury was suspected clinically, the electro-diagnostic tests were performed. Combined injuries, fracture types, and longitudinal displacements were examined for correlations with the neurologic injury.
RESULTS
There were 7 cases of AO/OTA type A, 37 cases of type B, and 18 cases of type C. Among them, 25 patients (40%) had combined spine fractures, and the average of longitudinal displacement was 7 mm (1-50 mm). Of the 62 patients, 13 (21%) had neurologic injury related with pelvic fractures; 5 with lumbosacral plexus injury, 5 with L5 or S1 nerve injury, 2 with obturator nerve injury, and 1 case of lateral femoral cutaneous nerve injury. There were no relationships between the neurologic injuries and fracture types (p=0.192), but the longitudinal displacements of posterior ring and combined spine fractures were related to the neurologic injury within pelvic ring injury (p=0.006, p=0.048).
CONCLUSION
The incidence of neurologic injury in pelvis fracture was 21%. In this study, the longitudinal displacements of posterior ring and combined spine fractures were risk factors for neurological injury in pelvic ring injury. -
Citations
Citations to this article as recorded by- Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
Kwang Hee Yeo, Nam Hoon Moon, Jae Min Ahn, Jae Yoon Jeong, Jae Hoon Jang
Journal of the Korean Fracture Society.2018; 31(1): 9. CrossRef
- Surgical Outcome of Posterior Pelvic Fixation Using S1, S2 Screws in Vertically Unstable Pelvic Ring Injury
- 382 View
- 1 Download
- 1 Crossref

- Delirium after Intertrochanteric Fractures of Femur in Elderly Patients
- Kyu Bok Kang, Dong Hun Suh, Seong Rok Oh
- J Korean Fract Soc 2011;24(2):131-137. Published online April 30, 2011
- DOI: https://doi.org/10.12671/jkfs.2011.24.2.131
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To evaluate the incidence, risk factors and prognosis of delirium in elderly patients with intertrochanteric fractures of femur.
MATERIALS AND METHODS
162 patients who underwent operation for intertrochanteric fracture of femur from July 2005 to January 2007 were reviewed retrospectively. Delirium was diagnosed by using Confusion Assessment Method (CAM). Medical records were reviewed for the information of the patients, Gross motor function classification of Palisano et al. was used for the evaluation of ambulatory status. Univariate analysis and multivariate analysis were done to find out the risk factors.
RESULTS
2 cases out of 162 (1.2%) met the criteria of delirium at admission, and 39 cases (24.1%) after surgery. Univariate analysis and multivariate analysis identified age, hematocrit, dementia, the duration of opiate use, and pulmonary complication as risk factors. Hospital stay was longer and postoperative ambulatory status was worse in the patients with delirium.
CONCLUSION
Delirium is a frequent complication of intertrochanteric fractures of old age and associated with worse results. Cognitive function as well as physical status should be evaluated before and after surgery. Delirium needs more active prevention and treatment for better results. -
Citations
Citations to this article as recorded by- Incidence and Associated Factors of Delirium after Orthopedic Surgery
Si-Wook Lee, Chul-Hyun Cho, Ki-Cheor Bae, Kyung-Jae Lee, Eun-Seok Son, Sang-Hyun Um
Journal of the Korean Orthopaedic Association.2019; 54(2): 157. CrossRef - Laozi. De la figure du maître mythique à la divinité taoïque
Kyong-Kon Kim
Archimède. Archéologie et histoire ancienne.2019; 6: 16. CrossRef - Outcomes of Patients With Delirium in Long-Term Care Facilities: A Prospective Cohort Study
Kyoung Ja Moon, Heeok Park
Journal of Gerontological Nursing.2018; 44(9): 41. CrossRef - Relationship between Delirium and Clinical Prognosis among Older Patients underwent Femur Fracture Surgery
Jae-Lan Shim, Seon-Young Hwang
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(2): 649. CrossRef - The effects of a tailored intensive care unit delirium prevention protocol: A randomized controlled trial
Kyoung-Ja Moon, Sun-Mi Lee
International Journal of Nursing Studies.2015; 52(9): 1423. CrossRef - Automatic Delirium Prediction System and Nursing-Sensitive Outcomes in the Medical Intensive Care Unit
Ha-young Cho, Xianghua Song, Jinshi Piao, Yinji Jin, Sun-Mi Lee
Clinical Nursing Research.2015; 24(1): 29. CrossRef - Postoperative Delirium in Elderly Patients with Osteoarthritis Surgery: Incidence and Risk Factors
Eun A Park, Min Young Kim
Journal of muscle and joint health.2015; 22(2): 57. CrossRef - Is Delirium an Unrecognized Threat to Patient Safety in Korean Intensive Care Units?
Kyoung-Ja Moon, Jinshi Piao, Yinji Jin, Sun-Mi Lee
Journal of Nursing Care Quality.2014; 29(1): 91. CrossRef
- Incidence and Associated Factors of Delirium after Orthopedic Surgery
- 601 View
- 7 Download
- 8 Crossref

- Risk Factors of Postoperative Delirium in Elderly Patients with Hip Fractures
- Ki Hwan Kim, Duk Hwan Kho, Ju Yong Shin, Jin Yong Choi, Eung Sik Kim, Dong Heon Kim
- J Korean Fract Soc 2008;21(3):189-194. Published online July 31, 2008
- DOI: https://doi.org/10.12671/jkfs.2008.21.3.189
-
 Abstract
Abstract
 PDF
PDF - PURPOSE
To find out the relationship between various risk factors and post-operative delirium in elderly patients with hip fractures.
MATERIALS AND METHODS
Out of 135 patients older than 65 years old who underwent the surgery for hip fracture in our department, between the periods of March 2003 to March 2005, 14 patients (10.4%) developed post-operative delirium and 121 patients (89.6%) did not. We studied risk factors of post-operative delirium in two groups.
RESULTS
In chi-square test between delirium group and non-delirium group, the patients were more likely to develop post-operative delirium if they had previous episodes of delirium, abnormal cognitive function, low walking ability before admission, high dependency on ADL (Activities of Daily Living), other medical accompanying diseases, history of dementia, post-operative hypoxia, post-operative electrolyte imbalance, low post-operative hemoglobin and hematocrit, low post-operative albumin and were older than 75 years old (p<0.05). Sex, type of fracture, anesthesia and the time between admission and operation did not show much difference between the two groups.
CONCLUSION
The risk factors of postoperative delirium in elderly patients with hip fracture have a tendency to be multifactorial. Therefore, we conclude that being prepared by thorough understanding of the risk factors and their relationships will help prevent post-operative delirium and result in good postoperative prognosis. -
Citations
Citations to this article as recorded by- Increased Serum Neuropeptide Galanin Level Is a Predictor of Cognitive Dysfunction in Patients with Hip Fracture
Zichao Xue, Ke Zhang, Biao Luo, Long Fan, Ruizhe Zhao, Guangliang Hu, Yuzhen Xu
Disease Markers.2021; 2021: 1. CrossRef - Sleep Disturbance Strongly Related to the Development of Postoperative Delirium in Proximal Femoral Fracture Patients Aged 60 or Older
Myung-Rae Cho, Suk-Kyoon Song, Cheol-Hwan Ryu
Hip & Pelvis.2020; 32(2): 93. CrossRef - Incidence and Associated Factors of Delirium after Orthopedic Surgery
Si-Wook Lee, Chul-Hyun Cho, Ki-Cheor Bae, Kyung-Jae Lee, Eun-Seok Son, Sang-Hyun Um
Journal of the Korean Orthopaedic Association.2019; 54(2): 157. CrossRef - Relationship between Delirium and Clinical Prognosis among Older Patients underwent Femur Fracture Surgery
Jae-Lan Shim, Seon-Young Hwang
Journal of the Korea Academia-Industrial cooperation Society.2016; 17(2): 649. CrossRef - Relationship between Knowledge, Stress, and Nursing Performance about Care for Delirium in Geriatric Hospital Nurses
Eun-Hee Kim
Journal of Korean Clinical Health Science.2016; 4(2): 593. CrossRef - The effects of a tailored intensive care unit delirium prevention protocol: A randomized controlled trial
Kyoung-Ja Moon, Sun-Mi Lee
International Journal of Nursing Studies.2015; 52(9): 1423. CrossRef - Is Delirium an Unrecognized Threat to Patient Safety in Korean Intensive Care Units?
Kyoung-Ja Moon, Jinshi Piao, Yinji Jin, Sun-Mi Lee
Journal of Nursing Care Quality.2014; 29(1): 91. CrossRef - The Effects of Delirium Care Training Program for Nurses in Hospital Nursing Units
Moonja Kim, Haejung Lee
Korean Journal of Adult Nursing.2014; 26(5): 489. CrossRef - Knowledge, Performance and Stress about Care for Delirium in Orthopedic Hospital Nurses
Mi Young Kim, Young Eun
Journal of muscle and joint health.2013; 20(1): 72. CrossRef - The Experience of Delirium Care and Clinical Feasibility of the CAM-ICU in a Korean ICU
Joo-Hee Jung, Jung-Hye Lim, Eun-Jung Kim, Hyo-Chan An, Min-Kyung Kang, Jin Lee, Yu-Kyung Min, Eun-Zoo Park, Xiang-Hwa Song, Hye-Ryoung Kim, Sun-Mi Lee
Clinical Nursing Research.2013; 22(1): 95. CrossRef - Development and validation of the Korean Nursing Delirium Scale
Kyoung-Nam Kim, Cheol-Ho Kim, Kwang-Il Kim, Hyun-Jung Yoo, Si-Young Park, Yeon-Hwan Park
Journal of Korean Academy of Nursing.2012; 42(3): 414. CrossRef - Influencing Factors of the Incidence of Delirium in Elderly Patients with Arthroplasty
Young-Whee Lee, Hye-Bin Im, Eun-Jeong Jeong, Hee-Sun Ma
Korean Journal of Adult Nursing.2012; 24(4): 348. CrossRef - Delirium After Spinal Surgery in Korean Population
Jin Kyu Lee, Ye-Soo Park
Spine.2010; 35(18): 1729. CrossRef - The Incidence and Related Factors of Delirium in Elderly Patients with Hip Fracture after Surgery
Bo-Kyung Sohn, Yerl-Bo Sung, Eun-Jin Park, Dong-Woo Lee
Journal of the Korean Geriatrics Society.2010; 14(3): 162. CrossRef
- Increased Serum Neuropeptide Galanin Level Is a Predictor of Cognitive Dysfunction in Patients with Hip Fracture
- 1,136 View
- 4 Download
- 14 Crossref


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS

 First
First Prev
Prev


