Articles
- Page Path
- HOME > J Musculoskelet Trauma > Volume 21(4); 2008 > Article
-
Review Article from Symposium
- What is an Ideal Treatment?
- Chang-Wug Oh, M.D.
-
Journal of the Korean Fracture Society 2008;21(4):347-352.
DOI: https://doi.org/10.12671/jkfs.2008.21.4.347
Published online: October 31, 2008
Department of Orthopaedic Surgery, School of Medicine, Kyungpook National University, Deagu, Korea.
- Address reprint requests to: Chang-Wug Oh, M.D. Department of Orthopaedic Surgery, School of Medicine, Kyungpook National University, 101, Dongin-dong 2-ga, Jung-gu, Deagu 700-422, Korea. Tel: 82-53-420-5630, Fax: 82-053-422-6605, cwoh@knu.ac.kr
Copyright © 2008 The Korean Fracture Society. All rights reserved.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 453 Views
- 1 Download
- 1. Brien WW, Wiss DA, Becker V Jr, Lehman T. Subtrochanteric femur fractures: a comparison of the Zickel nail, 95 degrees blade plate, and interlocking nail. J Orthop Trauma, 1991;5:458-464.
- 2. Curtis MJ, Jinnah RH, Wilson V, Cunningham BW. Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury, 1994;25:99-104.
- 3. Fracture and dislocation compendium. Orthopaedic trauma association committee for coding and classification. J Orthop Trauma, 1996;10:suppl 1. v-ix. 1-154.
- 4. Gerber C, Mast JW, Ganz R. Biological internal fixation of fractures. Arch Orthop Trauma Surg, 1990;109:295-303.
- 5. Johnson KD. Current techniques in treatment of subtrochanteric fractures. Tech Orthop, 1988;3:14-24.
- 6. Kim SJ, Oh CW, Jeon IH, et al. Minimally invasive plate osteosynthesis for distal femoral fractures. J Korean Soc Fract, 2003;16:474-481.
- 7. Kinast C, Bolhofner BR, Mast JW, Ganz R. Subtrochanteric fractures of the femur. Results of treatment with the 95 degrees condylar blade-plate. Clin Orthop Relat Res, 1989;238:122-130.
- 8. Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury, 1997;28:suppl 1. A20-A30.
- 9. Mahomed N, Harrington I, Kellam J, Maistrelli G, Hearn T, Vroemen J. Biomechanical analysis of the Gamma nail and sliding hip screw. Clin Orthop Relat Res, 1994;304:280-288.
- 10. Menezes DF, Gamulin A, Noesberger B. Is the proximal femoral nail a suitable implant for treatment of all trochanteric fractures? Clin Orthop Relat Res, 2005;439:221-227.
- 11. Oh CW, Oh JK, Kim SJ, et al. Minimally invasive plate osteosynthesis for comminuted subtrochanteric fracture of the femur. J Korean Fract Soc, 2006;19:407-411.
- 12. Pai CH. Dynamic condylar screw for subtrochanteric femur fractures with greater trochanteric extension. J Orthop Trauma, 1996;10:317-322.
- 13. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br, 2002;84:1093-1110.
- 14. Pryce Lewis JR, Ashcroft GP. Reverse LISS plating for proximal segmental femoral fractures in the polytrauma patient: a case report. Injury, 2007;38:235-239.
- 15. Ruff ME, Lubbers LM. Treatment of subtrochanteric fractures with a sliding screw-plate device. J Trauma, 1986;26:75-80.
- 16. Russell TA, Taylor JC. Subtrochanteric fractures of the femur. In: Browner BD, Jupiter JB, Levine AM, , editors. Skeletal trauma. Philadelphia: WB Saunders Co; 1992. p. 1485-1524.
- 17. Schatzker J, Mahomed N, Schiffman K, Kellam J. Dynamic condylar screw: a new device. A preliminary report. J Orthop Trauma, 1989;3:124-132.
- 18. Seinsheimer F. Subtrochanteric fractures of the femur. J Bone Joint Surg Am, 1978;60:300-306.
- 19. Tencer AF, Johnson KD, Johnston DW, Gill K. A biomechanical comparison of various methods of stabilization of subtrochanteric fractures of the femur. J Orthop Res, 1984;2:297-305.
- 20. Tordis TG. Stress analysis of the femur. J Biomech, 1969;2:163-174.
- 21. Vaidya SV, Dholakia DB, Chatterjee A. The use of a dynamic condylar screw and biological reduction techniques for subtrochanteric femur fracture. Injury, 2003;34:123-128.
- 22. Valverde JA, Alonso MG, Porro JG, et al. Use of the Gamma nail in the treatment of fractures of the proximal femur. Clin Orthop Relat Res, 1998;350:56-61.
- 23. Velasco RU, Comfort TH. Analysis of treatment problems in subtrochanteric fractures of the femur. J Trauma, 1978;18:513-523.
- 24. Yoshino N, Watanabe Y, Takenaka N, et al. Implant failure of long Gamma nail in a patient with intertrochanteric-subtrochanteric fracture. J Orthop Sci, 2006;11:638-643.
- 25. Zickel RE. A new fixation device for subtrochanteric fractures of the femur: a preliminary report. Clin Orthop Relat Res, 1967;54:115-123.
REFERENCES
Fig. 1

In subtrochanteric fractures, the proximal fragment is in abduction and flexion by the pulling of gluteus medius and iliopsoas muscle, and the distal fragment is in adduction by the adductor muscle.

Fig. 2

A varus malalignment with nonunion after cephalomedullary nailing of subtrochanteric fracture.

Fig. 3

(A, B, C) A comminuted subtrochanteric fracture was treated by MIPO (minimally invasive plate osteosynthesis) with DCS system. (D) The fracture healed uneventfully.

Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

What is an Ideal Treatment?
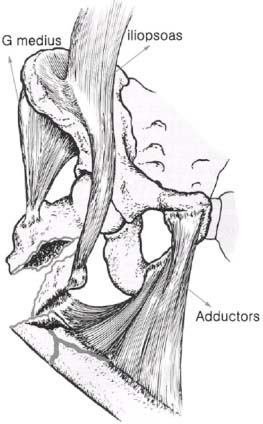


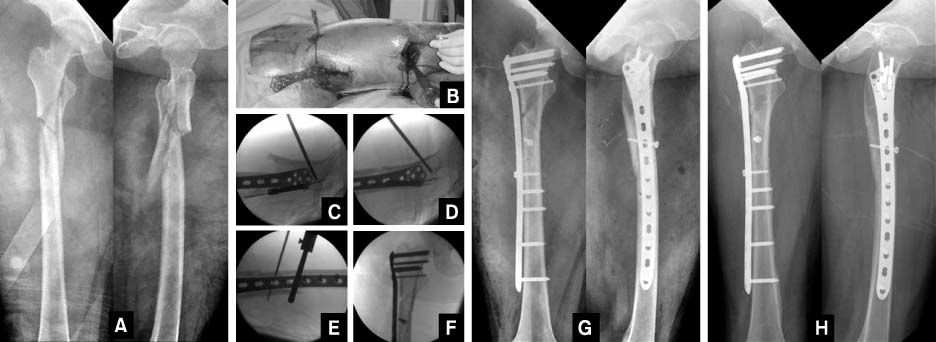
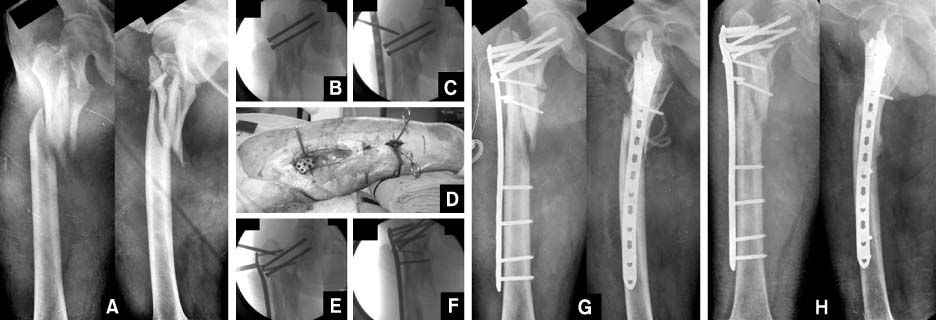
Fig. 1
In subtrochanteric fractures, the proximal fragment is in abduction and flexion by the pulling of gluteus medius and iliopsoas muscle, and the distal fragment is in adduction by the adductor muscle.
Fig. 2
A varus malalignment with nonunion after cephalomedullary nailing of subtrochanteric fracture.
Fig. 3
(A, B, C) A comminuted subtrochanteric fracture was treated by MIPO (minimally invasive plate osteosynthesis) with DCS system. (D) The fracture healed uneventfully.
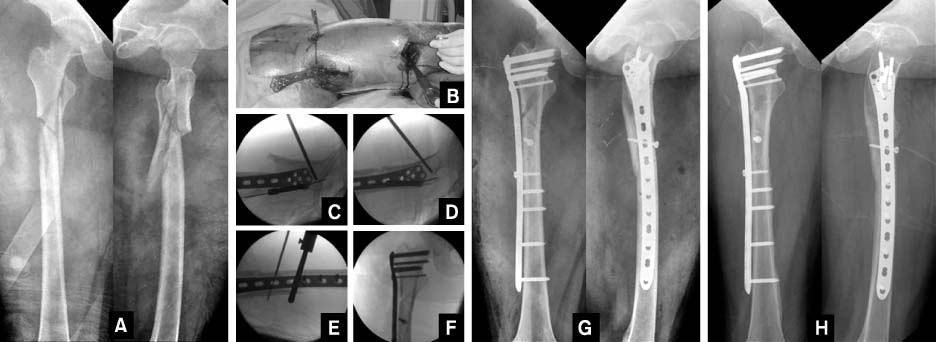
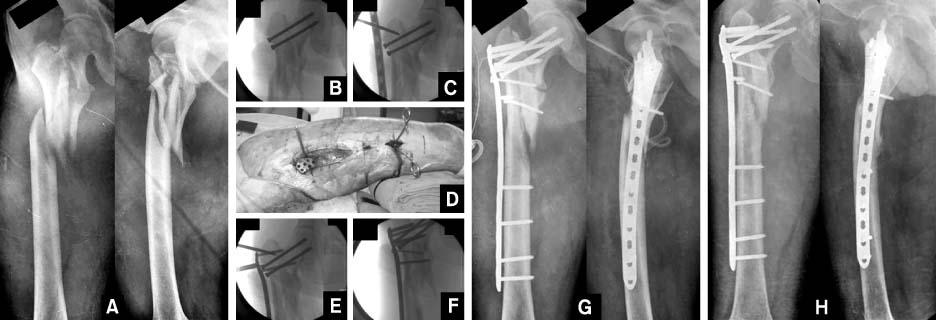
Fig. 4
In a subtrochanteric femoral fracture (A), MIPO was performed with various tips (joystick method, percutaneous lag screw) (B~F).
(G) A good alignment was achieved postoperatively.
(H) Union was achieved after 5 months.
Fig. 5
In a subtrochanteric femoral fracture extending to the neck (A), MIPO was performed after the fixation of neck fracture (B~F).
(G) A good alignment was achieved postoperatively.
(H) Union was achieved after 6 months.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
What is an Ideal Treatment?

 E-submission
E-submission KOTA
KOTA TOTA
TOTA TOTS
TOTS
 Cite
Cite

