Previous issues
- Page Path
- HOME > Browse articles > Previous issues
Original Articles
- Acute Compartment Syndrome of Thigh: Ten-Year Experiences from a Level I Trauma Center
- Hyung Keun Song, Won-Tae Cho, Wan-Sun Choi, Seung-Yeob Sakong, Sumin Im
- J Musculoskelet Trauma 2024;37(4):171-174. Published online October 25, 2024
- DOI: https://doi.org/10.12671/jmt.2024.37.4.171
-
 Abstract
Abstract
 PDF
PDF - Purpose
To assess the demographics, injury mechanisms, treatments, and outcomes of traumatic acute compartment syndrome in the thigh.
Materials and Methods
Patients diagnosed with thigh compartment syndrome were analyzed retrospectively at the authors’ level I trauma center from March 2012 to February 2022. Data were collected from medical and radiological records, focusing on demographics, injury details, treatment timelines, and clinical outcomes.
Results
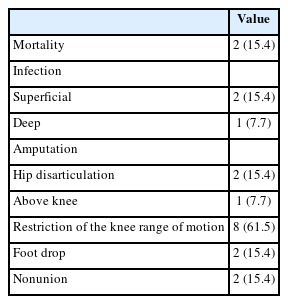
The cohort included 13 patients (11 males and 2 females) with a mean age of 46 years. Injuries primarily resulted from falls (6 patients) and vehicle accidents (5 patients). Fractures were noted in 11 patients, with seven involving the lower extremities and seven having open fractures; three of these were severe enough to be classified as Gustilo–Anderson type IIIc with associated femoral artery injuries. Time from the injury to fasciotomy ranged from within six hours to more than 24 hours. Fasciotomies were mainly single-sided (10 patients), targeting primarily the anterior compartments, and bilateral in three cases. Wound closures were performed using delayed primary closure (four patients) and partial- thickness skin grafts (five patients). Two patients died from multi-organ failure; other complications included infections (three patients), amputations (three patients), and long-term disabilities like drop foot (two patients), sensory deficits, joint stiffness (eight patients), and fracture non-unions requiring additional surgery (two patients).
Conclusion
Thigh-compartment syndrome, though infrequent, poses significant risks of mortality and chronic disability. This underscores the importance of prompt diagnosis and intervention.
- 1,759 View
- 52 Download

- Does the Operator’s Experience Affect the Occurrence of Complications after Distal Radius Fracture Volar Locking Plate Fixation? A Comparative Study of the First Four Years and Thereafter
- Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
- J Musculoskelet Trauma 2024;37(4):175-183. Published online October 25, 2024
- DOI: https://doi.org/10.12671/jmt.2024.37.4.175
- Correction in: J Musculoskelet Trauma 2025;38(1):40
-
 Abstract
Abstract
 PDF
PDF - Purpose
The management of distal radius fractures (DRFs) has evolved with the introduction of volar locking plate (VLP) fixation, offering stable fixation and better outcomes. Nevertheless, the impact of the surgeon’s experience on the complication rates in VLP fixation remains to be determined, particularly for less-experienced surgeons. This study compared the complication rates during the initial four years and subsequent two years of a hand surgeon’s practice of VLP fixation for DRFs.
Materials and Methods
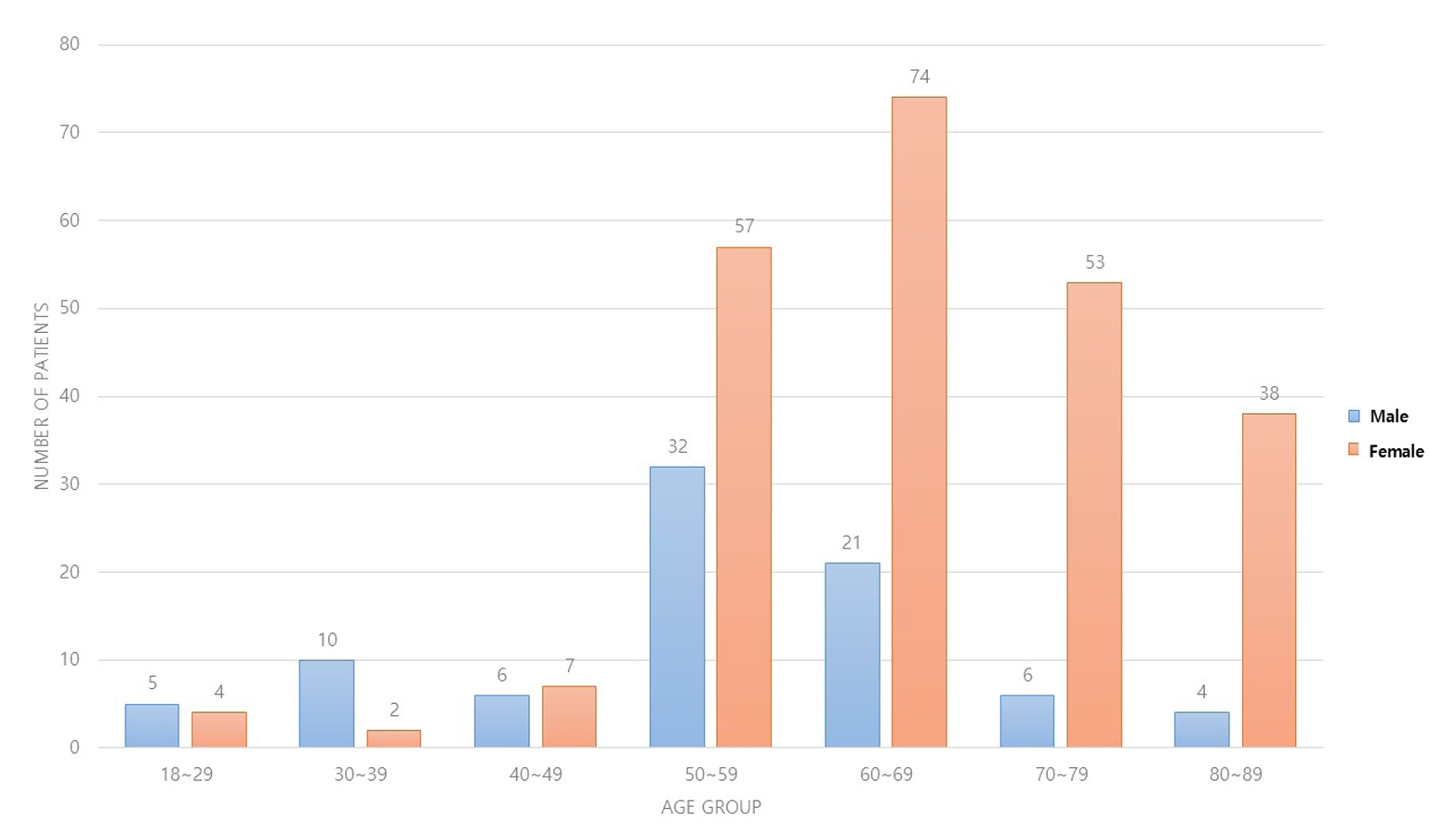
The data between March 2016 and December 2022 were analyzed retrospectively under the Institutional Review Board approval. A single surgeon performed all VLP fixation surgeries after finishing regular hand surgery training, with the first four years representing the less experienced phase (Group 1) and the following two years indicating the experienced phase (Group 2). The patients’ characteristics, operation-related factors, and postoperative complications, including tendon injuries, nerve-related complications, fixation and instrument-related issues, osteosynthesis-related problems, and infections, were compared. In addition, the authors compared the data with a large multicenter study conducted by experienced hand surgeons.
Results
Three hundred and nineteen patients (321 wrists) were included. The mean age was 63.3 years, and 26.3% were male and 73.7% were female. The operation time was 53.7±14.5 minutes and 74.4±26.5 minutes in groups 1 and 2, respectively, which was statistically significantly shorter (p<0.001). The complication rates between the two groups were similar, except for the higher implant removal rates in Group 1. A comparison with a previous multicenter study revealed higher reduction losses and carpal tunnel syndrome in this study, but the overall complication rate was low.
Conclusion
In DRF management, when the operating surgeon has completed an accredited training course, VLP fixation is a good treatment method that can be performed effectively even by less experienced surgeons with low complication rates. -
Citations
Citations to this article as recorded by- Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
Kee-Bum Hong, Chi-Hoon Oh, Chae Kwang Lim, Sungwoo Lee, Soo-Hong Han, Jun-Ku Lee
Journal of Musculoskeletal Trauma.2025; 38(1): 40. CrossRef - Characteristics of patients with distal radius fracture requiring arthroscopic foveal repair after bone union
Min Jung Park, Cheungsoo Ha, Hyun Tak Kang, Yong Hyun Yoon, Jun-Ku Lee, Soo-Hong Han
Arthroscopy and Orthopedic Sports Medicine.2025; 12(2): 70. CrossRef
- Author correction: “Does the operator's experience affect the occurrence of complications after distal radius fracture volar locking plate fixation? A comparative study of the first four years and thereafter”
- 2,593 View
- 53 Download
- 2 Crossref

Case Report
- Acute on Chronic Stress Fracture of a Varus Deformed Distal Tibia - A Case Report -
- Seong Kee Shin, Ki Chun Kim, Eli Schmidt, Seung Yeon Cho, Ki Chul Park
- J Musculoskelet Trauma 2024;37(4):184-189. Published online October 25, 2024
- DOI: https://doi.org/10.12671/jmt.2024.37.4.184
-
 Abstract
Abstract
 PDF
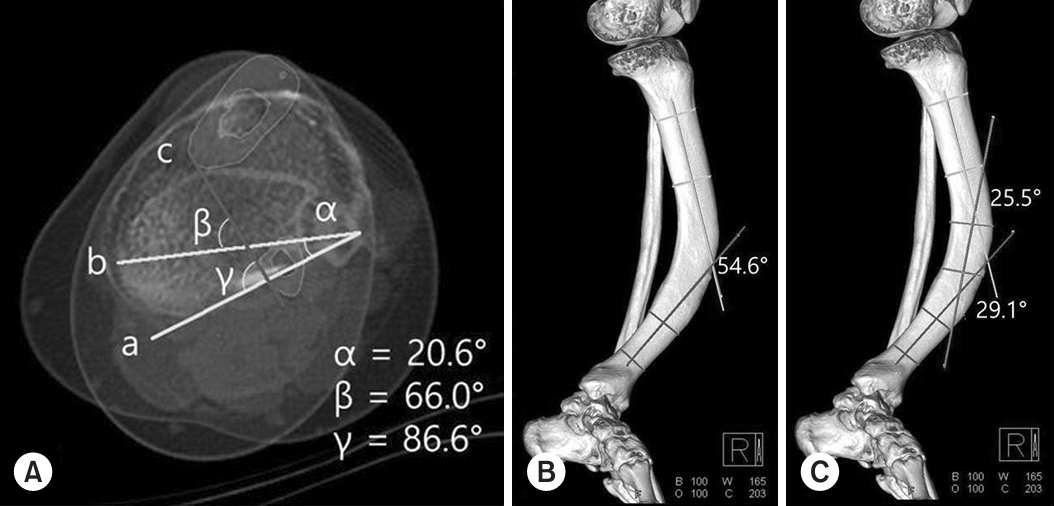
PDF - A severe post-traumatic distal tibia vara deformity is an uncommon condition in orthopedics. Typical symptoms include intractable recurrent pain, fragility related to stress fractures over the tensile area, and a limping gait caused by leg length discrepancy. Surgical management should be performed on acute fractures extending from a stress fracture gap. For successful surgical results, deformity correction is important for sustaining axial load bearing for standing and walking. Procedures to manage this condition have been proposed, but there is a high risk of complications, including metal failure, nonunion, and weakness caused by a long period of rehabilitation. In this case, the authors report a successful result using a modified clamshell osteotomy combined with a proximal and distal wedge bone resection in a single stage.
- 1,065 View
- 34 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS



 First
First Prev
Prev


