Previous issues
- Page Path
- HOME > Browse articles > Previous issues
Review Articles
- Current concepts in the management of phalangeal fractures in the hand
- Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):109-123. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00136
-
 Abstract
Abstract
 PDF
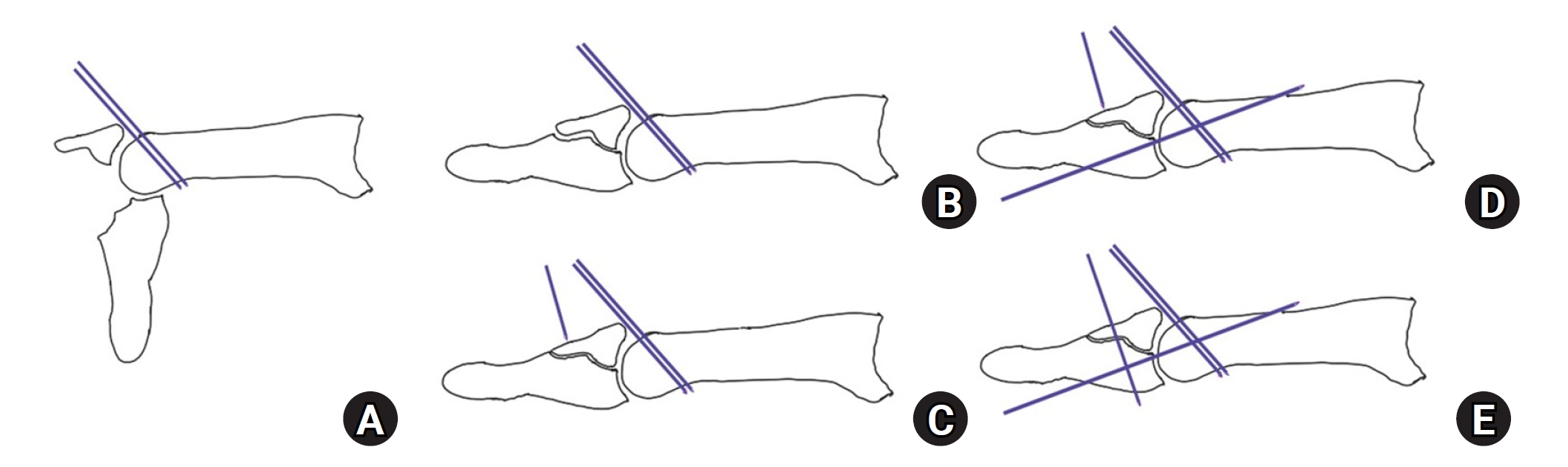
PDF - This review focuses on the treatment of hand fractures based on the anatomical location of the fractured phalanx, excluding the thumb, and examines recent studies on the topic. The main points are as follows: in most cases of hand fractures, conservative treatment should be prioritized over surgical intervention. The three key factors in determining whether surgical treatment is necessary are (1) whether the fracture is intraarticular, (2) the stability of the fracture itself, and (3) the extent of damage to surrounding soft tissues. The primary surgical treatment is closed reduction and Kirschner-wire fixation. The risk of rotational deformity increases with fractures closer to the proximal region. Intra- articular fractures may lead to subsequent stiffness and arthritis; thus, computed tomography is recommended to assess the fracture pattern. Anatomic reduction of intraarticular fragments is required, along with correction of the inherent joint instability. No surgical method has proven to be superior; it is advantageous for the surgeon to choose a surgical approach they are familiar with and confident in, based on the specific fracture and patient factors. Complications in hand fractures are various; the most frequent is stiffness, and nonunion is uncommon. Early joint motion is crucial in minimizing the risk of stiffness.
- 17,540 View
- 384 Download

- Atypical ulnar fractures: a narrative review of current concepts and a case of bilateral surgical management
- Chi-Hoon Oh, Hyun Tak Kang, Jun-Ku Lee
- J Musculoskelet Trauma 2025;38(3):124-132. Published online July 24, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00227
-
 Abstract
Abstract
 PDF
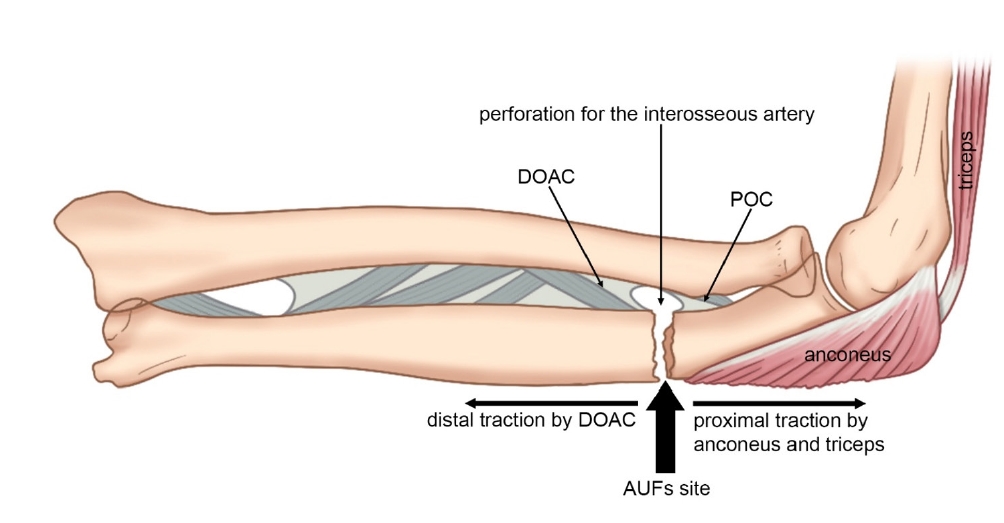
PDF - Atypical ulnar fractures (AUFs) are rare complications that are often linked to long-term antiresorptive therapy. Although atypical femoral fractures are well-studied, AUFs lack standardized diagnostic and treatment protocols. This review summarizes current knowledge on AUFs, including their pathophysiology, diagnostic criteria, and management. A case of bilateral AUFs treated with two distinct osteosynthesis methods is presented, emphasizing the principles of biological healing and mechanical stabilization.
- 1,526 View
- 47 Download

Original Articles
- Biomechanical finite element analysis of a femoral neck system fixation construct for femur neck fractures and clinical implications
- Hoon-Sang Sohn, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):133-142. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00108
-
 Abstract
Abstract
 PDF
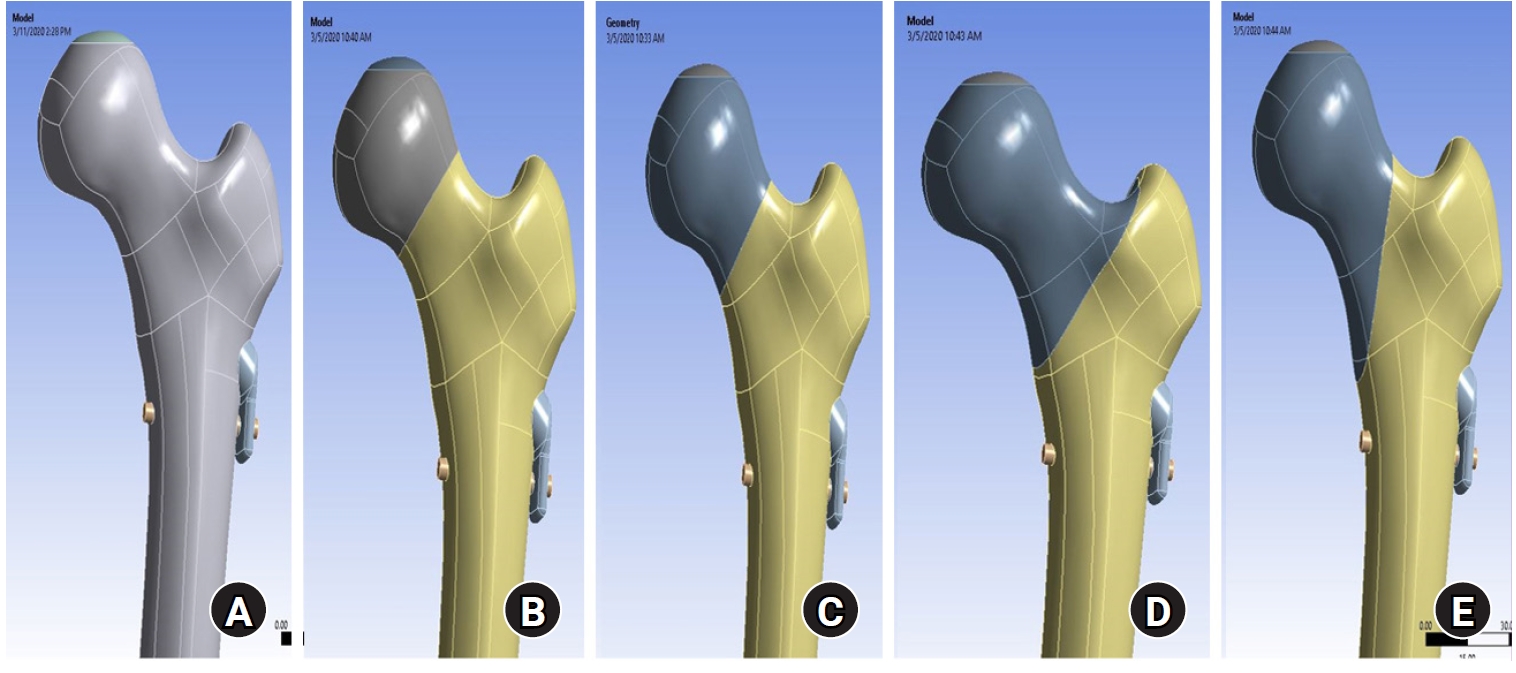
PDF - Background
This study assessed the structural/mechanical stability of fixation constructs with a femoral neck system (FNS) via finite element analysis after simulating femoral neck fractures and explored the clinical implications.
Methods
We simulated subcapital, transcervical, basicervical, and vertical fracture models using a right femur (SAWBONES) and imported the implant model of FNS to Ansys (Ansys 19.0, Ansys Inc.) to place the implant in the optimal position. The distal end of the femur model was completely fixed and was abducted 7°. The force vector was set laterally at an angle of 3° and posteriorly at an angle of 15° in the vertical ground. The analysis was conducted using Ansys software with the von Mises stress (VMS) in megapascals (MPa).
Results
The maximum VMS of the fracture site was 67.01 MPa for a subcapital, 68.56 MPa for a transcervical, 344.54 MPa for a basicervical, and 130.59 MPa for a vertical model. The maximum VMS of FNS was 840.34 MPa for a subcapital, 637.37 MPa for a transcervical, 464.07 MPa for a basicervical, and 421.01 MPa for a vertical model. The stress distribution of basicervical and vertical fractures differed significantly, and the basicervical fracture had higher VMS at the bone, implant, and fracture sites.
Conclusions
FNS fixation should be performed with consideration the osseous anchorage in the femoral head, and this technique might be appropriate for vertical fractures. Regarding the VMS at the fracture site, FNS might be applied cautiously only to basicervical fractures with anatomical reduction without a gap or comminution. Level of evidence: IV. -
Citations
Citations to this article as recorded by- Finite element analysis of screw thread geometry and titanium plate materials in internal fixation of the human femur
Abdessamed Bachiri, Mustapha Amine Arab, Nadia Kadouri
Computer Methods in Biomechanics and Biomedical Engineering.2026; : 1. CrossRef
- Finite element analysis of screw thread geometry and titanium plate materials in internal fixation of the human femur
- 1,944 View
- 82 Download
- 1 Crossref

- Computational simulation of coracoclavicular screw insertion through the superior distal clavicular plate for clinical applications in Korean cadavers
- Hyung-Lae Cho, Ji Han Choi, Se-Lin Jeong, Gu-Hee Jung
- J Musculoskelet Trauma 2025;38(3):143-151. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00122
-
 Abstract
Abstract
 PDF
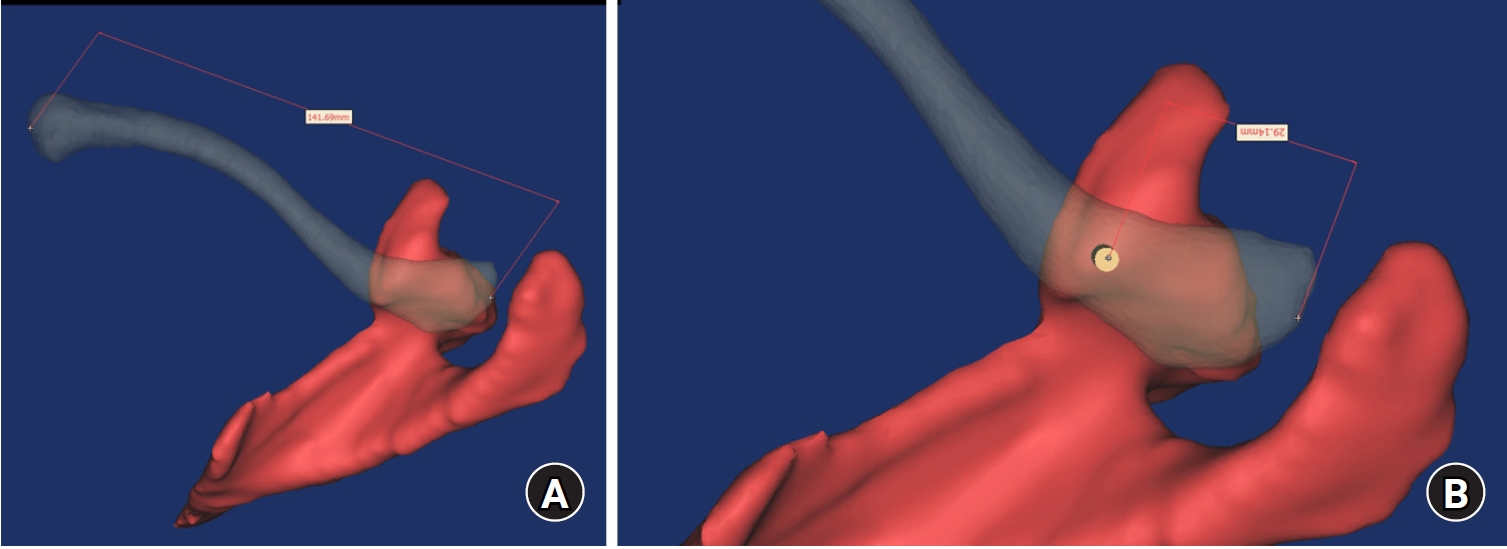
PDF - Background
The study was conducted to determine the practical area for inserting the coracoclavicular (CC) screw through the plate by analyzing three-dimensional (3D) shoulder models featuring virtually implanted, actual-size plates and screws.
Methods
Ninety cadaveric shoulders (41 males and 49 females) underwent continuous 1.0-mm slice computed tomography scans. The data were imported into image-processing software to generate a 3D shoulder model, including the scapula and clavicle. The overlapping area between the clavicle and the horizontal portion of the coracoid process (horizontal portion_CP) was analyzed in the cranial view. A curved pelvic recon plate was virtually placed on the upper surface of the distal clavicle, and an actual-size (3.5 mm) CC screw was inserted through the plate.
Results
The distal clavicle directly overlapped with the horizontal portion_CP in the vertical direction. The overlapping area was sufficient to place the 3.5 mm and 4.5 mm-sized screws. In all shoulder models, the CC screw could be inserted through the plate into the vertical direction, with an average length of 35.5 mm (range, 26.2–62.5 mm; standard deviation, 1.2 mm). In 87 models, the CC screw was inserted through the third hole from the lateral end of the plate. Two models were inserted through the second hole, and one model through the fourth hole.
Conclusions
The upper surface of the clavicle has sufficient overlapping area to place CC screws through the plate in the vertical direction in the corresponding hole. Supplemental CC screw fixation through the plate can be performed without additional or special equipment. Level of evidence: IV
- 674 View
- 22 Download

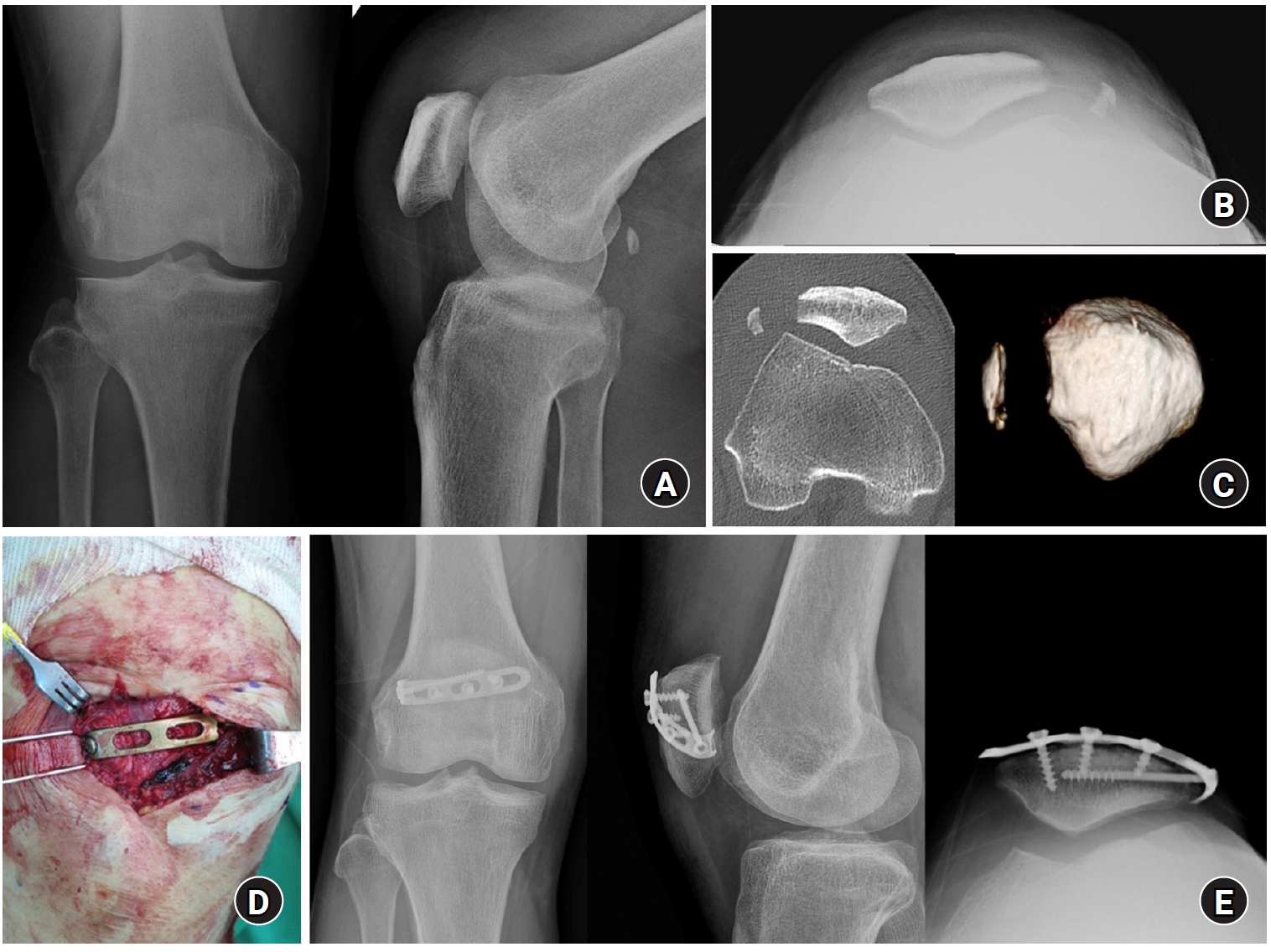
- Lateral marginal fractures of the patella and patellofemoral pain
- Jae-Ang Sim, Chul-Ho Kim, Ji Wan Kim
- J Musculoskelet Trauma 2025;38(3):152-159. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00171
-
 Abstract
Abstract
 PDF
PDF - Background
This study investigated the characteristics of lateral marginal fractures of the patella and evaluated the clinical outcomes.
Methods
We retrospectively reviewed all patients with lateral marginal fractures of the patella, defined as a vertical fracture line within 15 mm of the lateral patellar border, from 2008 to 2020. In total, 41 patients were included. Patient characteristics, radiologic findings, and clinical outcomes, including the Lysholm score at 1 year postoperation, were evaluated.
Results
The injury mechanisms were direct in 34 cases and indirect in seven. Furthermore, 85% of patients had a skyline view of the patella at the initial visit, and one medial subluxation of the patella was found. Forty of the 41 patients underwent surgery. Anatomical and nonanatomical (>1-mm displacement or excision) reductions were carried out in 36 cases (88%) and five cases (12%), respectively. The average Lysholm score was 89.1 (range, 67–99). The nonanatomical reduction group had a poorer functional score (79.8 vs. 90.4; P=0.010). Lateral patellar compression syndrome occurred in two patients with nonanatomical reduction.
Conclusions
Lateral marginal fractures of the patella affected patellofemoral stability. Anatomical reduction showed good functional outcomes, while nonanatomical reduction was associated with patellofemoral stability and pain. Therefore, surgeons should perform anatomical reduction with any appropriate fixation method. Level of Evidence: IV
- 1,324 View
- 26 Download

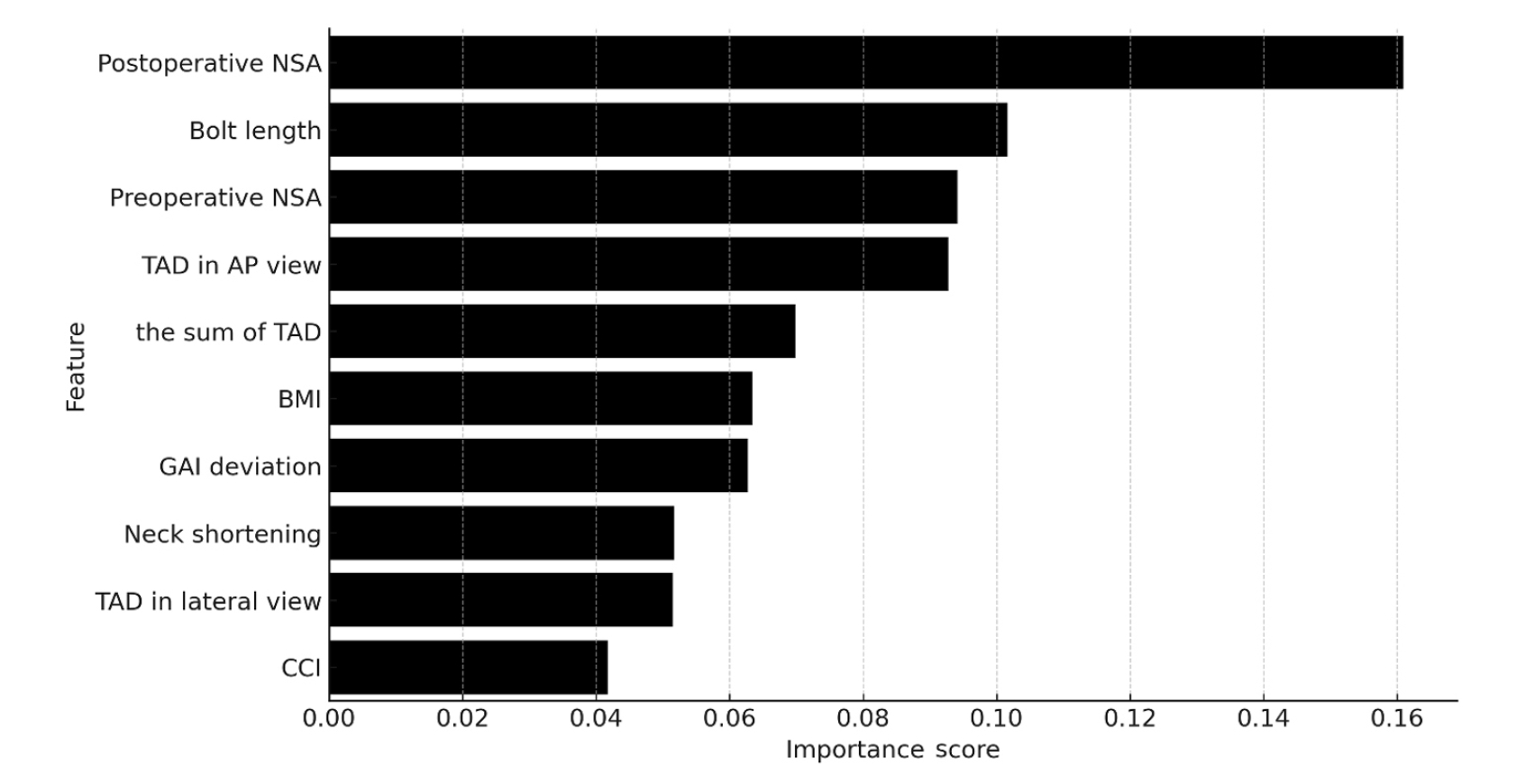
- Risk factors of surgical complications after use of the femoral neck system: a random forest analysis
- Chul-Ho Kim, Hyun-Chul Shon, Han Soul Kim, Ji Wan Kim, Eic Ju Lim
- J Musculoskelet Trauma 2025;38(3):160-167. Published online July 23, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00157
-
 Abstract
Abstract
 PDF
PDF - Background
The femoral neck system (FNS), a novel fixation device for managing femoral neck fractures (FNFs), has gained popularity in recent years. However, analyses of the surgical complications and reoperation risks associated with the use of FNS remain limited.
Methods
This retrospective observational study analyzed 57 patients who had undergone FNS fixation for FNF at two university hospitals between July 2019 and February 2024. Demographic, perioperative, and outcome variables, including age, sex, fracture classification (Garden, Pauwels, and AO), implant characteristics, tip-apex distance (TAD), neck shortening, and neck-shaft alignment, were analyzed. In addition to univariate analysis, a machine learning analysis was conducted using a random forest classifier with stratified sampling (80% training, 20% testing). The accuracy, precision, recall, F1-score, and area under the receiver’s operating curve were calculated to assess model performance.
Results
Ten patients experienced osteonecrosis of the femoral head (n=6), implant cut-out or penetration (n=3), and peri-implant fracture (n=1). Univariate analysis revealed that the TAD in the complication group was significantly shorter than that in the control group (12.1 vs. 16.7 mm; P=0.012). Additionally, neck shortening in the complication group was greater than that in the control group (4.9 vs. 2.3 mm; P=0.011). The random forest model achieved an accuracy of 83.3% and identified postoperative neck-shaft angle (NSA) as the most important predictor of complications (feature importance, 0.161), followed by bolt length (0.102) and preoperative NSA (0.094).
Conclusions
Risk factor analysis conducted using a random forest model identified postoperative NSA as the most important feature associated with postoperative complications following FNS. Therefore, care should be taken to normalize the postoperative NSA during FNF surgery. Level of Evidence: III. -
Citations
Citations to this article as recorded by- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
Seonghyun Kang, Wonseok Choi, Jeong Seok Choi, Eic Ju Lim, SungJin Ahn, Jong-Keon Oh, William T. Kent, Whee Sung Son, Jae-Woo Cho
Journal of Orthopaedic Surgery.2026;[Epub] CrossRef
- Length-stable fixation reduces femoral neck shortening in unstable femoral neck fractures: A retrospective comparative study of length-stable dynamic hip screw versus femoral neck system fixation
- 1,231 View
- 43 Download
- 1 Crossref

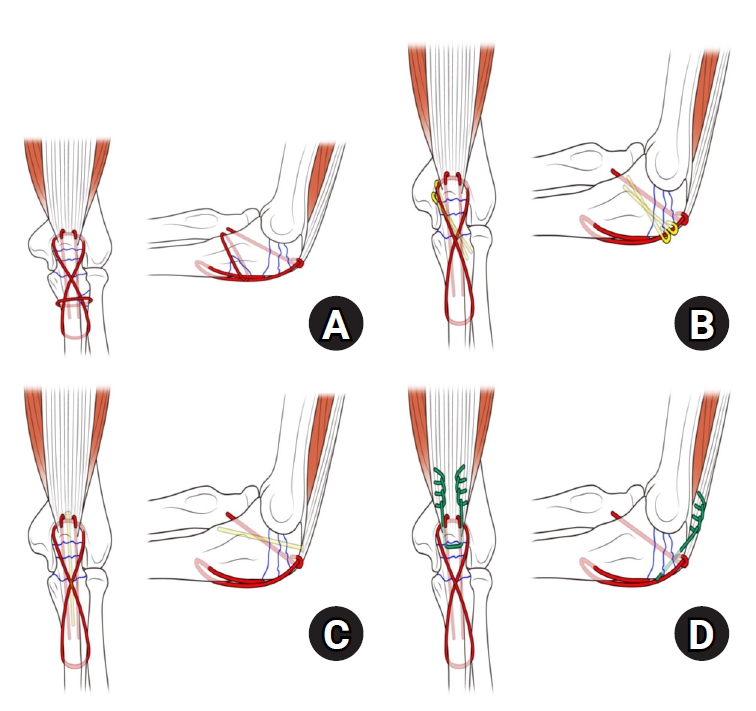
Correction
- Author correction: “Comparison of outcomes of reinforced tension band wiring and precontoured plate and screw fixation in the management of Mayo type IIIB olecranon fractures”
- Hyun Goo Kang, Tong Joo Lee, Samuel Jaeyoon Won
- J Musculoskelet Trauma 2025;38(3):168-168. Published online July 22, 2025
- DOI: https://doi.org/10.12671/jmt.2025.00059.e1
- Corrects: J Musculoskelet Trauma 2025;38(2):96
- 327 View
- 14 Download


 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS



 First
First Prev
Prev


